Abstract
Background The coronal alignment of the lower limb is important for knee reconstruction procedures. However, normal alignment is hard to define because of its wide variation among normal individuals. Our hypothesis was that the variation in the normal anatomy as assessed by radiography is greater than commonly accepted.
Methods We performed anteroposterior long-leg radiographs on 100 Caucasian patients without any known knee abnormality, to determinate the femorotibial angle, coronal orientation of the distal femoral condyles, and coronal orientation of the proximal tibial condyles. All measurements were performed by the same experienced knee surgeon.
Result The mean values observed were close to the values commonly described in the Caucasian population. However, only 15–20% of the cases met the mean values of Moreland et al. (1987) for the individual items, and only 2 cases had the exact normal values. There was a wide variation for all angles measured, with a standard deviation higher than the mean value.
Interpretation The variation in the lower limb axes is wider than commonly believed. There is a need for individual knee reconstruction which takes the specific knee axes of the patient to be operated into account.
The coronal alignment of the lower limb is important for some surgical procedures such as knee osteotomies and knee prostheses. It is then mandatory to know the normal coronal alignment of the lower limb. However, normal alignment is hard to define because of its wide variation among normal individuals. It is generally accepted that the normal angle between the mechanical axes of the femur and of the tibia is 0°, with a valgus inclination of the distal femur of 3° and varus inclination of the proximal tibia of 3°, as described by Moreland et al. (Citation1987). However, that particular study reported only 25 cases, and the small number of measurements may have concealed a wide degree of variation around the mean values. Few other studies have focused on this topic (Hsu et al. Citation1990, Tang et al. Citation2000). We thus analyzed the variation of the relevant axes of the lower limb in a normal Caucasian population.
Patients and methods
We selected patients operated on at our institution for upper limb pathology, and without any known lower limb pathology. There were 69 men and 31 women with a mean age of 39 (17–62) years. All selected patients gave their informed consent before entry into the study.
A long-leg anteroposterior radiograph of one randomly chosen lower limb was performed with a consistent technique: unipodal support, pelvis in the true anteroposterior direction, full knee extension, and the foot oriented according to the gait angle. The X-ray source was located 2.5 m from the film. As a quality control, the patella should be projected in the middle of the femoral condyles. To ensure homogeneity, all measurements were made by the same experienced knee surgeon (CB).
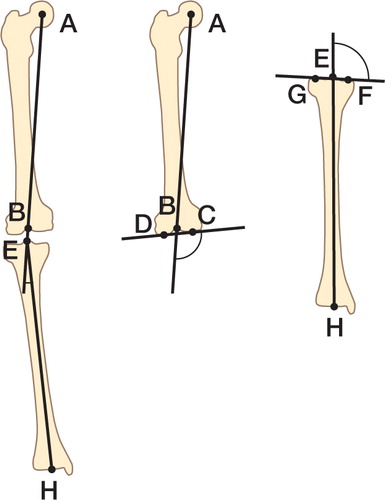
The following points were marked on the radiographs: A, center of the femoral head (concentric circles technique); B, center of the femoral condyles (highest point of the intercondylar notch); C, lowest point of the medial femoral condyle; D, lowest point of the lateral femoral condyle; E, center of the tibial condyles (middle of both tibial spines); F, lowest point of the medial tibial condyle; G, lowest point of the lateral tibial condyle; and H, center of the ankle joint (lowest point of the tibial plafond).
The axes were determined as follows: mechanical femoral axis, line AB; bicondylar femoral axis, line CD; anatomical tibial axis, line EH; and the bicondylar tibial axis, line FG. The following angles were measured according to these axes () using a manual goniometer: the femorotibial angle, axes AB/EH (the angle was considered positive in case of varus deformation); the distal femoral angle, axes AB/CD; and the proximal tibial angle, axes EH/FG.
Coronal orientation of the distal femur was defined as distal femoral angle – 90°; a varus orientation was considered positive. Coronal orientation of the proximal femur was defined as proximal tibial angle – 90°; a varus orientation was considered positive. The following angles were considered “normal”: 0° for femorotibial angle, –3° for coronal orientation of the distal femur, and 3° for coronal orientation of the proximal tibia.
We analyzed all angles with conventional descriptive statistics (mean, standard deviation, 95% confidence interval (CI), median). The normality of the distribution was tested by the Shapiro-Wilk test. The correlation between the coronal orientation of the distal femur and of the proximal tibia for each patient was studied with regression analysis. Influence of age was studied using regression analysis. Influence of sex was studied with Student’s t-test. All tests were performed with a level of significance of 0.05.
Results
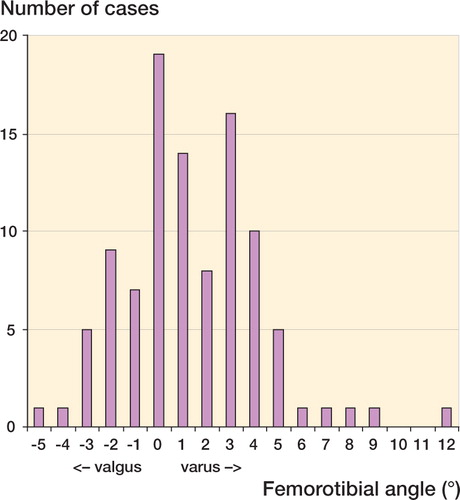
The mean femorotibial angle () was 1.4° (SD 2.8; range: –5 to 12°; 95% CI: -3.5 to 8.5°); median value was 1°. 19 cases had an angle of 0°. 57 cases had an angle between –2° and 2°. The Shapiro-Wilk test showed a distribution that was not normal (p = 0.005).
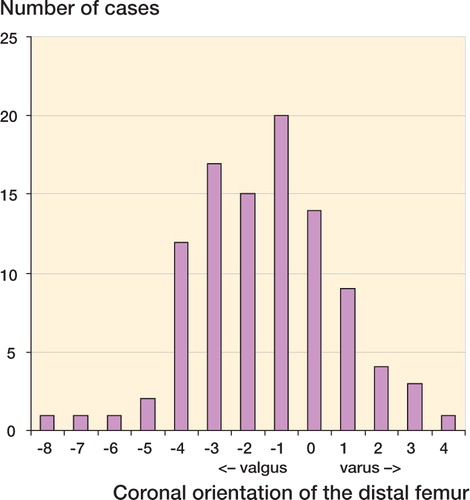
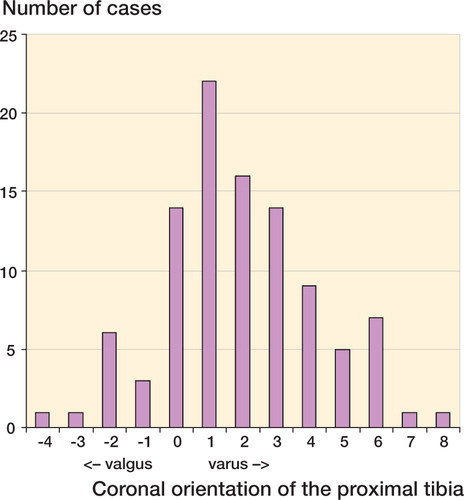
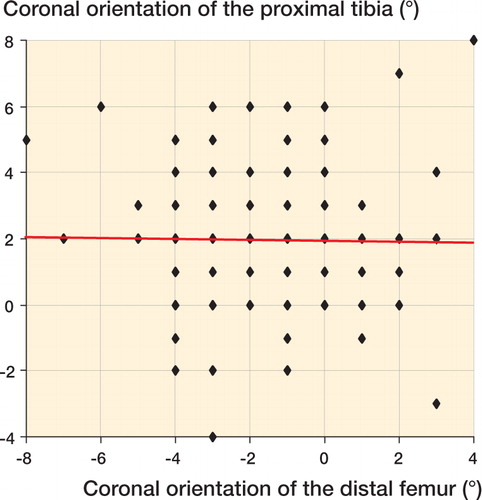
The mean coronal orientation of the distal femur () was –1.5°, (SD 2.2; range: –4 to 8°; 95% CI: -6.5 to 3.0°); median value was –1°. 17 cases had an angle of –3°. 66 cases had an angle between –2° and 2°. The Shapiro-Wilk test showed a normal distribution (p = 0.06). The mean coronal orientation of the proximal tibia () was 1.9° (SD 2.3; range: –4 to 8°; 95% CI: -2.5 to 6.5°); median value was 2°. 14 cases had an angle of 3°. 66 cases had an angle between –2° and 2°. The Shapiro-Wilk test showed a non-normal distribution (p = 0.05).
No case met all “normal” criteria. Only 2 cases had both a –3° coronal orientation of the distal femur and a 3° coronal orientation of the proximal tibia, with a femorotibial angle of 2° (1 case) and –2° (1 case), respectively. There was no correlation between the coronal orientation of the distal femur and of the proximal tibia in the same patient (), with a regression coefficient of 0.12 (p = 0.9). There was no correlation between age and femorotibial angle (regression coefficient: 0.34; p = 0.7), age and femoral angle (regression coefficient: –0.34; p = 0.7) or age and tibial angle (regression coefficient: –0.134; p = 0.2). There was no significant influence of gender on femorotibial angle (p = 0.09), femoral angle (p = 0.2) or tibial angle (p = 0.5).
Discussion
Angle measurements on knee- or long-leg radiographs are currently accepted methods for the study of the coronal lower limb alignment. How-ever, these techniques are known to have a large inter- and intraobserver variability. Ilahi et al. (Citation2001) reported that 4 different measurements performed on standard radiographs were within 4° of each other in 95% of the cases, with a maximum difference of 6°. In a separate study, we analyzed the inter- and intraobserver reproducibility of our measurement technique on 50 randomly chosen cases from the present series of patients. Only the intra-observer variability of the measurement of the tibial axis was significant. 95–100% of the cases had inter- or intraobserver variation of less than 3°. Computerized techniques may improve the reliability of the measurements (Prakash et al. Citation2001, Takahashi et al. Citation2004), but these techniques have still to be validated on a larger scale.
One should also consider the variability introduced by the radiological technique itself. It has been demonstrated that knee flexion or knee rotation might substantially alter measurements. Lonner et al. (Citation1996) reported a mean 2-degree difference for 10° of knee rotation when the knee was fully extended. There is no general agreement for the optimal rotational positioning of the knee. To centralize the patella on the femoral condyles on the AP view would not be appropriate in individuals with a lateralized patella. To superimpose the posterior border of the femoral condyles on a lateral view would not be appropriate in people with a femoral condyle dysplasia. The most accurate technique might be to align the center of the tibial spines with the highest point of the femoral intercondylar notch.
We have confirmed that there is a wide variation in the measurements of the different angles of the lower limb alignment in a normal Caucasian population, with a standard deviation higher than the mean value for all angles. We found no influence of gender or age on the coronal alignment of the lower limb in this population.
Based on 25, probably Caucasian, subjects, Moreland et al. (Citation1987) stated that the normal angle between the mechanical axes of the femur and of the tibia is 0°, with a valgus inclination of the distal femur of 3° and varus inclination of the proximal tibia of 3°. As subjects, people without clinically obvious malalignment were selected. These small series cannot, therefore, be considered to be a reference population.
Hsu et al. (Citation1990) studied a probably Caucasian population of 120 cases. They found a mean femorotibial angle of 1.2° (SD 2.2), a mean valgus orientation of the distal femur of 4.2° (SD 1.7), and a mean varus orientation of the proximal tibia of 0.4° (SD 1.6). These results are very close to ours. However, these authors did not report the distribution of angles.
Tang et al. (Citation2000) studied a Chinese population of 50 cases. They found a mean femorotibial angle of 2.2°, and a mean varus orientation of the proximal tibia of 5.0°. They did not study the coronal orientation of the distal femur. These results are somewhat different from ours. The distribution of angles was not reported.
We found that only 14 to 19% of the Caucasian population of our study met the mean values defined by Moreland et al. (Citation1987), which are commonly accepted in the current literature. It appears that the variation of the leg axes about the mean is wider than commonly accepted. The importance of this variation should be evaluated. However, it is accepted that ligament kinematics is strongly linked to the anatomy of the articular surfaces (Muller Citation1994). It might be reasonable to consider an individual axis reconstruction for knee procedures to take the normal ligament kinematics of the individual patient into account (Nagamine et al. Citation2000).
It has been shown that the long-term results after high tibial osteotomy are better under some specific anatomical conditions such as proximal bowing of the tibia (Jenny et al. Citation1998, Lootvoet et al. Citation1993). There is a need for some overcorrection of the deformation, but the actual amount is not well defined (Hernigou Citation1996). This procedure might require to be performed on an individual basis according to the normal anatomy of the operated patient.
Unicompartmental knee replacement should preserve the ligament physiology and only correct degenerative changes (Cartier et al. Citation1996). The global leg deformation is due to both anatomical deformation and degenerative changes. There is currently no measurement technique to differentiate these two deformations (Jenny et al. Citation2004). A small undercorrection of the leg axis has been advocated to protect against polyethylene wear (Hernigou and Deschamps Citation2004). A more individually based anatomical reconstruction might be more efficient for optimal ligament balancing and knee kinematics.
Conventional resections for total knee replacement (TKR) involve a 0° coronal resection of the proximal tibia and a 0° coronal resection of the distal femur (Insall et al. Citation1985). Consequently, performance of a routine 3° external rotation positioning of the femoral component has been advocated to compensate for the flexion gap after a 0° proximal resection of the tibia, because of the expected 3° varus orientation of the proximal tibia (Laskin Citation1995). These resections may not, however, respect the anatomical condition of the individual patient, with possible influence on the behavior of ligaments. As there is no correlation between the coronal orientation of the distal femur and of the proximal tibia, there is little support for the routine 3° external rotation positioning of the femoral component of a TKR based on anatomical considerations. Anatomical resections for TKR involve a 3° varus resection of the proximal tibia and a 3° valgus resection of the distal femur (Hungerford and Krackow Citation1985), but this technique might not respect the anatomical conditions of the individual patient for the reasons mentioned above.
No competing interests declared.
- Cartier P, Sanouillier J L, Grelsamer R P. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty 1996; 11: 782–8
- Hernigou P. Recul à plus de 20 ans de la gonarthrose fémorotibiale interne après ostéotomie tibiale de valgisation. Ostéotomie unique versus ostéotomie itérative. Rev Chir Orthop 1996; 82: 241–50
- Hernigou P. Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop 2004, 423: 161–5
- Hsu R W W, Himeno S, Coventry M B, Chao E Y S. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop 1990, 255: 215–27
- Hungerford D S, Krackow K A. Total joint arthroplasty of the knee. Clin Orthop 1985, 192: 23–33
- Ilahi O A, Kadakia N R, Huo M H. Inter- and intraobserver variability of radiographic measurements of knee alignment. Am J Knee Surg 2001; 14: 238–42
- Insall J N, Binazzi R, Soudry M, Mestriner L A. Total knee arthroplasty. Clin Orthop 1985, 192: 13–22
- Jenny J Y, Tavan A, Jenny G, Kehr P. Taux de survie à long terme des ostéotomies tibiales de valgisation pour gonarthrose. Rev Chir Orthop 1998; 84: 350–7
- Jenny J Y, Boeri C, Ballonzoli L, Meyer N. Reproductibilité de la mesure radiographique de l'axe épiphysaire proximal du tibia selon la technique de Dejour. Accepted for publication in Rev Chir Orthop.
- Laskin R S. Flexion space configuration in total knee arthroplasty. J Arthroplasty 1995; 10: 657–60
- Lonner J H, Laird M T, Stuchin S A. Effect of rotation and knee flexion on radiographic alignment in total knee arthroplasties. Clin Orthop 1996, 331: 102–6
- Lootvoet L, Massinon A, Rossillon R, Himmer O, Lambert K, Ghosez J P. Ostéotomie tibiale haute de valgisation pour gonarthrose sur genu varum. À propos d'une série de 193 cas revus après 6 à 10 ans de recul. Rev Chir Orthop 1993; 79: 375–84
- Moreland J R, Bassett L W, Hanker G J. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg (Am) 1987; 69: 745–9
- Muller W. The Knee. Springer, Berlin - Heidelberg - New York - London - Paris - Tokyo - Hong Kong - Barcelona Budapest 1994
- Nagamine R, Miura H, Bravo C V, Urabe K, Matsuda S, Miyanishi K, Hirata G, Iwamoto Y. Anatomic variations should be considered in total knee arthroplasty. J Orthop Sci 2000; 5: 232–7
- Parakash U, Wigderowitz C A, McGurty D W, Rowley D L. Computerised measurement of tibiofemoral alignment. J Bone Joint Surg (Br) 2001; 83: 819–24
- Takahashi T, Yamanaka N, Komatsu M, Ogawa Y, Yoshida S, Yamamoto H. A new computer-assisted method for measuring the tibio-femoral angle in patients with osteoarthritis of the knee. Osteoarthritis Cartilage 2004; 12: 256–9
- Tang W M, Zhu Y H, Chiu K Y. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg (Am) 2000; 82: 1603–8