Abstract
Background Different methods and devices are used to perform lengthening and deformity reconstruction in the tibia. Recently, the Taylor spatial frame (TSF) has been introduced as a computer-assisted and versatile external ring fixator. Lengthening index (LI) and complications are important result parameters, and the aim of this study was to review our first 20 tibial segments operated with the TSF and to compare the results with our experience of using the traditional Ilizarov external fixator (IEF).
Patients and methods We lengthened 20 tibial segments in 20 patients with the TSF. The results were compared with those of 27 tibial segments from 27 patients that were lengthened with the IEF. All segments were operated on with monofocal osteotomies.
Results In the overlapping zone of comparable lengthening distances between 2.4 and 6.0 cm, the LI of 2.4 and 1.8 months/cm was not significantly different between the TSF and IEF groups, respectively (p = 0.17). This non-significant difference was confirmed after adjustment for age.
Interpretation We found no difference between the TSF and IEF frames regarding LI and complication rate. However, rotational, translational, and residual deformity correction is easier to perform with the TSF.
Lengthening of long tubular bones is used both in children and adults to solve serious problems regarding leg length inequality, short stature, axial deformities and combinations of these conditions (Ilizarov Citation1992).
The callotasis method originally described by Ilizarov (Citation1987), using an external ring fixator to perform distraction osteogenesis, is well known and widely used. However, it is a common experience that the treatment time in the fixator is long—even if the increase in healing time is not proportional to the lengthening distance of the callotasis zone, at least for moderate lengthening (Fischgrund et al. Citation1994). In addition, the method is associated with many problems (Paley Citation1990, Velazquez et al. Citation1993, Kristiansen and Steen Citation1996).
The Taylor spatial frame (TSF) is a relatively new versatile external ring fixator that can enable accurate corrections in reconstructive surgery. Preoperative planning, with definition of the center of rotation of angulation (CORA) of the deformity (Paley et al. Citation1994), is essential in deformity correction and is used with both devices. The TSF is more flexible, however. It does not require exact construction of hinges and precise mounting of the ring fixator (Taylor Citation2000). Two rings are connected by 6 telescopic rods (struts) at oblique directions, at special universal joints. This hexapod system allows correction of multiple angular and translational deformities by adjustment of the length of the struts only. Comparable configurations of the TSF and the Ilizarov external fixator (IEF) have different mechanical characteristics (Taylor Citation2002) which may influence the clinical results.
We present the results of our first 20 cases of monofocal tibial lengthening with the TSF and compare these with the results of monofocal tibial lengthening performed with the IEF.
Patients and methods
During the period October 2000 through April 2004, we operated 20 tibial deformities in 20 patients (11 males) with TSF and monofocal osteotomy. The indications for operation were various congenital or acquired deformities (). All patients were operated by two of the authors, with the first author as the first surgeon. The results of these operations were compared with the results of 27 tibial monofocal and monolateral osteotomies in 27 patients (16 females) with the IEF performed during the period 1993–1998 (Kristiansen and Steen Citation2002).
Table 1. Indications for 47 cases of tibial lengthening in 47 patients
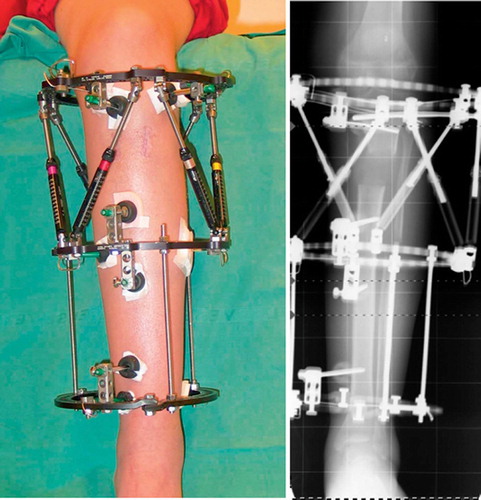
TSF lengthening was performed in the proximal metaphysis in 16 tibiae and distally in 4. The indications for TSF were shortening combined with multiplanar deformities including axial rotation. Correction of axial rotation may result in translational deformity due to eccentric localization of the bone in ring fixators. This problem is solved with the TSF by including mounting parameters in the calculation of reconstruction files using the internet-based software (www.spatialframe.com). The frame was constructed with 2 TSF rings with outposts, or 2 TSF rings with an additional Ilizarov ring (). Each fragment was fixed with 2 wires and 2 or 3 half-pins.
Figure 1. Tibial lengthening by use of proximal metaphyseal osteotomy and application of the Taylor spatial frame with an additional distal Ilizarov ring. Clinical view (A) and standing radiograph (B). The images were taken 3 weeks after end of distraction (10 weeks postoperatively). They show parallel rings and a lengthening of 43 mm.
Ilizarov lengthening was performed in the proximal metaphysis in 24 segments, and distally in 3. The frame was constructed with 3 rings and mounted with 7 Kirschner wires (3 wires in the ring on the metaphyseal side of the osteotomy and 2 wires in each of the other rings). Both in TSF and in IEF, the fibula was cut with an oblique mid-diaphyseal osteotomy and the segments were transfixed to the tibia both proximally and distally.
In both methods, the wires were tensioned to 1,080 N. In the proximal tibial metaphysis, we used the Gigli saw osteotomy technique. In the distal metaphysis, a corticotomy was performed with multiple cortical drill holes. Then the bone was cut with a curved chisel, taking care to protect the medullary cavity and vessels.
In all patients, daily distraction started at day 7 postoperatively and full weight bearing was allowed immediately. Lengthening was performed at a rate of 0.75 mm/day or 1 mm/day. In cases with shortening and additional deformity, lengthening and axial correction were started simultaneously by asymmetric distraction.
Oral antibiotics were given if superficial pin track infection occurred. The distraction and consolidation process in the lengthening zone were checked regularly and complications recorded. Bone grafting was performed as an additional procedure during the consolidation period if no new bone formation was seen on radiographs during a 12-week observation period. The external fixator was removed when symmetric callus and cortex on at least 3 sides were seen on biplanar radiographs. The lengthening index (LI) was calculated as months in the frame per cm lengthening (Paley Citation1990, Fischgrund et al. Citation1994).
Statistics
Averages are expressed as arithmetic means, and dispersion as 1 SD or range. Differences between TSF and IEF lengthening osteotomies were evaluated with ANOVA, adjustment for age with ANCOVA, a value of p < 0.05 being considered statistically significant.
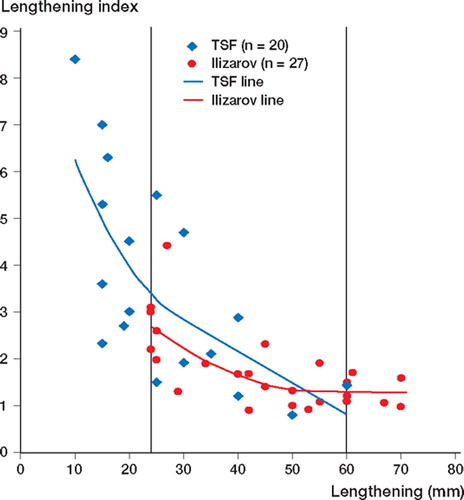
For graphical illustration, the data from both groups were entered into a multiphase best-fit model using software from SAS Institute Inc. (Cary, NC). The changing point for each group was calculated first and then the two curves were estimated using a maximum likelihood method. The curves for both groups were best-fitted by a quadratic-linear function ().
Results
There was a statistically significant difference between the ages of the patients undergoing the two treatments (mean 31 and 17 years for mono-focal lengthening by TSF and IEF, respectively; p < 0.001) (). However, within the overlapping zone, the average age was 16.8 (7–31) and 17.8 (4–48) years in the TSF and IEF groups, respectively (ns).
Table 2. Data in 47 patients with monofocal tibial lengthening
The average lengthening of 2.5 (0.5–6.0) cm by TSF was significantly different from the IEF osteotomies, which had a mean lengthening of 4.5 (2.4–7.0) cm (p < 0.001, ).
Table 3. Results following tibial lengthening of 47 segments in 47 patients by use of 20 Taylor spatial frame (TSF) and 27 Ilizarov external fixator (IEF) procedures. Values are mean, SD (range)
To evaluate the results of comparable lengthening distances, the segments were divided into 3 subgroups based on the overlapping zone (regarding lengthening distance): group 1 with lengthening of < 24 mm (TSF procedures only; n = 11); group 2 with lengthening of 24–60 mm (overlapping zone involving 9 TSF and 23 IEF; n = 32); and group 3 with lengthening of < 60 mm (IEF procedures only; n = 4).
With increasing lengthening distance, the average LI decreased significantly from 5.3 in short lengthenings to 1.3 in long lengthenings (p < 0.001, ). In the subgroup representing both methods with overlapping lengthening distance intervals (group 2), the LI was different from that of group 1 (p < 0.001), but not from that of group 3 (p = 0.3). Within group 2, both the lengthening distance (3.7 vs. 4.2; p = 0.4) and the LI (2.4 vs. 1.8; p = 0.2) of the segments operated with TSF were not statistically different from those operated with IEF.
There was no difference between the methods regarding the overall numbers of minor or major complications, additional surgeries, and number of segments where planned lengthening and axial correction were achieved (). However, the number of segments with reduced callus formation requiring bone transplant was higher in the TSF group, and the number of joint contractures requiring surgery or/ and deep pin track infections was higher in the IEF group ().
Table 4. Complications in 47 cases of tibial lengthening
Discussion
The Taylor spatial frame is a new and unique external ring fixator based on the Ilizarov principle. Its major advantage is the accuracy of the correction due to the “hexapod system” (Seide et al. Citation1999, Paley Citation2002). To date, only a few papers dealing with the TSF have been published (Rozbruch et al. Citation2002, Feldman et al. Citation2003a, Citationb, Sluga et al. Citation2003).
Mechanical properties of the TSF apparatus have been presented in the textbook of deformity correction by Dror Paley (Paley Citation2002). Compared with IEF, the TSF is 1.1 times stiffer in axial compression, 2.0 times stiffer in bending, and 2.3 times stiffer in torsion. In our material, the use of half pins in TSF indicates an even stiffer frame compared to IEF.
Both the TSF and IEF materials represent our first experience of each method. The overall average LI in the TSF and IEF groups was significantly different, with values of 4.0 and 1.7 months/cm (). The average lengthening was significantly less in the TSF group than in the IEF group, and the LI is known to be increased in smaller lengthenings (Kristiansen and Steen Citation2002). To our knowledge there has been only 1 report concerning LI in TSF (involving 5 patients) (Sluga et al. Citation2003). The authors found high LI (3.2 months/cm) in 1 patient with lengthening of 17 mm and low LI (1.2–1.7 months/cm) in 4 patients with lengthening of 67–72 mm. This is similar to our results with TSF and IEF (). Ideally, comparison of LI between the TSF and IEF monofocal procedures in lengthening of the tibia should only be performed between patients with similar lengthening distances. In the interval of overlapping lengthening (2.4–6.0 cm), the average LI was 2.4 months/cm and 1.8 months/cm in the TSF and IEF subgroups (). This difference in LI between TSF and IEF was not statistically significant (p = 0.17).
The average age in the TSF group was almost the double, and may have contributed to an increase in the LI and the number of segments with reduced callus formation needing bone grafting, as age is an important factor in determining the total treatment time (Fischgrund et al. Citation1994). In addition to the age difference, the TSF group mainly consisted of mal-unions (12/20 TSF vs. 7/27 IEF) which could be expected to lead to a disturbance in the bone/soft tissue conditions and may thus have resulted in increased LI ().
Major and minor complications occurred in both groups (). We experienced 4 segments with reduced callus formation requiring bone transplant and 3 segments with fracture after frame removal in the TSF group, but only 1 segment of each category in the IEF group. Disturbed bone and soft tissue conditions in malunions may also have contributed to a higher number of segments with reduced callus formation requiring bone graft and fractures of the regenerate after frame removal in the TSF group (7/20). 4 of these 7 patients were among the 12 TSF patients with preoperative mal-unions. In the IEF group, none of the 2 patients with reduced callus formation and fracture were among the patients with preoperative malunion. 1 of the 4 TSF patients with reduced callus formation was a smoker—which may have been an additional factor in this case (W-Dahl and Toksvig-Larsen Citation2004). 3/20 cases in the TSF group and 2/27 in the IEF group had no predisposing conditions that might explain the complications.
Joint contracture requiring operative treatment was found in the IEF group only. As joint contracture is associated with longer lengthening distances (Paley Citation1990), this is to be expected. In addition to long treatment time, the amount of lengthening may explain the high number of deep pin tract infections found in the IEF group only, as skin necrosis around the pins and wires is more frequent in cases of long lengthening.
In conclusion, the LI and complication rate when using TSF are similar to those of IEF, and the use of TSF does not represent any improvement regarding these parameters. However, in our hands the TSF is a versatile instrument for correction of 6-axis deformities—including rotational and translational deformities without (re)construction of hinge planes—and to perform residual adjustments.
No competing interests declared.
Contributions of authors
The original idea to the study was conceived by the two first authors who also operated the patients, collected the data and performed the data analysis, including statistical evaluation in cooperation with a professional statistician. All three authors contributed equally in the process of developing study design, interpretation of results, decision making on content and paper write-up, and revision of final draft.
- Feldman D S, David S, Shin S S, Madan S S, Koval K J. Correction of tibial malunion and nonunion with six-axis analysis deformity correction using the Taylor spatial frame. J Orthop Trauma 2003a; 17(8)549–54
- Feldman D S, Madan S S, Koval K J, van Bosse H JP, Bazzi J, Lehman W B. Correction of tibia vara with six-axes deformity analysis and the Taylor spatial frame. J Pediatr Orthop 2003b; 23(3)387–91
- Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop 1994, 301: 31–7
- Ilizarov G A. The principles of the Ilizarov method. Bull Hosp Joint Dis 1987; 48(1)1–11
- Ilizarov G A. Transosseous osteosynthesis. First ed. Springer Verlag, Berlin Heidelberg New York 1992
- Kristiansen L P, Steen H. The Ilizarov external fixator and method. Treatment of congenital and acquired deformities. Norwegian Tidsskr Nor Lægeforen 1996; 116(10)1216–8
- Kristiansen L P, Steen H. Reduced Lengthening index by use of bifocal osteotomy in the tibia. Comparison of monofocal and bifocal procedures with the Ilizarov external fixator. Acta Orthop Scand 2002; 73(1)93–7
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 1990, 250: 81–104
- Paley D. Principles of deformity correction. Springer-Verlag, Berlin Heidelberg NewYork 2002
- Paley D, Herzenberg J E, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994; 25(3)425–65
- Rozbruch S R, Helfet D L, Blyakehr A. Distraction of hypertrophic nonunion of tibia with deformity using Ilizarov/Taylor spatial frame. Report of two cases. Arch Orthop Trauma Surg 2002; 122: 295–8
- Seide K, Wolter D, Kortmann H-R. Fracture reduction and deformity correction with the hexapod Ilizarov fixator. Clin Orthop 1999, 363: 186–95
- Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: Two stage correction using the Taylor spatial frame. J Pediatr Orthop B 2003; 12(2)123–8
- Taylor J C. Six-axis deformity analysis and correction. In: jPrinciples of deformity correction. D Paley. Springer-Verlag, Berlin Heidelberg NewYork 2002
- Velazquez R J, Bell D F, Armstrong P F, Babyn P, Tibshirani R. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg (Am) 1993; 75(8)1148–56
- W-Dahl A, Toksvig-Larsen S. Cigarette smoking delays bone healing. A prospective study of 200 patients operated on by the hemicallotasis technique. Acta Orthop Scand 2004; 75(3)347–51
- www.jcharlestaylor.com, 2000, Taylor J C. Correction of general deformity with Taylor spatial frame.
- www.spatialframe.com, 2004, Smith & Nephew, Taylor Spatial Frame Web Software Version 3.0.