Abstract
Background There is no consensus on the best surgical treatment of periprosthetic femoral fractures. We report our experience with a dynamic compression plate.
Patients and methods We reviewed the results of 18 periprosthetic femoral fractures treated with open reduction and internal fixation using the dynamic compression plate (DCP). There were 7 Vancouver type B1, 2 type B2 and 9 type B3 fractures. 16 cases had previously undergone at least one revision procedure. In addition to a DCP plate, all B2 and B3 fractures were revised to cemented prostheses, and all B3 fractures were revised with impaction grafting. Mean follow-up was 39 months.
Results The mean healing time for those 11 cases that united was 13 months. One B1-type and one B3-type fracture with plate fracture within 8 months of surgery failed to heal. Furthermore, one B1-type fracture and one B2-type fracture failed and developed nonunion. 3 patients died, from causes not related to surgery, within 8 months after surgery without signs of healing.
Interpretation Open reduction and internal fixation using DCPs seems to be a valid method for the treatment of postoperative periprosthetic femoral fractures with stable stem in place. If the stem is unstable, we suggest that DCPs may be used in association with femoral revision using a long stem. In cases with stable stem (B1), we are inclined to agree with other authors that additional fixation using an extramedullary cortical strut graft may be necessary to improve stability and promote final healing.
The prevalence of postoperative periprosthetic femoral fractures increases as the population of patients with total hip arthroplasties (THAs) and compromized femoral bone around the prostheses grows (Beals and Tower Citation1996, Garbuz et al. 1998). This increased incidence seems to be the result of osteolysis or multiple revision operations, and is often associated with implant loosening (Kelley Citation1994, Berry Citation1999, Schmidt and Kyle Citation2002, Tsiridis et al. Citation2003a). Despite several case series in the literature, it is difficult to draw conclusions about the true incidence of these fractures due to discrepancies in methodology (Johansson et al. Citation1981, Bethea et al. Citation1982, Cooke and Newman Citation1988, Mont and Maar Citation1994, Lewallen and Berry Citation1998, Somers et al. Citation1998, Tower and Beals Citation1999, Tadross et al. Citation2000, MacDonald et al. Citation2001, Tsiridis et al. Citation2003b).
In a review of 1 442 THAs, Löwenhielm et al. (Citation1989) found the accumulated risk of postoperative fractures to be 25 per 1000 over a 15-year period, while Beals and Tower (Citation1996) estimated the incidence of such fractures over the lifespan of a prosthesis to be less than 1%. A recent review from the Mayo Clinic Joint Registry identified 262 (1%) postoperative periprosthetic femoral fractures following 23 980 primary THAs, and 252 (4%) such fractures following 6 349 revision THAs (Berry Citation1999).
Closed treatment of postoperative periprosthetic femoral fractures is associated with high nonunion and malunion rates, and frequently results in subsequent revision (Johansson et al. Citation1981, Beals and Tower Citation1996, Garbuz et al. Citation1998). In cases of stable prostheses, open reduction and internal fixation employs either cortical onlay allografts (Chandler and Tigges Citation1998), dynamic compression plates (DCPs), or special plates such as the Ogden, the Dall-Miles or the Mennen plates (Zenni et al. Citation1988, Serocki et al. Citation1992, Uchio et al. Citation1997, Jukkala-Partio et al. Citation1998, Tower and Beals Citation1999, Tadross et al. Citation2000). Alternatively, combined medial and lateral allograft struts with cerclage cables or lateral plating with a single anterior or medial allograft strut may be used (Ries Citation1997, Tower and Beals Citation1999). Furthermore, Haddad et al. (Citation1997) reported good results following the combination of a Dall-Miles plate with two strut grafts and cancellous autograft in four patients. In cases of a peri-prosthetic femoral fracture necessitating cemented revision, DCPs may also be used for reduction during the prosthesis insertion; they may be fixed with unicortical screws around the prosthesis and bicortical screws below it.
This report deals with the use of DCPs for the fixation of fractures (a) around stable prostheses and (b) during cemented revision of unstable prostheses with or without impaction grafting.
Patients and methods
Between June 1996 and February 2000, 16 patients (10 women) with 18 periprosthetic femoral fractures were treated with DCP plates in our unit, where an average of 527 primary and 135 revision THAs are performed annually. Cases 1 and 2 represent 2 consecutive fractures, within 8 months of each other, in the left femur of the same patient, whereas cases 17 and 18 represent bilateral fractures sustained by the same patient at different time points. The mean patient age at the time of fixation was 70 (44–83) years. 8 fractures occurred in the left femur and 10 in the right .
Data on the patients: Pre–operative findings, treatment and results
All fractures were around cemented implants. 2 fractures occurred after a primary THA (cases 4 and 13), and 16 occurred after revision procedures. Of the latter, 7 were sustained following 1 revision, 7 following 2 revisions and 2 following 3 revisions. 3 patients (3 fractures: cases 5, 6, 13) died within 8 months for reasons not related to surgery, whereas 13 (15 fractures: cases 1–4, 7–12, and 14–18) continued to be followed up.
Fractures were classified radiographically according to the Vancouver system. This system is based on the location of the fracture, the stability of the implant and the quality of the bone stock. Type A fractures involve the trochanteric region and are subclassified into AG fractures involving the greater trochanter, and AL fractures involving the lesser trochanter. Type B fractures occur around the stem of the femoral component, or extend slightly distal to it. They are further subclassified based on the stability of the implant and the quality of the bone stock. In type B1 fractures the implant is stable, whereas in type B2 and B3 fractures the implant is unstable. In both type B1 and type B2 fractures, the bone stock around the femoral component is adequate, whereas in type B3 fractures the bone stock around it is inadequate. Type C fractures are located distal to the stem. Despite the fact that the Vancouver classification system is based on preoperative radiographic assessment, it currently remains the most valid and reliable periprosthetic classification of fracture (Brady et al. Citation1999).
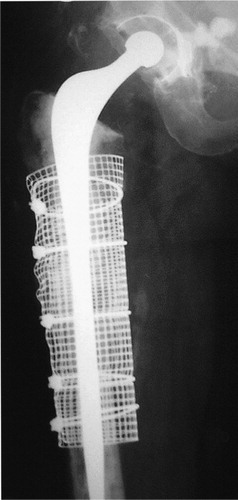
In our series, preoperative radiographic assessment matched intraoperative findings. 7 type B1, 2 type B2 and 9 type B3 fractures were identified. A DCP plate was used on all 18 fractures. The plate was stabilized with unicortical screws and cerclage wires proximally around the femoral component, and with bicortical screws distally below the tip of the femoral component. In addition to a DCP plate, all B2 and B3 fractures (11 cases in total) were revised to cemented prostheses and all B3 fractures were also treated using the impaction grafting technique. In 9 cases (2 type B2 and 7 type B3 fractures), the revision stem bypassed the most distal fracture line. In a further 2 cases, however (both type B3 fractures operated on in 1996), the revision stem was entirely in the proximal segment, as standard stems were being used with the impaction revision procedure at the time. Long cemented stems, by-passing the most distal fracture line, have been employed since 1996. In our series, no type B1 fracture had the stem revised.
The patients were reviewed clinically and radiographically. The mean follow-up time for our 18 cases was 39 (2–108) months. Fracture union was defined as the ability to bear weight fully with or without aids in the presence of radiographic evidence of callus bridging the fracture in both the antero-posterior and lateral radiographs. The callus formation could not always be visualized circumferentially, however, due to the presence of wires, cables, meshes, and plates. Clinical union was defined as pain-free full weight bearing or full weight bearing with slight occasional pain that did not compromise basic daily activities or walking, with or without aids.
The clinical outcomes were determined using Charnley's modification of the Merle D’Aubigne and Postel hip scoring system (Charnley Citation1972). 13 follow-up scores were available (cases 2–4, 7–11, and 14–18), including the 2 nonunion cases (cases 2 and 18). There were no scores available for the 2 cases in which the DCP plates fractured (cases 1 and 12), and for the 3 patients who died soon after surgery (cases 5, 6, and 13).
Postoperatively, patients having undergone impaction revision were instructed to walk toetouch weight bearing for 6 weeks, if the bone stock was not severely compromised prior to impaction grafting, and for 3 months if it was. For the patients who were treated without impaction grafting, partial weight bearing with crutches was encouraged soon after surgery, and as soon as pain allowed.
Results
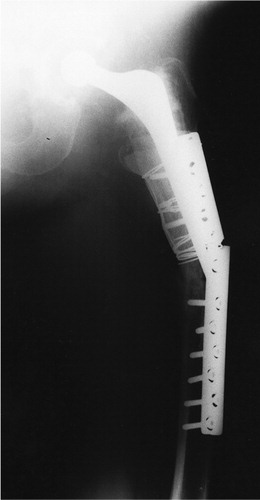
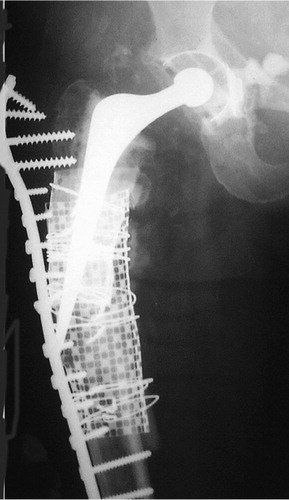
11 fractures eventually united (4 type B1, 6 type B3 and 1 type B2) ( and ). A type B1 fracture (case 1) in a woman with a history of one previous revision procedure and a B3 type fracture (case 12) in a male patient with a history of 3 previous revision procedures treated with DCP plates, failed to heal because of fracture of the plate (). Failure of these plates occurred within 8 months of surgery. A further 2 fractures of types B1 and B2 (cases 2 and 18), in 2 females with a history of 2 previous revision procedures each, also failed to heal due to nonunion. In the latter case, the DCP plate also pulled away from the femur ( and ). 3 patients (2 male; 3 fractures: cases 5, 6, 13) died 2–8 months after the operation, from causes unrelated to surgery, without evidence of fracture union. The mean healing time for the 11 fractures that united was 13 (8–24) months.
Figure 1. Vancouver type B2 fracture. The stem was unstable and was revised, whereas the quality of the surrounding bone was good.

Figure 2. 12 months postoperatively. Long-stem revision and DCP plate applied to the lateral aspect of the femur.

Figure 4. Long DCP plate. The plate was used for the treatment of a Vancouver type B2 fracture along with impaction grafting revision of the stem.
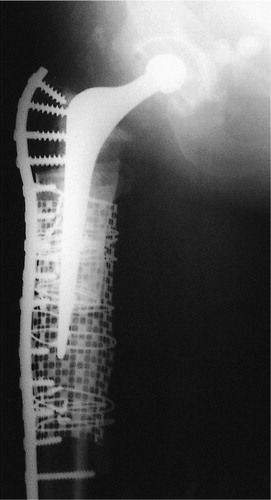
Using Charnley's modification of the Merle D’Aubigne and Postel hip scoring system, 3 category A, 2 category B, and 8 category C fractures were identified in 12 patients. Postoperatively, in category A, the median score for pain reached 4.5 (range 3–6), for function 3 (2–4), and for range of movement 4.5 (3–6). In category B, the median score for pain was 2.5 (2–3), for function 1.5 (1–2), and for range of movement 5 (4–6). In category C, the median scores for pain, function, and range of movement were 4 (2–6), 2 (1–5) and 5 (4–6), respectively. There was no infection in any of the 4 “failed to- unite” cases (cases 1, 2, 12 and 18). These cases were treated with long cemented stems by-passing the most distal fracture line. Cases 12 and 18 (type B3 and B2 fractures, respectively) were also treated with impaction grafting ().
Discussion
Most authors recommend revision with long-stem prosthesis for Vancouver type B2 and B3 fractures, with the combined nonunion, refracture and revision rates reported to be 12–20% (Cooke and Newman Citation1988, Duncan and Masri Citation1995, Garbuz et al. Citation1998, Berry Citation1999). Early reports suggested the use of long-stem cemented prostheses (Cooke and Newman Citation1988, Duncan and Masri Citation1995, Lewallen and Berry Citation1998) but recent reports have favored the use of uncemented prostheses (Mont and Maar Citation1994, Beals and Tower Citation1996, Incavo et al. Citation1998, Berry Citation1999, Schmidt and Kyle Citation2002). Revision with a long-stem prosthesis permits stabilization of the fracture in a similar way to that provided by an intramedullary rod, the goal being to by-pass the fracture by at least 2 shaft diameters.
Larson et al. (Citation1991) subjected canine femurs to an experimental cortical perforation in vitro, and demonstrated that the perforated femurs achieved only 44% of the strength of the intact ones. The strength of the perforated femur was raised to four fifths of that of the intact contralateral femur if the stem by-passed the defect by 2 femoral diameters. A long cemented stem can provide adequate stability, but cement may come between the fracture fragments and delay union (Cooke and Newman Citation1988, Eschenroeder and Krackow Citation1988).
Open reduction and internal fixation without revision, using stainless steel wires, multi-filament cables, or wide bands such as the Partridge bands (Partridge and Evans Citation1982), has been recommended for stable stem cases. Clinical studies, however, have shown that cerclage fixation alone is not rigid enough, and that it should be supplemented with other methods of internal fixation (Garcia-Cimbrelo et al. Citation1992). DCPs can be fixed around a stable stem with unicortical screws, with or without cerclage wires or cables, and with bicortical screws below it. Screws, however, may violate the cement mantle and act as a source of stress, increasing the risk of a later fracture or nonunion (Zenni et al. Citation1988, Serocki et al. Citation1992, Jukkala-Partio et al. Citation1998, Tower and Beals Citation1999, Park et al. Citation2003). Furthermore, combined DCPs with a single anterior or medial allograft strut appear to provide fixation which is superior to that achieved when either plate is used alone (Tower and Beals Citation1999). It has been advocated that the DCP plate protects the strut graft, which can be incorporated into host bone, thus augmenting the mechanical strength of the femur (Ries Citation1997). Tower and Beals (Citation1999) recommended that the allograft/plate construct should by-pass any cortical defect by 2 cortical diameters, and that it should be staggered (ladder pattern) distally, in order to avoid development of stress.
In our series, the postoperative outcome was not ideal, but it was considered to be satisfactory, given the complexity of the injuries, the number of previous revision procedures, the poor surrounding bone stock, and the age of the patients. Regarding the Charnley-D’Aubigne-Postel scoring system, the low pain score in category B, compared to the pain score in categories A and C, was not surprising, as, by definition, patients in this category have bilateral hip pathology.
In the 2 cases of plate fracture (1 type B1 and 1 type B3), the stem was either not revised and remained entirely above the most distal fracture line, imposing stress to the lateral femoral cortex and the plate (type B1 fracture, case 1), or it was revised to a stem that did not by-pass the most distal fracture line enough to secure fracture fixation and healing (type B3 fracture, case 12). In the 2 cases of nonunion (1 type B1 and 1 type B2), failure to heal was attributed to insufficient fracture stability due to a relatively short stem in situ (type B1 fracture, case 2) and, also, due to cement interposition into the fracture during the revision procedure (type B2 fracture, case 18).
2 of 7 type B1 fractures failed to heal, and in one further B1 fracture case, the patient died without evidence of union (case 6). A total of 4 B1-type fractures healed successfully, and only 1 of them (case 11) healed at a varus position (4°). Case 10 presented with partial sciatic nerve palsy, which resolved within 3 months. Based on the above results, we are inclined to agree with other authors that additional fixation using an extramedullary cortical strut graft may be necessary to improve stability and promote final healing (Haddad et al. Citation2002).
In type B2 and B3 fractures, a relatively short revision stem was considered to be the cause of failure in the first case (B3-type, case 12), whereas in the second case (B2-type, case 18), cement extrusion and interposition was thought to be the cause of nonunion. Having experienced several failures with the use of a short stem not bypassing the fracture, our practice has been changed to the use of long stems and impaction grafting. This is necessary in order to optimize fracture stability, enhance union rates and improve final outcome when the stem is unstable. Moreover, caution is required so that cement interposition between fracture fragments can be avoided.
Eleftherios Tsiridis was supported by the “Alexander S. Onassis Public Benefit Foundation”, Greek Section of Scholarships and Research.
No competing interests declared.
- Beals R K, Tower S S. Periprosthetic fractures of the femur. An analysis of 93 fractures. Clin Orthop 1996, 327: 238–46
- Berry D J. Epidemiology: hip and knee. Orthop Clin North Am 1999; 30: 183–90
- Bethea J S, III, DeAndrade J R, Fleming L L, Lindenbaum S D, Welch R B. Proximal femoral fractures following total hip arthroplasty. Clin Orthop 1982, 170: 95–106
- Brady O H, Garbuz D S, Masri B A, Duncan C P. Classification of the hip. Orthop Clin North Am 1999; 30(2)215–20
- Chandler H P, Tigges R G. The role of allografts in the treatment of periprosthetic femoral fractures. Instr Course Lect 1998; 47: 257–64
- Charnley J. Long term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 1972; 54: 61–76
- Cooke P H, Newman J H. Fractures of the femur in relation to cemented hip prostheses. J Bone Joint Surg (Br) 1988; 70: 386–9
- Duncan C P, Masri B A. Fractures of the femur after hip replacement. Instr Course Lect 1995; 44: 293–304
- Eschenroeder H C, Jr, Krackow K A. Late onset femoral stress fracture associated with extruded cement following hip arthroplasty: A case report. Clin Orthop 1988, 236: 210–3
- Garbuz D S, Masri B A, Duncan C P. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect 1998; 47: 237–42
- Garcia-Cimbrelo E, Munuera L, Gil-Garay E. Femoral shaft fractures after cemented total hip replacement. Int Orthop 1992; 16: 97–100
- Haddad F S, Marston R A, Muirhead-Allwood S K. The Dall-Miles cable and plate system for periprosthetic femoral fractures. Injury 1997; 28: 445–7
- Haddad F S, Duncan C P, Berry D J, Lewallen D G, Gross A E, Chandler H P. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg (Am) 2002; 84: 945–50
- Incavo S J, Beard D M, Pupparo F, Ries M, Wiedel J. One-stage revision of periprosthetic fractures around loose cemented total hip arthroplasty. Am J Orthop 1998; 27: 35–41
- Johansson J E, McBroom R, Barrington T, Hunter G A. Fracture of the ipsilateral femur in patients with total hip replacement. J Bone Joint Surg (Am) 1981; 63: 1435–42
- Jukkala-Partio K, Partio E K, Solovieva S, Paavilainen T, Hirvensalo E, Alho A. Treatment of periprosthetic fractures in association with total hip arthroplasty - a retrospective comparison between revision stem and plate fixation. Ann Chir Gynaecol 1998; 87(3)229–35
- Kelley S S. Periprosthetic femoral fractures. J Am Acad Orthop Surg 1994; 2: 164–72
- Larson J E, Chao E Y, Fitzgerald R H. By-passing femoral cortical defects with cemented intramedullary stems. J Orthop Res 1991; 9: 414–21
- Lewallen D G, Berry D J. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect 1998; 47: 243–9
- Löwenhielm G, Hansson L I, Kärrholm J. Fracture of the lower extremity after total hip replacement. Arch Orthop Trauma Surg 1989; 108: 141–3
- Macdonald S J, Paprosky W G, Jablonsky W S, Magnus R G. Periprosthetic femoral fractures treated with a long-stem cementless component. J Arthroplasty 2001; 16: 379–83
- Mont M A, Maar D C. Fractures of the ipsilateral femur after hip arthroplasty. A statistical analysis of outcome based on 487 patients. J Arthroplasty 1994; 9: 511–9
- Park M S, Lee Y K, Yang K H, Shin S J. Management of periprosthetic femoral fractures. J Arthroplasty 2003; 18: 903–6
- Partridge A J, Evans P E. The treatment of fractions of the shaft of the femur using nylon cerclage. J Bone Joint Surg (Br) 1982; 64: 210–4
- Ries M D. Periprosthetic fractures: Early and late. Orthopedics 1997; 20: 798–800
- Schmidt A H, Kyle R F. Periprosthetic fractures of the femur. Orthop Clin North Am 2002; 33: 143–52
- Serocki J H, Chandler R W, Dorr L D. Treatment of fractures about hip prostheses with compression plating. J Arthroplasty 1992; 7: 129–35
- Somers J F, Suy R, Stuyck J, Mulier M, Fabry G. Conservative treatment of femoral shaft fractures in patients with total hip arthroplasty. J Arthroplasty 1998; 13: 162–71
- Tadross T S, Nanu A M, Buchanan M J, Checketts R G. Dall-Miles plating for periprosthetic B1 fractures of the femur. J Arthroplasty 2000; 15: 47–51
- Tower S S, Beals R K. Fractures of the femur after hip replacement: the Oregon experience. Orthop Clin North Am. 1999; 30: 235–47
- Tsiridis E, Haddad F S, Gie G A. The management of peri-prosthetic femoral fractures around hip replacements. Injury 2003a; 34: 95–105
- Tsiridis E, Haddad F S, Gie G A. Dall-Miles plates for peri-prosthetic femoral fractures. A critical review of 16 cases. Injury 2003b; 34: 107–10
- Uchio Y, Shu N, Nishikawa U, Takata K, Ochi M. Mennen plate fixation for fractures of the femoral shaft after ipsilateral hip arthroplasty. J Trauma 1997; 42: 1157–60
- Zenni E J, Jr, Pomeroy D L, Caudle R J. Ogden plate and other fixations for fractures complicating femoral endoprostheses. Clin Orthop 1988, 231: 83–90