Abstract
Background Recurrent patellar dislocation may be associated with trochlear dysplasia. Trochleaplasty is a surgical procedure which strives to deepen the trochlear groove. We evaluated the clinical and radiological effect of trochleaplasty after a minimum follow-up of 2 years.
Patients and methods We examined 19 knees in 16 patients at a mean of 3 years after trochleaplasty. Postoperatively, a subjective questionnaire, a Kujala score, and tests for potential patellar redislocation and apprehension were evaluated. On radiographs we evaluated the preoperative and postoperative crossing sign, trochlear depth, trochlear bump, and patellar height. On CT scans, the pre- and postoperative tibial tuberosity to trochlear groove distance (TTTG) and the patellar inclination angle were measured.
Results 16 of 19 knees improved subjectively. The Kujala score increased from 56 to 80 points at the latest follow-up. None of the patients sustained a redislocation. 5 patients had medial parapatellar tenderness, including 4 with persistent apprehension. Radiological signs of trochlear dysplasia were corrected.
Interpretation Patellofemoral instability with underlying trochlear dysplasia can be treated successfully by trochleaplasty.
As a consequence of trochlear dysplasia with a low lateral condyle, the depth of the trochlear groove is reduced and the patella cannot engage properly (Pollard Citation1891, Drew Citation1908). Trochlear dysplasia was first described by Richerand in 1802 (Isermeyer Citation1967). Brattström (Citation1965) found that the lateral condyle was significantly lower in patients with recurrent patellar dislocation than in patients without patellofemoral pathology. Dejour et al. (Citation1994) found that dysplasia of the femoral groove occurred in 85% of patients with recurrent patellar dislocation.
Different techniques have been described to correct trochlear dysplasia surgically. Albee (Citation1915) elevated the lateral condyle by an osteotomy and interposition of a tibial graft. Masse (Citation1978) described a technique in which the trochlear groove was remodeled, and Dejour et al. (Citation1990) deepened the trochlea by an osteotomy after peeling off the cartilage. Bereiter and Gautier (Citation1994) described a similar technique in which the cartilage is peeled off, and the subchondral trochlea is deepened with a highspeed burr.
We compared preoperative and postoperative clinical and radiological parameters in patients with recurrent patellar instability and trochlear dysplasia before and after trochleaplasty using the technique described by Bereiter and Gautier (Citation1994).
Patients and methods
Indications for operation
Indications for trochleaplasty were 2 or more patellar dislocations or 1 patellar dislocation with a persistent Fairbank’s apprehension sign of more than
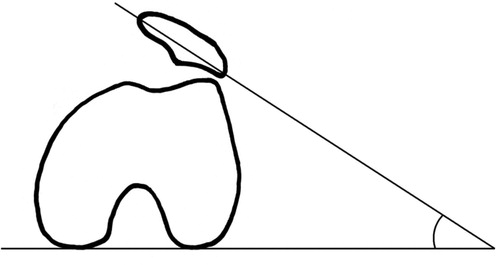
1 year (patient experiences pain and anxiety, while the examiner attempts to lateralize the patella in the extended leg) in the presence of all radiological signs of trochlear dysplasia. This includes a positive crossing sign, where the trochlea is crossing the lateral femoral condyle on a straight lateral view, a reduced trochlear depth, a trochlear bump, and minimal translation on a straight lateral radograph (Dejour et al. Citation1994). Every patient had preoperative MRI to evaluate the cartilage of the trochlea. Contraindications for operation were degenerative deformation of the trochlea and open epiphyseal plates.
Surgical technique
Through a parapatellar lateral incision, the trochlea is exposed by retracting the patella medially in full extension. The cartilage is separated from the synovium and is detached with a rasp. The medial and lateral condyles are peeled off using curved osteotomes until 5 mm cranial of the notch, together with the trochlea in one piece, leaving a bone stock of 2 mm on the cartilaginous fragment (). Then the subchondral groove is deepened using a straight chisel and a highspeed burr. The trochlear cartilagobony flake is now pressed into the newly formed bony groove and fixed with 2 transosseous vicryl strings in the deepest part of the new trochlea. The synovium is reattached to the condylar edges with a continuous absorbable suture (). The insertion of the vastus medialis obliquus muscle at the patella is tightened with one suture.
Figure 2. Intraoperative finding after trochleaplasty with the deeper trochlear groove. The trochlear cartilage is fixed with 2 transosseous vicryl strings. The synovia is reattached with continuous absorbable braided 2-0 suture to the condylar edges.

The lateral retinaculum is left open. The joint is closed by adaptation of the synovium and the skin is closed. Intraarticular drainage is removed after 24 h. A knee immobilizer at 30° of flexion is left for 6 weeks. Daily knee flexion exercises are allowed without restriction, but with a physiotherapist. No more than 30° of extension is allowed for 6 weeks. Full weight bearing is allowed from the first day.
Patients (Table)
Between 1999 and 2001, we performed trochleaplasty in 19 knees of 16 patients (3 bilateral). 13 patients were women (2 bilateral). The average age at surgery was 22 (17–40) years. 16 knees had suffered from recurrent patellar dislocation, and 3 knees had suffered from persistent apprehension of more than 1 year after 1 patellar dislocation. The apprehension sign was positive in all patients. 5 patients had undergone previous surgery, such as cartilage debridement, medial retinacular suture, lateral retinacular release, or medialization of the tibial tuberosity.
Patient data
All patients were available for follow-up at a mean of 3 (2–4) years. The clinical postoperative evaluation consisted of a subjective questionnaire (Drez et al. Citation2001), the Kujala knee score (Kujala et al. Citation1993), and of a physical examination (apprehension to lateral displacement, medial quadriceps tenderness, patellofemoral pain). Signs of trochlear dysplasia (Dejour et al. Citation1994), and also patellar height were evaluated on straight lateral radiographs, the latter by using the Caton ratio (Citation1989).
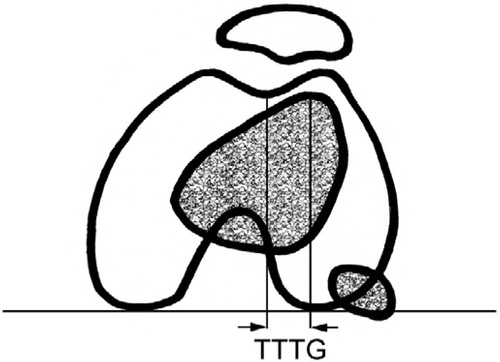
The tibial tuberosity to trochlear groove distance (TTTG) () (Goutallier et al. Citation1978) and the patellar inclination angle (PIA) () (Beaconsfield et al. Citation1994) were measured on transverse CT scans.
Statistics
Pre- and postoperative clinical and radiological findings were compared using the Wilcoxon signed rank test, with significance set at p < 0.05. We used the mean values of the 3 patients operated bilaterally. Thus, only 16 knees were used for the statistical analysis. We hypothesized that the Kujala score should increase, the “crossing sign and positive trochlear translation disappear, the trochlear depth increase, the Caton index and the number of patella alta decrease, and that the TTTG and the PIA should increase.
Results (Table)
16 of 19 knees had improved subjectively. According to Drez’s subjective score (Drez et al. Citation2001), 10 knees had an excellent result, 6 had a good result, 1 had a fair result and 2 patients had a bad result. All patients reported improved stability. No redislocation occurred, but 4 patients reported a persistent apprehension, still suffering from anxiety, while the examiner attempted to lateralize the patella in the extended leg. 5 patients had a tenderness of the medial patellofemoral retinacular area. In 12 knees the pain level became reduced, while there was increased pain in 2 knees postoperatively. Overall, the Kujala score increased from 56 (27–67) points to 80 (43–99) points at the latest follow-up (p = 0.003). The preoperative crossing sign was grade I in 7 cases, grade II in 3, and grade III in 9 cases according to Dejour et al. (Citation1990). Postoperatively, a persistent crossing sign of grade I was found in 3 cases (p < 0.001), but none of these patients had a fair or bad result. Postoperatively, a positive trochlear translation remained in 3 knees (p < 0.001); 1 of them had a fair result and two had a good result. The mean depth increased from 0.6 (–3 to 3) mm preoperatively to 7 (4–9) mm post-operatively (p < 0.001). All knees had a normal trochlear depth postoperatively. The Caton ratio decreased from 1.2 (0.85–1.47) preoperatively to 1.1 (0.82–1.28) postoperatively. The number of knees with patella alta decreased from 10 to 2 (p = 0.004). The mean TTTG decreased from 20 (10–24) mm preoperatively to 9.9 (5–15) mm post-operatively (p = 0.001). The mean PIA decreased from 22° (5– 35) preoperatively to 8° (1–20) post-operatively (p < 0.001). 2 of 3 patients with fair or bad results had degenerative changes of the trochlea preoperatively, which increased in 1 of them postoperatively.
Discussion
Trochlear dysplasia is a predisposing factor for recurrent patellar instability (Dejour et al. Citation1994). Proximal or distal soft tissue realignment procedures, with or without transfer of the tuberosity, have had limited success in patients with trochlear dysplasia (Harilainen and Sandelin Citation1993, Aglietti et al. Citation1994, Schneider et al. Citation1997, Fulkerson Citation2002).
Since the medial patellofemoral ligament (MPFL) ruptures or lengthens regularly after patellar dislocation (Fithian et al. Citation1995), MPFL reconstruction has a high success rate in patients with normal trochlear anatomy (Fithian et al. Citation1995, Muneta et al. Citation1999, Garth et al. Citation2000, Nomura et al. Citation2000, Drez et al. Citation2001). However, in knees with an underlying trochlear dysplasia, the ligamentous insufficiency is not a cause, but rather a consequence of recurrent dislocation (Masse Citation1978, Dejour et al. Citation1990, Bereiter and Gautier Citation1994).
Our findings show that trochleaplasty is an effective and safe procedure, which prevents patellar subluxation or dislocation.
Other than the technique of Albee (Citation1915), which elevates the lateral condyle and increases lateral patellofemoral pressure, the techniques of Masse (Citation1978), Dejour et al. (Citation1990) and Bereiter and Gautier (Citation1994) deepen the trochlea, which results in a relative increase of the lateral condyle. Such a remodeling of the trochlear groove in the proximal part might lead to an improved engagement of the patella in the early flexion phase. The technique of Masse impacts the cartilage without fixation of the underlying bone, while the technique of Dejour peels off the cartilage before the trochlea is remodeled by an osteotomy of the two condyles, lowering them in the central aspect. Using this technique, a V-shape of the trochlea is achieved rather than a concave shape. The technique of Bereiter allows a concave modeling of the trochlea, as has been demonstrated on postoperative transverse CT scans in our study ( and ). In addition, the TTTG is normalized without having performed a transfer of the tuberosity in any knee.
Figure 6. Postoperative axial CT scan with an improvement of the trochlear depth, measured at the same level and in the same patient as in .

A less satisfactory result can be expected if the trochlear cartilage has degenerated. To force the degenerated and unelastic cartilagobony layer back to the deepened subchondral groove may result in cartilage fracture and further. However, the procedure by itself seems not to initiate evident degenerative changes of the condyles during the first 2 years after surgery, although Bereiter and Gautier (Citation1994) found the development of pannus on histological examination of the groove where the vicryl sutures were placed. We did not see any postoperative detachment of the cartilagobony layer in any patient; however, the long-term vitality of the cartilage after trochleaplasty is still an open question.
Preoperative imaging work-up with straight lateral view and a CT scan is important for identification of all features of trochlear dysplasia (Dejour et al. Citation1980, Citation1994, Galland et al. Citation1990, Beaconsfield et al. Citation1994). Preoperative MRI may show degenerative trochlear cartilage. The goal of the operation is the anatomical reconstruction of the trochlea by eliminating the crossing sign and the trochlear bump, and by deepening the groove and decreasing the TTTG.
Trochleaplasty should be avoided in the case of open epiphysis. It is unclear whether preoperative arthritic changes are a contraindication and whether the procedure enhances or initiates femoropatellar arthritis, since recurrent instability itself results in patellofemoral arthrosis in one third of the patients (Maenpaa and Lehto Citation1997, Maenpaa et al. Citation1997).
No competing interests declared.
- Aglietti P, Buzzi R, De Biase P, Giron F. Surgical treatment of recurrent dislocation of the patella. Clin Orthop 1994, 308: 8–17
- Albee F H. The bone graft wedge in the treatment of habitual dislocation of patella. Med Rec 1915; 88: 257–9
- Beaconsfield T, Pintore E, Maffulli N, Petri G J. Radiological measurements in patellofemoral disorders. A review. Clin Orthop 1994, 308: 18–28
- Bereiter H, Gautier E. Die Trochleaplastik als Chirurgische Therapie der Rezidivierenden Patellaluxation bei Trochleadysplasie. Arthroskopie 1994; 7: 281–6
- Brattström H. Shape of the intercondylar groove normally and in recurrent dislocation of the patella. Acta Orthop Scand (Suppl 68) 1965; 1–144
- Caton J. Method of measuring the height of the patella. Acta Orthop Belg 1989; 55: 385–6
- Dejour H, Goutallier D, Furioli J. Unbalanced patella. Criticism of therapeutic methods and indications. Rev Chir Orthop 1980; 66: 238–44
- Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop 1990; 76: 45–54
- Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994; 2: 19–26
- Drew D. Dislocation of patella. Proc R Soc Med 1908; 1: 11
- Drez D, Jr., Edwards T B, Williams C S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy 2001; 17: 298–306
- Fithian D C, Mishra D K, Balen P F, Stone M L, Daniel D M. Instrumented measurement of patellar mobility. Am J Sports Med 1995; 23: 607–15
- Fulkerson J P. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med 2002; 30: 447–56
- Galland O, Walch G, Dejour H, Carret J P. An anatomical and radiological study of the femoropatellar articulation. Surg Radiol Anat 1990; 12: 119–25
- Garth W P, Jr., DiChristina D G, Holt G. Delayed proximal repair and distal realignment after patellar dislocation. Clin Orthop 2000, 377: 132–44
- Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity. atella groove distanced technique and results. Rev Chir Orthop 1978; 64: 423–8
- Harilainen A, Sandelin J. Prospective long-term results of operative treatment in primary dislocation of the patella. Knee Surg Sports Traumatol Arthrosc 1993; 1: 100–3
- Isermeyer H. Über die pathologische Luxation der Patella. Arch Klin Chir 1967; 8: 1–23
- Kujala U M, Jaakkola L H, Koskinen S K, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy 1993; 9: 159–63
- Maenpaa H, Lehto M U. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop 1997, 339: 156–62
- Maenpaa H, Huhtala H, Lehto M U. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand 1997; 68: 424–6
- Masse Y. Trochleoplasty. Restoration of the intercondylar groove in subluxations and dislocations of the patella. Rev Chir Orthop 1978; 64: 3–17
- Muneta T, Sekiya I, Tsuchiya M, Shinomiya K. A technique for reconstruction of the medial patellofemoral ligament. Clin Orthop 1999, 339: 151–5
- Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee 2000; 7: 211–5
- Pollard B. Old dislocation of patella reduced by intra articular operation. Lancet 1891; 1: 988
- Schneider T, Menke W, Fink B, Ruther W, Schulitz K P. Recurrent dislocation of the patella and the Goldthwait operation. Arch Orthop Trauma Surg 1997; 116: 46–9