ABSTRACT
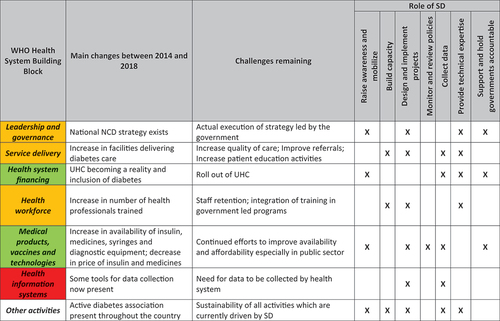
Non-governmental organizations play a vital part in the achievement of the Sustainable Development Goals as defined by the United Nations. These Goals also include targets related to noncommunicable diseases. However, non-governmental organizations have played a limited role in this area despite such diseases causing the bulk of morbidity and mortality worldwide. Through their activities, non-governmental organizations should aim to strengthen health systems, yet they often only support these for a single disease. Mali, like many other low- and middle-income countries, is facing an increasing burden of diabetes and a health system not adapted to address this challenge. Santé Diabète, a non-governmental organization based in Mali since 2003, has been working specifically on diabetes, and has developed a wide range of activities to improve the national health system. This paper describes changes in the diabetes environment in Mali between 2004 and 2018 based on two health system assessments carried out using a Rapid Assessment Protocol. Over this period, the health system was strengthened with regard to financing and access to medical products. Leadership and governance, service delivery and health workforce were all improved but still partially rely on sustained support from Santé Diabète. The key lesson from this study is that to be effective in changing the management of noncommunicable diseases in a low- and middle-income country, non-governmental organizations need to play a variety of roles, many of which may change over time.
RESPONSIBLE EDITOR
Jennifer Stewart Williams
Background
Non-governmental organizations (NGOs) play a vital part in the attainment of the United Nations. Sustainable Development Goals (SDG) to: ‘raise awareness and mobilize; build capacity; design and implement projects; monitor and review policies; collect data; provide technical expertise, and both support and hold governments accountable to their commitments.’[Citation1] In the area of noncommunicable diseases (NCDs), NGOs have played a limited role despite NCDs representing the largest burden of morbidity and mortality worldwide [Citation2,Citation3].
The World Health Organization (WHO) prioritizes five NCDs: cardiovascular diseases, diabetes, cancers, chronic respiratory diseases and mental health [Citation4]. In response to this global challenge, the WHO has developed a Global Action Plan (GAP) and established a High-Level Commission on NCDs. The GAP and High-Level Commission Reports call for a strengthening of health system responses to NCDs and emphasize the link between NCDs and Universal Health Coverage (UHC) [Citation4–6]. These documents also highlight that NGOs should be involved in this global response, without detailing the specific roles [Citation4–6]. The focus in these documents is more on NGOs as partners than as actors for change [Citation6].
The roles of NGOs in global health and strengthening health systems include: working in partnership with Ministries of Health (MoH); managing joint projects and programs; piloting innovative service delivery approaches; involving communities; developing human resources, and strengthening infrastructure and information systems [Citation7–9]. However, in some cases, this assistance has been ‘vertical’, focusing on a specific disease (e.g. HIV/AIDS), and not seen as strengthening the overall health system [Citation10].
Chee et al. [Citation11] distinguish between health system support and health system strengthening. Health system strengthening requires making comprehensive changes that durably impact the six health system building blocks proposed by WHO [Citation12]. In contrast, health system support includes activities that improve how the health system functions by providing additional inputs that have a narrow or short-term focus [Citation11].
Mali is located in West Africa with a population of about 20 million, a life expectancy at birth of 59 years and a Gross National Income per capita of US$ 840 [Citation13]. The country is ranked 184 out of 189 countries on the Human Development Index [Citation14] and faces a humanitarian crisis due to the ongoing military conflict [Citation15]. The current 10-year health system plan (2014–2023) includes objectives such as: maternal and child health; communicable diseases; NCDs; the environment; health emergencies; health system strengthening, and governance [Citation16]. The NCD component in this plan comprises activities in the areas of prevention, management, research, strengthening partnerships and coordination, and surveillance. The Malian health system is structured around Community Health Centers (Centres de Santé Communautaire, or CSCOMs), which are private not-for-profit associations managed by communities. CSCOMs are staffed by a doctor, a midwife and a nurse, who provide general medical consultations, pre- and postnatal consultations and assist with simple deliveries [Citation17]. They also play a role in linking with communities. Only 58% of the population lives less than 5 km from a facility providing these basic services [Citation17]. One of the reasons for this is the lack of health professionals and their unequal distribution within Mali [Citation18]. In addition, households in Mali face high out-of-pocket expenditures for healthcare [Citation18]. For some health issues, (e.g. HIV/AIDS, tuberculosis, caesarian deliveries, malaria testing for pregnant women and children under five, as well as surgery for fistulae) different programs provide care for free, funded by donors or the government [Citation19].
Since 2009 the government has initiated Obligatory Medical Assistance (AMO), which is a health insurance scheme financed by employee and employer contributions in both the public and private sectors [Citation20]. The AMO covers 80% of hospital and 70% of ambulatory care expenses. The government has also created the Medical Assistance Regimen (RAMED), which offers free services for the most vulnerable in Mali (about 5% of the population are considered as such) [Citation20]. A system of Voluntary Medical Insurance (AMV) for people working in the informal sector is also available through community health insurance schemes. In June 2018, the Malian government legislated a Universal Health Insurance Regimen (RAMU) which aims for UHC [Citation20].
Santé diabète: a diabetes NGO in Mali
The International Diabetes Federation estimates that about 152,000 adults in Mali (aged 20–79) live with type 2 diabetes (a 2.1% prevalence) [Citation21] and another 1,550 people with type 1 diabetes [Citation22]. Santé Diabète (SD) is a French NGO based since 2003 in Mali, working specifically on diabetes throughout the country. The NGO started its work in Mali because several founding members had carried out research work on fonio (a West African millet/cereal) and diabetes in Mali, forging a close collaboration with medical specialists in the country. From this, a variety of challenges were identified which resulted in the implementation of the first Rapid Assessment in 2004, which was aimed at documenting these problems more clearly.
SD has positioned itself as both providing technical assistance to the MoH as well as implementing activities agreed upon by the MoH and other partners. These activities include: a peer education program for type 2 diabetes; education ‘days’ for children with type 1 diabetes; diabetes training for health professionals at national hospitals; training of diabetes referral doctors at regional hospitals and referral health centers (CSREF); a one-year and four-year University training program in endocrinology, metabolic diseases and nutrition at the Faculty of Medicine and Odonto-stomatology of Mali; a working group created by the National Health Directorate and SD to improve the supply and availability of diabetes medicines in Mali, as well as to negotiate prices of medicines; ensuring availability of diagnostic equipment adapted to each level of the health system; increasing awareness of diabetes in the population through education campaigns (communities and schools) as well as in the media, and the development and roll-out of patient education material for healthcare providers. Many of these initiatives in other settings would be the responsibility of actors such as the government, academia, diabetes associations or professional medical associations. All these activities were funded by SD from different sources, including development grants from governments and private foundations, support from regional authorities in France and research funding for specific initiatives.
The aim of this study was to investigate how an NGO can strengthen health services for diabetes care in sub-Saharan Africa. We used WHO’s health system building blocks [Citation12] as a framework for analysis, linking these to the different roles NGOs can play [Citation1].
Methods
This study was based on data from two health system assessments in Mali that were carried out in 2004 and 2018. Both studies used the Rapid Assessment Protocol for Insulin Access (RAPIA) [Citation23], which has been used in different low-and middle-income countries (LMICs) to assess access to insulin and diabetes care [Citation24–27]. The protocol includes a multi-level assessment using interviews with semi-structured questionnaires, site visits, secondary analysis of existing data and document reviews (). Because the information collected is largely qualitative and semi-quantitative, no formal statistical comparison between the RAPIAs in 2004 and 2018 was performed. Any quantitative data are presented using descriptive statistics. All prices are standardized to 2018 US$ [Citation28,Citation29].
Table 1. Level and number of interviews carried out in 2018 and total interviews in 2004
The protocol was approved by the Comité d’Éthique de la Faculté de Médecine et d’Odonto-Stomatologie, Bamako, Mali and informed consent was sought and obtained from all participants. Data was collected by trained field workers. All questionnaires were in French. Translation to local languages was done when necessary, mainly for interviews with people with diabetes. Interviews were carried out with different individuals at various levels of the health system (). All interviewees were selected purposively. Interviewees responding at the macro-level were individuals from different government ministries and organizations, diabetes associations as well as clinical or academic opinion leaders. At the meso-level questionnaires targeted individuals from regional health authorities, health facilities, public and private laboratories, or public and private pharmacies. Finally, at the micro-level respondents were health professionals, traditional healers and people with diabetes. All interviews used adapted questionnaires targeted for the different interviewees covering the following themes: national policies and programs on NCDs and diabetes; policies impacting the importation, pricing and distribution of medicines and health-related supplies; organization of diabetes care; pricing and distribution of insulin, diabetes medicines and other related supplies; treatment and management of people with diabetes; barriers to care, and costs related to diabetes [Citation23].
All data (interviews, document reviews, etc.) from the RAPIA in 2018 were entered in an Excel spreadsheet and analyzed using thematic analysis across different interviews and sources of information using the six health system building blocks proposed by the WHO as a framework [Citation30]. These results were then compared with the data from the RAPIA in 2004 [Citation31]. The results were also presented linking the six health system building blocks with the different roles played by NGOs [Citation1].
Results
A total of 362 interviews were carried out in nine regions of Mali in 2018 (), compared to 150 interviews in three regions in 2004. The results are presented for each of the six WHO building blocks.
Leadership and governance
Activities implemented by SD for this health system component focused on raising awareness of diabetes as a health problem in Mali, as well as designing and implementing projects in collaboration with the MoH. In addition, SD provided technical expertise to the MoH for the development of a new strategy on NCDs running from 2019 to 2023. SD also ensured that NCDs and diabetes were included in the current health system plan (2014–2023) [Citation16]. Since 2004, this work has been facilitated by SD through a memorandum of collaboration with the MoH. In addition, an ad-hoc group bringing together different governmental and non-governmental partners was established, to ensure synergies and to create space for dialogue around different issues regarding the prevention and management of diabetes. More recently, this group was restructured as a steering committee, created by Ministerial decree, that includes patient organizations, professional medical associations, communities, other governmental organizations and SD.
In 2004, a draft NCD strategy was in the process of being developed. In 2018, the national NCD strategic plan (2015–2019) [Citation32] covered very specific activities with regard to diabetes, including: screening for diabetes, linked with health promotion and sensitization activities for the population and health professionals; provision of insulin, oral medicines and other diabetes supplies (blood glucose meters, test strips and syringes) to patients; development of surveillance tools; defining referral pathways, and strengthening partnerships between different actors.
The health system plan established in 2014 included NCDs with specific objectives relative to NCD morbidity, mortality and disability linked to NCDs [Citation16]. This strategy focused on certain key actions including improving the availability and affordability of medicines and other supplies, training of health professionals in the prevention and management of NCDs, integration of NCDs within basic training, and the creation of specialized units for NCD management at CSREF and hospitals. In 2018, SD also worked with the Malian government to ensure that gestational diabetes and care for pregnant women with diabetes was included in the National Maternal and Child Health Strategy.
In addition to these national guiding documents, each region visited in 2018 had an NCD focal point at the Regional Health Directorate. The role of these focal points was the regional implementation of the national strategy. At a national level, a diabetes-specific coordinating mechanism was created bringing together the MoH, SD, civil society, healthcare providers, Central Medical Stores and the National Agency for Telemedicine and Medical Informatics. This contrasts with 2004, when only one person was responsible for the national NCD and diabetes response.
Service delivery
To address the challenges of service delivery, capacity building was an absolute necessity given how diabetes care was provided in 2004. Through designing and implementing different projects, as well as providing technical expertise, SD was able to strengthen diabetes care as well as decentralize services. Beyond direct health system activities, SD also implemented different activities relating to the education of people with diabetes, and a study on peer-led education [Citation33]. This study and others carried out by the NGO also highlighted that the role SD played in data collection within the service delivery component had a role in increasing awareness, mobilizing local stakeholders, as well as informing further interventions.
Diabetes care in 2004 was mainly delivered in three places: two tertiary hospitals in Bamako, and a clinic run by the diabetes association. Outside of Bamako there were no referral hospitals with dedicated diabetes services, and care was dependent on the level of training of health professionals. In 2018 ‘l’Hôpital du Mali’ in Bamako has become the national referral center for diabetes with a specialized unit for children with type 1 diabetes. Today, 32 decentralized diabetes clinics are now operational throughout Mali, with each district hospital including a diabetes unit. Moreover, some CSREFs and CSCOMs in different regions and districts provided diabetes care. A problem with referrals was noted with individuals bypassing lower levels of the health system and going directly to the national referral center. Another persistent problem were the long waiting times in the facilities.
In the 2004 survey, many expressed feeling abandoned by the system and suffered from the lack of care outside the three facilities in Bamako. In 2018 most people with diabetes interviewed mentioned the need for increased therapeutic patient education as well as for other educational and informational tools. Fifty percent of facilities in 2018 had received educational support tools for people with type 2 diabetes via the work of SD and the MoH. Among interviewed health professionals, 92% stated they held education activities, however only 67% of people with diabetes stated having participated in such an activity. An evaluation of peer-led education activities in Mali found that these had a positive impact on Glycated Hemoglobin (HbA1c) [Citation33].
The 2004 RAPIA highlighted the important role played by traditional healers in the overall delivery of care in Mali, but noted there was little interaction with allopathic medicine. Traditional healers’ roles and linkage with the health system remained the same in 2018.
Health system financing
With regard to the financing of health care, SD has played a role in collecting data, providing technical expertise and advocating for the government to ensure that diabetes medicines and other aspects of care are included in the different insurance packages proposed by the Malian government.
Mali has seen dramatic changes in healthcare financing since 2004. details the elements of diabetes care that were covered in 2018 by the different insurance schemes available to the Malian population as well as their strengths and weaknesses. Consultation fees in 2018 were FCFA 600 (US$ 1.08) in CSCOMs, FCFA 1,000 (US$ 1.80) in CSREFs and Regional Hospitals and FCFA 1,500 (US$ 2.70) for a specialized consultation at a national hospital. These fees allow for a medical consultation and the associated care received, and are included in AMO, AMV and RAMED baskets. In 2004, these fees varied from FCFA 200 (US$ 0.50) to FCFA 1,000 (US$ 2.52). In contrast, in 2004 most care was provided by the diabetes association clinic and people had to pay membership fees and consultation fees to receive their care, on top of the cost of medicines.
Table 2. Strengths and weaknesses of different insurance schemes in Mali relative to diabetes
Health workforce
One of the main weaknesses found in 2004 was a lack of trained health professionals. Since then, SD has focused on building capacity through different training programs as well as designing and implementing different projects. In addition, it coordinated technical support from a variety of external partners in the area of healthcare worker training. In 2018, 32 focal diabetes doctors collectively managed more than 20,000 people in the different regions of Mali. With a total of 850 health professionals having received diabetes training this has boosted the development of human resources specialized in diabetes, as well as sustained diabetes training in continuous professional development.
Among interviewed health professionals, 93% of doctors and 82% of nurses who worked in diabetes consultations stated having received specific training in diabetes. In addition, the two University diploma training programs in endocrinology, metabolic diseases and nutrition enabled a total of 59 students from Mali to receive advanced certification courses in diabetes and endocrinology. This allowed for the development of human resources specialized in diabetes as well as strengthening diabetes training in continuous professional development. This contrasts with a lack of training in diabetes in 2004 besides training in medical school and learning-on-the-job in one of the diabetes-specific consultations.
Medical products and technologies
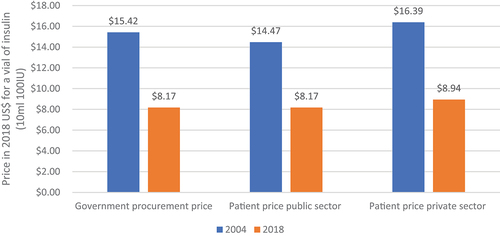
Another important change between 2004 and 2018 was the increased availability of insulin. In 2004 insulin was only available in 17% of facilities (public and private). In 2018 in contrast, 65% of facilities visited had at least one type of insulin. Prices in the public and private sectors also decreased, and became more uniform (). Data on oral medicines was not collected in 2004, but data from 2018 showed a wide range of prices within and between the sectors. For example, Glibenclamide (5 mg) varied 26-fold in price in the private sector. Between public and private sectors, the average prices for Glibenclamide and Metformin (850 mg) were 3.4 and 2.6 times more expensive in the private sector, respectively. In 2004 syringes were only available in the private sector, at an average cost of US$ 0.43. In contrast in 2018, syringes were available in 44% of public and 93% of private pharmacies. The average price had halved, to US$ 0.22 and US$ 0.24 in public and private pharmacies, respectively.
Figure 1. Government procurement and patient public and private prices for a vial (10 ml 100IU) insulin (2018 US$).
Another positive change between 2004 and 2018 was the availability of diagnostic tools, including blood glucose meters, urine ketone strips and other analytics. In 2004, HbA1c tests were available only in one private sector laboratory at a cost of US$ 25.72, in contrast to US$ 14.75 and US$ 12.68 in 2018 in the private and public sectors, respectively (2018 prices). In 2018, 60% of national hospitals, 50% of regional hospitals and 56% of CSREFs had equipment and consumables to carry out this test.
These changes in the availability and affordability of medicines and related supplies were due to awareness raising and collaboration between the MoH and SD. For insulin access, SD provided technical support as well as advocacy. For HbA1c, SD together with the MoH organized supplies, with SD purchasing the analytical equipment and initial reagents and transferring these to facilities, followed by sustained supply by the MoH.
Health information systems
In 2004, there had been a complete lack of standardized tools for data collection at facilities. Diabetes registries and individual patient records now exist thanks to SD projects, which required such data to monitor and evaluate the implementation of their projects. Ninety percent of facilities visited in 2018 had a consultation register created by the National Health Directorate and SD. A specific database for type 1 diabetes was developed. This diabetes data is not yet routinely collected centrally by the health system, but work is ongoing to integrate this into the District Health Information Software (DHIS2) in Mali.
Other areas of activity
Three other areas of improvement are worth noting. Firstly, the creation of the Malian National Federation of Diabetics (FENADIM) with its local branches in all regions (30 in total). This is yet another change from 2004 when the association was only active in the capital, with some activities in Sikasso in the south of the country. SD provided capacity building for the FENADIM with regard to management, governance, and developing the role of the association in the Malian context. Secondly, different health promotion and prevention activities have been developed and implemented by SD. These include: World Diabetes Day events with screening campaigns; awareness raising, and school-based health promotion around nutrition and physical activity. Finally, SD has shown its capacity for innovation by supporting the humanitarian response in northern Mali in 2012 [Citation34] and, since 2017, also working to integrate the services provided for diabetes with those for HIV/AIDS and tuberculosis in Mali. These other areas of activity cut across the different roles of an NGO resulting in general awareness raising, capacity building, design and implementation of projects, collection of data, and provision of technical expertise roles.
Discussion
SD is playing a significant role in raising awareness and providing support to the Malian government, with health system financing and access to medical products being areas where the NGO has enabled the health system to be strengthened. Leadership and governance, service delivery and health workforce fall in-between health system support and its strengthening. Although progress was made, these areas are still dependent on SD input, and sustained funding and technical support are not yet fully integrated into the health system. For example, the health workforce component has clearly shown improvements between 2004 and 2018 in terms of the number of personnel trained, how these professionals work within the Malian health system and how specific training courses have been put into place. However, SD in many cases organizes and funds these trainings through external support and these are not yet part and parcel of the health system. The health information systems component is an example of health system support, in that not all the data collection tools used for diabetes are currently integrated within the Malian health system.
The design and implementation of projects led by NGOs is a shared component that underpins all these activities (). The experience with SD shows that an important first step was the initial assessment of the health system using the RAPIA in 2004; this was followed by targeted activities. The other lesson, in a context like Mali, is that in order to strengthen health systems for effective management of NCDs and diabetes, NGOs have to play a variety of roles, which may evolve over time.
Figure 2. Summary of health system support or strengthening activities and role SD played in this.
This study was descriptive in nature rather than a formal evaluation, and it is impossible to quantify exactly the impact of SD’s work on the various areas of the health system. But it can be argued that SD’s work has been catalytic, and its impact can be indirectly measured by the increase in people diagnosed with type 1 diabetes. In 2004 only 14 people with type 1 diabetes were registered, in comparison to 584 in 2018 [Citation31,Citation35]. As argued previously, type 1 diabetes is a useful tracer condition for assessing health systems [Citation24,Citation36,Citation37] and this increase in number of people with type 1 diabetes within the system can be seen as a proxy for improvements in the management of diabetes in Mali, and the impact of the work of SD.
An analysis in Mozambique found similar impacts of this approach to improving diabetes care between 2003 and 2008 [Citation38] and in Rwanda health system support activities have shown improvements in the numbers of people with type 1 diabetes due to increased survival [Citation39]. What is unique with the example of SD is how, beyond its direct impact on health system strengthening that the approaches developed by SD have had, this NGO has played a role in addressing diabetes for the Malian population in an LMIC by fulfilling the roles of other actors. Society can be portrayed as a three-legged stool with one leg being the public sector that protects the health and well-being of its population; a responsible private sector that supplies the products needed, and finally civil society that provides the links between communities [Citation40]. In the Malian context, SD, which is a part of the ‘civil society’ leg, fulfils roles of both public and private sectors within the complex context of diabetes.
The limitations of this study are that, although it compares 2004 and 2018, data was not collected at the same facilities, and is descriptive in nature with no specific outcomes being assessed. Overall, the sample is purposive and is relatively small. In addition, the results present two snapshots rather than a true evolution of the situation over time. As with all mixed method approaches with interviews and observations, there are both interviewer and interviewee biases. Another source of bias in the analysis of the data is that three of the authors (SB, AS and DB) are intimately linked to the work of SD.
NGOs or civil society in diabetes and NCDs in general have to a large extent been absent or focused primarily on advocacy and awareness-raising rather than actual implementation of programs in a given country. In sub-Saharan Africa, the focus for diabetes associations has been on advocacy and provision of care if this was lacking [Citation41]. The example of SD highlights that, to address the global NCD burden, local NGOs should be empowered to be a force for change in addressing this challenge in their local contexts.
Notes contributors
SB and DB conceived this paper and AS, DS and CT were involved in different aspects of the work in Mali from 2004 to 2018. JSY was actively involved in the assessment in Mali in 2004 and JA with the assessment in 2018. SB and DB wrote the first draft of the manuscript. All authors discussed, revised, and approved the final manuscript after revisions.
Ethics and Consent
All material obtained from interviews was part of a protocol submitted and approved by the Comité d’Éthique de la Faculté de Médecine et d’Odonto-Stomatologie, Bamako, Mali and all participants provided their consent. Approval was also obtained from the Ministry of Health in Mali to carry out these assessments in 2004 and 2018.
Paper context
NGOs are part and parcel of the global health landscape and play an important role in addressing health-related issues globally and nationally through various means. We present the experience from Mali where Santé Diabète, an NGO based in Mali since 2003, has implemented a variety of projects and programs. The lessons from this experience are that to be effective in changing the management of diabetes in a context like Mali, NGOs have to play a variety of roles and these may evolve with time. This example suggests that, to address the global diabetes burden, local NGOs should be empowered to be a force for change in addressing this challenge in their local contexts.
Disclosure statement
DB is a member of the Board of SD. No conflict of interest was reported by all other authors
Additional information
Funding
References
- NGO Major Group. Non-governmental organizations (ngo) major group official position paper for the 2017 high-level political forum New York: United Nations; 2017. [cited 2021 June 17]. Available from: https://sustainabledevelopment.un.org/content/documents/15002NGO.pdf.
- Heller O, Somerville C, Suggs LS, et al. The process of prioritization of non-communicable diseases in the global health policy arena. Health Policy Plan. 2019;34:370–9. Epub 2019/06/15. PubMed PMID: 31199439; PubMed Central PMCID: PMCPMC6736081
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. Epub 2018/11/30. PubMed PMID: 30496104; PubMed Central PMCID: PMCPMC6227754.
- World Health Oragnization. It’s time to walk the talk: WHO independent high-level commission on noncommunicable diseases final report. Geneva: World Health Organization, 2019.
- World Health Organization. Time to Deliver: report of the WHO Independent High-level Commission on Noncommunicable Diseases. Geneva: World Health Organization, 2018.
- Wolrd Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013-2020 - Revised draft (Version dated 11 February 2013). Geneva: World Health Organization; 2013.
- Connelly M The Role of NGOs in Strengthening Health Systems Cambridge MA: Global Health Delivery Project at Harvard University; 2011. [cited 2021 June 17]. Available from: https://www.ghdonline.org/uploads/12_13_2011_Role_of_NGOs_in_Health_Systems_Strengthening__.pdf
- Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. 2011;11:122. Epub 2011/05/26 PubMed PMID: 21609480; PubMed Central PMCID: PMCPMC3112396.
- Landes M, Pfaff C, Zerihun M, et al. Calling non-governmental organisations to strengthen primary health care: lessons following Alma-Ata. Afr J Prim Health Care Fam Med. 2019;11:e1–e2. Epub 2019/05/01 PubMed PMID: 31038348; PubMed Central PMCID: PMCPMC6556919.
- Mussa AH, Pfeiffer J, Gloyd SS, et al. Vertical funding, non-governmental organizations, and health system strengthening: perspectives of public sector health workers in Mozambique. Hum Resour Health. 2013;11:26. Epub 2013/06/19 PubMed PMID: 23768178; PubMed Central PMCID: PMCPMC3691708
- Chee G, Pielemeier N, Lion A, et al. Why differentiating between health system support and health system strengthening is needed. Int J Health Plann Manage. 2013;28:85–94. Epub 2012/07/11. PubMed PMID: 22777839; PubMed Central PMCID: PMCPMC3617455
- World Health Organization. Health systems: improving performance. The World Health Report 2000. Geneva: World Health Organization, 2000.
- World Bank. Mali Washington DC: World Bank Group; 2020. [cited 2021 June 17]. Available from: https://data.worldbank.org/country/ML
- United Nations Development Programme. 2019. Human development index ranking new york2019. [cited 2021 June 17]. Available from: http://hdr.undp.org/en/content/2019-human-development-index-ranking
- UN News. Unprecedented humanitarian crisis in Mali revealed in new report New York: United Nations; 2019. [cited 2021 June 14]. Available from: https://news.un.org/en/story/2019/12/1053391
- Secretariat Permanent du PRODESS - Cellule de Planification et de Statistique Secteur Santé, Developpement social et promotion de la famille. Plan Decennal de Developpement Sanitaire et Social (PDDSS) 2014-2023 Bamako: ministère de la Santé et de l’Hygiène Publique, Ministère du Travail et des Affaires Sociales et Humanitaires, Ministère de la Promotion de la Femme, de l’Enfant et de la Famille, 2014.
- Cellule de Planification et de Statistique, Institut National et de Statistique, Secteur Santé, Développement Social et Promotion de la famille. Annuaire 2015: système d’information Sanitaire et Sociale. Bamako: ministère de la Santé et de l’Hygiène Publique, Ministère du Travail et des Affaires Sociales et Humanitaires, Ministère de la Promotion de la Femme, de l’Enfant et de la Famille, 2015.
- Direction des ressources humaines. Secteur Santé, Développement Social et Promotion de la Famille. Annuaire Statistique 2016 des Ressources Humaines du secteur Santé, Développement Social et Promotion de la Famille. 1ère édition. Bamako: Ministère de la Santé et de l’Hygiène Publique, Ministère de la Solidarité et de l’Action Humanitaire, Ministère de la Promotion de la Femme, de l’Enfant et de la Famille, 2017.
- Juillet A, Touré B, Ouedraogo H, et al. Évaluation du Système de Santé au Mali. Bethesda: Health Finance and Governance Project, Abt Associates Inc; 2017.
- Deville C, Hane F, Ridde V, et al. La Couverture universelle en santé au Sahel: la situation au Mali et au Sénégal en 2018, Working Paper Paris: Ceped (UMR 196 Université Paris Descartes IRD), 2018.
- International Diabetes Federation. IDF Atlas 10th Edition. Brussels: International Diabetes Federation; 2021.
- Green A, Hede SM, Patterson CC, et al. Type 1 diabetes in 2017: global estimates of incident and prevalent cases in children and adults. Diabetologia. 2021;64:2741–2750. Epub 2021/10/03 PubMed PMID: 34599655; PubMed Central PMCID: PMCPMC8563635
- Beran D, Yudkin J, de Courten M. Assessing health systems for type 1 diabetes in sub-Saharan Africa: developing a ‘rapid assessment protocol for Insulin Access’. BMC Health Serv Res. 2006;6:17.
- Beran D, Yudkin JS, de Courten M. Access to care for patients with insulin-requiring diabetes in developing countries: case studies of Mozambique and Zambia. Diabetes Care. 2005;28:2136–2140. Epub 2005/08/27. PubMed PMID: 16123479
- Beran D, Abdraimova A, Akkazieva B, et al. Diabetes in Kyrgyzstan: changes between 2002 and 2009. Int J Health Plann Manage. 2013;28:e121–37. Epub 2012/11/06. PubMed PMID: 23125073
- Beran D, Higuchi M. Delivering diabetes care in the Philippines and Vietnam: policy and practice issues. Asia Pac J Public Health. 2013;25:92–101. PubMed PMID: 21727084.
- Cardenas MK, Miranda JJ, Beran D. Delivery of Type 2 diabetes care in low- and middle-income countries: lessons from Lima, Peru. Diabet Med. 2016;33:752–760. Epub 2016/05/20. PubMed PMID: 27194174
- CPI Inflation Calculator. Value of $1 from 2004 to 2018 San Mateo CA: CPI Inflation Calculator; 2020. [cited 2021 July 12]. Available from: https://www.officialdata.org/us/inflation/2004?endYear=2018&amount=1
- Converter C. Historical Rates Sartrouville: FXTOP SARL; 2020 [ cited 2020 July 20]. Available from: https://fxtop.com/en/historical-exchange-rates.php?A=1&C1=USD&C2=XOF&YA=1&DD1=01&MM1=01&YYYY1=2004&B=1&P=&I=1&DD2=31&MM2=12&YYYY2=2004&btnOK=Go%21
- World Health Oragnization. The World Health Report Health systems: improving performance. Geneva: World Health Organization, 2000.
- International Insulin Foundation. Final Report of the International Insulin Foundation on the Rapid Assessment Protocol for Insulin Access in Mali. London: International Insulin Foundation, 2004.
- Ministère de la santé et de l’hygiène publique. Plan stratégique national de lutte contre les maladies non transmissibles 2015-2019. Bamako: République du Mali; 2014.
- Debussche X, Besancon S, Balcou-Debussche M, et al. Structured peer-led diabetes self-management and support in a low-income country: the ST2EP randomised controlled trial in Mali. PLoS One. 2018;13:e0191262. Epub 2018/01/23. PubMed PMID: 29357380; PubMed Central PMCID: PMCPMC5777645
- Besancon S, Fall IS, Dore M, et al. Diabetes in an emergency context: the Malian case study. Confl Health. 2015;9:15. PubMed PMID: 25937831; PubMed Central PMCID: PMC4416388.
- Sandy JL, Besancon S, Sidibe AT, et al. Rapid increases in observed incidence and prevalence of Type 1 diabetes in children and youth in Mali, 2007–2016. Pediatr Diabetes. 2021;22:545–551. Epub 2021/02/16. PubMed PMID: 33586301.
- Kessner D, Carolyn E, Singer J. Assessing health quality: the case for tracers. N Engl J Med. 1973;288:189–194.
- Beran D, Health systems and the management of chronic diseases: lessons from Type 1 diabetes. Diabetes Management is the name of the Journal. 2012;2:1–13. Diabetes Management
- Beran D, Silva Matos C, Yudkin JS. the diabetes uk mozambique twinning programme. Results of improvements in diabetes care in mozambique: a reassessment 6 years later using the rapid assessment protocol for insulin access. Diabet Med. 2010;27:855–861. Epub 2010/07/27. PubMed PMID: 20653740
- Marshall SL, Edidin D, Sharma V, et al. Current clinical status, glucose control, and complication rates of children and youth with type 1 diabetes in Rwanda. Pediatr Diabetes. 2013;14:217–226. Epub 2013/01/03. PubMed PMID: 23279222
- Beran D, Hirsch IB, Yudkin JS. Why are we failing to address the issue of access to insulin? a national and global perspective. Diabetes Care. 2018;41:1125–1131. Epub 2018/05/23. PubMed PMID: 29784696
- Beran D, Yudkin JS. Diabetes care in sub-Saharan Africa. Lancet. 2006;368:1689–1695. Epub 2006/11/14. PubMed PMID: 17098088
