ABSTRACT
Background: Several evaluative studies demonstrate that a well-coordinated Integrated Management of Childhood Illnesses (IMCI) program can reduce child mortality. However, there is dearth of information on how frontline providers perceive IMCI and how, in their view, the program is implemented and how it could be refined and revitalized.
Purpose: To determine the key challenges affecting IMCI implementation from the perspective of health care workers (HCWs) in primary health care facilities.
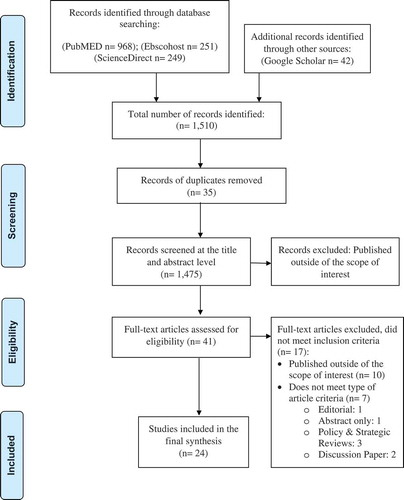
Methods: A scoping review based on the five-step framework of Arskey and O’Malley was utilized to identify key challenges faced by HCWs implementing the IMCI program in primary health care facilities. A comprehensive search of peer-reviewed literature through PubMed, ScienceDirect, EBSCOhost and Google Scholar was conducted. A total of 1,475 publications were screened for eligibility and 41 publications identified for full-text evaluation. Twenty-four (24) published articles met our inclusion criteria, and were investigated to tease out common themes related to challenges of HCWs in terms of implementing the IMCI program.
Results: Four key challenges emerged from our analysis: 1) Insufficient financial resources to fund program activities, 2) Lack of training, mentoring and supervision from the tertiary level, 3) Length of time required for effective and meaningful IMCI consultations conflicts with competing demands and 4) Lack of planning and coordination between policy makers and implementers resulting in ambiguity of roles and accountability. Although the IMCI program can provide substantial benefits, more information is still needed regarding implementation processes and acceptability in primary health care settings.
Conclusion: Recognizing and understanding insights of those enacting health programs such as IMCI can spark meaningful strategic recommendations to improve IMCI program effectiveness. This review suggests four domains that merit consideration in the context of efforts to scale and expand IMCI programs.
Responsible Editor Stig Wall, Umeå University, Sweden
Background
The World Health Organization (WHO), the United Nations Children’s Fund (UNICEF) and other partners developed the Integrated Management of Childhood Illnesses (IMCI) strategy in the mid-1990s to address child mortality and improve health care workers’ (HCWs) ability to diagnose, classify, and manage childhood illnesses [Citation1]. IMCI, a case-management strategy for common childhood illnesses, is designed primarily for non-physician clinicians working in resource-poor settings. IMCI guidelines are framed as a series of simple questions in a step-by-step algorithm, meant to help HCWs classify illnesses based on presenting signs and symptoms, severity and danger signs [Citation2–Citation5]. When used correctly, these guidelines have been shown to improve quality of care, and reduce the cost of treatment [Citation6–Citation8]. Since its inception, two key goals of the IMCI program have been to strengthen the capacity of HCWs to manage childhood illnesses, and to increase mothers’ abilities to recognize danger signs [Citation5,Citation9,Citation10]. Despite the successes of the IMCI program, few countries have achieved full expansion of IMCI implementation, and coverage remains problematic even after 20 years of IMCI implementation [Citation8,Citation11].
While there have been a number of systematic and analytic reviews conducted on IMCI, most emphasize the early stages of implementation and how IMCI contributes to reductions in childhood mortality and its effect on health systems [Citation7,Citation12]. Hansoti and colleagues [Citation13] have provided information on the reliability and validity of the IMCI tool in low- and middle-income countries (LMICs). Still other reviews have evaluated IMCI trainings in terms of effectiveness of a shortened training [Citation14], and whether trainings improve HCWs performance [Citation15,Citation16]. UNICEF [Citation11] published a working paper highlighting diverse scientific and programmatic evidence on IMCI from its establishment to the present. Poor families were viewed as greatly benefitting from IMCI because it could, in theory, increase equitable access to basic childcare services in revitalized and enabled the primary health care (PHC)-facilities [Citation3,Citation17]. However, evidence suggests implementation has suffered from larger structural problems and weakness in IMCI program execution by global and in-country partners [Citation8,Citation11,Citation12]. Jacobs and Merson [Citation18] note the failures of IMCI to provide continuous care between the home, first level PHC-facilities and referring health facilities. Generally speaking, IMCI’s impact on reducing inequity is difficult to assess given the varied extent of implementation [Citation19].
Although the existing body of evidence provides analysis of the impact of IMCI, little information exists regarding how the strategy can best be delivered in PHC-facilities from the perspective of HCWs [Citation7]. There is relatively less evidence in terms of how providers, who are the key actors in implementation, perceive the IMCI program in terms of quality, relevance, acceptability and sustainability.
To address this gap, we conducted a scoping review focusing on the experiences and perspectives of HCWs implementing IMCI in PHC-facilities in LMICs. This review aimed to provide a synthesis of the data and to lay the groundwork for health professionals, public health practitioners and policy makers to draw on perspectives of those at the frontlines of IMCI delivery when determining whether or how to refine program implementation.
Methods
The scoping review approach was based on the framework developed by Arksey and O’Malley [Citation20], which outlines an iterative and reflexive way of understanding the extent and range of the scientific literature on a given topic. The five-step framework entails: 1) identifying the research question, 2) identifying relevant studies, 3) selecting studies, 4) charting the data, and 5) collating, summarizing and reporting the results.
Identifying the research question
A brainstorming session was conducted to develop potential scoping questions focused around IMCI program implementation. The preliminary question was sent to members of the study team to evaluate its relevance and applicability. After discussions, the scoping question was refined to the following: determine the key challenges affecting IMCI implementation from the perspective of HCWs in PHC-facilities.
Following the finalization of the scoping question, core concepts were discussed and a set of keywords identified and narrowed down after checking Medical Subject Headings (MeSH) browser, including Non-MESH terms. Boolean operators were used to exhaust the variations of terms scoped. The final search strings and electronic databases searched are shown in .
Table 1. Electronic databases and search strings of the IMCI scoping review, 2018–2019
Identifying relevant studies
The lead author performed all searches from 27 December 2018–15 January 2019. Three electronic databases were used: PubMed, ScienceDirect and EBSCOhost, to identify peer-reviewed journals relating to the scope of review. Google Scholar was also used to search for publications in the grey literature. Only studies in English and only scientific papers from 2005 to 2018 were included. The majority of LMICs introduced the program by 1999–2004 and initial analytic reviews and a multi-country evaluation study were conducted in 2002–2005 [Citation21]. The 2005–2018 window was therefore selected to capture countries in the implementation and expansion phases discussed by the WHO Guidelines on IMCI Program [Citation8]. A full list of inclusion and exclusion criteria are outlined in .
Table 2. Inclusion and exclusion criteria of the IMCI scoping review, 2018–2019
Study selection and charting the data
The lead author listed all details, assessed and read the abstracts and evaluated whether they met the inclusion criteria, and noted themes emerging from analysis using Microsoft Excel. A data extraction spreadsheet was developed to chart the information in the literature, adapted from The Joanna Briggs Institute Reviewers’ Manual [Citation22]. Details were extracted regarding publication information, study design, methodology, sample population (if applicable), and all relevant information pertaining to the scoping questions.
Collating and summarizing the results
We used descriptive statistics to summarize all included studies. Counts and proportions were used to describe all other information gathered such as specific research design, publication details, and locale of the study. We also conducted a content analysis to summarize key concepts from the studies and relating to the study scope of interest [Citation23]. Each text pertaining to the experiences of the HCWs implementing IMCI program was coded or broken down into categories on a multi-level: words, word sense, phrase, sentence or theme. All included studies were read and re-read for content on the HCWs’ experiences and professional challenges. The lead author, working on printed copies of the studies with markers and highlighters, conducted the coding manually. Relevant statements were highlighted, with notes taken on themes emerging from our analysis. These notes helped to progress the substance of meanings and depth of understanding on the HCWs experience. All relevant data from the final included studies were extracted into the data extraction spreadsheet in Microsoft Excel. Coded data extracts for each theme were reviewed by the members of the study team (see Supplementary Table 1) to ensure patterns were clearly understood and defined. Themes were organized and reorganized through collaborative dialogues via Skype calls and email exchanges to arrive at consensus. We structure our results around common themes, to show the extent and range of themes within included studies. Initial analysis emphasizes various levels of implementation challenges. Later analysis led to the development of a four domains framework, reflecting the connections and relationship between each theme.
Results
A total of 1,475 publications were screened and assessed for eligibility based on inclusion and exclusion criteria. outlines this process. A total of 1,434 publications were screened out on initial assessment of the title and abstract; 41 publications were read full-text. Of these, 17 publications did not meet the inclusion criteria because their content was outside the scope of interest and/or they were not of the appropriate article type.
Characteristics of the included studies
This scoping review yielded 24 studies (see summary in Supplemental Table 1). Among these studies, 11 utilized quantitative designs (cross-sectional surveys, exploratory and observational surveys); eight were mixed-method designs, and the rest used a qualitative design. Three papers utilized a multi-country evaluation survey design. A majority of included studies were conducted in the WHO African region (65%), followed by the Eastern Mediterranean region (15%) and South-East Asia (10%); the remaining studies were conducted in the Americas, Western Pacific and European regions. The reviewed studies differed in study design, number of participants and length of the study. All included studies were published as research articles in peer-reviewed journals, most frequently in Health Policy and Planning (16.7%), BMC Health Services Research (8.3%), BMC Public Health (8.3%), PLOS One (8.3%) and Global Health Action (8.3%).
Key findings
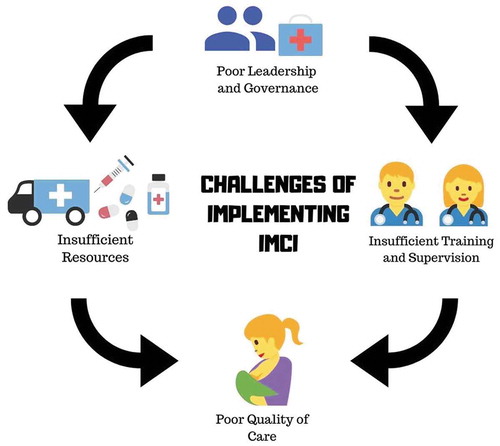
presents the key findings of the included studies, organized by theme. The findings identified the existing barriers reported in the implementation of the IMCI program, which limited the accomplishment of its program objectives, from the point of view of HCWs in PHC-facilities. Bottlenecks and challenges across four domains – (1) leadership and governance; (2) resources; (3) training, mentoring and supervision; and (4) quality of care – impede the optimal performance of the HCWs in delivery of IMCI services by causing staff turnover, demotivation and burnout. shows the interplays of the four main domains identified by this review. It highlights the negative effect of poor leadership and governance, lack of resources and inadequate training, all leading to poor performance of HCWs – and compromising care – in PHC-facilities.
Table 3. Key findings of the included studies in the scoping review, 2018–2019
Figure 2. Interplays of four main domains in IMCI implementation. Icons credit: courtesy of www.canva.com
Leadership and governance
Nine studies found that poor leadership dynamics and ineffective decentralization were among the main causes of failures in implementation of IMCI programs. A lack of planning and coordination, and wide communication gaps between various stakeholders, contributed to problems of limited coverage. Pradhan and colleagues [Citation24] expounded the ambiguity of the roles given to the HCW implementers. HCWs in Pakistan were uncertain about expected tasks for IMCI program implementation. An IMCI trained district level implementer said, ‘The ball is thrown in our court after providing IMCI training by MNCH [Maternal and Neonatal Child Health] program. I am helpless at this level … I am helpless … [Citation24],’ showing the disconnect between policy makers and implementers. Furthermore, in South Africa, Pandya and colleagues [Citation25] concluded that the lack of clarity of roles and accountability among various stakeholders were critical components of IMCI implementation failures.
Pandya and colleagues [Citation25] highlighted that there is a problem with integrating IMCI into existing health programs, which caused fragmentation of governance structures that influence the IMCI program and other child health programs. Other vertical programs such as expanded program on immunization (EPI) and tuberculosis were often prioritized and not synchronized to the IMCI program. Moreover, the coordinators managing these vertical programs were not trained in IMCI, creating a lack of awareness of the IMCI aspects within these child health programs. In Yemen, Basaleem and Amin [Citation26] also mentioned a lack of harmonization between IMCI and other programs in the health system, including overlapping programs on nutrition, immunization and malaria control, magnifying problems with poor IMCI implementation. HCWs sometimes said they were better off without IMCI due to inflexible rules and a lack of integration with other programs. They felt that they were losing time due to IMCI’s huge administrative burden and required reports.
Meanwhile, Huicho, et al [Citation27] found that one of the major constraints in scaling-up IMCI in Peru stemmed from problems within the health sector policy and strategic management levels. The lack of IMCI institutionalization at ministry or district levels had profound effects on service delivery in PHC-facilities. The lack of political commitment, poor governance, absence of specific budget allocations, and a failure to prioritize child health at the national level were also highlighted. Goga and Muhe [Citation28] also reported that among the challenges in scale-up in six countries was a lack of buy-in from the national stakeholders. Nsabagasani, et al [Citation29] in their study in Uganda also mentioned that donors shifted interests to the Integrated Community Case Management (iCCM) program and abandoned the IMCI program. One Ministry of Health official said: ‘At the moment we do not have money for continuing some of the IMCI activities the way we are supposed to. Donors have shifted to iCCM. We have adopted the IMCI approach as a routine, but we do not have needed resources to sustain some of the core activities including revision of guidelines and refresher training [Citation29]’.
Resources
A majority of studies (17 of 24) highlighted issues of inadequate human and material resources. These studies found that some of the IMCI recommendations are not carried out because of insufficient support from the government and stakeholders. Vhuromu & Davhana-Maselesele [Citation30] explored the experiences of HCWs in South Africa, highlighting the lack of human and material resources as one of the reasons that hampered the implementation of IMCI services in Limpopo province. Because of problems with shortages of medication, HCWs said there were instances that they referred patients to nearby hospitals just to get medications, even if it was not otherwise necessary. Physical structures did not support the delivery of IMCI services (for example, the rooms were not big enough to render counseling services). Participants in the study said, ‘There is no open space as the rooms are very small. This fails us to implement the rehydration plan for a dehydrated baby according to the IMCI standards [Citation30]’. Such poor working conditions led HCWs to suffer from ‘burnout’ (such as exhaustion and poor morale), which affected the uptake of the IMCI program.
The basic materials and supplies required to provide care under IMCI were often lacking. In Ethiopia, Seid and Sendo [Citation31] showed that 57% of nurses in four districts reported a lack of essential drugs, IMCI wall charts and chart booklets. Pandya, et al [Citation25] in their study in Gauteng province in South Africa also reported major deficiencies in medical supplies, such as a shortage of growth monitoring equipment, as well as vitamin A and deworming drugs, due to the poor performance of the centralized drug dispensing system. In Yemen, Basaleem & Amin [Citation26] found shortages of mothers’ counseling cards (the IMCI recommendation was to give one to every mother), as well as the unavailability of thermometers and issues with drug supply. Participants in the study said, ‘The last time we received drugs was 6 months back, and most of the commonly prescribed drugs are either finished or about to finish and we will not receive a new supply in the near future [Citation26].’ Because of these inadequacies, HCWs were dissatisfied with the working conditions when applying some of the IMCI recommendations.
Training, mentoring and supervision
Several studies (14 of 24) highlighted the short duration and cost of IMCI training, as well as poor supervision and lack of follow-up after training, which affected the performance of HCWs. Horwood, et al [Citation4] in their study in Limpopo and Kwazulu-Natal province in South Africa found that the standard 11-day IMCI training was too short to acquire all skills required and that the follow-up after training was insufficient to ensure competency in the conduct of the comprehensive assessments. HCWs’ compliance to IMCI algorithms was uneven and HCWs often made incorrect classifications even after the training. The study found a need to re-evaluate the training materials and methods to ensure that the IMCI program was properly implemented.
Goga and Muhe [Citation28] also concluded in a multi-country survey of 27 countries (representing the six WHO regions) that a majority of countries struggled to conduct follow-ups after IMCI training, mainly due to insufficient funding to cover travel costs, a limited number of trained supervisors, and inadequate job aids for follow-up. Difficulties in achieving adequate reach and coverage of IMCI training were also reported; HCWs who were supposed to implement IMCI needed approximately 11–16 days of training, according to WHO guidelines, but were criticized by national IMCI focal persons or representatives from Ministries of Health for requiring this amount of time. IMCI training was found to be logistically difficult and expensive, as HCWs needed to leave their workplace, thus creating problems of lack of personnel to manage the PHC-facilities during trainings. The cost and time for these trainings, frequent changes in staff and a lack of skilled facilitators and training sites significantly contributed to limited uptake of implementation of the IMCI program. Rowe and colleagues [Citation32] in southeastern Benin also revealed obstacles of supervision at multiple levels of the health system. IMCI supervision checklists were too long, leading to demotivation. Among the root causes of why supervision was not effectively occurring, there was also no standard method of supervision, a lack of committees to coordinate supervision and problems of decentralization.
Seid and Sendo [Citation31] also reported that 89% of trained HCWs were not getting any supervision, and that training was inadequate due to limited mentoring and a lack of refresher courses. HCWs in South Africa and India also shared the same sentiments, namely that support from supervisors was poor and no regular supervision was conducted [Citation30,Citation33]. Huicho, et al [Citation27] found that only 43.5% of trained HCWs in Peru received follow-up visits, and that those supervisory activities were not IMCI-specific and were usually conducted as part of other vertical programs (such as immunization, acute respiratory infections). Facilitators and course directors in a multi-country survey also experienced difficulties integrating IMCI follow-up activities into their routine duties and responsibilities, and facilitators felt that their presence was unwelcome during site visits [Citation28]. Results also highlighted how hierarchical tensions between HCWs and supervisors contributed to demotivated IMCI staff [Citation28]. HCWs viewed supervision as a punitive rather than positive or corrective procedure. One participant said, ‘Participants feel supervisors will police them [Citation28]’.
Quality of care
Nearly half of the articles included in the review (10 of 24) found that HCWs’ IMCI assessments were not performed consistently and comprehensively, and that clinical activities not related directly to the presenting complaint were frequently omitted. Such incomplete case assessments could lead to misclassification and missed referrals. For example, in Ethiopia, Gerensea and colleagues [Citation34] documented that out of 384 cases, 37.2% were classified incorrectly and 57.3% were wrongly treated. Despite nationwide training and expansion of the program, in their study of 4 sub-Saharan African countries (Namibia, Kenya, Tanzania and Uganda), Krüger and colleagues [Citation35] also reported that HCWs failed to recognize IMCI danger signs and primary symptoms, which are crucial for the succeeding steps in the IMCI algorithm. Moreover, in South Africa nutritional assessments such as checking for signs of malnutrition were not conducted, and providing advice on feeding practices was usually omitted [Citation4]. Thus, HCWs often failed to promote breastfeeding and provide counseling about complementary feeding.
There was notably poor adherence to IMCI case management procedures regarding the prescription of antibiotics [Citation36]. Naimoli and colleagues (2006) showed that IMCI-trained HCWs do not always follow the guidelines. Specifically, physicians with higher levels of pre-service training tended to prescribe more antibiotics to children, since they felt that the guidelines were only suggestions and not binding guidance.
Further, HCWs faced problems with long IMCI consultations, given the shortage of manpower in their clinics, resulting in longer waiting hours for patients and making it impossible to implement it properly [Citation31,Citation37,Citation38]. HCWs reported needing 20 minutes to an hour for a single IMCI consultation, causing longer patient waiting times, or requiring HCWs to skip steps in the IMCI algorithm due to time constraints [Citation25,Citation39]. As one participant said, ‘The problem is when there are a lot of people in the clinic, there is no time for you to go through all those things for the child. You will be working fast fast fast to push the queue. Sometimes, sisters (nurses) will just be looking at conditions that the child has been brought with and then they leave the rest and you find that the child has not received immunizations and stuff like that [Citation25]’. Further, the IMCI-trained HCWs were also required to provide other health care services, which limited their availability, creating a cycle of insufficient staffing [Citation38].
Discussion
This scoping review examined a range of factors that impede the uptake and implementation of IMCI from the perspective of HCWs, providing further detail to the implementation challenges discussed in Boschi-Pinto and colleagues’ study [Citation40], which provided a high-level and global view of IMCI implementation. While earlier reviews such as Bryce’s [Citation21] highlighted the positive role and contribution of the IMCI program in strengthening health systems, more recent literature highlights the uneven nature of IMCI implementation across countries. Our review focuses on the point of view of HCWs, and finds that IMCI implementation works best with a program structure with strong leadership and governance, with HCWs specifically dedicated to scaling-up IMCI program implementation at national, governorate and district levels, with the ultimate goal of having a positive impact on child health. Unfortunately, only a few countries achieved a full scale-up and implementation frequently remains incomplete especially in PHC-facilities [Citation40,Citation41]. We found major barriers to HCWs’ successful delivery of IMCI at PHC-facilities, more commonly, HCWs struggled to deliver IMCI services due to non-enabling and unsupportive health systems.
The sustainability of IMCI has been considered a major concern among LMIC stakeholders since the beginning of program rollout in early 1990s. Bryce’s review [Citation21] found that expectations of health systems improvements were only partially fulfilled based on the IMCI impact model, due to some weakness in program design execution and lack of basic health system structures. Our results parallel those of the ‘Strategic Review’ of the IMCI program conducted by the WHO and UNICEF, which reported that after 20 years, IMCI was suffering from waning interest and decreased funding, making it difficult to reach IMCI coverage at scale [Citation42]. Our review suggests that HCWs in PHC-facilities struggle to keep up to the evolving pace in the health system, as there are major competing child health programs that make HCWs unsure of what to prioritize and how to deliver IMCI services.
The lack of training and resources, and minimal supervision after training were among the weakest areas of IMCI implementation, as identified here and in studies of other LMICs [Citation27,Citation32,Citation33,Citation43]. Our work also highlights the magnitude of the poor supervision and monitoring after the early phases of implementation of IMCI in LMICs, reflecting larger problems relating to scale-up, such as lack of political commitment, human resources issues, fragmented program management and ineffective decentralization [Citation24,Citation25,Citation30,Citation32,Citation40,Citation44–Citation46]. It appears that IMCI programs are also not harmonized to other vertical programs, creating linkage issues for HCWs [Citation25,Citation26,Citation47]. HCWs lack clear roles around the IMCI program and often received no clear directives from higher authorities, resulting in fragmentation of services. As a result, HCWs lost their motivation to perform their duties because of inadequate resources and mis-aligned structures. Indeed evidence from other systematic reviews and global health studies confirms that the performance, attrition and retention of frontline HCWs are linked to intrinsic and extrinsic motivational factors such as being proud of their contributions to communities, opportunities for skills improvement and self-development, supportive supervision, proper remuneration, and healthy organizational cultures and work environments [Citation48–Citation50]. Some recent studies, for example, highlight opportunities to motivate health care providers in terms of performance-based incentives [Citation51,Citation52] and team-based goals and incentives model [Citation50].
In the light of the WHO Health Systems Framework [Citation53], it is also clear that IMCI programs should strike a better balance between and among the six building blocks to achieve desired child health outcomes. We identified leadership and governance as a strong determinant, suggesting opportunities to proceed by refining other blocks in a flexible manner given country-specific contexts. Indeed it has already been seen that IMCI can be a lever to improve the overall existing health system [Citation10,Citation21,Citation24,Citation25]. In Egypt, IMCI was shown to strengthen the health system, improve the availability of medicines, supplies and equipment [Citation54]. Leon, et al [Citation55] also described how some sub-Saharan African countries (Ethiopia, Mali and Niger) used IMCI to tackle problems in the health system, especially in relation to human resources, by intensifying their delivery of basic health services through a two-tiered community health worker system. Namely, volunteers and HCWs were given clear roles and were provided with training, stipends and essential supplies to perform their work [Citation55].
Major progress has been made in terms of HCW knowledge and child health through the accelerated implementation of IMCI when HCWs were adequately supported. Rakha, et al [Citation54] reported that the proportion of caretakers’ knowledge on antibiotics use increased from 7% to 67% or above when the child was seen by IMCI-trained HCWs. Moreover, treatment was more often sought from community HCWs and eventually led to substantive availability of medicines as well as equipment and supplies. Masanja, et al [Citation17] from their study in rural Tanzania, demonstrated that the IMCI program led to significant improvements in child health (such underweight, stunting, measles immunization among others) and also bolstered improvements in caretakers’ knowledge on danger signs. Mohan, et al [Citation33] also provided evidence on the improvement of some key newborn and child care practices such as increased health seeking behavior for acute respiratory infections, and early initiation and exclusive breastfeeding.
To ensure that the IMCI program stays relevant after 20 years, further implementation research is needed to understand what works and what does not at the implementation level [Citation56,Citation57]. International and national efforts to strengthen district health management teams should be the linchpin of this effort, and it is imperative to update existing policies to ensure adequate fiscal space for the IMCI program at this level [Citation18,Citation19,Citation58]. It is critical for the future of the IMCI program and child health that policy and implementation levels work more closely. Doherty and colleagues [Citation58] outlined evidence supporting the presence of a well-functioning district health system as a core component in improving quality of care in child health programs, specifically the IMCI program. Egypt and Tanzania have successfully allocated a separate funding stream for IMCI within all district budgets to ensure sufficient and reliable funding of program activities [Citation11]. The health system must also consider the importance of legitimacy and ownership at district level [Citation58–Citation60]. In Nepal and Democratic Republic of Congo (DRC), strengthening district health capacity has been an integral part in reaffirmation of IMCI and prevents donor-driven re-prioritization [Citation58]. Experiences from Kenya and Tanzania also highlight that positive uptake can be attributed to empowered district leaders [Citation61,Citation62].
Review strengths and limitations
Due to its precise inclusion criteria and the large scope of literature on the IMCI program, this review may have inadvertently excluded some articles discussing factors of relevance to implementation of IMCI at PHC-facility level. Although the researchers believed that the exhaustive search terms utilized in this review captured the relevant publications within the scope of interest, we might have missed other relevant studies that were not published in the databases used. However, a biomedical librarian was consulted to help finalize the search strategy, to ensure the most important articles were included. While we believe we have been able to thoroughly describe the literature on IMCI implementation challenges at the PHC-facility level, the diversity of contexts in which IMCI is implemented means that researchers should exercise caution in generalizing findings about the challenges of scaling-up of the IMCI program. Finally, while a second coder was not used to extract themes, we believe this limitation is mitigated by the involvement of co-authors sufficiently familiar with the literature to validate findings.
Conclusion
This review demonstrates the range and extent of literature regarding conditions that impede the uptake and implementation of IMCI globally from the lens of the frontline providers. Our review highlighted opportunities to tease out some bottlenecks in program implementation, revealing four critical domains which frequently underpin a negative feedback loop. It shows that the experiences of HCWs in implementing IMCI showed demotivating realities of an unsupportive health system and weak program execution. National and international efforts are needed to magnify the adequate fiscal space for increasing investment in the IMCI program. Government leadership, along with more structured and continued resource and training support, is necessary to foster sustainable IMCI health care services within the needs of the local community. Additional evidence is required on the quality of IMCI program implementation across country contexts and study settings. In this regard, future implementation research should be conducted in PHC-facility settings delivering the IMCI to explore program processes and acceptability by HCWs.
Author contributions
Conceived and conceptualized the study: MDR, KB, SM. Conducted analysis and performed data interpretation: MDR, KB, SM, SD. Prepared the initial draft of the manuscript and contributed to the report writing and critically reviewed the manuscript: MDR, KB, SM, SD.
Ethics and consent
Not applicable.
Paper context
As IMCI reaches its 20-year milestone; it is critical to draw lessons from the lens of health care workers (HCWs) to amplify IMCI reach and coverage. This review provides a synthesis of HCWs key challenges in implementing the IMCI program in primary health care facilities. Further, this review provides support to the revitalization of IMCI to respond to the changing landscape in child health.
Supplemental Material
Download MS Word (34.3 KB)Acknowledgments
The lead author acknowledges the scholarship grant received from Katholischer Akademischer Ausländer-Dienst (KAAD). We acknowledge financial support for open access publishing from Heidelberg Institute of Global Health, University of Heidelberg.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplementary data for this article can be accessed here
Additional information
Funding
References
- Gove S. Integrated management of childhood illness by outpatient health workers: technical basis and overview. The WHO working group on guidelines for integrated management of the sick child. Bull World Health Organ. 1997;75:7–12. Epub 1997/ 01/01.PubMed PMID: 9529714; PubMed Central PMCID: PMCPMC2486995.
- Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–440. Epub 2014/ 10/05. PubMed PMID: 25280870.
- Taffa N, Chepngeno G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health. 2005;10:240–245. Epub 2005/02/26. PubMed PMID: 15730508.
- Horwood C, Vermaak K, Rollins N, et al. An evaluation of the quality of IMCI assessments among IMCI trained health workers in South Africa. PLoS One. 2009;4:e5937. Epub 2009/06/19. PubMed PMID: 19536288; PubMed Central PMCID: PMCPMC2693922.
- Arifeen SE, Hoque DM, Akter T, et al. Effect of the integrated management of childhood illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: a cluster randomised trial. Lancet. 2009;374:393–403. Epub 2009/ 08/04. PubMed PMID: 19647607.
- Armstrong Schellenberg JR, Adam T, Mshinda H, et al. Effectiveness and cost of facility-based Integrated Management of Childhood Illness (IMCI) in Tanzania. Lancet. 2004;364:1583–1594. Epub 2004/ 11/03. PubMed PMID: 15519628.
- Gera T, Shah D, Garner P, et al. Integrated management of childhood illness (IMCI) strategy for children under five. Cochrane Database Syst Rev. 2016;CD010123. Epub 2016/ 07/06. DOI:10.1002/14651858.CD010123.pub2. PubMed PMID: 27378094; PubMed Central PMCID: PMCPMC4943011.
- WHO. Integrated management of childhood illnesses global survey report. Switzerland: World Health Organization; 2017.
- Lambrechts T, Bryce J, Orinda V. Integrated management of childhood illness: a summary of first experiences. Bull World Health Organ. 1999;77:582–594. Epub 1999/ 08/13.PubMed PMID: 10444882; PubMed Central PMCID: PMCPMC2557705.
- El Arifeen S, Blum LS, Hoque DM, et al. Integrated Management of Childhood Illness (IMCI) in Bangladesh: early findings from a cluster-randomised study. Lancet. 2004;364:1595–1602. Epub 2004/ 11/03. PubMed PMID: 15519629.
- UNICEF. Integrated Management of Childhood Illness (IMCI) in the 21st century: a review of the scientific and programmatic evidence. New York: United Nations Children’s Fund (UNICEF); 2016.
- WHO. The analytic review of the integrated management of childhood illness strategy. Geneva (Switzerland): World Health Organization; 2003.
- Hansoti B, Jenson A, Keefe D, et al. Reliability and validity of pediatric triage tools evaluated in Low resource settings: a systematic review. BMC Pediatr. 2017;17 37. Epub 2017/01/27. PubMed PMID: 28122537; PubMed Central PMCID: PMCPMC5267450.
- Rowe AK, Rowe SY, Holloway KA, et al. Does shortening the training on integrated management of childhood illness guidelines reduce its effectiveness? A systematic review. Health Policy Plan. 2012;27:179–193. Epub 2011/ 04/26. PubMed PMID: 21515912.
- Amaral J, Gouws E, Bryce J, et al. Effect of Integrated Management of Childhood Illness (IMCI) on health worker performance in Northeast-Brazil. Cad Saude Publica. 2004;20:S209–19. Epub 2004/12/21. PubMed PMID: 15608935.
- Nguyen DT, Leung KK, McIntyre L, et al. Does integrated management of childhood illness (IMCI) training improve the skills of health workers? A systematic review and meta-analysis. PLoS One. 2013;8:e66030. Epub 2013/ 06/19. PubMed PMID: 23776599; PubMed Central PMCID: PMCPMC3680429.
- Masanja H, Schellenberg JA, de Savigny D, et al. Impact of integrated management of childhood illness on inequalities in child health in rural Tanzania. Health Policy Plan. 2005;20:i77–i84. Epub 2005/11/25. PubMed PMID: 16306073.
- Jacobs M, Merson M. Introductory commentary: a strategic review of options for building on lessons learnt from IMCI and iCCM. BMJ. 2018;362:bmj k3013. Epub 2018/08/01. PubMed PMID: 30061381; PubMed Central PMCID: PMCPMC6081995 interests and declare no conflicts of interest.
- Dalglish SL, Vogel JJ, Begkoyian G, et al. Future directions for reducing inequity and maximising impact of child health strategies. BMJ. 2018;362:k2684. Epub 2018/08/01. PubMed PMID: 30061111; PubMed Central PMCID: PMCPMC6283368 form. We have read and understood BMJ policy on declaration of interests and declare no conflicts of interest. The authors alone are responsible for the views expressed in this article, which does not necessarily represent the views, decisions, or policies of the institutions with which the authors are affiliated.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Sci Res Method. 2007;8:19–32.
- Bryce J, Victora CG, Habicht JP, et al. Advisors M-IT. Programmatic pathways to child survival: results of a multi-country evaluation of integrated management of childhood illness. Health Policy Plan. 2005;20:i5–i17. Epub 2005/ 11/25. PubMed PMID: 16306070.
- Institute TJB. Joanna Briggs institute reviewers’ manual: 2015 edition/supplement. South Australia: The Joanna Briggs Institute; 2015.
- Finfgeld-Connett D. Use of content analysis to conduct knowledge-building and theory-generating qualitative systematic reviews. Qual Res. 2013;14:341–352.
- Pradhan NA, Rizvi N, Sami N, et al. Insight into implementation of facility-based integrated management of childhood illness strategy in a rural district of Sindh, Pakistan. Glob Health Action. 2013;6:20086. Epub 2013/07/09. PubMed PMID: 23830574; PubMed Central PMCID: PMCPMC3703511.
- Pandya H, Slemming W, Saloojee H. Health system factors affecting implementation of integrated management of childhood illness (IMCI): qualitative insights from a South African province. Health Policy Plan. 2018;33:171–182. Epub 2017/ 11/22. PubMed PMID: 29161375.
- Basaleem HO, Amin RM. Integrated management of childhood illness in Lahej, Yemen: a qualitative analysis from the perspective of health providers. East Mediterr Health J. 2011;17:101–108. Epub 2011/ 07/09.PubMed PMID: 21735943.
- Huicho L, Davila M, Campos M, et al. Scaling up integrated management of childhood illness to the national level: achievements and challenges in Peru. Health Policy Plan. 2005;20:14–24. Epub 2005/ 02/04. PubMed PMID: 15689426.
- Goga AE, Muhe LM. Global challenges with scale-up of the integrated management of childhood illness strategy: results of a multi-country survey. BMC Public Health. 2011;11:503. Epub 2011/ 06/29. PubMed PMID: 21708029; PubMed Central PMCID: PMCPMC3155839.
- Nsabagasani X, Ogwal-Okeng J, Hansen EH, et al. ‘Better medicines for children’ within the integrated management of childhood illness framework: a qualitative inquiry in Uganda. J Pharm Policy Pract. 2016;9:22. Epub 2016/ 06/10. PubMed PMID: 27280024; PubMed Central PMCID: PMCPMC4897804.
- Vhuromu EN, Davhana-Maselesele M. Experiences of primary health care nurses in implementing integrated management of childhood illnesses strategy at selected clinics of Limpopo Province. Curationis. 2009;32:60–71. Epub 2010/ 03/17. PubMed PMID: 20225745.
- Seid SS, Sendo EG. A survey on integrated management of neonatal and childhood illness implementation by nurses in four districts of West Arsi zone of Ethiopia. Pediatric Health Med Ther. 2018;9:1–7. Epub 2018/02/15. PubMed PMID: 29443325; PubMed Central PMCID: PMCPMC5804021.
- Rowe AK, Onikpo F, Lama M, et al. The rise and fall of supervision in a project designed to strengthen supervision of integrated management of childhood illness in Benin. Health Policy Plan. 2010;25:125–134. Epub 2009/ 11/20. PubMed PMID: 19923206.
- Mohan P, Kishore B, Singh S, et al. Assessment of implementation of integrated management of neonatal and childhood illness in India. J Health Popul Nutr. 2011;29:629–638. Epub 2012/ 01/31. PubMed PMID: 22283037; PubMed Central PMCID: PMCPMC3259726.
- Gerensea H, Kebede A, Baraki Z, et al. Consistency of Integrated Management of Newborn and Childhood Illness (IMNCI) in shire governmental health institution in 2017. BMC Res Notes. 2018;11 476. Epub 2018/07/18. PubMed PMID: 30012196; PubMed Central PMCID: PMCPMC6048809.
- Kruger C, Heinzel-Gutenbrunner M, Ali M. Adherence to the integrated management of childhood illness guidelines in Namibia, Kenya, Tanzania and Uganda: evidence from the national service provision assessment surveys. BMC Health Serv Res. 2017;17:822. Epub 2017/ 12/15. PubMed PMID: 29237494; PubMed Central PMCID: PMCPMC5729502.
- Senn N, Rarau P, Salib M, et al. Use of antibiotics within the IMCI guidelines in outpatient settings in Papua New Guinean children: an observational and effectiveness study. PLoS One. 2014;9:e90990. Epub 2014/ 03/15. PubMed PMID: 24626194; PubMed Central PMCID: PMCPMC3953204.
- Febir LG, Baiden FE, Agula J, et al. Implementation of the integrated management of childhood illness with parasitological diagnosis of malaria in rural Ghana: health worker perceptions. Malar J. 2015;14:174. Epub 2015/ 04/23. PubMed PMID: 25899509; PubMed Central PMCID: PMCPMC4430025.
- Titaley CR, Jusril H, Ariawan I, et al. Challenges to the implementation of the integrated management of childhood illness (IMCI) at community health centres in West Java province, Indonesia. WHO South East Asia J Public Health. 2014;3:161–170. Epub 2014/ 04/01. PubMed PMID: 28607302.
- Lange S, Mwisongo A, Maestad O. Why don’t clinicians adhere more consistently to guidelines for the Integrated Management of Childhood Illness (IMCI)? Soc Sci Med. 2014;104:56–63. Epub 2014/ 03/04. PubMed PMID: 24581062.
- Boschi-Pinto C, Labadie G, Dilip TR, et al. Global implementation survey of Integrated Management of Childhood Illness (IMCI): 20 years on. BMJ Open. 2018;8:e019079. Epub 2018/ 08/01. PubMed PMID: 30061428; PubMed Central PMCID: PMCPMC6067364.
- WHO. Towards a grand convergence for child survival and health: a strategic review of options for the future building on lessons learnt from IMNCI. Geneva (Switzerland): World Health Organization; 2016.
- Costello AM, Dalglish SL; Team obotSRS. Towards a grand convergence for child survival and health: astrategic review of options for the future building on lessons learnt from IMNCI. Geneva (Switzerland): World Health Organization; 2016.
- Kiplagat A, Musto R, Mwizamholya D, et al. Factors influencing the implementation of integrated management of childhood illness (IMCI) by healthcare workers at public health centers & dispensaries in Mwanza, Tanzania. BMC Public Health. 2014;14:277. Epub 2014/ 03/29. PubMed PMID: 24666561; PubMed Central PMCID: PMCPMC3987128.
- Arrivé E, Perez F, Pierre LM. The integrated management of childhood illness: Haiti’s example. Sante. 2004;14:137–142.
- Costello A, Peterson S, Rasanathan K, et al. Where’s the leadership? Future commitments of Unicef and WHO for global child health. BMJ. 2018;362:k3219. Epub 2018/ 08/01. PubMed PMID: 30061193; PubMed Central PMCID: PMCPMC6064977 interests and have no relevant interests to declare.
- Fick C. Twenty years of IMCI implementation in South Africa: accelerating impact for the next decade. Durban: Health System Trust; 2018.
- Robertson SK, Manson K, Fioratou E. IMCI and ETAT integration at a primary healthcare facility in Malawi: a human factors approach. BMC Health Serv Res. 2018;18:1014. Epub 2018/12/31. PubMed PMID: 30594185; PubMed Central PMCID: PMCPMC6310991.
- Shipton L, Zahidie A, Rabbani F. Motivating and demotivating factors for community health workers engaged in maternal, newborn and child health programs in low and middle-income countries: a systematic review. J Coll Physicians Surg Pak. 2017;27:157–165. Epub 2017/ 04/14. PubMed PMID: 28406775.
- Alhassan RK, Nketiah-Amponsah E. Frontline staff motivation levels and health care quality in rural and urban primary health facilities: a baseline study in the Greater Accra and Western regions of Ghana. Health Econ Rev. 2016;6:39. Epub 2016/09/02. PubMed PMID: 27580725; PubMed Central PMCID: PMCPMC5007234.
- Grant C, Nawal D, Guntur SM, et al. ‘We pledge to improve the health of our entire community’: improving health worker motivation and performance in Bihar, India through teamwork, recognition, and non-financial incentives. PLoS One. 2018;13:e0203265. Epub 2018/ 08/31. PubMed PMID: 30161213; PubMed Central PMCID: PMCPMC6117047.
- Rudasingwa M, Uwizeye MR. Physicians’ and nurses’ attitudes towards performance-based financial incentives in Burundi: a qualitative study in the province of Gitega. Glob Health Action. 2017;10:1270813. Epub 2017/ 04/30. PubMed PMID: 28452651; PubMed Central PMCID: PMCPMC5328346.
- Bhatnagar A, George AS. Motivating health workers up to a limit: partial effects of performance-based financing on working environments in Nigeria. Health Policy Plan. 2016;31:868–877. Epub 2016/ 03/08. PubMed PMID: 26946273.
- WHO. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva (Switzerland): World Health Organization; 2010.
- Rakha MA, Abdelmoneim AM, Farhoud S, et al. Does implementation of the IMCI strategy have an impact on child mortality? A retrospective analysis of routine data from Egypt. BMJ Open. 2013;3:e001852.
- Leon N, Sanders D, Van Damme W, et al. The role of ‘hidden’ community volunteers in community-based health service delivery platforms: examples from sub-Saharan Africa. Glob Health Action. 2015;12:27214.
- Theobald S, Brandes N, Gyapong M, et al. Implementation research: new imperatives and opportunities in global health. Lancet. 2018;392:2214–2228. Epub 2018/10/14. PubMed PMID: 30314860.
- Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ. 2013;347:f6753. Epub 2013/ 11/22. PubMed PMID: 24259324.
- Doherty T, Tran N, Sanders D, et al. Role of district health management teams in child health strategies. BMJ. 2018;362:k2823. Epub 2018/08/01. PubMed PMID: 30061110; PubMed Central PMCID: PMCPMC6063257 interests and have no relevant interests to declare.
- Patel S, Zambruni JP, Palazuelos D, et al. Rethinking the scale up of integrated management of childhood illness. BMJ. 2018;362:k2993. Epub 2018/08/01. PubMed PMID: 30061095; PubMed Central PMCID: PMCPMC6064974 interests and have no relevant interests to declare.
- Prost A, Sanders D, Costello A, et al. Strengthening the capabilities of families and communities to improve child health in low and middle income countries. BMJ. 2018;362:bmj k2649. Epub 2018/08/01. PubMed PMID: 30061185; PubMed Central PMCID: PMCPMC6081994 interests and have no relevant interests to declare.
- Mushi HP, Mullei K, Macha J, et al. The challenges of achieving high training coverage for IMCI: case studies from Kenya and Tanzania. Health Policy Plan. 2011;26:395–404. Epub 2010/ 11/05. PubMed PMID: 21047808; PubMed Central PMCID: PMCPMC3157918.
- Mullei K, Wafula F, Goodman C. A case study of Integrated Management of Childhood Illness (IMCI) implementation in Kenya. Nairobi (Kenya): Kenya Medical Research Institute; 2008. CREHS, Consortium for Research on Equitable Health Systems.