1. The StentrodeTm
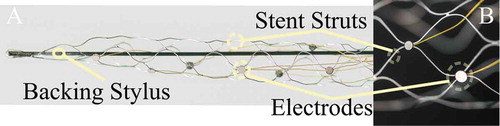
The StentrodeTM is a miniaturized neural interface that can record and stimulate the brain from within a blood vessel [Citation1,Citation2]. The StentrodeTM derives its name from the amalgamation of its component parts – stent plus electrode – where the stent is used as a scaffold to support the electrodes (). This device has been delivered through the jugular vein and placed adjacent to the brain in the superior sagittal sinus (SSS) without the need for brain surgery. The idea of recording and stimulating the brain from within a blood vessel has existed since 1973 [Citation3]. Improvement over previous attempts for endovascular recording and stimulation came from mounting electrodes on a self-expanding stent allowing it to be anchored in place over long periods of time [Citation3]. Neurovascular stents, such as those of the StentrodeTM, have been used in treating stroke and intracranial hypertension, and have been applied successfully in the clinic for many years with a growing record of safety [Citation4]. The possibility of accessing the brain without brain surgery is appealing and represents a promising outlook for the future of brain-machine interfaces (BMIs) and neuromodulation.
2. StentrodeTm-based BMI
Research using the StentrodeTM has reported signal bandwidths (usable signal range) of up to 250 Hz, signal-to-noise ratios above 2 for a single trial, and spatial resolution of 3 mm [Citation5]. StentrodeTM recorded signals were, therefore, comparable to those from subdural or epidural electrodes and were within the ranges considered useful for a BMI [Citation5,Citation6]. Preliminary results on the safety of the device have also shown that the SSS remains open over 6 months, which is also promising.
Another benefit of the StentrodeTM is the potential ability to record from within the sulci, interhemispheric regions, and deep brain sites, particularly in regions such as visual area V1, where it is often difficult to place electrodes without highly invasive surgery or stereotactic insertion of electrodes. For access to V1, the StentrodeTM will be placed in the SSS or transverse sinus. The medial walls of V1 are adjacent to the interhemispheric fissure and accommodate the SSS and the transverse sinus, which extends medio-laterally from the confluence of the sinus to the sigmoidal sinus. A StentrodeTM placed in the SSS can access the medial wall of the V1 lining the interhemispheric fissure; a StentrodeTM placed in the transverse sinus can access the inferior wall of V1.This alternative StentrodeTM BMI approach could use previously difficult to reach brain regions, which may provide considerably greater benefit than can be expected with a motor cortical BMI approach alone.
To date, the most impressive demonstrations of BMIs came from penetrating intracortical recordings from the BrainGate consortium, where some users could type up to 30 characters per minute by using thought to move a cursor on a screen to type letters [Citation7]. While this is impressive, the technology faces several challenges in translation to clinical application. The StentrodeTM approach has so far shown reliable two-class classification in sheep [Citation8] but continuous trajectory decoding is yet to be demonstrated. However, from a user’s point of view, functional control in a take-home BMI is appealing even if the speed of control is reduced. Only one BMI is presently in use at home by a person with paralysis, who uses a single command to select an object on a screen [Citation9]. Even this single class classification system provides improvement to her everyday life. At the very least, the StentrodeTM is expected to be capable of separating movement intent or imagination versus rest. The first-in-human clinical trial (ClinicalTrials.gov Identifier: NCT03834857) using the StentrodeTM is scheduled for 2019. This trial is an Early Feasibility Study in participants with paralysis resulting from spinal cord injury, motor neuron disease, stroke, muscular dystrophy, or amputation.
3. StentrodeTm-based neuromodulation
The StentrodeTM was also used to stimulate the motor cortex to generate gross movements [Citation2]. Neuromodulation or stimulation of the brain has offered life-changing treatments for people with neurological conditions such as Parkinson’s disease and epilepsy, usually by deep-brain stimulation. Using the venous approach, the StentrodeTM can reach prefrontal brain regions, motor and somatosensory regions, and parietal regions adjacent to the interhemispheric fissure [Citation1,Citation10]. Although more challenging, an intravascular device like the StentrodeTM may potentially reach the thalamus, fornix, nucleus accumbens, subgenual cingulate white matter, and ventral capsule [Citation11]. However, the device will need to be made substantially smaller to access these regions with smaller blood vessels. At present, the StentrodeTM has not been able to show reliable stimulation since approximately 60% of experiments were successful in generating a motor response when stimulating in the region of the motor cortex of sheep [Citation2]. An important first step to showing neuromodulation of the brain would be to generate consistent cortical responses. Initial evidence is positive and future work should be able to ascertain the limits of endovascular stimulation and its effect on the vasculature.
4. Beyond healthcare
With the dawn of the start-up culture, we have seen a great interest from technology entrepreneurs toward experimenting with medical technologies. The last decade has seen tremendous growth in the non-medical use of implants [Citation12] from bio-hackers in their backyards to large companies such as Google [Citation13]. The thought that a BMI may become an integral part of everyday life and directly communicate with our smartphones and computers is exciting. For example, Google aims to put ‘the web in your head by 2020’ [Citation13]; Facebook aims to ‘build a mind-reading machine’ [Citation14] and promises to type 100 words per minute by thinking. Investors in Silicon Valley have invested $billions already in healthcare start-ups focusing on BMI [Citation15].
While on the one hand, it is promising that more people are interested in this area than ever before, on the other hand, there may be a certain degree of naivety in thinking that invasive technologies will become commonplace in society within 1–2 years. While BMI use in everyday life with implanted electrodes may eventuate, it must first solve several critical challenges. This includes improving our understanding of neural circuits, miniaturization of electronics, and improving the safety of implantation. If we can develop a way to create a device that can be positioned within the brain without causing adverse events, then translation of medical technology into the consumer space may be possible. This is where the StentrodeTM may have an advantage, provided that the safety of the device can be shown. But before we can even think about neurotechnology for the consumer, our priority is to help people with paralysis who need it the most by making the technology safe and effective.
5. The challenges
Both safety and efficacy are equally important and need to be considered together when developing implantable technologies. Early indications of the safety and efficacy of the StentrodeTM are promising, with few adverse events reported in animal trials [Citation16] and some early successes in signal-to-noise, signal bandwidth, and spatial resolution results. However, as a relatively new method for accessing long-term recordings and stimulation, there is much that we do not yet understand.
Efficacy results are limited due to what can be achieved with ovine or porcine models, which are typically used in preclinical evaluation of the endovascular approaches. Higher-order animal models, such as primates, may provide greater insight in developing BMI algorithms based on statistical analyses of brain recordings. However, ethical and societal concerns can impede the transition of new technologies into primate models.
Safety issues of the StentrodeTM that must be considered are vascular injury, infection, stenosis, and thrombosis [Citation17]. The long-term stability of the StentrodeTM, like other neurovascular stents, will depend on its incorporation into the walls of blood vessels and ability to limit the neointimal proliferation into the stent, which can lead to stenosis and occlusion of the blood vessels. However, initial results are promising and the neuroradiology clinical community has been quick to welcome this minimally invasive method [Citation18]. Neuroradiologists routinely use permanent stents in patients’ brains to keep blood vessels open. Endovascular therapy is the standard of care [Citation18] in several clinical procedures including the treatment of thrombectomy, idiopathic intracranial hypertension, vascular malformation, and aneurysms. The safety record of cerebrovascular stenting has been improving and they can now reach remote locations of the brain more safely than surgical methods [Citation4].
6. Miniaturization
One major drawback of the present generation StentrodeTM is the need for wires that connect the recording sensors to the electronics. Wires pass along the length of the blood vessels from the recording electrodes to the chest where the electronics are placed. The transvascular exit of these wires from the jugular vein is a concern that needs to be addressed. It may render the implantation site unusable for medical monitoring, it may prevent intravenous injections, and the blood vessel may possibly rupture causing internal bleeding. Therefore, it would be ideal to miniaturize the electronics and integrate them into the StentrodeTM such that there is no need for wires. However, scaling down the electronics and power supply is not trivial and will require years of research and development to make them small enough to fit through a deployment catheter while also fitting into a cylindrical (or irregular) blood vessel.
7. Final remarks
In conclusion, the endovascular approach and the StentrodeTM are exciting developments. They open a new field of study in endovascular electrophysiology. The StentrodeTM provides potentially safe access to regions of the brain that we had not previously considered accessing. This opens new opportunities for diagnosis and treatment of various conditions including epilepsy, Parkinson’s disease, paralysis, and other neurological conditions. Further work is needed to establish safety, miniaturize the device, and demonstrate efficacy. For now, it is exciting to imagine the possibilities for the next generation of medical devices with the StentrodeTM.
Declaration of interest
SE John is supported by The University of Melbourne(Australia), with grants from, The Department of Health and Human Services, Victorian Government(Australia), National Health and Medical Research Council (Australia), Department of Defense (USA). SE John was previously employed at Synchron Corp. who is the holder of the Stentrode trademark. T Yanagisawa is supported by the Department of Neurosurgery at Osaka University. DB Grayden is supported by The University of Melbourne (Australia). He has grants from, The Department of Health and Human Services, Victorian Government (Australia), National Health and Medical Research Council (Australia), Department of Defense (USA), Defense Advanced Research Projects Agency (USA). DB Grayden is on the Scientific Advisory Committee of Synchron Corp. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer Disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Oxley TJ, Opie NL, John SE, et al. Minimally invasive endovascular stent-electrode array for high-fidelity, chronic recordings of cortical neural activity. Nat Biotechnol. 2016;34:320–327. doi: 10.1038/nbt.3428.
- Opie NL, John SE, Rind GS, et al. Focal stimulation of the sheep motor cortex with a chronically implanted minimally invasive electrode array mounted on an endovascular stent. Nat Biomed Eng. 2018;2:907–914. Available from: http://www.nature.com/articles/s41551-018-0321-z
- Sefcik RK, Opie NL, John SE, et al. The evolution of endovascular electroencephalography: historical perspective and future applications. Neurosurg Focus. 2016;40:1–8.
- Aguilar-Pérez M, Martinez-Moreno R, Kurre W, et al. Endovascular treatment of idiopathic intracranial hypertension: retrospective analysis of immediate and long-patients. Neuroradiology. 2017;59(3):277–287. doi:10.1007/s00234-017-1783-5
- John SE, Opie NL, Wong YT, et al. Signal quality of simultaneously recorded endovascular, subdural and epidural signals are comparable. Sci Rep. 2018;8:8427. Available from: http://www.nature.com/articles/s41598-018-26457-7
- Forsyth IA, Dunston M, Lombardi G, et al. Evaluation of a minimally invasive endovascular neural interface for decoding motor activity. In proceedings of conference on IEEE/EMBS Conf Neural Eng NER. 2019 Mar;750–753.
- Pandarinath C, Nuyujukian P, Blabe CH, et al. High performance communication by people with paralysis using an intracortical brain-computer interface. Elife. 2017;6:1–27. Available from: http://elifesciences.org/lookup/doi/10.7554/eLife.18554
- Forsyth IAIA, Dunston M, Lombardi G, et al. Evaluation of a minimally invasive endovascular neural interface for decoding motor activity. 9th Int IEEE/EMBS Conf Neural Eng. San Francisco, CA: IEEE; 2019. p. 750–753.
- Vansteensel MJ, Pels EGM, Branco MP, et al. Fully implanted brain signal recording device for communication in severe paralysis reveals feasibility of chronic home use of neuronal activity. Eur Neuropsychopharmacol. 2017;27:S556. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0924977X17310672
- Oxley TJ, Opie NL, Rind GS, et al. An ovine model of cerebral catheter venography for implantation of an endovascular neural interface. J Neurosurg. 2018;128:1020–1027.
- Teplitzky BA, Connolly AT, Bajwa JA, et al. Computational modeling of an endovascular approach to deep brain stimulation. J Neural Eng. 2014;11:026011. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24608363
- Darvishi S, Gharabaghi A, Ridding MC, et al. Reaction time predicts brain-computer interface aptitude. IEEE J Transl Eng Heal Med. 2018;6:1–11.
- Trenholm R Google boss predicts google implant will put the web in your head by 2020 [Internet]. cnet. 2010 [cited 2019 May 14]. Available from: https://www.cnet.com/news/google-boss-predicts-google-implant-will-put-the-web-in-your-head-by-2020/
- Cohen N Zuckerberg wants facebook to build a mind-reading machine [Internet]. Wired. 2019 [cited 2019 May 14]. Available from: https://www.wired.com/story/zuckerberg-wants-facebook-to-build-mind-reading-machine/
- The AI industry series: top healthcare AI trends to watch. CB Insights, New York, NY; 2018. [Internet], [cited 2019 June 1]. Available from: https://www.cbinsights.com/research/report/ai-trends-healthcare/
- Opie NL, Rind GS, John SE, et al. Feasibility of a chronic, minimally invasive endovascular neural interface. In 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp. 4455-4458. IEEE, 2016.
- Fisher RS. Intravascular stimulation of the motor cortex. Nat Biomed Eng. 2018;2:883–884. Available from: http://www.nature.com/articles/s41551-018-0330-y
- Rajah G, Saber H, Singh R, et al. Endovascular delivery of leads and stentrodes and their applications to deep brain stimulation and neuromodulation: a review. Neurosurg Focus. [Internet]. 2018;45:E19. Available from: http://browzine.com/articles/218994852