ABSTRACT
Common mental health disorders are studied extensively among adult women globally. However, they remain under-researched among young women. This study aims to determine whether gender disadvantage factors are associated with psychological distress among young women in rural India, where the child sex ratio is lower than the national average. A cross-sectional survey was conducted in rural Pune, India. A total of 229 young married women who had a live birth in the last 12 months were screened for psychological distress. The predictors of psychological distress were estimated using multivariable logistic regression analyses. Psychological distress was found among 50 respondents (21.9%). Young women who were married before 18 years had 2.19 times higher odds of distress than women who were married after 18 years. Young women who gave birth to a female infant had 2.43 times higher odds of distress than those who gave birth to a male infant. Lack of partner support and experience of postnatal health complications were other predictors. Study findings ascertain the role of gender disadvantage factors in causing psychological distress. From a public health perspective, early identification and treatment of psychological distress, is imperative, along with addressing gender inequitable practices.
Introduction
Depressive disorders, anxiety, and behavioural problems among young people are one of the most significant contributors to the burden of disease globally, with a high prevalence among married girls and women in low and middle-income countries (LMICs) (Patel, Citation2013). Girls are almost two times more likely than boys to be diagnosed with common mental health disorders (CMHDs) (WHO, Citation2017). There is a well-established body of evidence on risk factors, including gender-based factors of postnatal psychological distress among adult women from low and middle-income countries (LMICs) (Upadhyay et al., Citation2017). However, there is a limited understanding of gender drivers of mental health among young married women. The gender disadvantage factors that can elevate the risk of psychological distress among women in South Asia include giving birth to a female child, intimate partner violence, lack of partner support and child marriage (Patel et al., Citation2004; Shidhaye et al., Citation2017; Upadhyay et al., Citation2017).
Studies from India and South Asia found son preference was a huge stressor for married women, which negatively affected their postnatal functioning (Clarke et al., Citation2014; Patel et al., Citation2002, Citation2004; Upadhyay et al., Citation2017). Further, there is evidence that lack of partner support during the postnatal period disrupts the mother's mental health. These studies have reported positive benefits of male involvement that have led to reduced chances of maternal depression. Young women married during adolescence are particularly vulnerable to psychological distress (Kapungu et al., Citation2018). Child marriage has been associated with a limited number of studies with increased common mental health problems in South Asia and Africa, according to recent research from LMICs (Beattie et al., Citation2019; John et al., Citation2019). The systematic research shows that girls married early are particularly at greater risk of experiencing intimate partner violence, pregnancy-related complications and limited social network and support (Gelaye et al., Citation2016; Kapungu et al., Citation2018; Raj, Citation2010). These are also the established risk factors for depression and anxiety among women during the postnatal period (2).
In India, as per a recent survey, more than 30% of girls were married below 18 years in rural India (International Institute for Population Sciences [IIPS], Citation2017). The latest data (Census of India, Citation2011) shows that the child sex ratio (0–6 years of age) has decreased in India from 927 to 911 which indicates son preference. In India, an increasing number of studies are establishing the prevalence of common mental health disorders among married adolescent girls (Beattie et al., Citation2019). Girls aged 15–19 years, among all adolescents, showed the highest rate of depression (7.5%) in two states of India (Uttar Pradesh and Bihar). For married girls, the main reasons for feeling depressed centred around the stress related to child bearing, child marriage, domestic violence, and infant death (Population Council, Citation2017).
Despite the increased emphasis on gender correlates of CMHDs among young girls, little research exists on how gender factors influence young women's postnatal psychological distress (15–24 years) in India. Given this background, the current study seeks to address these gaps. The specific objectives of the paper are: (a) To understand the prevalence of psychological distress among young married women (aged 15–24 years) in rural India who had a live birth in the last 12 months (b) To assess the association of gender disadvantage factors (giving birth to a female child, child marriage, and lack of partner support) with psychological distress, a proxy for CMHD among young women (aged 15–24 years) in rural India.
Methods
Study design and site
The current study includes analysis of cross-sectional baseline data collected as a part of a large maternal mental health intervention for young pregnant and lactating womenFootnote1 in the Pune district of Maharashtra state in 2017. It was designed to increase utilisation of maternal and mental health care facilities, using a combination of psycho-social counselling, behaviour change therapies, and access to the public health system. The survey was conducted in the state of Maharashtra, (Pune district) where child sex ratioFootnote2 is lower (883 girls per 1000 boys) than the national average (919 girls per 1000 boys) and state average (894 girls per 1000 boys) (Census of India, Citation2011). Also, the rate of child marriageFootnote3 and early pregnancy was higher than the national and state average (IIPS, Citation2017). This paper is based on the analyses of data on young married women living in marital homes, aged 15–24 years (Total = 229), who gave birth to singleton babies in the last 12 months who were alive at the time of interview. There is no consistent definition of the postnatal period in psychiatric literature, so we adopted a working definition- the first 12 months after delivery, which is in line with previous studies (Miller, Citation2002; Rojas et al., Citation2007). Therefore, we included the data for all the women who were in a postnatal period of 12 months or less.
Recruitment
The multi-stage sampling design was implemented in randomly selecting first a block, and then 12 villages were selected from the block using probability proportional to size. Systematic random sampling was used to select the respondents from the completed household list of 12 selected villages. A listing exercise was conducted with a village health functionary's help in each selected village to identify all the married women in the age group of 15–24 years, who had a live birth in the previous 12 months. Women were eligible for recruitment if they were married, 15–24 years of age with a child (0–12 months old), speaking one of the study languages (English, Hindi or Marathi); and not experiencing cognitive or physical impairment, which would make responding to the interview and giving informed consent difficult.
All data were collected by trained female investigators who were provided with rigorous training on General Health Questionnaire-12 (GHQ-12) in English and a local language (Marathi) by a team of psychologists. The investigators used the Marathi translated version of the GHQ-12, and Psychologists accompanied the female investigators during the interview.
Ethics approval and consent to participate
All study participants provided consent and/or assent to participate in the study. Verbal informed consent of young women was sought prior to the survey. Respondents aged below 18 years provided assent, while verbal informed consent was sought from their parents. The questionnaires did not request the name or other identifying variables, to ensure anonymity of data for research purpose only. Since adolescent girls aged 15–19 years are the most vulnerable populations in research, the study minimised all possible risks to the participants during the survey. Every effort was made to ensure protection and confidentiality and to reduce any potential adverse consequence to the participants. We referred women who experienced psychological distress to primary care services and to the tertiary hospital in study sites. The study from which our data are drawn was granted ethical approval from the Institutional Ethics Review Committee of the MAMTA Health Institute for Mother and Child.
Measurements
Outcome variable
Psychological distress
Psychological distress was measured through the validated GHQ-12 item questionnaire. GHQ-12 is one of the most widely used and validated screening questionnaires for measuring psychological distress in primary care and community settings. The 12-item versions of the GHQ-12 have been field-tested and validated as a screening measure for current common mental disorders in India. The Cronbach's alpha showed a good internal consistency of the GHQ-12 bimodal scale (α = 0.78). Each item was scored ‘1’ or ‘0’, thus a possible total score of 12 for each woman.
In this study, we have used the cut-off point as ‘4 and above’ to discriminate between the presence or absence of a probable current psychological distress. Respondents with a GHQ-12 score of less than 4 were considered ‘not being psychologically stressed’ (indicate low GHQ-12), and respondents with GHQ-12 scores of 4 and above were considered ‘psychologically distressed’ (indicate high GHQ-12). The optimal threshold for screening was 4 or more on the GHQ-12 and this was used in a few studies conducted in the community settings. This optimum score had a sensitivity of 43.7% and specificity of 88.1% with a positive predictive value of 86.29%. Studies in a few states of India have recommended lowered cut-off points for community use as it would be beneficial to reach all possible cases and reduce the number of false negatives. The use of the cut-off point of 4 and above for common mental disorders has been applied in community settings because it performs better in terms of sensitivity and specificity for community-based studies (Endsley et al., Citation2017; Kim et al., Citation2013)
Predictors
Socio-demographic factors included mother's age, economic status, type of family, caste, religion, woman's education, and husband's education. Gender-based and cultural factors included age at marriage, having a son, and partner's support during the postnatal period. Reproductive health factors included parity, sex of infant, institutional delivery, breastfeeding, and postnatal complications.
Socio-demographic factors
Mother's age was segregated into 18 years or above, and below 18 years. Economic status was assessed with the possession of a Below Poverty Line Footnote4(BPL) card which entitles one's household to subsidised food grain. Those women whose household possessed a BPL card were considered to be Below Poverty Line (BPL), and those who did not have a card were considered to be Above Poverty Line (APL). Women were considered to be living in a joint family if they lived with their husbands, children, parents, and a nuclear family if they lived with husbands and children only. Caste was categorised as Scheduled TribesFootnote5 (STs), Other Backward ClassFootnote6(OBCs) and Scheduled CastesFootnote7 (SCs) and general. Religion was categorised as Hindu and Muslim. Education levels were defined as primary or less (no education or below primary), primary (1–5 years), secondary (6–10 years), senior secondary and higher (11 years and above) education as standards.
Gender-based and cultural factors
Age at marriage was coded on the basis of the participant's age at the time of first marriage and was divided as 18 or above and below 18 years. Women were also categorised into those who had a son and those who did not have a son. Partner support was defined as women who perceived receiving support provided from their husbands during the postnatal period.
Reproductive health factors
Parity was segregated into first-time parents and multiparous. Sex of infant was categorised as male and female. Women who delivered at a health facility were considered to have an institutional delivery. Women were also categorised into those who were still breastfeeding (at the time of interview) and those who were not breastfeeding. Women who faced any health issues (high fever for more than 24 h, severe lower abdominal pain, foul-smelling vaginal discharge, excessive bleeding, convulsions, and/or severe headache) during the first six weeks after delivery were considered having had serious postnatal complications. Definitions of all these symptom categories were derived from recent guidelines for reproductive health research.
Statistical analysis
Odds ratios and 95% confidence intervals were calculated to estimate the association between predictors and psychological distress. We assessed the odds of distress according to the presence or absence of each predictor First, univariate analysis was conducted to generate unadjusted ORs with 95% confidence intervals to assess the association of each factor with psychological distress (GHQ 12 ≥ 4). The odds ratios were calculated with GHQ-12 score (low GHQ with score < 4 and high GHQ with score ≥ 4) as the dependent variable and the other factors as the independent variables. We entered all the independent variables that showed an association at p < 0.05 with the high GHQ score ≥ 4 in univariable analyses into a multivariable logistic regression model. The statistical significance level for the multivariable logistic regression model was set at p < 0.05 and p < 0.10. All statistical analyses were performed using IBM SPSS for Windows 22.0 (IBM, Chicago, IL, USA).
Results
Participant characteristics
describes the key characteristics of the participants. The mean age of the sample was 21.9 (SD 1.86). Almost all participants were Hindu (96.9%). Regarding economic status, almost half of them belonged to families that lived below the poverty line (BPL). Fifty-five percent belonged to the general caste category, one third (32.8%) belonged to the Scheduled Caste/Scheduled Tribe (SC/ST) and 12.2% belonging to the Other Backward Class (OBC). More than one third had received higher secondary education or above (34.4%), and the same pattern was observed among their husbands who received higher secondary education or above (37.1%). More than one fifth of young women were married below 18 years of age (22%) and lived with their partners. More than half of the women (52.7%) were multiparous. The majority of the women had delivered in an institution (93%). Majority of the women (93.4%) were still breastfeeding. More than one-third of them reported postnatal complications (36.2%). Half of the women (52.4%) had received a partner's support post-delivery. The overall prevalence of postnatal psychological distress (GHQ-12 score ≥ 4) among young women was 21.9%.
Table 1. Characteristics of young women included in the study.
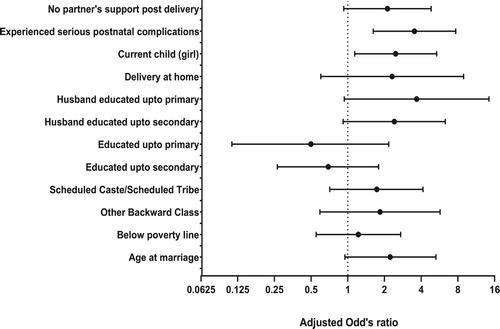
. shows the univariable and multivariable results assessing the association of socio-demographic, gender-based, reproductive health, and postnatal factors with the GHQ-12 score. In the univariable analysis, we found an association of having received primary education and below, living below the poverty line, belonging to the nuclear family, schedule caste/tribe and other backward class, and having husbands who had completed secondary education and below with postnatal psychological distress in young women. Among the gender-based factors, being married before 18 years, giving birth to a female infant, receiving no partner support during the postnatal period were significantly associated with psychological distress. Also, experiencing postnatal complications were significantly associated with distress.
Table 2. Univariable and Multivariable Logistic Regression of significant predictors of Psychological distress among young women.
The multivariable logistic regression showed that women whose husbands had no education or until primary levels were at higher odds of facing postnatal psychological distress (AOR = 3.61, CI: 0.92–14.17) than those with higher secondary or above education (reference category). The association between women's education and psychological distress was significant in the crude but not in the adjusted model. Similarly, crude regression analysis indicated that women from BPL families and those belonging to the Scheduled Caste/Scheduled Tribe or Other Backward Class were significantly associated with distress. However, this association was lost after adjusting other covariates in the adjusted model.
As for gender correlates, giving birth to a female infant, child marriage, and lack of partner support were significant predictors for psychological distress after controlling all the major confounding factors in the adjusted logistic regression analysis ( and ). Young women who gave birth to a female infant were at higher odds of postnatal psychological distress than those who gave birth to a male infant (AOR = 2.43; 95% CI: 1.12–5.27). Young women who were married before the age of 18 years were 2.19 times at higher odds (AOR = 2.19; 95% CI: 0.93–5.20) to suffer from psychological distress than those who were married after the 18 years. Partner support was also a significant predictor of psychological distress under the multivariable model. The odds of psychological distress were 2.08 times higher among young women who had no partner support during postnatal care than those who had partner support (AOR = 2.08; 95% CI: 0.91–4.75). Further, postnatal psychological distress was also significantly associated with more than threefold-increased odds of postnatal health compilations (AOR = 3.46; 95% CI: 1.59–7.56) when compared with the women who had no serious postnatal health complications.
Discussion
To our knowledge this is the first study focussing on postnatal psychological distress among young married women aged 15–24 years in rural India. The rates of postnatal psychological distress in our study population were found to be 21.9%. This is in line with earlier studies from low and middle-income countries, including India, where maternal psychological distress was reported to be 20%–30% in community-based cohorts (Patel et al., Citation2008). Our findings show that giving birth to a female infant has a strong, negative association with the mental health of a young woman. This finding is consistent with previous studies in south Asia that show women undergo psychological distress after giving birth to a female child due to biased gender norms around son preference (Fisher et al., Citation2012; Kapungu et al., Citation2018; Prost et al., Citation2012; Shidhaye & Patel, Citation2010; Upadhyay et al., Citation2017). Further, we found that child marriage was associated with an increased risk of psychological distress. Child marriage has been associated with a limited number of studies with increased odds of depression, self-harm, and suicidal thoughts (Gage, Citation2013; Loaiza & Wong, Citation2012). The latest study from India found a strong association of child marriage with high psychological distress levels among married girls in rural Karnataka (Beattie et al., Citation2019). In a study from Ethiopia, girls had 3-fold greater odds of mental distress if they were married below 18 years (John et al., Citation2019). In a study on young mothers in Nepal, being married at the age of 16–17 years was significantly associated with psychological distress in the crude regression analysis (Clarke et al., Citation2014). Previous research on child marriage in South Asia also highlighted that girls married as children are at increased risk of depression, especially due to exposure to gender-based violence (Kapungu et al., Citation2018). Moreover, qualitative studies explain that child marriage brings with it multiple stressors, including the burden of marital responsibilities, childbearing, and child-rearing during adolescence, which leads to significant emotional distress (John et al., Citation2019).
Our study also showed that young women who had no partner support were at a higher risk of psychological distress. This concurred with the findings from a recent systematic review in India (Upadhyay et al., Citation2017) and from low and middle-income countries, which found that that the risk of CMHD was higher among women who had no partner support (Fisher et al., Citation2012; Gelaye et al., Citation2016). These study findings show that women whose partners provided support and encouragement had better mental and emotional health.
Young women who undergo postnatal complications are at a much higher risk of developing distress than their counterparts without such complications. Studies have reported links between poor reproductive health and perinatal common mental health disorders in other low and middle-income settings, including India (3). However, this is reported less in the case of young women. Our findings are also consistent with findings from research in South Asian and developing countries (Clarke et al., Citation2014) where common mental disorders were strongly associated with gynaecological complaints, however more in the context of adult women in rural India (Patel & Oomman, Citation1999; Prasad et al., Citation2003; Prost et al., Citation2012). Women who are married at a young age may be more vulnerable because child marriage is associated with early motherhood and an increased risk of perinatal health problems (Kapungu et al., Citation2018). There was no significant difference between distressed and non-distressed mothers with respect to age and number of existing children in our study.
The study has important implications for programmes and policies. This study provides compelling evidence of the important association between gender disadvantage factors in a sample of young postnatal women. Programmes and policies targeting post-natal women can maximise their impact by combining psychological well-being and partner support. In particular, the study recommends detection, (screening) and management of psychological distress during post-partum. Further, it also recommends promoting partner support and addressing gender discriminatory norms against daughter aversion in maternal health programmes in India.
The study also has a few limitations, which are important to mention. The sample taken for the analysis was small (n = 229) and from the larger data on young women. Thus, the findings may not hold true across other geographic and socioeconomic contexts, and hence there can be limited generalisations. Secondly, the cross-sectional nature of the study means that we can only report associations between predictors of psychological distress and cannot make claims of causality. This study did not collect information on previous diagnoses of psychological distress among participants, which would aid in differentiating a history of distress before or during pregnancy. Further systematic research will be required to extend and validate this analysis by including a larger representative sample size across different contexts to develop a greater understanding of the role of gender-based factors in creating psychological distress among young women in rural India.
Conclusion
Overall, young mothers are exposed to a greater number of life stressors very early in life, including child marriage, giving birth to a female child, lack of partner support, and health complications. These stressors are underlying reasons for postnatal psychological distress. The practice of child marriage can have adverse effects on adolescent girls and young women's mental health in the postnatal period. Infants are dependent on their mothers for breastfeeding, physical care, comfort, and social interaction. The absence of partner support could influence postnatal complications, further affecting young mothers’ postnatal functioning. Our study adds significantly to the small body of literature on the association between gender-based factors, especially giving birth to a female infant, and child marriage and psychological distress among young women in the postnatal stage, in rural India. This research makes a strong case to focus on women's psychological well-being, incorporating an integrated approach to address gender inequitable norms and practices and psychological distress into postnatal public health interventions and policies. Identification of pregnant women experiencing psychological distress through community health care providers presents an opportunity to assess the nature of distress and work towards decreasing psychological distress for maternal well-being. Further, counselling to husband and family to promote gender equity and partner support must be incorporated into routine postnatal care.
Acknowledgements
First and foremost, the authors thank all the study participants for giving their time and sharing their experiences with us. The authors would like to thank Dr. Mohan Ghule for providing specific inputs on the study. The authors would also like to thank Ms. Madhuri Thorat Nalavade for coordinating the research study in the field and the research team for collecting the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes
1 Adolescence is defined by the World Health Organization as between 10 and 19 years, while youth refers to 15–24 years. Young people refer to the 10–24-year-old age group. For this paper's purpose, we have used the term young women throughout to refer to women of 15–24 years in study population.
2 In India, the child sex ratio is defined as the number of females per thousand males in the age group 0–6 years in a human population.
3 Child marriage in India is defined as a marriage of a girl below the age of 18 years and marriage of a boy before 21 years, respectively.
4 BPL (Below Poverty Line) is an economic benchmark and poverty threshold used by the Government of India to indicate the economic disadvantage and to identify individual and household in need of government aid.
5 ST is an official category. The tribal population, except some of the nomadic and denotified groups, is known as ‘scheduled tribes’ by Constitution of India.
6 OBC is an acronym for Other Backward Classes. It is an official category under the Indian constitution that defines/classifies classes that are educationally and socially backward.
7 SC is an official category that defines the former ‘untouchable caste’. They are entitled to affirmative action under the Indian constitution, which aims to get them to a level playing field as they have suffered historical injustice.
References
- Beattie, T. S., Prakash, R., Mazzuca, A., Kelly, L., Javalkar, P., Raghavendra, T., Isac, S., & Watts, C. (2019). Prevalence and correlates of psychological distress among 13–14 year old adolescent girls in North Karnataka, South India: A cross-sectional study. BMC Public Health, 19(1), 48. https://doi.org/10.1186/s12889-018-6355-z.
- Census of India. (2011). Provisional population Totals. Office of the Registrar General and Census Commissioner.
- Clarke, K., Saville, N., Shrestha, B., Costello, A., King, M., Manandhar, D., & Prost, A. (2014). Predictors of psychological distress among postnatal mothers in rural Nepal: A cross-sectional community-based study. Journal of Affective Disorders, 156, 76–86. https://doi.org/10.1016/j.jad.2013.11.018
- Endsley, P., Weobong, B., & Nadkarni, A. (2017). The psychometric properties of GHQ for detecting common mental disorder among community dwelling men in Goa, India. Asian Journal of Psychiatry, 28, 106–110. https://doi.org/10.1016/j.ajp.2017.03.023
- Fisher, J., Mello, M. C. D., Patel, V., Rahman, A., Tran, T., Holton, S., & Holmes, W. (2012). Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bulletin of the World Health Organization, 90(2), 139–149H. https://doi.org/10.2471/BLT.11.091850
- Gage, A. J. (2013). Association of child marriage with suicidal thoughts and attempts among adolescent girls in Ethiopia. Journal of Adolescent Health, 52(5), 654–656. https://doi.org/10.1016/j.jadohealth.2012.12.007
- Gelaye, B., Rondon, M. B., Araya, R., & Williams, M. A. (2016). Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. The Lancet Psychiatry, 3(10), 973–982. https://doi.org/10.1016/S2215-0366(16)30284-X
- International Institute for Population Sciences (IIPS). (2017). National Family Health Survey (NFHS-4), 2015–16.
- John, N. A., Edmeades, J., & Murithi, L. (2019). Child marriage and psychological well-being in Niger and Ethiopia. BMC Public Health, 19(1), 1029. doi: 10.1186/s12889-019-7314-z
- Kapungu, C., Petroni, S., Allen, N. B., Brumana, L., Collins, P. Y., De Silva, M., & Pringle, B. (2018). Gendered influences on adolescent mental health in low-income and middle-income countries: Recommendations from an expert convening. The Lancet. Child & Adolescent Health, 2(2), 85–86. https://doi.org/10.1016/S2352-4642(17)30152-9
- Kim, Y. J., Cho, M. J., Park, S., Hong, J. P., Sohn, J. H., Bae, J. N., & Park, J. I. (2013). The 12-item general health questionnaire as an effective mental health screening tool for general Korean adult population. Psychiatry Investigation, 10(4), 352–358. https://doi.org/10.4306/pi.2013.10.4.352.
- Loaiza, E., & Wong, S. (2012). Marrying too young: End child marriage. United Nations Population Fund (UNFPA).
- Miller, L. J. (2002). Postpartum depression. The Journal of the American Medical Association, 287(6), 762–765. https://doi.org/10.1001/jama.287.6.762
- Patel, V. (2013). Reducing the burden of depression in youth: What are the implications of neuroscience and genetics on policies and programs? Journal of Adolescent Health, 52(2), S36–S38. https://doi.org/10.1016/j.jadohealth.2012.04.016
- Patel, V., Araya, R., Chowdhary, N., King, M., Kirkwood, B., Nayak, S., Simon, G., & Weiss, H. A. (2008). Detecting common mental disorders in primary care in India: A comparison of five screening questionnaires. Psychological Medicine, 38(2), 221–228. https://doi.org/10.1017/S0033291707002334
- Patel, V., & Oomman, N. (1999). Mental health matters too: Gynaecological symptoms and depression in South Asia. Reproductive Health Matters, 7(14), 30–38. https://doi.org/10.1016/S0968-8080(99)90004-6
- Patel, V., Rahman, A., Jacob, K. S., & Hughes, M. (2004). Effect of maternal mental health on infant growth in low income countries: New evidence from South Asia. BMJ, 328(7443), 820–823. https://doi.org/10.1136/bmj.328.7443.820
- Patel, V., Rodrigues, M., & DeSouza, N. (2002). Gender, poverty, and postnatal depression: A study of mothers in Goa, India. American Journal of Psychiatry, 159(1), 43–47. https://doi.org/10.1176/appi.ajp.159.1.43
- Population Council. (2017). Understanding the lives of adolescents and young adults (UDAYA) in Bihar, India.
- Prasad, J., Abraham, S., Akila, B., Joseph, A., & Jacob, K. S. (2003). Symptoms related to the reproductive tract and mental health among women in rural southern India. The National Medical Journal of India, 16(6), 303–308.
- Prost, A., Lakshminarayana, R., Nair, N., Tripathy, P., Copas, A., Mahapatra, R., Rath, S., Gope, R. K., Rath, S., Bajpai, A., Patel, V., & Costello, A. (2012). Predictors of maternal psychological distress in rural India: A cross-sectional community-based study. Journal of Affective Disorders, 138(3), 277–286. https://doi.org/10.1016/j.jad.2012.01.029
- Raj, A. (2010). When the mother is a child: The impact of child marriage on the health and human rights of girls. Archives of Disease in Childhood, 95, 931–935. https://doi.org/10.1136/adc.2009.178707
- Rojas, G., Fritsch, R., Solis, J., Jadresic, E., Castillo, C., González, M., Guajardo, V., Lewis, G., Peters, T. J., & Araya, R. (2007). Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: A randomised controlled trial. The Lancet, 370(9599), 1629–1637. https://doi.org/10.1016/S0140-6736(07)61685-7
- Shidhaye, R., & Patel, V. (2010). Association of socio-economic, gender and health factors with common mental disorders in women: A population-based study of 5703 married rural women in India. International Journal of Epidemiology, 39(6), 1510–1521. https://doi.org/10.1093/ije/dyq179
- Shidhaye, P., Shidhaye, R., & Phalke, V. (2017). Association of gender disadvantage factors and gender preference with antenatal depression in women: A cross-sectional study from rural Maharashtra. Social Psychiatry and Psychiatric Epidemiology, 52(6), 737–748. https://doi.org/10.1007/s00127-017-1380-2
- Upadhyay, R. P., Chowdhury, R., Salehi, A., Sarkar, K., Singh, S. K., Sinha, B., Pawar, A., Rajalakshmi, A. K., & Kumar, A. (2017). Postpartum depression in India: A systematic review and meta-analysis. Bulletin of the World Health Organization, 95(10), 706–717C. https://doi.org/10.2471/BLT.17.192237
- World Health Organization. (2017). Summary report on the WHO/UNAIDS/UNFPA/UNICEF joint regional meeting on the global accelerated action for the health of adolescents: Guidance to support country implementation, Cairo, Egypt. (Report No. WHO EM/CAH/202/E).