Drug delivery in the airways by inhalation can be used for local and/or systemic action, depending on the ability of the aerosolized drug to cross the air–blood barrier. For proteins, this is partly conditioned by the drug’s molecular weight, as well as aerosol characteristics. This editorial focuses on protein inhalation for topical delivery purposes. Even though systemic applications (such as insulin inhalation) are not considered herein, it is worth noting that systemic diffusion following topical delivery may happen in some cases, and provide therapeutic benefit (as is the case for granulocyte-macrophage colony-stimulating factor (GM-CSF)).
1. Advances in inhaled protein therapeutics for topical delivery
Respiratory diseases constitute a major public health issue worldwide: four of them are among the ten most common causes of death (pneumonia, tuberculosis, lung cancer, and chronic obstructive pulmonary disease (COPD)). They also represent a major socioeconomic burden through disability, health-care costs, and loss of productivity.
In view of their advantageous pharmacological features, protein therapeutics (including antibodies) have ushered in a new era in respiratory medicine; they provide significant clinical benefit and are becoming increasingly important tools in the therapeutic armamentarium [Citation1]. Given the limited diffusion of protein therapeutics from the bloodstream to the lungs (partly due to their high molecular weight), pulmonary delivery of aerosolized proteins seems an obvious choice – provided that the therapeutic target operates in the lungs, of course [Citation2]. Approval of the first inhaled protein (the enzyme dornase alfa, marketed as Pulmozyme®, F. Hoffmann-La Roche, Basel, Switzerland) in 1993 reshaped the management of patients with cystic fibrosis; when combined with standard medications, the protein significantly improved lung function. After two decades, a number of promising new inhaled protein therapeutics with topical lung delivery are finally reaching the clinic – especially since 2010 (). To the best of our knowledge, 18 inhaled protein therapeutics have entered clinical trials and are being tested in either major respiratory diseases (asthma and pneumonia) or in rare/orphan lung diseases (e.g. cystic fibrosis, pulmonary alveolar proteinosis, and alpha-1 antitrypsin deficiency). It is noteworthy that two fatal respiratory diseases are missing from the list: lung cancer and COPD. First, lung cancer is often detected late (i.e. with large, metastatic tumors), and inhaled protein therapeutics may not enter either the tumor tissue or the systemic circulation. However, in situ lung carcinoma with lepidic growth may be a relevant target for inhalation therapy [Citation3]. Second, the mechanisms leading to COPD remained unclear, which may explain the lack of drug targets for protein therapeutics. Today, several protein therapeutics aim at countering infection-triggered acute exacerbations of COPD, as exemplified with the recent announcement of a Phase II trial of inhaled interferon beta to boost antiviral defenses in patients with COPD. Likewise, other proteins might help treating manifestations of COPD such as emphysema or bronchitis, which are correlated with disease progression and a decline in lung function.
Table 1. Inhaled protein therapeutics in clinical development for topical lung applications.
2. Strategies for designing inhaled protein therapeutics
Although proteins can be formulated as dry powders for aerosolization, 75% of the inhaled protein therapeutics in clinical development have been developed as liquids for nebulization (). Accordingly, this editorial will mainly comment on advances in protein nebulization for topical lung delivery. Protein nebulization is often the first step in the development process because it offers several advantages over dry powders: it avoids drying steps, it is suitable for all clinical situations, and it enables greater pulmonary deposition than dry powder inhalers. Nebulizers have been significantly improved in recent years, and can deliver a 70% lung dose versus a maximum of 30% with current dry powder inhalers or the 50% expected with next-generation devices [Citation4,Citation5]. Indeed, dornase alfa is administered daily (2.5 mg per session) by nebulization. Nevertheless, nebulization exposes proteins to stressful conditions by generating a huge air–liquid interface (ALI) and, in some cases, high temperatures and/or shear forces. These conditions may cause protein unfolding, aggregation, oxidation, deamidation, or glycation, which may lead to changes in biological activity and safety concerns. In this prospect, nebulizers and formulations constitute two relevant tools to optimize protein stability during nebulization.
Many marketed or investigational technologies have given encouraging preclinical or clinical results when used to aerosolize protein therapeutics (). Comparative studies of nebulizers (reviewed by Hertel et al.) allow to identify a number of trends [Citation6,Citation7]. As with other new inhaled therapeutics, vibrating-mesh nebulizers are now frequently used for therapeutic protein delivery in humans (86% of the cases in which the nebulizer technology is disclosed) [Citation8].Vibrating-mesh nebulizers allow the delivery of high drug amounts (often required for protein therapeutics) and are less harsh with regard to chemical and physical constraints [Citation6]. For example, the ALX-0171 Nanobody™ aerosols displayed satisfactory aerodynamic properties and biologic potency when produced by vibrating-mesh nebulization, with no protein aggregation [Citation9].
Table 2. Desirable characteristics for protein inhalers, and trends in nebulization devices.
Formulation is also an important parameter in protein nebulization; it not only modulates the aerosol’s aerodynamic profiles but also offers a unique opportunity to stabilize the protein. Since the mechanisms underlying protein degradation during nebulization are not always well understood, formulation design often relies on an empirical screening of excipients already known to stabilize proteins and/or improve aerosols. To prevent aggregation (occurring mainly at the ALI), surfactants (e.g. polysorbates) have been successfully included in formulations of monoclonal antibodies and aviscumine [Citation7,Citation10]. Polyethylene glycols have also been used to stabilize proteins by generating steric repulsion between monomers [Citation7]. Likewise, protein therapeutics can be stabilized by other excipients (buffers, sugars, polyols, and amino acids, ). However, due to intellectual property concerns, formulation details are rarely disclosed for inhaled proteins in clinical development (i.e. for only six proteins in ). This clearly limits the extrapolation of general principles to the nebulization of protein therapeutics.
Formulation may also make it possible to enhance a protein’s pharmacological properties. For instance, modified-release formulations (such as microparticles, nanoparticles, or liposomes) might customize pharmacokinetic profiles while avoiding rapid protein degradation [Citation11]. Nevertheless, few FDA-approved excipients for inhalation (i.e. endogenous lung compounds or inactive formulation ingredients) are currently available. Thus, progress in formulation advances may require the safety of new excipients to be assessed.
3. Expert opinion
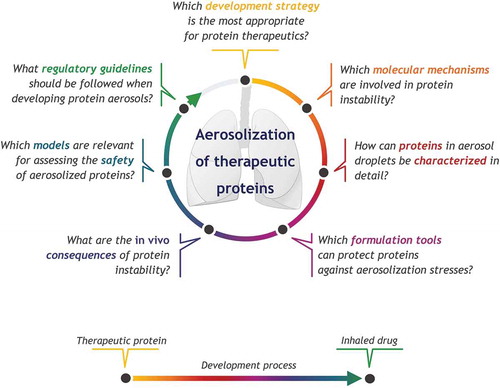
Nebulization is now a leading approach for administering proteins to the airways, as evidenced by the number of ongoing clinical trials in this field. Today’s success stories highlight the advantages and potential of nebulization for topical lung delivery – as long as the inhalation system ensures protein stability and effective drug deposition within the respiratory tract. However, a number of molecule- and/or administration-route-related challenges remain ().
Figure 1. The development of nebulized protein formulations: several key questions have yet to be addressed
At present, there are several relevant device and formulation options for effective, safe protein aerosolization. The significant interplay between these two parameters has prompted the development of unique drug–device combinations tailored to the protein of interest (in which the device and the formulation are engineered in tandem). Four of the inhaled proteins in clinical trials are delivered with a customized nebulizer (). However, redesigning the device and the formulation might not be feasible or relevant for every new protein. If rapid development is required or if the protein is only moderately sensitive to aerosolization stresses, it may be more straightforward and affordable to adjust the formulation to a marketed device.
One of the particularities of the inhaled route relates to the mechanisms of protein degradation, which are still partially elucidated. Although all proteins will be exposed to a large ALI (the magnitude of which depends on the droplet size), the level of applied stress probably differs from one device to another. For example, aerosolization with two different mesh nebulizers generated distinct aggregate populations with the same protein [Citation10]. Hence, aerosol development approaches might need to be reconsidered for each new protein. Gaining insight into the physical/chemical mechanisms contributing to protein degradation will be crucial for protecting the active compound and making formulation design more rational and time-efficient.
It still remains not clear how to assess protein stability. Although aggregation and biological activity are common read-outs, other protein alterations (e.g. oxidation or deamidation) are less frequently studied – despite their obvious links to protein activity and immunogenicity [Citation12]. In the literature, a range of analytical techniques are employed to assess protein stability and aggregation, with various levels of performance. This complicates inter-study comparisons and the ability to highlight key parameters in protein stability. In addition, most of today’s analytical methods are not applicable to aerosol droplets. Thus, droplets must be pooled into a bulk liquid before analysis, which might modify protein stability and thus induce pre-analytical bias. Hence, there is a need for in-depth, relevant assessments of the physicochemical and biological aspects of protein stability following aerosolization.
Given the specific characteristics of the inhalation route, dedicated studies of aerosol-specific stresses, subsequent protein modifications, and their impacts on efficacy, pharmacokinetics and safety are required. For example, immunogenicity appears to vary markedly among the four proteins studied to date, and is difficult to predict (). As evidenced by several in vivo studies, the protein aggregates formed in response to various stresses may raise immunogenicity, and prompt the production of potentially neutralizing anti-drug antibodies. This issue has not yet been well addressed for aerosolization stress and airway delivery.
The use of animal models to analyze the efficacy, pharmacokinetics, and safety of inhaled drugs has been informative but remains cumbersome and ethically problematic. It is difficult to extrapolate animal data on inhaled protein therapeutics to humans because of physiological, anatomical, biological, and respiratory differences between species; the use of dissimilar aerosol devices induces distinct stresses on protein therapeutics and unequal drug deposition within the respiratory tract [Citation13]. The recent implementation of promising in vitro models (such as multilayer cell-based models in an aerosol chamber) may simplify inhaled drug development by integrating advanced functional studies in the early formulation steps [Citation14]. Aerosol delivery in complex organ-mimicking systems (such as ‘lungs-on-a-chip’) might also generate other options [Citation15].
In conclusion, the development of proteins for nebulization is eminently possible, in view of the current state of scientific knowledge and recent successes in this field. However, addressing unresolved questions about protein stability () is critical to standardize the development processes, facilitate the elaboration of dedicated regulatory guidelines, and accelerate progression toward clinical applications. The advent of highly engineered antibody-based therapeutics (e.g. antibody–drug conjugates) and other classes of inhaled biotherapeutics (such as vaccines and bacteriophages), with increasing levels of complexity and protein-like characteristics, supports further the requirement of strategies to overcome these concerns. Besides, the growing development of full-length antibodies (with high molecular weights) might bring significant technical challenges for inhalation devices regarding the delivery of higher therapeutic doses (i.e. hundreds of milligrams), with satisfactory lung deposition profiles. Some of these points are also applicable to dry protein aerosols, which are expected to increase over the coming years and decades (as already observed for anti-infectives).
Declaration of interest
N Heuzé-Vourc’h is a business associate in a CRO dedicated to respiratory medicine (Cynbiose Respiratory). L Vecellio is an employee of Nemera, a medical device company. English writing assistance, provided by David Fraser, Biotech Communication, was utilized in the production of this manuscript. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer Declaration of interest
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Sécher T, Guilleminault L, Reckamp K, et al. Therapeutic antibodies: a new era in the treatment of respiratory diseases? Pharmacol Ther. 2018 published online 2018 May 4. DOI:10.1016/j.pharmthera.2018.05.003.
- Dall’Acqua WF, Kiener PA, Wu H. Properties of human IgG1s engineered for enhanced binding to the neonatal Fc receptor (FcRn). J Biol Chem. 2006;281:23514–23524.
- Guilleminault L, Azzopardi N, Arnoult C, et al. Fate of inhaled monoclonal antibodies after the deposition of aerosolized particles in the respiratory system. J Control Release. 2014;196:344–354.
- de Boer AH, Hagedoorn P, Hoppentocht M, et al. Dry powder inhalation: past, present and future. Expert Opin Drug Deliv. 2017;14:499–512.
- Carvalho TC, McConville JT. The function and performance of aqueous aerosol devices for inhalation therapy. J Pharm Pharmacol. 2016;68:556–578.
- Respaud R, Vecellio L, Diot P, et al. Nebulization as a delivery method for mAbs in respiratory diseases. Expert Opin Drug Deliv. 2015;12:1027–1039.
- Hertel SP, Winter G, Friess W. Protein stability in pulmonary drug delivery via nebulization. Adv Drug Deliv Rev. 2015;93:79–94.
- Pritchard JN, Hatley RH, Denyer J, et al. Mesh nebulizers have become the first choice for new nebulized pharmaceutical drug developments. Ther Deliv. 2018;9:121–136.
- Van Heeke G, Allosery K, De Brabandere V, et al. Nanobodies as inhaled biotherapeutics for lung diseases. Pharmacol Ther. 2017;169:47–56.
- Loira-Pastoriza C, Todoroff J, Vanbever R. Delivery strategies for sustained drug release in the lungs. Adv Drug Deliv Rev. 2014;75:81–91.
- Respaud R, Marchand D, Parent C, et al. Effect of formulation on the stability and aerosol performance of a nebulized antibody. MAbs. 2014;6:1347–1355.
- Filipe V, Jiskoot W, Basmeleh AH, et al. Immunogenicity of different stressed IgG monoclonal antibody formulations in immune tolerant transgenic mice. MAbs. 2012;4:740–752.
- Guillon A, Sécher T, Dailey LA, et al. Insights on animal models to investigate inhalation therapy: relevance for biotherapeutics. Int J Pharm. 2018;536:116–126.
- Röhm M, Carle S, Maigler F, et al. A comprehensive screening platform for aerosolizable protein formulations for intranasal and pulmonary drug delivery. Int J Pharm. 2017;532(1):537–546.
- Doryab A, Amoabediny G, Salehi-Najafabadi A. Advances in pulmonary therapy and drug development: lung tissue engineering to lung-on-a-chip. Biotechnol Adv. 2015;34:588–596.
