ABSTRACT
Implemented in several African countries, medical drones have emerged as a major infrastructural innovation in national healthcare systems and are widely hailed for improving, if not revolutionising, access to medicine and care for rural populations. Being based on digitally driven, autonomous aviation systems, drones are part of wider efforts to use digital technologies in health systems. In this article, we explore the paradoxes that emerge from definitions of logistics as the bottleneck of quality healthcare. Based on ethnographic research in Ghana, we explore the ways in which drone systems have been built up and justified by private and political actors and used by pharmacists and other healthcare professionals along the supply chain as serving emergencies. However, they have transformed the existing landscape of medical supply chiefly because of the multiple ways in which emergencies are defined. We find that while the introduction of drones has dynamised supply chain processes but also reveals structural bottlenecks, e.g. the lack of medical products and malfunctioning institutions. Situated at the interface of critical studies on infrastructures and medical anthropology, our article contributes to the thriving scholarship on digital innovation in healthcare.
Introduction
Infrastructural and technological advances in the field of global health, as well as in the development world as a whole, usually target sites where performances and outcomes are considered inadequate, despite being crucial for achieving development goals. Following development jargon, we call these sites ‘bottlenecks of health care’. This article explores the consequences and paradoxes that emerge when logistics are defined as the bottleneck of healthcare and drones as the solution. In Ghana, the introduction of medical drones – drones that deliver medical products to health centres in remote, rural areas – have started to reconfigure a complex landscape of healthcare and health logistics. As part of broader efforts to introduce state-of-the-art technologies and to digitise the healthcare system, drones are used to improve supply and access to medical items such as medicines, blood and vaccines.
Significantly, over the past decade, the Ghanaian state has been pushing digitisation projects in several areas, including a registry of landownership, a system of residential addresses and the introduction of digital identity cards (Thiel, Citation2020). Nourishing widespread fantasies of infrastructural leapfrogging, many policymakers and experts celebrate such technical solutions as a panacea for the country's economic and administrative problems (Burchardt & Umlauf, Citation2023). Significantly raising the stakes of the national digitisation agenda, Ghana's Vice President Mahamudu Bawumia even stated in a television interview in 2017: ‘We need to essentially remove a lot of the human interfaces so that we could deliver services to ordinary people devoid of corruption’.Footnote1 Removing humans from service delivery as a way of fighting corruption became part of a more general hope that the increasing digitisation of governmental services would contribute to creating a more inclusive society.
In this article, we take the promises of digital solutions to improve access to healthcare as a starting point in investigating some of the more implicit assumptions associated with the adoption of digital technologies in healthcare and the way they are played out on the ground. More specifically, we are interested in the ways in which the relationships between existing analogue and new, digitally driven infrastructures of supply unfold. In the field of medical logistics in Ghana, this means primarily the relationship between road transport and the newly introduced drone system.
In 2018, the government of Ghana signed a contract with the Silicon Valley start-up company Zipline, which was tasked with building up drone infrastructure (including its own distributions centres) and with organising up to 600 deliveries a day to health facilities across the country. While Zipline initially built four distribution centres, when the contract was renewed in 2021, four other centres were added to finally allow the company to serve approximately 3200 health facilities covering large parts of the national territory. Significantly, to avoid competition between land transport and airborne deliveries, drone use was limited to medical emergencies, such as the blood products for mothers suffering from postpartum haemorrhaging, snake-bite medicines and other products needed to support medical interventions in emergency situations. From the perspectives of medical anthropology and critical studies of infrastructure, this raises an intriguing set of questions: Through what kinds of practices did the introduction of these systems unfold on the ground? How did the availability of drone services change access to medical products? How did logistics and healthcare practitioners adapt these services to their daily routines to make them serve their needs? And how do the realities of drone logistics relate to the lofty promises that are meant to promote them?
According to classic social-science approaches, when it comes to technological innovation in infrastructural provision, new infrastructure tends to develop in a cycle. This means starting by complementing the existing infrastructure and then gradually replacing it. The relationship between the old and new infrastructure is based on technical affordance. In Ghana, where the project is also called fly-to-save-a-life,Footnote2 public innovation discourses portray these relationships as productive and synergetic modes of supply. Thus, the Minister of Health, Kwaku Agyeman-Manu, emphasised that the project ‘is not in any way expected to replace the existing regular supply chain system for the delivery of blood and medical products’.Footnote3 There are also echoes of such understandings in software language, where the term ‘interoperability’ describes system interactions, as well as experimental and organisational factors that become newly assembled.
However, more recent studies have emphasised the ways in which new digital infrastructure gives rise to disputes and conflicts, as they shift consumption patterns, empower new groups of actors, disempower others and reconfigure markets (e.g. Langley & Leyshon, Citation2022; Thorat, Citation2020). Following up on these studies, we find that, while in rural areas especially healthcare workers make massive use of drone logistics and actually celebrate them as gamechangers, drone operations are actually marked by a series of paradoxes: while drones were chiefly meant to transport products for medical emergencies, in practice they are often used for other purposes. These other purposes strike us as being justified and enabled through shifting understandings of emergency. On a more technical level, while actual airborne services function very smoothly, deliveries are often delayed or hampered by medical products going out of stock, revealing structural bottlenecks from which the company cannot simply disconnect itself. Our article unearths the mechanisms through which these paradoxes came about, providing important lessons for social theories of technological and institutional change (Star & Griesemer, Citation1989; Watkins & Swidler, Citation2013).
We begin by situating the rise of drone logistics in African healthcare in the context of social sciences debates on emergencies, medical humanitarianism and medical technologies that have flourished over the past two decades. While we highlight the importance of shifting the focus away from macro-perspectives towards more concrete empirical circumstances in which infrastructure is configured and used, we note the dearth of research on logistics in anthropological studies on the nexus of healthcare and infrastructure. Our analysis is therefore geared towards foregrounding the ways in which innovations in infrastructure depend on definitions of logistics as a bottleneck in healthcare.
Theorising digitisation in healthcare, logistics and emergencies
Our research on the introduction of medical drones and their consequences for access to healthcare is situated at the interface of three scholarly debates: research on the digitisation of healthcare, infrastructural leapfrogging and research on emergencies in Global Health. We briefly revisit these scholarly fields in order to explain our conceptual approach, highlight our contribution to these literatures and delineate the features of the emerging field of digital health infrastructure.
Over the past decade, there have been massive investments in the digitisation of healthcare on a global scale (Storeng et al., Citation2021). These include digitalised patient records and insurance schemes, wearables, algorithm-based applications in mental health, advances in Big Data-driven precision medicine, digitised stock and supply chain management, and digitally driven logistics such as drones. All this infrastructure and the associated technologies have benefited from advances in machine learning, cloud-computing and new sensor technologies (Lupton, Citation2014, Citation2017; Miller & Horst, Citation2020). Investments in digital health technologies have been financed by both private companies and states and have shaped new alliances and consortia involving large, multinational pharmaceuticals companies, public research institutions, public health authorities and tech start-ups. As almost all efforts to launch new digital technologies are based on large server capacities for data processing, big internet companies (Amazon, Meta, Microsoft, Apple and Google) provide the so-called core infrastructure of the platform economy (van Dijck et al., Citation2018). Because of the increasing importance of established tech players as well as new start-ups, their business strategies, conceptual approaches and jargon – typical of Silicon Valley-styled ‘digital solutionism’ (Morozov, Citation2013) – have made their way into the cultural worlds of healthcare in general and global health in particular. In our research, for instance, Silicon Valley drone operators were fond of using the slogan ‘Press a button and get what you need’ for describing how drone technologies would revolutionise healthcare in rural Africa. If digital solutionism means the idea that the internet or Big Data-based algorithms offer solutions not only to business problems but also to global social problems (e.g. to climate change, water scarcity, or a lack of access to healthcare), then it has surely fallen on fertile ground in the field of global health (Krieg et al. Citation2017).
One reason for this is that digital solutionism resonates powerfully with magic-bullet approaches to global health problems, e.g. vaccines, mobile test kits and so on (Biehl, Citation2016). Also referred to as vertical interventions, these approaches similarly favour breakthroughs in specific medical technologies over structural approaches aimed at improving health outcomes through horizontal approaches, for instance, by improving access to primary healthcare (Storeng et al., Citation2021). Such approaches have long been criticised for causing far-reaching institutional and technological fragmentations in African healthcare systems.
Importantly, during the early 2000s, the WHO declared HIV/AIDS to be a global humanitarian emergency aiding the formation of the new paradigm of global health (Nguyen, Citation2009) and new institutional arrangements, e.g. the Global Fund (Collier & Lakoff, Citation2008). One commonly observed side-effect of these new assemblages (Ong & Collier, Citation2007) was a strong growth in funding, which increased the fragmentations in national public health systems (Kelly & Beisel, Citation2011). Due to a lack of coordination, these large programmes created chaotic replications, inefficient resource use and failures to meet targets (e.g. in relation to health-related millennium development goals) (Biesma et al., Citation2009). In our study, we follow this line of argument and ask to what extend such fragmentations are reproduced through the rise of digitally driven logistics, paying particular attention to the differences between institutional fragmentation and infrastructural disconnection (Dilger and Mattes Citation2018).
There are now also thriving scholarly debates and research on digitisation in African countries (Friederici et al., Citation2020; Heeks, Citation2022). In this context, initial contributions highlighted the ways in which the digital divide not only reflected existing global economic disparities, but also exacerbated the structural disadvantages of African economies and populations (Heeks, Citation2022). More recent scholarship, by contrast, has focused on the establishment of digital infrastructure, as well as the spread and adoption of digital technologies among Africans (Neumark & Prince, Citation2021). Building on different areas of digitisation and the use of the internet, recent studies have started to explore the concrete impact of the intensified use of smart, digital devices in various social fields, like work and labour relations, governance, and security, as well as processes of datafication (Ruckenstein & Schüll, Citation2017; Plantin et al., Citation2018; Plantin & Punahtmabekar Citation2019). Much attention has been paid to Kenya and its ‘Digital Savannah’ (Poggiali, Citation2016). However, relatively few studies have so far discussed current developments in the growing field of digital health in Africa (Mawere & van Stam, Citation2020). In addition, even within the wider social scientific literature on access to medicine and healthcare in relation to digitisation, only a few studies explore the role of logistics.
In general, among anthropologists and scholars of science and technology studies (STS), access to medicine is still predominantly framed as an outcome of global pharma-capitalism and the ways in which global legal frameworks around intellectual property (e.g. patent and copyright law), the spatial order and the regional concentration of pharma capital, the price structures in pharmaceutical markets and the brain-drain induced by health professionals’ migration all contribute to reproducing the massive global disparities that currently exist (see Pollock, Citation2019). Surprisingly little attention has been paid to how start-up companies in the digital sector have sought to reframe access to medicine almost exclusively as a problem of logistics. Within this wider problem space, we consider it worthwhile to relate digital health logistics back to these existing debates around magic bullets, the fragmentations in global health and infrastructural leapfrogging (Burchardt & Umlauf, Citation2023).
Importantly, questions of how infrastructure and access to the services it provides are the backbone of everyday life, shaping both the boundaries and inner workings of societies, co-constructing social hierarchies and becoming subject to political contestation, have been widely discussed over the past two decades. Scholars have argued that infrastructure literally connects people and the state and thus underwrites notions of citizenship (Von Schnitzler, Citation2018). In medical anthropology, by contrast, the links between material infrastructure and healthcare have been studied primarily in the context of epidemics. In HIV/AIDS, the logistical-infrastructural aspects of access to medicines have been shown to influence local patterns of relationships and to generate specific treatment logics (Park, Citation2012; Umlauf, Citation2017). However, the insights of critical studies of infrastructure have only sparsely been taken up in global health scholarship, and with few exceptions (Beisel, Citation2014), research on the interplay of infrastructure, space and logistics has yet to emerge. In our article, we advance such approaches by exploring how digital logistics pivots on space as a problem and bottleneck.
The digitisation of healthcare introduces new actors into the existing arena of global health programmes. So far, African countries have had only limited experience with US-based start-ups, especially with those, such as Zipline, that actually take off by offering their services in Africa. At the same time, these processes champion different fields of medical care, such as emergency medicine, which had not received much attention hitherto in global health funding (Hsia et al., Citation2010). With a view to avoiding competition between land transport and drones, the contract between Zipline and Ghana's Ministry of Health explicitly limited the use of drones to emergency situations. This focus on emergency medicine emerged from the idea that this field would most dramatically benefit from the speed and precision of Zipline's autonomous aviation system. Yet, as we will show, it also came with its own challenges. More specifically, the necessity for stock managers, clinic-based pharmacists and other actors in the supply chain to demonstrate that their orders are linked to emergencies provided incentives to frame their needs in such terms, but it also led to an incessant proliferation of new meanings and outright confusion about what an emergency actually is.
In thinking about the role of emergencies in shaping the drone field and about the lessons they provide for theories of institutional and technological change, we have primarily been inspired by cultural theorists Watkins and Swidler (Citation2013) as well as the ground-breaking work of STS scholars Star and Griesemer (Citation1989). In their studies on NGOs and development projects around HIV/AIDS in Africa, Watkins and Swidler (Citation2013) have argued that institutional change not only occurs because a novel technology works better in the sense intended by dominant actors, or because some actors are able to impose their institutions and technologies because of their superior capital and power. Instead, ‘institutional capacities created for one purpose may be animated by new purposes and may serve new interests’ (Watkins & Swidler, Citation2013, p. 213, see also Burchardt, Citation2013). This is especially likely to happen when actors with divergent interests and agendas gather around shared symbols and themes. Actors may have different understandings of such symbols and, in this sense, misunderstand each other when using them. But, nonetheless, using these symbols works such that misunderstandings become ‘working misunderstandings’ (Watkins & Swidler, Citation2013, p. 197). We argue that the terms saving lives, and especially emergencies operate precisely in such ways.
In a similar vein, in STS scholarship Star and Griesemer (Citation1989) have introduced the term boundary object to explore the conditions that enable coordination. They defined boundary objects ‘objects which are both plastic enough to adapt to local needs and constraints of the several parties employing them, yet robust enough to maintain a common identity across sites’ (Star & Griesemer, Citation1989, p. 393). As we show, in Ghana's drone field emergencies operate and are framed as objects in that sense, enabling the consolidation of drone deliveries precisely because of the plasticity and malleability of their definition across different sites.
The rest of the article is structured as follows: in the following section, we briefly explain our methodology. After that, we present our findings, beginning with an analysis of the ideas of saving lives and emergency. Subsequently, we demonstrate how these ideas began operating as ‘symbols’ that unite divergent agendas and interests (Watkins & Swidler, Citation2013, p. 204) and boundary objects (Star & Griesemer, Citation1989). Under the header ‘Stock-out: Inheriting a System’ we show how these dynamics play out in the field of blood supply. In the conclusions, we specify how our findings contribute to theories of social and technological change.
Methodology
Methodologically, the article is based on ethnographic research in different regions of Ghana carried out between 2020 and 2022. In particular, the article draws on our ethnographic fieldwork in the key sites of health logistics. We visited the national offices of the Ghana Health Service and National Blood Services Ghana in Accra, interviewing leading figures and national decision-makers. We also collected data at the regional medical stores in Kofuridua and Tamale where medical products are stored and distributed to health facilities, talking to their directors, dispatchers and fulfilment managers. Here, we interviewed the directors as well as those responsible for the distribution of goods to the health facilities. In addition, we did ethnographic research in Zipline's distribution centres in Omenako and Vobsi, exploring the ways in which personnel handled, managed and prioritised incoming orders.Footnote4 Our data interpretation led us, first, to the identification of divergent narratives about the use of drone and ordering practices, and, second, to the identification of those symbols and understandings that allows the system to work the way it does.
The idea of emergency and ‘saving lives’
From the very beginning, the idea that Zipline's drones ‘save lives’ was an essential element of the discourses through which the company branded its products and exhorted their benefits to African governments, and the way governments, in their turn, promoted their support of drone logistics to their citizens and constituencies. In 2005, Zipline's CEO boldly declared that his mission was to ‘put every human on the planet within a 15- to 30-minute delivery of any essential medical product’.Footnote5 In a similar vein, after signing an agreement with Zipline in early 2021 for the delivery of COVID-19 vaccines, the government of the northern Nigerian state of Kaduna stated that drones ‘will revolutionize access and availability of critical and lifesaving medicines for millions of people’.Footnote6 While clearly resonating with neo-colonial tropes of the white saviour (Mathers, Citation2022), this emphasis on ‘saving lives’ had several ramifications: it was meant to provide a sense of urgency, mobilise political will, and convince policy-and decision-makers that technological fixes existed and just had to be implemented; it sought to aid the rebranding of drones, shifting popular understandings from military to civil and humanitarian uses; and it was important in opening up African skies to Western tech companies who were in need of the flight data necessary to convince regulators in the US and Europe that the technology was foolproof (Umlauf & Burchardt, Citation2022). As a field of intervention, health was thus construed as the common denominator that helped to align moral agendas (‘saving lives’), market imperatives (i.e. becoming profitable) and safety concerns with one another.
However, the idea that drones ‘save lives’ also found its way into the self-understanding and everyday discourses of Zipline's employees. When we talked to Anthony, an electrical engineer at Vobsi in the Northern region, about maintaining the launcher and the drones, he explained: ‘When you are doing checks on the Zip, because it's flying to go and save a life, don't just do rapid checks on it, you have to ensure that you follow the SOP [standard operational procedures]’. Curiously, he used that phrase although, as we explore in greater detail below, only a marginal share of all deliveries actually save lives in the narrow sense of the word. In addition, the logo on all Zipline vehicles pictures the silhouette of a drone dropping a package on a parachute with the line ‘Life-saving deliveries by drone’ right next to it (see ). In the event, however, in most cases, drones transported products such as cough syrup, paracetamol or hand sanitiser to health facilities. How does it happen that, once these items had been transported by drones through a technologically complex, digitally driven system of autonomous aviation, they are transformed into live-saving objects?
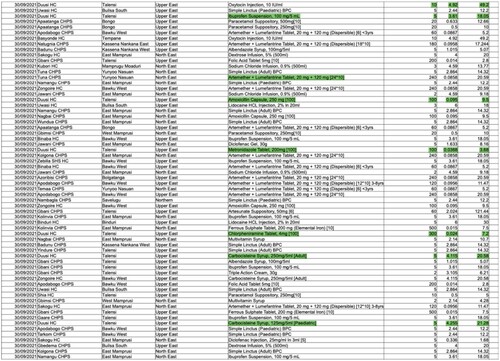
Figure 1. Screenshot from the September 2021 delivery list Zipline sends to health authorities in the district and regions.
To answer this question, it was useful to follow these objects ethnographically as they travelled to regional medical stores and from there to Zipline's distribution centres, where they were packed into the drones and sent to far-flung clinics. The argument is not that cough syrup and hand sanitisers do not have the potential to save lives, but rather that categorising medical equipment and mundane medical products as ‘lifesaving’ means projecting potentialities onto routine cases. There are highly fine-grained but important differences between the overly dramatic instances advertised by Zipline (‘A patient's life was saved through blood delivery’), routine healthcare delivery, based on what is usually perceived as an emergency case (‘life-threatening condition requiring immediate attention’) and scenarios simply involving the lack of a medical product.
In October 2021, we first visited the regional medical store (RMS) of the Eastern Region and interviewed the staff working there. The next day, we moved on to one of Zipline's Ghanaian distribution centres. In entering the fulfilment centre, the contrast was dramatic, and the atmosphere appeared both utopian and outlandish. Compared to the humid, hot and tropical environment of the RMS, the entire premises were aseptic, clean, transparent and heavily air-conditioned. Employees walked across the shiny bluish floor to clean shelves, which were often half empty. The employees told us that medical products such as antimalarials, paracetamol and antibiotics had been placed on the shelves manually and marked with a bar code for reasons of accountability. Obviously, each item had been stored with dedication and care, making the shelves appear like display cabinets, and humans and machines appeared as if they were seamlessly connected to one another.
In the RMS warehouse, by contrast, massive piles of boxes, bags and folders were stacked one on top of the other, waiting to be registered and dispatched. These two very different images of medical supply-chain management highlight the conditions under which such contrasting treatments are possible, namely bulk and scale. The sheer volume of medical products passing through the RMS warehouse makes temporary storage a messy logistical endeavour. The RMS not only had to coordinate three to four supply cycles per year and to account for the delivery and distribution of essential drugs for several thousand health facilities a year in the region. It also had to handle the transition to the so-called last-mile delivery system, which in most regions is carried out by a private company. Before last-mile delivery was in introduced in Ghana in 2017, all health facilities were required to send their own vehicles to pick up their entire medical supply at the RMS warehouse. In this regard, the quantity of medical products delivered through Zipline's drones appeared quite negligible.
For Zipline, of course, it was essential to prove that their technology was safe and trustworthy, and to fulfil the promise that once the bottleneck of health logistics had been addressed lives would be saved. To that end, they had developed their own emergency plan at an operational level. For Zipline's engineers and employees, the notion of emergency services chiefly translated into technical requirements, especially by introducing technical redundancies ensuring that, if one part of a machine or process broke down or did not function properly, another piece would take over. For instance, if one propeller broke during a mission, a second one could jump in. If this part also failed, the machine automatically pulled a parachute that brought it down slowly in order to avoid damage and harm to people and property. Operating in low-resource settings, Zipline had developed an awareness of frequent disruptions of essential infrastructure such as the electricity or mobile networks on which their drones crucially relied. Zipline was eager to give the impression that emergency and preparedness had become part of the company's self-understanding. Proving itself able to operate in harsh environments (e.g. in terms of the weather), but also in infrastructurally weak and unreliable settings was especially linked to the fact that the company sought to convince American media, investors and regulators that their concept would safely work on US territory. As one of Zipline's senior employees told us:
So, our philosophy is both to strive to create technology and systems that have as close to our goals at 100 percent uptime across the board, whether it's electricity, whether it's Telecom, whether it's staff, whether it's, you name it, our equipment, just being well maintained and not breaking, whether that's the zip or the fridges, and whatever. So, our goal is as a system to have 100 percent uptime.
For electricity, for example, all of our systems are on the grid, but they also have a backup generator. […] And so critical items are backed into the UPS [Uninterruptable Power Supply, authors]. We are also monitoring everything. Or, for example, on the fulfilment side, our most critical equipment is the storage equipment, and temperature management. So, we also have monitoring of all of that. So, if for whatever reason - and to my knowledge, this has never happened where both the UPS and the generator have failed - but if it were to happen, we’d have the sensors go off right away. And then the fourth thing we’re investigating using phase change material, which basically can maintain the temperature and use that to line the shelving. So that it can extend the longevity of the temperature, assuming the fridges are unplugged. In Nigeria, where we will be expanding, we will be launching there very shortly, I believe that they’ve looked into solar panels.
At this point, 25 million people depend on us with their lives and the lives of their kids. That will be 40 million by the end of the year. That's a huge responsibility, and everyone here takes it very seriously.
However, we also observed and were intrigued by a set of contradictions: health professionals whom we had interviewed and who were critical of drone logistics argued that drone infrastructure only addressed a marginal section of deliveries because its use was limited to medical emergencies. As only a small portion of all healthcare facilities have the technical equipment and human resources to perform emergency interventions, in their eyes the small number of medical emergencies did not justify the financial investment in drone infrastructure. At the same time, pharmacists and stock managers appeared to make frequent use of drone deliveries for all sorts of purposes. This raises questions as to how these different purposes for using drones were justified and how drone infrastructure began to compete with land transport. As we show in the following section, what enabled pharmacists to demand drone deliveries for what was little more than regular replenishment, routine resupply or scheduled deliveries were – among other things – creative interpretations, manipulations, or circumventions of the notion of emergency.
Non-emergencies and parallel supply chains
Researcher: “So do you only order at the point of emergencies?”
Pharmacist: “No! We order when we have a stock-out!” Kukurantumi CHPS
In one of Zipline's more frequently used distribution centres, operators manage roughly 4000 flights per month. As indicated in , the company lists all the information, starting from the date of delivery, the name of the facility, the district, the region, the drug that was ordered and the quantity delivered, and ending with a list of the costs. Our research showed that approximately 80% of the monthly deliveries can be considered non-emergency deliveries. Among these deliveries are drugs such as antimalarials (approx. 25%), cough medication (approx. 15%), pain medication (approx. 15%) and antibiotics (approx. 15%). Thus, more than 70% of the deliveries account for these five categories of drugs, which form part of routine primary healthcare services. In turn, fewer than 10% of the deliveries are carried out for clear emergency interventions.Footnote7 Yet, when we asked stock managers at the RMS and Zipline's distributions centre, as well as pharmacists at the health facilities, how emergencies were actually defined, and who was to decide authoritatively whether a delivery was an emergency delivery or not, understandings clearly differed. Some pharmacists suggested that situations in which they were out of stock of certain drugs qualified as emergency. Others would answer that such definitions should not be too rigid, that context always mattered and that the negative, mid-term consequences of the failure to administer a certain drug due to it not being in stock would also allow them to place drone orders. Thus, some pharmacists argued, as soon as a particular medication was out of stock, this constituted a supply emergency regardless of whether it concerned simple painkillers or strong broadband antibiotics. While definitions varied greatly among our interlocutors, only deliveries of blood (<5%), oxytocin (approx. 3%) and anti-snake venom (approx. 0.05%) could be counted as medical emergencies in the narrower sense. In some conversations, we were also told that it was the responsibility of Zipline's pharmacists to check whether an incoming order was an emergency or not.
Such categorisations of incoming orders were indeed critical in several ways. First, sometimes fulfilment managers at the distribution centres had to handle several orders within a short period of time and were thus forced to prioritise. An order categorised as an emergency would immediately move to the top of the order list and be treated as priority. But again, in spite of the clear practical relevance of definitions of emergency for their work, Zipline's employees argued that there was no unified understanding. Second, because of the rapidly accelerating use of Zipline among facility-based pharmacists in northern Ghana, regional health directorates limited the maximum number of orders through drones per month. The main reason for this was that the massive use led to repeatedly stock-outs at the distribution centres, further complicating the supply relations between the RMS and Zipline (we return to this point below). More dramatically still, some health facilities already used up the drone orders available to them during the first days of the month for all sorts of non-urgent purposes. That would mean that they would sometimes be unable to place drone orders in the case of a ‘real emergency’ if it occurred later in the month. In 2022, the health directorate of the Upper East region even created a blacklist of health facilities that would be banned from using drone infrastructure because of their alleged misuse of the system.
Checking the supply list, one senior manager at the RMS commented to us as follows:
But ACT, artemether-lumefantrine anti-malaria, ibuprofen suspension, amoxycillin capsules – […] metronidazole tablet, these are clearly not emergencies! And to me, we must begin to look at it because we don't want to create a parallel supply chain. The Regional Medical Stores are undertaking what you call the last-mile distribution. So, we try to distribute to the last mile, as the name suggests, and these are routine commodities. Carbocysteine that they can have for cough mixtures. Chlorpheniramine is a Piriton metronidazole, amoxycillin, these are routine pharmaceuticals. […] But actually, calling on Zipline to be delivering this to them, I mean, Piriton! Can you tell him Piriton is an emergency? No! So, these are some of the challenges. If this continues, we begin to see a parallel supply chain going, and that is a very dangerous one for the country.
As mentioned above, most pharmacists in rural health facilities were impressed by Zipline's performance. By contrast, some facility-based pharmacists who approach issues around logistics on a more practical level were also critical of developments that the introduction of Zipline engendered but that were not made explicit. In the following interview transcript, one healthcare worker reflected on the new temporalities that were introduced through Zipline:
Pharmacist: “Well for me, if Regional Medical Stores is consistent, Zipline is just delaying the delivery of medication.”
Researcher: “Delaying? How?”
Pharmacist: “Anti-snake venoms could have been brought to the hospital, and when there is a snakebite case you pick and dispense, not wait for the drone to fly and come. I think the delivery time is 20 to 30 minutes or so. Yes, Zipline is doing well, that we admit. But when Zipline was not there, how was the medicine brought in? They would bring it in in bulk. Let's say a hundred, they would be in the hospital, and then we managed that over time.”
Researcher: “Are you trying to say that because of Zipline some of the products are no longer sent directly?”
Pharmacist: “Good! Exactly, that is what I am saying.”
Another concern among nurses and other health professionals was that, if done several times per day, ordering itself (through WhatsApp or phone calls) was turning into an additional, time-consuming task that was added to their work schedule. The same applies to collecting the deliveries and handling the bills. In many of our interviews with healthcare workers, especially facility managers, issues of human resources played a major role. As one nurse at the Gimbsi facility desperately argued:
Consider the number of requests: you request a drug, a syrup etc., and then the maximum they can give you a day is five, which I think is very very low. The quantity is actually low, it is very very little. Zipline should really do something about that.
Stock-outs: Inheriting a system
In policy discourses, the main rationale for the introduction of drone infrastructure was that the bottleneck of providing high-quality healthcare to Ghanaians was in fact a matter of medical logistics. As we now demonstrate, in practice such discourses served to make the far-reaching shortages of medicines and pharmaceuticals of all kinds invisible. This shortage manifests itself in chronic ‘stock-outs’ (i.e. stock running out) on all levels of the supply chain, from the local health centre up to the national medical stores. In this context, the excessive use of drone deliveries by local healthcare personnel in northern Ghana led to frequent stock-outs in Zipline's distributions centres. Somehow, therefore it merely shifted the problem of stock-outs from the regional medical stores to Zipline's aseptic fridges as the new logistical intermediaries. More importantly, these stock-outs dramatically revealed what some of our local interlocutors – stock managers and pharmacists – assumed all along: that in reality the bottleneck on the way to achieving universal health coverage lay elsewhere.
Problems of supply in terms of availability were even compounded in the field of blood products – one of Zipline's main assignments. Unlike pharmaceuticals, blood products need to undergo complex procedures of matching and screening, require technological equipment and cannot be produced industrially. As we now show, this introduced a range of particular challenges.
Blood Manager: “We hardly request blood … It was September 15th, that was the last time we requested [it]. We made request: ‘Good evening. Urgent need of 0 negative!’ And Zipline responded: ‘Good evening, sir. Sorry we are out of stock at the moment! We will notify you as soon as we restock! Thank you!’”
Researcher: “Did they notify you?”
Blood Manager: “No. No, I did not see any notification!”
Despite Zipline's far-reaching efforts to free themselves from the uncertainties they encountered in their technical and infrastructural environment, the weaknesses and shortages within Ghana's national blood-supply services ended up hampering effective drone deliveries.Footnote8 During our visits to Zipline's distribution centres, we were surprised to find expensive state-of-the-art refrigerators set aside for blood storage almost empty. In one centre, we found only about six bags of the most common blood types (0+, A +). According to the pharmacist, they had difficulty getting resupplied because they relied on supplies from the national blood services in Accra and Kumasi. At the headquarters of the national blood service in Accra, we were told that this was mainly a result of the COVID-19 pandemic, which had made people more reluctant and hesitant to donate. The drop in the number of donors since the onset of the pandemic was observed around the world.Footnote9 In the case mentioned above of a request for 0- blood, the likelihood of Zipline having such a rare blood type in stock would also have been rather low, even under more ordinary circumstances before the onset of the pandemic.
Yet the example also shows that there is an unevenness in the levels of redundancies with which Zipline must operate. The segment in the supply chain, which Zipline serves, appears to be the least challenging part. Their task does not involve the recruitment and mobilisation of blood donors, nor are they involved in the technicalities of screening full blood or preparing blood components. And finally, Zipline is also not involved in the cross-matching between blood donors and recipients. The intermediate position in which Zipline finds itself consists mainly of storing, monitoring temperatures and maintain the fridges. For a trained pharmacist at Zipline's distribution centres, this task is hardly a challenge.Footnote10 In an effort to explain the technical procedures involved in the acquisition, storage, and administration of blood in individual hospitals, in an interview Zipline's CEO described the situation as follows:
Fifty percent of that is going to moms who are suffering from post-partum haemorrhaging and 30 percent is going to kids under the age of five who suffer from severe anaemia due to malaria. This is really important, it's a complete emergency. Someone's life is on the line when you need one of these products! But it is very difficult to stock these products reliably because you have red blood cells, platelets, plasma, you need all three, they all have different storage requirements, different shelf lives. And with red blood cells [full blood] you’ve got eight different types, A, B, AB and O and positive and negative Rh factor of each. So, it's basically an impossible logistical challenge, and so what's so great about this is that it allows them to go from trying to make these impossible predictions of what's needed, where to keep the blood in one place and send it when you have a patient whose life is in danger. It's a vast simplification of the supply chain.
In our conversation, the regional hospital's blood manager explained their relations with Zipline, telling us how her unit would usually engage in community mobilisations in order to recruit and collect voluntary blood donations. During these so-called blood drives, her team would visit boarding schools or vocational training centres, give health education to students, and then collect some voluntary blood donations. During a recent visit to one of the local vocational training schools, the manager discovered that the school had already donated some blood. To her surprise, she learned that ‘people from Zipline’ had visited the school to collect blood in the name of the national blood services the week before. When she learned about this, she was angry that Zipline had intruded into their recruitment area, in which they had built up trust with the school authorities and local communities, whom they had mobilised to secure a reliable blood supply for their facility.
Talking to Zipline about this incident, they admitted that from a certain point, and in order to cope with the shortages of blood, they indeed engaged in blood collection campaigns to support the national blood services. As the statement indicates – but was also reiterated several times during the interview – the blood manager explained that they usually do not use Zipline's services when it comes to blood. They manage well themselves, being able to collect just enough blood to sustain their demand at the hospital.
There is thus an ironic twist in the implementation of Zipline's blood-related emergency services. In their many public media appearances, Zipline never openly mentioned the existence of local blood donation activities or the practice of replacement donations. Both activities grant hospitals flexibility and greater independence from unreliable national blood services. Whether consciously or not, Zipline's efforts to assist the national blood services produced tensions with the very local blood supply practices that allowed hospitals to operate largely autonomously regarding this precious commodity. The patient mentioned earlier for whom 0 blood was requested survived. In cases of rarer blood types, the hospital kept a list of local individuals whose blood type is known. In emergencies these individuals were called and asked if they could come and donate blood, promising that their costs would be covered.
Conclusions
As we showed, the definition of medical logistics as the bottleneck of quality healthcare in Ghana that Zipline promoted and the introduction of their drone infrastructures led to a series of paradoxes: First, while drones were meant to improve access to life-saving products such as blood in medical emergencies, we found that blood was often out of stock in Zipline's distribution centres. Second, whereas drones were expressly not meant for the routine re-supplies of medical products, this has become their dominant purpose. Third, while in many ways rational from the facilities’ point of view, such usage risks undermining the existing supply-chain management. It has created the kind of parallel system that, according to high-level health professionals, should be avoided at all costs. Drone deliveries are only cost-effective when used in ways that go against the contractual agreements, which holds true for both Zipline and the Ghanaian state.
This, of course, raises important questions about the ambivalent role and responsibility of the developmental state in projects of infrastructural innovation. Many of the involved actors appear to do what they can to make the system work. And they do so, chiefly, by creating and creatively manipulating notions of saving lives and emergencies as symbols and boundary objects. But there are also limits to their capacities to do so, arising from the large degree of autonomy the Ghanaian state afforded Zipline and the particular interests of sections of Ghana's digitisation elites.
In their work, Star and Griesemer (Citation1989) mainly used the term boundary objects as a solution to problems actors encountered in communicating across different epistemological backgrounds. With our article, by contrast, we demonstrated how boundary objects solve problems but also introduce new ones. Stretching the definition of emergency allowed local healthcare workers to use drone infrastructures but it also highlighted the contingency of the definition of where the bottleneck really lay.
Finally, and most importantly, the very success of the system and the excessive ordering by the stock managers at health facilities have led to frequent stock-outs at Zipline's distribution centres. It has thus not only shifted stock-out problems from the regional medical stores to Zipline's centres but also altered perceptions of where the bottleneck in Ghanaian healthcare really lies. Discourses around digital logistics suggested that access to healthcare is primarily about bringing medical products to patients. Yet by causing stock-outs, the solution to the logistical problem, however partial, has made visible the sheer lack of medicines and pharmaceuticals. As a pharmacist in one of Zipline's distribution centres lamented: ‘Often, there is just nothing we can send them’. This lack is, of course, a product not only of Africa's marginalisation in the global economy and unfavourable manufacturing conditions but also of the lack of governmental investments in the pharmaceutical sector and research, organisational deficiencies, and often massive corruption in medical procurement processes: What is lacking, has sometimes simply been stolen along the medical supply chain.
We suggest that future research pay more attention to these gaps between the promises and outcomes of digital innovation in medical logistics and the paradoxes that emerge from their implementation. Both, studies on infrastructural leapfrogging and on healthcare infrastructures can benefit from focusing more explicitly on the multifarious mechanisms through which bottlenecks are defined, including symbols and boundary objects, how such definitions shift, as well as to the consequences they have on access to healthcare on the ground.
Information on ethical approval
The study was approved by the Ghana Health Service Ethics Committee (GHS-ERC 009/08/21) on 11 October 2021 and complies with Ghanaian legislation. After being informed about study purposes and data management procedures, interviewees have given written consent to being interviewed and, when done, to the recording of the interviews.
Supplemental Material
Download MS Word (35 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
2 ‘Fly-To-Save-A-Life Project complementary to the existing health system:’ see https://www.moh.gov.gh/fly-to-save-a-life-project-complementary-to-the-existing-health-system/
4 Due to the COVID-19 pandemic, we could gather only some of the data ourselves. We wish to highlight the contributions to this article of John Ganle of the University of Ghana. In addition, we also thank Kim Chung and Edwin Ameso, both of Leipzig University.
5 See https://www.bbc.co.uk/sounds/play/w3ct03pq, accessed 23 March 2021.
6 See https://www.urbanairmobilitynews.com/medical-pharmaceutical-transport/zipline-to-deliver-covid-19-vaccines-in-nigerian-state-kaduna/?utm_source=rss&utm_medium=rss&utm_campaign=zipline-to-deliver-covid-19-vaccines-in-nigerian-state-kaduna, accessed 01 March 2021. On this point, see Euchi (Citation2021).
7 We have no reliable information on the number of blood deliveries. According to our estimates, it is likely to be less than a hundred units of blood a month. In addition, vaccine deliveries are also made via Zipline, but adhering to a fixed schedule on days when facilities have scheduled their immunization days.
8 Stock-outs also affect Zipline's deliveries of essential medicines. Many interviewees confirmed that this happens quite frequently, as the following examples indicate: ‘Back to Zipline has there been the case when you called on them and they also didn't have it?’ ‘A lot … a lot!’ ‘So, in those times, when you need the product, what happens?’ ‘Ahh, we all have to go to the streets like that, the patient will have to look for that;’ or also: ‘Ah well, on a normal day you can get 60 to 65% of the medication.’
9 See https://www.afro.who.int/news/drop-blood-donations-add-maternal-health-threats-africa, accessed 14 April 2023.
10 However, one of the main tasks at the facilities seems to be monitoring the redundancy system the company has put in place.
References
- Beisel, U. (2014, October 6). On gloves, rubber and the spatio-temporal logics of global health. Somatosphere, http://somatosphere.net/2014/10/rubber-gloves-global-health.html.
- Biehl, J. (2016). Theorizing global health. Medicine Anthropology Theory, 3(2), 127–142. https://doi.org/10.17157/mat.3.2.434
- Biesma, R. G., Brugha, R., Harmer, A., Walsh, A., Spicer, N., & Walt, G. (2009). The effects of global health initiatives on country health systems: A review of the evidence from HIV/AIDS control. Health Policy and Planning, 24(4), 239–252.
- Burchardt, M. (2013). Faith-based humanitarianism: Organizational change and everyday meanings in South Africa. Sociology of Religion, 74(1), 30–55. https://doi.org/10.1093/socrel/srs068
- Burchardt, M., & Umlauf, R. (2023). Dreams and realities of infrastructural leapfrogging: Airspace, drone corridors, and logistics in African healthcare. In M. Burchardt & D. van Laak (Eds.), Making spaces through infrastructure (pp. 221–240). De Gruyter.
- Collier, S., & Lakoff, A. (2008). The problem of securing health. In A. Lakoff & S. Collier (Eds.), Biosecurity interventions: Global health and security questions (pp. 7–32). Columbia University Press.
- Dilger, H., & Mattes, D. (2018). Im/mobilities and dis/connectivities in medical globalisation: How global is global health? Global Public Health, 13(3), 265–275. https://doi.org/10.1080/17441692.2017.1414285
- Euchi, J. (2021). Do drones have a realistic place in a pandemic fight for delivering medical supplies in healthcare systems problems? Chinese Journal of Aeronautics, 34(2), 182–190. https://doi.org/10.1016/j.cja.2020.06.006
- Friederici, N., Wahome, M., & Graham, M. (2020). Digital entrepreneurship in Africa: How a continent is escaping Silicon Valley's long shadow. The MIT Press.
- Heeks, R. (2022). Digital inequality beyond the digital divide: Conceptualizing adverse digital incorporation in the global south. Information Technology for Development, 28(4), 688–704. https://doi.org/10.1080/02681102.2022.2068492
- Hsia, R., Razzak, J., Tsai, A. C., & Hirshon, J. M. (2010). Placing emergency care on the global agenda. Annals of Emergency Medicine, 56(2), 142–149. https://doi.org/10.1016/j.annemergmed.2010.01.013
- Kelly, A., & Beisel, U. (2011). Neglected malarias: The frontlines and back alleys of global health. BioSocieties, 6(1), 71–87. https://doi.org/10.1057/biosoc.2010.42
- Krieg, L. J., Berning, M., & Hardon, A. (2017). Anthropology with algorithms? Medicine Anthropology Theory, 4(3), 21–52. https://doi.org/10.17157/mat.4.3.458
- Langley, P., & Leyshon, A. (2022). Neo-colonial credit: FinTech platforms in Africa. Journal of Cultural Economy, 15(4), 401–415. https://doi.org/10.1080/17530350.2022.2028652
- Lupton, D. (2014). Critical perspectives on digital health technologies. Sociology Compass, 8(12), 1344–1359. https://doi.org/10.1111/soc4.12226
- Lupton, D. (2017). Digital health: Critical and cross-disciplinary perspectives. Routledge.
- Mathers, K. (2022). White saviorism and popular culture: Imagined Africa as a space for American salvation. Routledge.
- Mawere, M., & van Stam, G. (2020). Digital health, technology, and digital diplomacy: African solutions for African challenges. Journal of Sustainable Development in Africa, 22(1), 35–45.
- Miller, D., & Horst, H. A. (2020). The digital and the human: A prospectus for digital anthropology. In H. Geismar & H. Knox (Eds.), Digital anthropology (pp. 3–35). Routledge.
- Morozov, E. (2013). To save everything, click here: The folly of technological solutionism. PublicAffairs.
- Neumark, T., & Prince, R. J. (2021). Digital health in East Africa: Innovation, experimentation and the market. Global Policy, 12(6), 65–74. https://doi.org/10.1111/1758-5899.12990
- Nguyen, V.-K. (2009). Government-by-exception: Enrolment and experimentality in mass HIV treatment programmes in Africa. Social Theory & Health, 7(3), 196–217. https://doi.org/10.1057/sth.2009.12
- Ong, A., & Collier, S. (eds.) (2007). Global assemblages. Technology, politics and ethics as anthropological problems. Duke.
- Park, S.-J. (2012). Stock-outs in global health: Pharmaceutical governance and uncertainties in the global supply of ARVs in Uganda. In R. Rottenburg, W. Geissler, & J. Zenker (Eds.), Rethinking biomedicine and governance in Africa (pp. 122–140). Transcript Verlag.
- Plantin, J. C., Lagoze, C., Edwards, P. N., & Sandvig, C. (2018). Infrastructure studies meet platform studies in the age of Google and Facebook. New Media & Society, 20(1), 293–310. https://doi.org/10.1177/1461444816661553
- Plantin, J. C., & Punathambekar, A. (2019). Digital media infrastructures: Pipes, platforms, and politics. Media, Culture & Society, 41(2), 163–174. https://doi.org/10.1177/0163443718818376
- Poggiali, L. (2016). Seeing (from) digital peripheries: Technology and transparency in Kenya’s silicon savannah. Cultural Anthropology, 31(3), 387–411. https://doi.org/10.14506/ca31.3.07
- Pollock, A. (2019). Synthesizing hope: Matter, knowledge, and place in South African drug discovery. University of Chicago Press.
- Ruckenstein, M., & Schüll, N. D. (2017). The datafication of health. Annual Review of Anthropology, 46(1), 261–278. https://doi.org/10.1146/annurev-anthro-102116-041244
- Star, S. L., & Griesemer, J. R. (1989). Institutional ecology, translations’ and boundary objects: Amateurs and professionals in Berkeley’s Museum of Vertebrate Zoology, 1907-39. Social Studies of Science, 19(3), 387–420. https://doi.org/10.1177/030631289019003001
- Storeng, K. T., Fukuda-Parr, S., Mahajan, M., & Venkatapuram, S. (2021). Digital technology and the political determinants of health inequities: Special issue introduction. Global Policy, 12(S6), 5–11. https://doi.org/10.1111/1758-5899.13001
- Thiel, A. (2020). Biometric identification technologies and the Ghanaian ‘data revolution’. Journal of Modern African Studies, 58(1), 115–136. https://doi.org/10.1017/S0022278X19000600
- Thorat, D. (2020). Digital infrastructures and technoutopian fantasies: The colonial roots of technology aid in the global south. In M. Dodd & N. Kalra (Eds.), Exploring digital humanities in India (pp. 17–30). Routledge.
- Umlauf, R. (2017). Precarity and preparedness: Non-adherence as institutional work in diagnosing and treating malaria in Uganda. Medical Anthropology, 36(5), 449–463. https://doi.org/10.1080/01459740.2017.1318282
- Umlauf, R., & Burchardt, M. (2022). Infrastructure-as-a-service: Empty skies, bad roads, and the rise of cargo drones. Environment and Planning A: Economy and Space, 54(8), 1489–1509. https://doi.org/10.1177/0308518X221118915
- Van Dijck, J., Poell, T., & De Waal, M. (2018). The platform society: Public values in a connective world. Oxford University Press.
- Von Schnitzler, A. (2018). Democracy’s infrastructure: Techno-politics and citizenship after apartheid. In Princeton studies in culture and technology. Princeton University Press.
- Watkins, S. C., & Swidler, A. (2013). Working misunderstandings: Donors, brokers, and villagers in Africa’s AIDS industry. Population and Development Review, 38(s1), 197–218. https://doi.org/10.1111/j.1728-4457.2013.00560.x
