ABSTRACT
Researchers and practitioners recognise the importance of context when implementing healthcare interventions, but the influence of wider environment is rarely mapped. This paper identifies the country and policy-related factors potentially explaining the country differences in outcomes of an intervention focused on improving detection and management of heavy alcohol use in primary care in Colombia, Mexico and Peru. Qualitative data obtained through interviews, logbooks and document analysis are used to explain quantitative data on number of alcohol screenings and screening providers in each of the countries. Existing alcohol screening standards in Mexico, and policy prioritisation of primary care and consideration of alcohol as a public health issue in Colombia and Mexico positively contributed to the outcome, while the COVID-19 pandemic had a negative impact. In Peru, the context was unsupportive due to a combination of: political instability amongst regional health authorities; lack of focus on strengthening primary care due to the expansion of community mental health centres; alcohol considered as an addiction rather than a public health issue; and the impact of COVID-19 on healthcare. We found that wider environment-related factors interacted with the intervention implemented and can help explain country differences in outcomes.
Introduction
Providing alcohol screening and brief intervention in primary care (PC) can reduce individual alcohol consumption (Ghosh et al., Citation2022; Kaner et al., Citation2018; O’Donnell et al., Citation2014), and has the potential to improve population health outcomes if implemented at scale (Manthey et al., Citation2021), however the intervention often lacks uptake in practice. SCALA (Scale-up of Prevention and Management of Alcohol Use Disorders in Latin America) was a Horizon 2020 funded implementation study aiming to scale up the intervention and increase PC providers’ delivery of screening for risky alcohol use and comorbid depression (Jane-Llopis et al., Citation2020) in Colombia, Mexico and Peru. The setting was chosen because of the observed and further projected increases in alcohol consumption in the middle-income countries, including in the Latin American region (Manthey et al., Citation2019), in combination with increased prioritisation of PC in the selected countries (Atun et al., Citation2015). Furthermore, previously implemented and evaluated interventions in Latin America have to large degree focused on young people, with majority of the studies on general population focused on Brazil (Ronzani et al., Citation2019). The SCALA study tested whether training providers (detailed description in Kokole et al., Citation2022), and providing community support (a range of adoption mechanisms and support systems, Solovei et al., Citation2021) increased rates of alcohol and depression screening amongst patients in PC practice. Training was found to be the key implementation strategy to increase rates of both alcohol and depression activities before the implementation was majorly disrupted by the COVID-19 pandemic (Anderson et al., Citation2021).
The current paper, as part of process evaluation (Kokole et al., Citation2023), aims to examine the country and policy context of Colombia, Mexico and Peru and consider its impact on the outcomes of the SCALA study. Understanding the context and its influence and interaction with the intervention has for a while been recognised as important in explaining the intervention’s implementation and outcomes (Moore et al., Citation2014; Pfadenhauer et al., Citation2017), but there is inconsistency in the term’s interpretation and application – definitions ranging from wider physical, social and political environment (Steckler & Linnan, Citation2002); to any external factor that might influence the intervention’s implementation (Moore et al., Citation2014). For this paper, we focus on the ‘wider environment’ aspect of context – exogeneous influences on implementation in health care organisations (Nilsen & Bernhardsson, Citation2019). The wider environment factors are rarely explicitly evaluated in healthcare implementation studies (Daivadanam et al., Citation2019; Liu et al., Citation2019; Rogers et al., Citation2020), despite existing evaluations showing the importance of their consideration, also in low- and middle-income countries (Faregh et al., Citation2019; Shannon et al., Citation2021). Studies evaluating implementation of alcohol screening and brief interventions have scarcely been focusing on wider environment beyond citing factors such as time constraints, patients’ beliefs about alcohol, or lack of financial incentives (Rosário et al., Citation2021). The SCALA study was conducted simultaneously in Colombia, Mexico, and Peru, providing us with an opportunity to compare the country and policy contexts of the three countries and their impact on the implementation of alcohol screening.
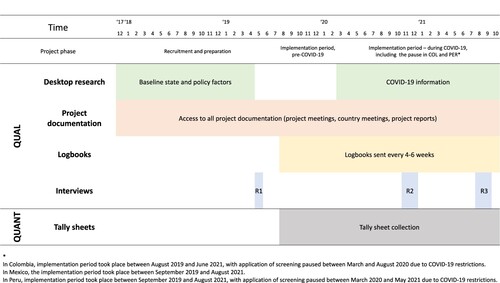
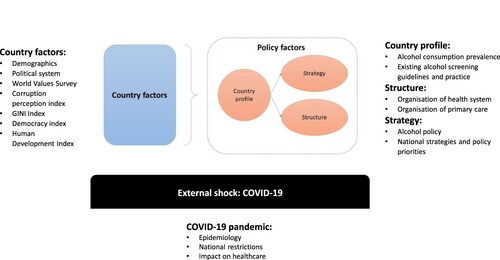
As the main analysis framework, the model proposed by Ysa et al. (Citation2014), was taken as a starting point and adapted for the purposes of this study. This model was selected from a range of possible frameworks considering the factors of the wider environment (e.g. Damschroder et al., Citation2009; Fleuren et al., Citation2004; Flottorp et al., Citation2013; Pfadenhauer et al., Citation2017), as it focused on our factors of interest (including structure of healthcare system as a whole rather than only on organisational level), and provided broad scaffolding, while enabling sufficient flexibility for inductive analysis of factors within the given categories. The model (summarised in and further described in Appendix 1) builds on two levels of analysis: (1) country factors, which are the general characteristics of the studied countries (demographics, political structure, values etc.), not directly related to the implementation of alcohol screening as the studied intervention and (2) policy factors (more proximal to the studied intervention): policy profile of the country (e.g. existing alcohol consumption and guidelines), strategies (e.g. alcohol-related strategies and policy priorities) and structures which the intervention is embedded (healthcare system and PC). Later, external shocks category (unexpected external events impacting the intervention), as framed in Craig et al. (Citation2018) was also added to the model, due to the onset of the COVID-19 pandemic during the implementation period.
Figure 1. Framework for the contextual analyses, adapted from Ysa et al. (Citation2014).
In summary, the current paper aims to describe the initial country and policy context of the countries in which the SCALA study took place (Colombia, Mexico and Peru), including the impact of COVID-19; and to evaluate the impact of the country and policy factors, including the impact of COVID-19, on the implementation of alcohol screening in PC.
Methods
Design
This mixed methods study is part of a broader process evaluation of the SCALA study (Jane-Llopis et al., Citation2020). Both qualitative and quantitative data have been collected with the purpose of complementarity (Palinkas & Rhoades Cooper, Citation2018) with qualitative data used to describe the country and policy factors and quantitative data used to present the outcomes of the SCALA study, with data integration carried out at the point of analysis and interpretation.
Data sources and collection
To describe the country and policy context in each country, targeted desktop research of relevant sources was performed according to the predetermined list of factors (as described in ), based on the framework of Ysa et al. (Citation2014). The lead author searched websites of national and international organisations for information on demographics, development indices, organisation of healthcare systems, alcohol-related epidemiology, national strategies, and action plans. Additionally, local research partners in each country were approached to provide any documents they considered helpful to help describe the country and policy context. With the beginning of the COVID-19 pandemic, we also started systematically collecting data on the progression and impact of the pandemic in the countries through the reports from the local implementers.
To map the impact of country and policy factors on the implementation of alcohol screening (as the primary study outcome), we relied on three main sources of data: logbooks, interviews and project documentation.
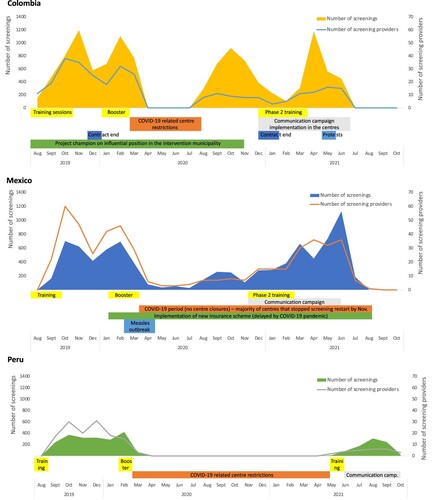
Every 4–6 weeks, implementation and research partners from each country sent logbooks to the process evaluation coordinator. The implementers had to shortly describe whether any changes had occurred on a national or regional level that could an impact the project implementation. The logbooks also contained space to provide information about field visits and feedback received from the providers. Project documentation refers to project meeting minutes, project presentations and project reports, which were shared with the process evaluation coordinator after every relevant meeting. These sources were scanned for any discussions pertaining to the impact of social and political context on implementation. Semi-structured (group) interviews (one per country at each time point) with local stakeholders involved in the implementation (researchers and liaisons with the participating centres (present in all countries); trainers (Mexico and Peru)) were conducted at three different time points during the project: prior to implementation of the intervention (Colombia (N = 2) and Mexico (N = 5) in May 2019), in Peru the interviews were not feasible due to time constraints; midway through the implementation period (Colombia (N = 2), Mexico (N = 4) and Peru (N = 2) in November/December 2020); and at the end of the implementation period (Colombia (N = 2), Mexico (N = 5), and Peru (N = 3) in August/September 2021). Group interviewing rather than focus group discussion was chosen as there was focus on sharing their experiences and perceptions rather than on the group interaction (Morgan, Citation1996). The initial topic guides (before the start of the project) for the interviews covered issues regarding general changes in the socio-political context, as well as any specific factors influencing project implementation, the general (non-tailored) materials are available as supplementary material in the protocol (Kokole et al., Citation2023). Later topic guides were tailored to each country based on the information obtained through logbooks and project documentation, to enable the exploration of any issues pertaining to country and policy context that had emerged during project implementation. Interviews were conducted in Spanish by the process evaluation coordinator, PhD candidate in background in psychology and health promotion, audio recorded, transcribed, and translated into English. The interviews ranged between 30 and 90 min in length. A complete overview of the data collection process is summarised in .
To describe the number of alcohol screenings over time, the number of tally sheets collected throughout the study period was considered, namely the number of alcohol screenings (applications of AUDIT-C questionnaire (Babor et al., Citation2001)) by country and month, as well as the number of providers applying the questionnaire at least once. Only data from the intervention arms were considered (not from the control arm), as we assumed that the implementation of the tested implementation strategies was comparable between the countries (despite some timing and execution differences), thus the remaining differences in the outcomes could be attributed to non-implementation related factors.
Data analysis
The qualitative data obtained through the sources described above were analysed through a combination of inductive and deductive coding (National Institutes of Health, Citation2018). The analysis was done in collaboration between one researcher from outside the countries and the research teams within the countries. First, one researcher (DK) thematically analysed the qualitative data sources for the country and policy factors that were discussed as impacting alcohol screening during the implementation period, and mapped those factors to the main framework (as depicted in ) (Ysa et al., Citation2014). Any available explanation on how those factors were purported to have influenced alcohol screening practices was also extracted, as was categorisation of factors as having a predicted positive (+) or negative (–) impact on the outcome. The identified factors and assessment of mechanisms and direction of the impact on country level were then additionally checked and validated by the research teams from each of the studied countries.
Next, SPSS and Excel were used to analyse and present the available outcome data (overall and monthly number of alcohol screenings and screening providers). Quantitative and qualitative data were merged for analysis through data transformation (Fetters et al., Citation2013) (qualitative factors categorised as having positive or negative impact, and then compared with the quantitative outcomes) and further compared with the construction of joint display, with both categories of findings presented side-by-side (Guetterman et al., Citation2015). Initial assessment and interpretation were done by one researcher, which were then again validated by the research teams from each of the studied countries.
Ethics
The SCALA study, including the process evaluation plan, has been reviewed and approved by the research ethics board at the TU Dresden, Germany (registration number: ‘EK 90032018’), and by the ethics boards in Colombia, Mexico, and Peru. All the interviewed participants provided informed consent to participation.
Results
Describing the country and policy factors at the beginning of implementation
The key country and policy factors identified at baseline are detailed and referenced in the Appendix 1, based on the 32 identified literature sources, and briefly summarised in . The three studied countries are similar in income level, human development and democracy, inequality, corruption perception as well as in values; therefore, these factors were unlikely to affect differences in country screening rates. The average per capita alcohol consumption is highest in Peru and lowest in Mexico, with marked differences between males and females in all three countries. Mexico has official standards that require inclusion with regard to the information on alcohol use in patient’s clinical history, and both Colombia and Mexico have standalone alcohol policies and action plans on the implementation of the policy. In all three countries, there has been a focus on strengthening PC through reforms, and in Peru, mental health reform was ongoing at the start and during SCALA implementation.
Table 1. Summary of the country and policy factors at the beginning of the implementation and impact of COVID-19.
Mapping impact of the country and policy factors on alcohol screening
The country and policy factors identified as potentially affecting the alcohol screening implementation in each of the countries are summarised in and further detailed in Appendix 2, including interview quotes for additional illustration. The identified factors were classified as general (features of the wider environment possibly impacting the overall results of the intervention in the countries) or time-bound (events during the implementation period that could impact the implementation during a specific time frame). For each of the factors identified through the qualitative investigation, the perceived mechanism and direction of impact is also presented.
Table 2. Overview of the country and policy factors influencing the implementation of alcohol screening.
Among the general factors, country factors such as characteristics of the population in Colombia and Peru, and political factors in Peru were identified, all of them perceived to have a negative impact on the SCALA implementation. In Colombia, the population in the intervention municipality changed often because they were only temporarily living in the town, meaning the providers had less opportunity to establish longer-term relationships with patients attending the centre (which would facilitate conversations about alcohol consumption). In Peru, some patients responded aggressively to their provider attempting to start a conversation on alcohol, particularly in centres located in disadvantaged areas with a high crime rate. Additionally, general political instability in the Peru was reflected also at a regional level, with five regional health authorities’ directors changing over two years, which hindered attempts to assure continuous project support from the health authorities. The existing screening practice was perceived to have a positive impact especially in Mexico, and to some extent in Colombia, but not in Peru. Likewise, policy priorities both in terms of existence of alcohol policy and policy prioritisation of PC were perceived as having positive impact in Colombia and Mexico. Healthcare system-related factors such as higher resistance to study participation among a small subset of unionised providers in Mexico, and general fragmentation of the healthcare system in Peru were seen as having a negative impact.
Among the time-bound factors, the COVID-19 pandemic had a negative impact in all three countries, but to a largest extent in Peru, as the activity of the healthcare centres was severely restricted for the longest period. Other external events negatively impacting the ability of the providers to screen were anti-government protests across Colombia, including in the intervention municipality of Soacha in the end of April 2021 (through decreasing patient attendance in the centres), and a measles outbreak in Mexico in February/March 2020 (through redirecting providers’ priorities to manage the outbreak). Some time-bound factors related to existing healthcare systems were also identified as relevant, such as yearly termination of providers contracts in Colombia, and introduction of the new insurance scheme in Mexico (Instituto de Salud para el Bienestar), which through increased coverage increased patient attendance, and allowed some centres to employ new providers (some of which ended up joining the study). Finally, a combination of political factors and COVID-19-related changes affected the length of the term of the project champion on the influential position in Colombia: initially, the project champion would have to end her term in April 2020 due to election-related changes of personnel, but this was then delayed due to COVID-19, so the project champion was able to stay in the (influential) position five additional months. In conclusion, in Peru, all of the identified contextual factors negatively impacted the implementation, whereas in Mexico and Colombia, both facilitating and hindering factors were identified.
Association with the outcome – general factors
In the previous section, we presented the factors identified through qualitative data collection and their perceived direction of impact. In this section, we used those factors to help explain the quantitative results of the study. While the large majority of screenings should be primarily attributed to the implemented activities related to training and community support in each of the countries, which despite the local tailoring represented comparable amount of implementation dosage (for detailed list of implemented activities, see Appendix 3), the overall country differences can (at least partially) be attributed to the specifics of the country contexts.
presents some key outcomes in each of the countries and uses the identified policy factors to help explain the comparative country differences. The general positive factors possibly explaining the comparatively higher overall numbers of screenings in Colombia and Mexico were the prioritisation of PC and the consideration of alcohol as public health issue, meaning that the project fitted well within wider policy priorities, leading to support from the (regional) health authorities. On the other hand, the comparatively lower number of screenings in Peru could be explained by a combination of: a weak PC system and implementation of a mental health reform redirecting the priorities away from PC; the framing of alcohol as an addiction (leading to perception that that alcohol problems should be dealt by specialists on individual level, rather than by PC providers), general political instability in the country which trickled down to regional health authorities, and the COVID-19 bringing the already under-resourced healthcare system to the brink of collapse.
Figure 3. Explanation of country differences in number of alcohol screenings and screening providers.
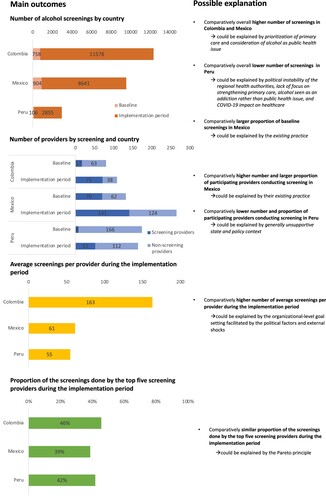
In Mexico, the existing alcohol practice and guidelines (official standards stipulating inclusion of alcohol use in patient’s medical file), could explain both the comparatively high number of providers conducting screening, as well as the high number of screenings at baseline; providers were (at least occasionally) already using the instrument in their daily practice. When considering the average number of screened patients however, we can observe that Colombian providers on average screened a much higher number of patients compared to their Mexican and Peruvian counterparts. One possible explanation of this finding could be that in case of Colombia, the community support-related activities implemented as part of SCALA (such as involving an individual in an influential position as a project champion, regular communication with providers through in-person contact, setting targets and monitoring screening numbers, and small financial incentives for the highest screening providers), could have contributed to the higher average number of screened patients per provider, and ultimately to the highest number of patients screened (despite the lower number of screening providers among the three countries).
Finally, there was one similarity between the countries: in all three, a small number of providers was responsible for conducting a large proportion of screening: the top five screening providers in each of the countries (representing 7%, 4% and 10% of all screeners respectively in Colombia, Mexico and Peru) screened 46% (Colombia), 39% (Mexico) and 42% (Peru) patients. This could be explained by the Pareto principle, a version of power law which in which the majority of consequences can be attributed to a small number of causes (Pareto, Citation2014).
Association with the outcome – time-bound factors
presents the monthly number of screenings and screening providers by country and overlays the time-bound factors identified in to see if they could contribute to the explanation of the screening numbers throughout the implementation period. Periods in which the providers were trained are also noted, as training has been shown to have an impact on screening practices (Anderson et al., Citation2021), explaining the general increase in the screening uptakes after the training period.
In Colombia, a decrease in the number of providers and screenings was observed in December and January every year, which may be due to the end of contracts as described above (although the decrease in December can also be partially attributed also to holiday-related decreased patient attendance). Between March and August 2020, providers were not screening because of COVID-19-related restrictions. After restarting the project in August 2020, screenings again increased, until November 2020 when a decrease can be observed after the departure of the project champion. This was mitigated by the next round of training (as well as community support activities described in the previous section), and the number of screenings culminated in April 2021, with further decreases possibly related to the anti-governmental protests (as described in Appendix 2) starting at the end of April and continuing in May, in combination with a new COVID-19 wave.
In Mexico, there were fewer external factors influencing the monthly trajectory of screening. After the training and booster session-related increases in screening numbers in the first months of the implementation period, the number of screenings started decreasing in March 2020, likely due to a combination of preparation for the COVID-19 pandemic and response to the measles outbreak. While small number of providers continued with screening in the early months of the pandemic, the number of screenings and screening providers only picked up with the next round of training. The subsequent increase could partially be attributed also to new providers joining the project after being employed due to the expansion of the new insurance scheme (INSABI, described in Appendix 2).
Finally, in Peru, COVID-19 had the greatest impact, making it impossible to conduct any alcohol screening between March 2020 and May 2021, due to the impact of the pandemic on the whole country and its healthcare system.
Discussion
This paper describes the country and policy context of Colombia, Mexico and Peru, and explores which country and policy factors appear to have contributed to alcohol screening rates by the PC providers in these three countries.
Our findings reveal that the country factors did not substantially differ between the three countries in question, and were therefore unlikely to explain country differences in the alcohol screening numbers, apart from the political factors, such as general political instability in Peru and (regional) governmental election leading to changes on the organisational level of the Colombian centres. Policy factors, on the other hand, especially existing practice, policy priorities and healthcare system structure were likely to contribute to country differences in the study outcome (alcohol screening numbers). External shocks (including COVID-19 pandemic) also negatively impacted the number of screenings.
In Colombia and Mexico, the policy context was overall supportive, facilitating the alcohol screening implementation. Policy framing of alcohol as a public health rather than medical issue likely contributed to better acceptance of alcohol screening as a population health approach among the PC providers and managers, which could explain our previous findings that doctors were more likely to both participate compared to other professional roles (nurses, psychologists etc) (Kokole et al., Citation2022). Presence of national policy plans or programmes has previously been shown to facilitate implementation of mental health-related programmes in PC in low- and middle-income countries (Esponda et al., Citation2019). Another important factor was existing alcohol screening practice, which can explain the higher number of providers participating in Mexico, as they were already familiar with using AUDIT due to the official standards stipulating inclusion of alcohol use information in patient history. The existence of experienced providers can also explain the high levels of alcohol screening-related self-efficacy at baseline in Mexico compared to other participating countries, and its association with higher likelihood of screening (Kokole, Jané-Llopis, et al., Citation2021). However, despite the existing practice, the average number of screenings per provider was similar in Mexico and Peru, potentially indicating the impact of commonly mentioned barriers such as lack of time in consultation on practice (Rosário et al., Citation2021). Alternatively, in Colombia, the comparatively smaller number of screening providers that contributed to the overall highest number of screenings suggests the exceptionally strong impact of the community support activities implemented as part of SCALA, and their interaction with both the wider environment and the organisational context. Despite the existence of the supportive policy context in the both Mexico and Colombia, however, effects of unforeseen events on the alcohol screening could still be noticed on smaller time-scale: disease outbreaks served to redirect providers work priorities in Mexico, and anti-government protests in Colombia led to decreased patient attendance. External shocks such as political events and disease outbreaks have previously been identified to negatively impact the resilience of health workers and health systems (Sripad et al., Citation2021).
In Peru however, the context was very unsupportive already before COVID-19 pandemic hit due to a mix of political (instability among the regional health authorities) and policy-related factors (decentralisation of the healthcare system, lack of focus on strengthening PC, and alcohol being seen as an addiction rather than a public health issue). This policy context also explains some of our previously published process evaluation findings, for example, the perceived lack of guidelines and available screening instruments as a barrier (Kokole, Mercken, et al., Citation2021) and higher proportion of participating and screening psychologists in comparison to other professional roles (Kokole et al., Citation2022). Furthermore, the lack of external encouragement to participate in the study, as well as lack of previous education in alcohol prevention provision, could explain their comparatively higher therapeutic commitment (Kokole, Jané-Llopis, et al., Citation2021) and very high appreciation of the training sessions (Kokole et al., Citation2022). More simply put, in this unsupportive environment, the Peruvian providers who ended up joining the SCALA study were those with higher intrinsic motivation to learn about the alcohol prevention provision, but less previous education in it.
Implications for research and practice
The main implication of this study is the necessity of considering the wider environment in which an intervention is to be implemented, especially when seeking to scale relatively novel healthcare practices. Several reviews evaluating implementation strategies, both in the field of alcohol screening and other alcohol and mental health interventions (Louie et al., Citation2021; Piat et al., Citation2021; Williams et al., Citation2011), found few or no implementation strategies targeting the wider environment, likely because they are difficult to target – although some factors can be considered more modifiable than others (Bruns et al., Citation2019). When it comes to modifiable factors such as introducing policies (on healthcare level or broader), strategies such as knowledge brokering, policy briefs, workshops or targeted messaging can be used, although more research is necessary into their effectiveness, taking into account that low resource intensity might be better suited (Sarkies et al., Citation2017). While the need for such research is increasingly being recognised (Emmons & Chambers, Citation2021), as a starting point, researchers and implementers should at least map the relevant characteristics, especially policy-related factors (e.g. policy priorities related to the intervention, or structure and incentives of the broader healthcare system in case of a healthcare innovation) at baseline, and plan to capture any changes throughout the implementation phase.
A related question is how should the assessment of the wider environment impact the attempts to scale-up; are the countries identified as having an unsupportive implementation context automatically excluded, knowing that much more effort will be needed for a (comparatively) smaller output? We would advise against that, as scale-up should primarily be based on the need, followed by the availability of the resources. Examination of the wider environment (in combination with assessment of the local stakeholder network and locally relevant factors) can aid in knowing how to best use those resources and, in line with systems approaches, which leverage points should be targeted to achieve the largest change (e.g. Meadows, Citation1999).
A theoretical implication based on the examination of existing literature in this field is the need for greater clarity on how the term ‘context’ is used. While all definitions (Moore et al., Citation2014; Nilsen & Bernhardsson, Citation2019; Pfadenhauer et al., Citation2017; Steckler & Linnan, Citation2002) include the wider environment, some are broader, and include also additional factors beyond the wider environment as described in the introduction (e.g. Moore et al., Citation2014; Nilsen & Bernhardsson, Citation2019). This can hinder search for the relevant literature, e.g. sometimes individual attitudes are already framed as ‘contextual factors’ (Rogers et al., Citation2020). There is an increasing number of studies recognising the importance of the wider environment, especially in low- and middle-income countries, but there is no consistent term that is used across literature – terms ‘wider environment’ (Nilsen & Bernhardsson, Citation2019), ‘macro context’ (Willging et al., Citation2021) or simply ‘context’ are used interchangeably, and concepts such as ‘outer setting’ (Damschroder et al., Citation2009, Citation2022) or ‘social, legal and political factors’ (Flottorp et al., Citation2013) are used in the implementation frameworks to denote this category.
Limitations
The main limitation is that due to the explicit contextual nature of the research, it is not possible to generalise the findings to other settings. For example, while the country context was largely similar in the three Latin American countries and did not appear to contribute to country differences in this study, this might not be the case in multi-country studies with a differing country context. Furthermore, the identified general factors are not static and reflect the situation during the study period (in the years 2018–2021). Rather than providing absolute claims about the factors relevant across all contexts, our aim is to point towards categories to consider when implementing future interventions, as well as to provide an approach that can be used to assess the country and policy contexts and their contribution to outcome, which will inevitably show up in differing constellations in other studies. Related to this, the outcome data came from single regions rather than from the entire country, and the impact of the same contextual factors might be different in other regions within the same country. Secondly, the data collected for the qualitative part to certain extent reflected perceptions of the implementers in the three countries and might be therefore be criticised of for being overly subjective (especially the interpretation of the event impact, rather than the event itself). To mitigate this possibility, we interviewed at least two people in each country. Additionally, the results were analysed by a researcher not living in any of the studied countries, which provided an opportunity to balance the internal (in the countries) and external (outside the countries) perspectives. Integration with the quantitative outcome data also allowed us to confirm the hypothesised direction of the impact at least for some of the identified factors. Finally, in terms of the initial baseline context description, we had to limit our scope and decided to focus on certain set of country and policy factors, as it would be too time- and resource-intensive to consider all possible wider environmental factors. This means we may have missed the description of some baseline factors that could also be relevant for better situating our study. However, we allowed any additional factors to emerge with the subsequent qualitative investigation.
Conclusion
Country factors could not explain the outcome differences between countries as the three countries were comparatively similar in many of the relevant dimensions. The only exception was political factors, which impeded alcohol screening, particularly in Peru. Policy factors such as the prioritisation of primary care, framing alcohol as a public health issue, and existing alcohol screening practice, helped to facilitate the implementation of alcohol screening on a larger scale, as seen in Colombia and Mexico. External shocks (including COVID-19 pandemic) substantially and adversely affected alcohol screening. Wider environmental factors should be captured and monitored in future implementation interventions, and better conceptualised within the field of the implementation science.
Supplemental Material
Download MS Word (300.8 KB)Acknowledgements
EJL, HDV, PA, AOD, BS, AP, JMT, GNR, MP and IB contributed to the Grant Application for the study, and provided feedback on evaluation design and instrument development. DK, EJL, LM, HDV and PA conceptualised the study. DK collected and analysed the data. JMT, AP, GNR, PSMA, NBA, MA, APL, MP and IB contributed to analysis and interpretation of the results on country level. DK, EJL, LM, HDV and PA drafted the first version of the paper. DK revised the paper based on co-authors’ feedback and comments. All co-authors commented on subsequent drafts of the manuscript, read and approved the final version.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anderson, P., Manthey, J., Jané-Llopis, E., Natera Rey, G., Bustamante, I. V., Piazza, M., Aguilar, P. S. M., Mejía-Trujillo, J., Pérez-Gómez, A., Rowlands, G., Lopez-Pelayo, H., Mercken, L., Kokole, D., O’Donnell, A., Solovei, A., Kaner, E., Schulte, B., de Vries, H., Schmidt, C., … Rehm, J. (2021). Impact of training and municipal support on primary health care-based measurement of alcohol consumption in three Latin American countries: 5-month outcome results of the quasi-experimental randomized SCALA trial. Journal of General Internal Medicine, 1–9. https://doi.org/10.1007/s11606-020-06503-9
- Atun, R., de Andrade, L. O. M., Almeida, G., Cotlear, D., Dmytraczenko, T., Frenz, P., Garcia, P., Gómez-Dantés, O., Knaul, F. M., Muntaner, C., de Paula, J. B., Rígoli, F., Serrate, P. C. F., & Wagstaff, A. (2015). Health-system reform and universal health coverage in Latin America. The Lancet, 385(9974), 1230–1247. https://doi.org/10.1016/S0140-6736(14)61646-9
- Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). AUDIT – the alcohol use disorders identification test. World Health Organization. https://doi.org/10.1177/0269881110393051
- Bruns, E. J., Parker, E. M., Hensley, S., Pullmann, M. D., Benjamin, P. H., Lyon, A. R., & Hoagwood, K. E. (2019). The role of the outer setting in implementation: Associations between state demographic, fiscal, and policy factors and use of evidence-based treatments in mental healthcare. Implementation Science, 14(1), 1–13. https://doi.org/10.1186/s13012-019-0944-9
- Craig, P., Di Ruggiero, E., Frohlich, K. L., Mykhalovskiy, E., White, M., Campbell, R., Cummins, S., Edwards, N., Hunt, K., Kee, F., Loppie, C., Moore, L., Ogilvie, D., Petticrew, M., Poland, B., Ridde, V., Shoveller, J., Viehbeck, S., & Wight, D. (2018). Taking account of context in population health intervention research: Guidance for producers, users and funders of research. National Institute for Health Research. https://doi.org/10.3310/CIHR-NIHR-01
- Daivadanam, M., Ingram, M., Annerstedt, K. S., Parker, G., Bobrow, K., Dolovich, L., Gould, G., Riddell, M., Vedanthan, R., Webster, J., Absetz, P., Alvesson, H. M., Androutsos, O., Chavannes, N., Cortez, B., Devarasetty, P., Fottrell, E., Gonzalez-Salazar, F., Goudge, J., … Zhang, P. (2019). The role of context in implementation research for non-communicable diseases: Answering the “how-to” dilemma. PLoS ONE, 14(4), 1–22. https://doi.org/10.1371/journal.pone.0214454
- Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4(1), 1–15. https://doi.org/10.1186/1748-5908-4-50
- Damschroder, L. J., Reardon, C. M., Widerquist, M. A. O., & Lowery, J. (2022). The updated consolidated framework for implementation research based on user feedback. Implementation Science, 17(1), 1–16. https://doi.org/10.1186/s13012-021-01157-5
- Emmons, K. M., & Chambers, D. A. (2021). Policy implementation science – an unexplored strategy to address social determinants of health. Ethnicity & Disease, 31(1), 133–138. https://doi.org/10.18865/ed.31.1.133
- Esponda, G. M., Hartman, S., Qureshi, O., Sadler, E., Cohen, A., & Kakuma, R. (2019). Barriers and facilitators of mental health programmes in primary care in low-income and middle-income countries. The Lancet Psychiatry, 0366(19), 1–15. https://doi.org/10.1016/s2215-0366(19)30125-7
- Faregh, N., Lencucha, R., Ventevogel, P., Dubale, B. W., & Kirmayer, L. J. (2019). Considering culture, context and community in mhGAP implementation and training: Challenges and recommendations from the field. International Journal of Mental Health Systems, 13(1), 1–13. https://doi.org/10.1186/s13033-019-0312-9
- Fetters, M. D., Curry, L. A., & Creswell, J. W. (2013). Achieving integration in mixed methods designs – principles and practices. Health Services Research, 48(6pt2), 2134–2156. https://doi.org/10.1111/1475-6773.12117
- Fleuren, M., Wiefferink, K., & Paulussen, T. (2004). Determinants of innovation within health care organizations literature review and Delphi study. International Journal for Quality in Health Care, 16(2), 107–123. https://doi.org/10.1093/intqhc/mzh030
- Flottorp, S. A., Oxman, A. D., Krause, J., Musila, N. R., Wensing, M., Godycki-Cwirko, M., Baker, R., & Eccles, M. P. (2013). A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implementation Science, 8(1). https://doi.org/10.1186/1748-5908-8-35
- Ghosh, A., Singh, P., Das, N., Pandit, P. M., Das, S., & Sarkar, S. (2022). Efficacy of brief intervention for harmful and hazardous alcohol use: A systematic review and meta-analysis of studies from low middle-income countries. Addiction, 117(3), 545–558. https://doi.org/10.1111/add.15613
- Guetterman, T. C., Fetters, M. D., & Creswell, J. W. (2015). Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Annals of Family Medicine, 13(6), 554–561. https://doi.org/10.1370/afm.1865
- Jane-Llopis, E., Anderson, P., Piazza, M., O’Donnell, A., Gual, A., Schulte, B., Gomez, A. P., Vries, H. D., Rey, G. N., Kokole, D., Bustamente, I., Braddick, F., Trujillo, J. M., Solovei, A., Leon, A. P. D., Kaner, E., Matrai, S., Manthey, J., Mercken, L., … Rehm, J. (2020). Implementing primary health care-based measurement, advice and treatment for heavy drinking and comorbid depression at the municipal level in three Latin American countries: Final protocol for a quasi-experimental study (SCALA study). BMJ Open, 10(e038226), 1–14. https://doi.org/10.21203/rs.2.22734/v1
- Kaner, E. F. S., Beyer, F. R., Muirhead, C., Campbell, F., Pienaar, E. D., Bertholet, N., Daeppen, J. B., Saunders, J. B., & Burnand, B. (2018). Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews, 2018(2), 1–200. https://doi.org/10.1002/14651858.CD004148.pub4
- Kokole, D., Jané-Llopis, E., Mercken, L., Natera Rey, G., Arroyo, M., Pérez Gómez, A., Mejía-Trujillo, J., Piazza, M., Bustamante, I., O’Donnell, A., Kaner, E., Schulte, B., de Vries, H., & Anderson, P. (2023). Protocol for a process evaluation of SCALA study – intervention targeting scaling up of primary health care-based prevention and management of heavy drinking and comorbid depression in Latin America. Evaluation and Program Planning, 97, Article 102217. https://doi.org/10.1016/j.evalprogplan.2022.102217
- Kokole, D., Jané-Llopis, E., Mercken, L., Piazza, M., Bustamante, I., Natera Rey, G., Medina, P., Pérez-Gómez, A., Mejía-Trujillo, J., O’Donnell, A., Kaner, E., Gual, A., Schmidt, C. S., Schulte, B., Candel, M. J. J. M., de Vries, H., & Anderson, P. (2021). Factors associated with primary health care providers’ alcohol screening behavior in Colombia, Mexico and Peru. Substance Abuse. https://doi.org/10.1080/08897077.2021.1903658
- Kokole, D., Jané-Llopis, E., Natera, G., Bautista, N., Medina, P., Mejía-Trujillo, J., Mora, K., Restrepo, N., Bustamante, I., Piazza, M., O’Donnell, A., Solovei, A., Mercken, L., Schmidt, C., Lopez-Pelayo, H., Matrai, S., Braddick, F., Gual, T., Rehm, J., … de Vries, H. (2022). Training primary health care providers in Colombia, Mexico and Peru to increase alcohol screening: Mixed methods process evaluation of implementation strategy. Implementation Research and Practice, 3, 263348952211126. https://doi.org/10.1177/26334895221112693
- Kokole, D., Mercken, L., Jané-Llopis, E., Natera Rey, G., Arroyo, M., Medina, P., Pérez-Gómez, A., Mejía-Trujillo, J., Piazza, M., Bustamante, I. V., O’Donnell, A., Kaner, E., Gual, A., Lopez-Pelayo, H., Schulte, B., Manthey, J., Rehm, J., Anderson, P., & de Vries, H. (2021). Perceived appropriateness of alcohol screening and brief advice programmes in Colombia, Mexico and Peru and barriers to their implementation in primary health care-a cross-sectional survey. Primary Health Care Research and Development, 22(e4). https://doi.org/10.1017/S1463423620000675
- Liu, H., Mohammed, A., Shanthosh, J., News, M., Laba, T. L., Hackett, M. L., Peiris, D., & Jan, S. (2019). Process evaluations of primary care interventions addressing chronic disease: A systematic review. BMJ Open, 9(8), e025127. https://doi.org/10.1136/BMJOPEN-2018-025127
- Louie, E., Barrett, E. L., Baillie, A., Haber, P., & Morley, K. C. (2021). A systematic review of evidence-based practice implementation in drug and alcohol settings: Applying the consolidated framework for implementation research framework. Implementation Science , 16(1), 22. https://doi.org/10.1186/s13012-021-01090-7
- Manthey, J., Shield, K. D., Rylett, M., Hasan, O. S. M., Probst, C., & Rehm, J. (2019). Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. The Lancet, 393(10190), 2493–2502. https://doi.org/10.1016/S0140-6736(18)32744-2
- Manthey, J., Solovei, A., Anderson, P., Carr, S., & Rehm, J. (2021). Can alcohol consumption in Germany be reduced by alcohol screening, brief intervention and referral to treatment in primary health care? Results of a simulation study. PLoS One, 16(8), e0255843. https://doi.org/10.1371/journal.pone.0255843
- Meadows, D. (1999). Leverage points: Places to intervene in a system. https://donellameadows.org/archives/leverage-points-places-to-intervene-in-a-system/.
- Moore, G., Audrey, S., Barker, M., Bond, L., Bonell, C., Hardeman, W., Moore, L., O’Cathain, A., Tinati, T., Wight, D., & Baird, J. (2014). Process evaluation of complex interventions UK Medical Research Council (MRC) guidance. https://mrc.ukri.org/documents/pdf/mrc-phsrn-process-evaluation-guidance-final/
- Morgan, D. L. (1996). Focus groups. Annual Review of Sociology, 22(1), 129–152. https://doi.org/10.1146/annurev.soc.22.1.129
- National Institutes of Health. (2018). Qualitative methods in implementation science. https://cancercontrol.cancer.gov/sites/default/files/2020-09/nci-dccps-implementationscience-whitepaper.pdf
- Nilsen, P., & Bernhardsson, S. (2019). Context matters in implementation science: A scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Services Research, 19(1), 1–21. https://doi.org/10.1186/s12913-019-4015-3
- O’Donnell, A., Wallace, P., & Kaner, E. (2014). From efficacy to effectiveness and beyond: What next for brief interventions in primary care? Frontiers in Psychiatry, 5(113), 1–8. https://doi.org/10.3389/fpsyt.2014.00113
- Palinkas, L. A., & Rhoades Cooper, B. (2018). Mixed methods evaluation in dissemination and implementation science. In R. C. Brownson, G. A. Colditz, & E. K. Proctor (Eds.), Dissemination and implementation research in health: Translating science to practice (2nd ed., pp. 335–354). Oxford University Press.
- Pareto, V. (2014). Manual of political economy: A critical and variorum edition. Oxford University Press.
- Pfadenhauer, L. M., Gerhardus, A., Mozygemba, K., Lysdahl, K. B., Booth, A., Hofmann, B., Wahlster, P., Polus, S., Burns, J., Brereton, L., & Rehfuess, E. (2017). Making sense of complexity in context and implementation: The context and implementation of complex interventions (CICI) framework. Implementation Science, 12(1), 1–17. https://doi.org/10.1186/s13012-017-0552-5
- Piat, M., Wainwright, M., Sofouli, E., Vachon, B., Deslauriers, T., Préfontaine, C., & Frati, F. (2021). Factors influencing the implementation of mental health recovery into services: A systematic mixed studies review. Systematic Reviews, 10(1), 1–21. https://doi.org/10.1186/s13643-021-01646-0
- Rogers, L., De Brún, A., & McAuliffe, E. (2020). Defining and assessing context in healthcare implementation studies: A systematic review. BMC Health Services Research, 20(1), 1–24. https://doi.org/10.1186/S12913-020-05212-7/FIGURES/4
- Ronzani, T. M., Fuentes-Mejía, C., Mota, D. C. B., Gomide, H. P., Ferreira, M. L., & Cruvinel, E. (2019). Brief interventions for substance abuse in Latin America: A systematic review. Psicologia Em Estudo, 24(e44393), 1–16. https://doi.org/10.4025/PSICOLESTUD.V24I0.44393
- Rosário, F., Santos, M. I., Angus, K., Pas, L., Ribeiro, C., & Fitzgerald, N. (2021). Factors influencing the implementation of screening and brief interventions for alcohol use in primary care practices: A systematic review using the COM-B system and theoretical domains framework. Implementation Science, 16(1), 1–25. https://doi.org/10.1186/s13012-020-01073-0
- Sarkies, M. N., Bowles, K. A., Skinner, E. H., Haas, R., Lane, H., & Haines, T. P. (2017). The effectiveness of research implementation strategies for promoting evidence-informed policy and management decisions in healthcare: A systematic review. Implementation Science, 12(1), 1–20. https://doi.org/10.1186/S13012-017-0662-0/FIGURES/2
- Shannon, C. L., Bartels, S. M., Cepeda, M., Castro, S., Cubillos, L., Suárez-Obando, F., Williams, M. J., Gómez Restrepo, C., Uribe, M., Marsch, L., & Torrey, W. C. (2021). Perspectives on the implementation of screening and treatment for depression and alcohol use disorder in primary care in Colombia. Community Mental Health Journal, 57(8), 1579–1587. https://doi.org/10.1007/s10597-021-00781-1
- Solovei, A., Mercken, L., Jané-Llopis, E., Bustamante, I. S., Evers, S., Gual, A., Medina, P., Mejía-Trujillo, J., Natera-Rey, G., O’donnell, A., Pé Rez-Gó Mez, A., Piazza, M., De Vries, H., & Anderson, P. (2021). Development of community strategies supporting brief alcohol advice in three Latin American countries: A protocol. Health Promotion International, 2021, 1–11. https://doi.org/10.1093/HEAPRO/DAAB192
- Sripad, P., Casseus, A., Kennedy, S., Isaac, B., Vissieres, K., Warren, C. E., & Ternier, R. (2021). “Eternally restarting” or “a branch line of continuity”? Exploring consequences of external shocks on community health systems in Haiti. Journal of Global Health, 11, 1–11. https://doi.org/10.7189/JOGH.11.07004
- Steckler, A., & Linnan, L. (Eds.). (2002). Process evaluation for public health interventions and research. Jossey-Bass/Wiley.
- Willging, C. E., Jaramillo, E. T., Haozous, E., Sommerfeld, D. H., & Verney, S. P. (2021). Macro- and meso-level contextual influences on health care inequities among American Indian elders. BMC Public Health, 21(1), 1–14. https://doi.org/10.1186/S12889-021-10616-Z/TABLES/2
- Williams, E. C., Johnson, M. L., Lapham, G. T., Caldeiro, R. M., Chew, L., Fletcher, G. S., McCormick, K. A., Weppner, W. G., & Bradley, K. A. (2011). Strategies to implement alcohol screening and brief intervention in primary care settings: A structured literature review. Psychology of Addictive Behaviors, 25(2), 206–214. https://doi.org/10.1037/a0022102
- Ysa, T., Colom, J., Albareda, A., Ramon, A., Carrión, M., & Segura, L. (2014). Governance of addictions: European public policies. Oxford University Press.