ABSTRACT
Background
More children are surviving through interventions to address the infectious causes of under-5 mortality; subsequently, the proportion of deaths caused by birth defects is increasing. Prevention, diagnosis, treatment and care interventions for birth defects are available but are needed where the burden is highest, low-and-middle-income countries.
Objectives
A selection of birth defect focused publications, conferences, and World Health Assembly resolutions from 2000 to 2017 show that global efforts were made to raise the profile of birth defects in global public health. However, recent donor support and national government interest has waned. Without concerted global action to improve primary prevention and care for children born with birth defects, the Sustainable Development Goal targets for child survival will not be met.
Results
Birth defects make up 8% and 10% of global under-5 and neonatal deaths respectively, making them significant contributors to preventable loss of life for children. Survivors face long-term morbidity and lifelong disability which compounds the health and economic woes of individuals, families, communities and society as a whole. Demographic changes in sub-Saharan Africa portend a growing number of births with 1.6 billion projected from 2021 to 2050. More births and better survival without effective prevention and treatment for birth defects translates into more mortality and disability from birth defects.
Conclusions
We recommend interventions for prevention of birth defects. These are evidenced-based and affordable, but require low- and middle-income countries to strengthened their health systems. Action against birth defects now will prevent premature deaths and long-term disability, and lead to stronger, more resilient health systems.
Responsible Editor Stig Wall
Background
An estimated 8 million newborns are born with a birth defect each year, and of these an estimated 240,000 die worldwide in their first month of life, making birth defects a leading cause of both neonatal and postneonatal child deaths [Citation1]. In addition, some of the 1.9 million babies stillborn in 2021 will be the result of a congenital anomaly [Citation2]. Those who survive a serious birth defect often face a lifetime of severe disability and stigma.
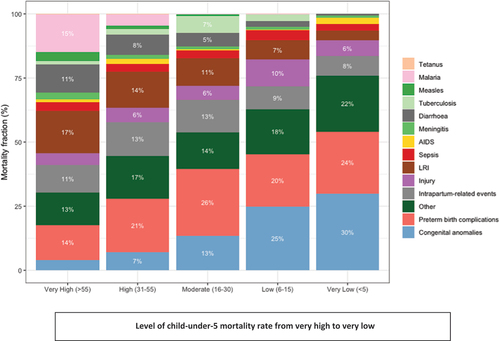
The leading causes of birth defects globally are congenital heart anomalies and neural tube defects [Citation3]. These two preventable and/or treatable conditions account for over half of all neonatal deaths due to birth defects [Citation3]. Crucially, as child survival improves through improved control of infectious childhood diseases, birth defects account for an increasing proportion of under-5 deaths, up to 30% in low-mortality settings [Citation1,Citation4] ().
Figure 1. Proportional mortality for children under-5 years according to all-cause mortality rate categories (very high, U5MR greater than 55 deaths per 1000 live births to very low, U5MR less than 5 deaths per 1000 live births). Cause specific mortality is from the child and adolescent cause of death estimation group, 2021(1). Congenital anomalies increase as a proportion of total under-5 mortality as survival improves.
The vast majority of newborns with a birth defect, including an estimated 94% of those with severe disorders, are born in low- and middle-income countries (LMICs) where diagnostic, treatment and management services are limited [Citation3]. Absence of birth defects surveillance programs in most LMICs coupled with a lack of global consensus on birth defect terminology, means that we vastly underestimate the true burden of birth defects in these countries [Citation5].
The ability to identify, treat and successfully manage birth defects is key to building bridges from survival to optimal growth and development for affected children and to eliminate discrimination, unequal educational opportunities, physical and psychological violence [Citation6]. Newborns and children with birth defects are often unable to receive the treatment and care they need due to delayed diagnoses, lack of referral systems, limited access to facilities and resources, shortage of trained healthcare providers, misinformation and misconceptions, all of which are compounded by stigma and discrimination [Citation6]. In brief, for many birth defects the tools for primary prevention and effective management are well known and tested [Citation7]: much of the current burden of birth is a failure of implementation. We argue that immediate action from the global public health community is needed to fund effective primary prevention and early detection (e.g. via expanded newborn screening), and improved early diagnostic services. These actions, coupled with effective, family-centered medical and surgical treatment and follow up that supports early childhood development will support optimal growth and development for all affected children.
Sustainable development goal child survival targets will not be met by 2030 without action against birth defects
National governments and the global public health community are investing in interventions to accelerate progress towards achieving the Sustainable Development Goals (SDGs) for child survival,Footnote1 through the Global Strategy for women’s, children’s and adolescents’ health [Citation8,Citation9], Ending Preventable Maternal Mortality [Citation10] the Every Newborn Action Plan (ENAP) [Citation11], and the Child Survival Action initiative [Citation12]. These global initiatives are important accountability mechanisms for child survival and development; yet birth defects are not specifically addressed in any of them. Surveillance, prevention and providing care for children with birth defects are important strategies to reach the SDG child survival targets and align with the SDG commitment to equity to “leave no one behind” [Citation8].
Unfortunately, despite World Health Assembly Resolutions, a global report, and multiple calls for action by professional and patient organizations (), little progress has been made in championing birth defect prevention and care. Lack of progress is especially concerning as the impact of birth defects is greatest where need for progress is largest. The highest rates of both stillbirths and child deaths occur in sub-Saharan Africa, a region that will see 339 million births and a 12% increase in the under-5 population, which will reach more than 200 million by 2030 [Citation13]. This demographic reality coupled with the fact that the majority of those born with severe disorders are in low-and-middle income countries, especially in sub-Saharan Africa, makes the need for equal access for prevention, screening and curative treatment an urgent priority for global public health.
Table 1. Highlights of global reports, conferences, professional association statements and UN resolutions. Many other national advocacy actions have been produced in the last two decades. Collectively, very little result has come from these efforts.
Effective interventions to prevent, treat and care for children with birth defects exist and their use requires investment from health systems
Evidence shows that there are affordable interventions available now to prevent many cases of birth defects. Examples include vaccination against rubella, universal salt iodization and food fortification with folic acid [Citation7]. The latter is a clear example of an population-based and relatively inexpensive intervention that can reduce the impact of birth defects by reducing the number of children born with a neural tube defect [Citation14]. At the same time, health systems – particularly those in LMICs – need to invest in the development of comprehensive policies and approaches to ensure newborns and children with birth defects have universal access to affordable, timely and appropriate medical, surgical and long-term developmental care without financial hardships [Citation15]. Health systems need to have measures in place to protect families and caregivers from the devastating impact of high out-of-pocket expenditures related to the care their child will need. As with other health services, treatment and care for children with birth defects and disabilities needs to be respectful, nurturing and based on quality-of-care principles [Citation16]. Families need to have voice in the care their children receive, and children need to be protected from violence and discrimination to survive and thrive as productive, valued members of society. We make the following recommendations to support prevention and treatment of birth defects and to support care for people living with them, cognizant that sectors other than health will also need to be strengthened:Footnote2Footnote3Footnote4Footnote5Footnote6
(1) Expand and integrate birth defects prevention into clinical and public health practice.
Introduce and scale evidence-based risk reduction interventions into national health campaigns, health and wellness programs, preconception and antenatal care [Citation17].
Renew the focus on effective primary prevention, including but not limited to population-based food fortification with folate and iodine; integration of rubella vaccination into the Expanded Programme on Immunization; improved nutrition for girls and women including micronutrient supplementation before and during pregnancy; family planning knowledge and services; management of chronic illness and infection from before conception through prenatal care; and reducing/eliminating exposure to harmful substances, drugs and environmental pollutants prior to and during pregnancy [Citation18].
(2) Improve diagnosis, management and care within health care systems.
Strengthen and expand newborn screening, early detection, and diagnosis of birth defects, followed by referral to appropriate medical and surgical treatment that is family-centered and includes early childhood development and follow-up care [Citation19].
Promote a multidisciplinary approach for specialized care such as surgery, mental health, and speech and occupational therapy, among other professional services.
Train health professionals to practice respectful and family-centered care.
Integrate prevention, identification, diagnosis and care of newborns and children with birth defects into universal health coverage and reproductive, maternal, newborn, child and adolescent health policies, guidelines, strategies, and action plans at the national, regional, and sub-regional levels.
(3) Protect the rights of individuals affected by birth defects.
Promote a rights-based and equitable approach to diagnosis and care (including respectful and family-centered care) in newborns and children, across their lifespan.
Listen to, empower, and incorporate parent and family voices into all policies, strategies and practices targeting birth defects.
Ensure timely access to screening, diagnosis, and care, including surgical care, for newborns and children with birth defects as an essential aspect of health coverage.
Eliminate violence, stigma, and discrimination against persons with birth defects.
(4) Support and expand sustainable information systems to generate key data on birth defects – their occurrence, risk factors, and outcomes – throughout the lifespan.
Develop and advocate for standard definitions for birth defects [Citation5].
Establish new estimates for the global burden of birth defects.
Strengthen registration of births and of children born with birth defects.
Expand public health surveillance systems to monitor birth defects occurrence, measure risk factors, and monitor health outcomes with follow-up that extends beyond the first year of life [Citation20].
Link surveillance to birth defects treatment and care by creating referral pathways.
(5) Dedicate funds and resources at the global and national level to support a comprehensive approach to the prevention, surveillance, screening, diagnosis and treatment of newborns and children with birth defects [Citation21].
Actions needed now and into the future
While we applaud the reductions in neonatal and child mortality globally, we know that as the overall childhood mortality rates decline, birth defects become a larger proportion of the causes of neonatal and child under-5 deaths. To further reduce neonatal and under-5 mortality, particularly in LMICs struggling to meet SDG targets for newborn and child survival, global efforts to prevent birth defects and to care for affected children need to be expanded and reinforced now.
Our recommendations align with the core principles of Universal Health Coverage (UHC) and the broader Reproductive, Maternal, Newborn, Child and Adolescent Health agenda and must be placed within UHC commitments and with renewed energy around primary health care. Prevention, surveillance, screening, diagnosis, treatment and care for newborns and children with birth defects are important strategies to achieve established SDG and ENAP targets. In the absence of a significant global response, further gains in child survival will be undermined by preventable mortality due to birth defects and we will not meet the neonatal and under-5 SDG survival targets.
Children with birth defects are subjected to multiple inequities – they have functional limitations, poorer health, and shorter life spans. We call for immediate action from the global public health community to fund effective three crucial areas for meaningful progress: a) primary prevention; b) early diagnosis, including newborn screening and early detection of birth defects; and c) appropriate medical and surgical treatment that is family-centered and includes follow-up and support for early childhood development. Actions in these three priority areas will be effective to the extent that they are included in comprehensive and sustained maternal, newborn and child health frameworks, action plans, and funding priorities – global as well as national. Through such sustained action, we can fulfill the SDG commitment to leave no one behind and ensure brighter futures for millions of children born with birth defects and disabilities.
Author contributions
JRM original draft; KLS subsequent draft and . SW, CM, LB, GLS, TD, TB, KL, AB, recommended interventions, references and edits to the manuscript. All authors contributed to the development of the original concept, and structure of the paper
Disclaimer
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Paper context
As child survival continues to improve through concerted efforts against infectious childhood diseases, the proportion of under-5 mortality due to birth defects is increasing.
We present recommendations for effective primary prevention, expanded newborn screening, early detection and diagnosis of birth defects, followed by referral to appropriate medical and surgical treatment that are needed to prevent deaths and life-long disability and continue progress toward Sustainable Development Goal child survival targets for 2030.
We argue that surveillance, prevention, treatment and providing care for children with birth defects are important strategies to reach the Sustainable Development Goal child survival targets and align with the commitment to equity of the Sustainable Development Goals, ‘to leave no one behind’.
title_page_GHA.docx
Download MS Word (17.1 KB)Acknowledgments
We thank the participants of the last International Conference on Birth Defects and Disabilities in the Developing World held in 2023 in Santiago, Chile for inspiring presentations, productive workshops and stimulating discussions. We thank Jamie Perin for provision of .
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/16549716.2024.2354002
Additional information
Funding
Notes
1 SDG 3.2.1 to reduce under-5 mortality to at least as low as 25 deaths per 1000 live births and SDG 3.2.2 to reduce neonatal mortality to at least as low as 12 deaths per 1000 live births.
2 Christianson A, Howson C, Modell B. March of Dimes: Global.Report on Birth Defects, the Hidden Toll of Dying and Disabled Children. New York: March of Dimes Birth Defects Foundation; 2006.
3 World Health Organization. Sixty-Third World Health Assembly.Resolution 63.17. Birth Defects. Geneva: World Health Organization; 2010.
4 Darmstadt GL, Howson CP, Walraven G, Armstrong RW, Blencowe HK, Christianson AL, et al. Prevention of Congenital Disorders and Care of Affected Children: A Consensus Statement. JAMA Pediatr. 2016;170(8):790–793. do i:1 0.1001/jamapediatrics.2016.0388.
5 Zarante I, Hurtado-Villa P, Walani SR, Kancherla V, López Camelo J, Giugliani R, et al. A consensus statement on birth defects surveillance, prevention, and care in Latin America and the Caribbean. Rev Panam Salud Publica. 2019;43:e2. https://doi.org/10.26633/RPSP.2019.2
6 World Health Organization. Sixty-Seventh World Health Assembly.Resolution 76.19. Accelerate efforts to prevent micronutrient deficiencies through safe and effective food fortification, a population-wide health intervention to prevent some severe birth defects of the brain and spine. Geneva: World Health Organization; 2023. https://apps.who.int/gb/ebwha/pdf_files/WHA76/A76_R19-en.pdf
References
- Villavicencio F, Perin J, Eilerts-Spinelli H, et al. Global, regional, and national causes of death in children and adolescents younger than 20 years: an open data portal with estimates for 2000–21. Lancet Glob Health. 2024;12:e16–6. doi: 10.1016/S2214-109X(23)00496-5
- United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Never forgotten: the situation of stillbirth around the globe. New York: United Nations Children’s Fund; 2023.
- Perin J, Mai C, De Costa A, et al. Systematic estimates of the global, regional and national under-5 mortality burden attributable to birth defects in 2000–2019: a summary of findings from the 2020 WHO estimates. BMJ Open. 2023;13:e067033. doi: 10.1136/bmjopen-2022-067033
- Strong KL, Pedersen J, White Johansson E, et al. Patterns and trends in causes of child and adolescent mortality 2000–2016: setting the scene for child health redesign. BMJ Global Health. 2021;6:e004760. doi: 10.1136/bmjgh-2020-004760
- Malherbe H, Modell B, Blencowe H, et al. A review of key terminology and definitions used for birth defects globally. J Comm Genet. 2023;14:241–262. doi: 10.1007/s12687-023-00642-2
- United Nations Children’s Fund. Seen, counted, included: using data to shed light on the well-being of children with disabilities. New York: United Nations Children’s Fund; 2021. Available from: https://data.unicef.org/resources/children-with-disabilities-report-2021
- Institute of Medicine (US). Committee on improving birth outcomes. Reducing birth defects: meeting the challenge in the developing world. In: Bale J, Stoll B, Lucas A, editors. Interventions to reduce the impact of birth defects. Washington (DC): National Academies Press (US); 2003 3. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222083/
- United Nations. The global strategy for women’s, children’s and adolescents’ health (2016–2030): survive, thrive, transform. Geneva: United Nations; 2018.
- United Nations. Every woman, every child. Saving lives, protecting futures: progress report on the global strategy for women’s and children’s health. New York: United Nations; 2015.
- World Health Organization. Ending preventable maternal mortality (EPMM): a renewed focus for improving maternal and newborn health and well-being. Geneva: World health Organization; 2021.
- World Health Organization. Newborn health: draft action plan. Every newborn: an action plan to end preventable deaths. Report by the secretariat. World health assembly executive board report A67/21. Geneva: World Health Organization; 2014 May 2. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_21-en.pdf
- Child Health Task Force. Child survival action: a renewed call to action to end preventable child deaths. Washington (DC): Child Health Task Force; 2023. Available from: https://www.childhealthtaskforce.org/resources/action-plan/2022/child-survival-action-initiative-narrative-vision-document
- United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Levels & trends in child mortality: report 2023, estimates developed by the United Nations inter-agency group for child mortality estimation. New York: United Nations Children’s Fund; 2024.
- Rodrigues VB, Silva END, Santos MLP, et al. Cost-effectiveness of mandatory folic acid fortification of flours in prevention of neural tube defects: a systematic review. PLOS ONE. 2021;16:e0258488. doi: 10.1371/journal.pone.0258488
- Botto LD, Mastroiacovo P. Triple surveillance: a proposal for an integrated strategy to support and accelerate birth defect prevention. Ann N Y Acad Sci. 2018;1414:126–136. doi: 10.1111/nyas.13600
- Zarante I, Hurtado-Villa P, Walani SR, et al. A consensus statement on birth defects surveillance, prevention, and care in Latin America and the Caribbean. Rev Panam Salud Publica. 2019;43:e2. doi: 10.26633/RPSP.2019.2
- World Health Organization. Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity. Meeting report. Geneva: World Health Organization; 2012 [cited 2012 Feb 6–7]. Available from: https://www.who.int/publications/i/item/9789241505000
- Kancherla V, Botto LD, Rowe LA, et al. Preventing birth defects, saving lives, and promoting health equity: an urgent call to action for universal mandatory food fortification with folic acid. Lancet Glob Health. 2022 Jul;10:e1053–e1057. doi: 10.1016/S2214-109X(22)00213-3
- Boyle CA, Cordero JF. Birth defects and disability: a public health issue for the 21st century. Am J Public Health. 2005 Nov;95:1884–1886. doi: 10.2105/AJPH.2005.067181
- Botto LD, Mastroiacovo P. From cause to care: triple surveillance for better outcomes in birth defects and rare diseases. Eur J Med Genet. 2018 Sep;61:551–555. doi: 10.1016/j.ejmg.2018.06.007
- Darmstadt GL, Howson CP, Walraven G, et al. Prevention of congenital disorders and care of affected children: a consensus statement. JAMA Pediatr. 2016;170:790–793. doi: 10.1001/jamapediatrics.2016.0388
