Abstract
We treated 4 female patients (mean age 80) with complex intraarticular acute fracture of the distal humerus with a Kudo humeral component, i.e. a hemiarthroplasty. All fractures were considered impossible to treat with open reduction and internal fixation. At mean 10 (3–14) months, 3 patients had an excellent result and 1 a good result according to the Mayo elbow performance score. We conclude that a hemiarthroplasty may be a valuable alternative in eldery patients with complex fractures of the distal humerus.
For the past few years, semiconstrained total elbow arthroplasty (TEA) has been reported as an acceptable treatment for fractures in elderly patients in whom stable internal fixation and early mobilization are difficult due to poor bone stock and severe comminution (Garcia et al. Citation2002, Frankle et al. Citation2003, Kamineni and Morrey Citation2004).
The concept of elbow hemiarthroplasty (HA) is not new, but has been confined to either case reports (Shifrin and Johnsson Citation1990) or in patients with rheumatoid arthritis (Swoboda and Scott Citation1999). Hemiarthroplasty for fracture treatment was briefly mentioned by Gramstad et al. (Citation2005), but no results were reported. Here we report our preliminary experiences of HA in 4 patients using the Kudo humeral component (Biomet Inc., Warsaw, IN, USA).
Patients and methods
During the period November 2004 through October 2005 we operated on 4 female patients, average age 80 (79–89) years, with distal humerus fractures. All patients were living at home and were independent. The inclusion criterion was a non-reconstruc-table fracture, e.g. a low transcondylar fracture with severe comminution (OTA 13.C2/C3).
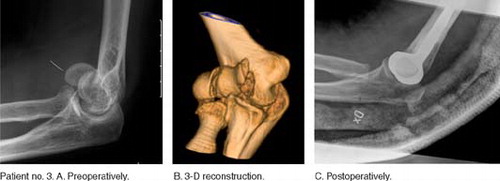
Preoperative evaluation was based on conventional radiography and CT with 3-D reconstruction (Figure). 1 patient had a fracture extension into the lateral column, 1 into the medial column, and 2 into both columns. A dorsal standard approach with triceps split was used in all 4 patients (Sanches-Sotelo et al. Citation2001). The final decision to reconstruct or replace with a hemiarthroplasty was taken after surgical exploration of the fracture.
We used the Kudo humeral component in all 4 patients. The main reason for selecting this prosthesis was primarily long experience of this implant when used as a TEA. In addition, when this study was started there was no commercially available humeral component specially designed for hemiarthroplasty on the market.
The Kudo humeral component is not designed for use as an HA. There is no radiohumeral articulating surface and the ulnohumeral surface is designed to fit to the olecranon component when used as a semiconstrained total arthroplasty. Thus, the radial head was removed through the same dorsal approach in all 4 patients in order to reduce the risk of radiohumeral impingement.
The initial removal of fracture fragments and debridement was conservative and completed in successive steps, paying special attention to preservation of the collateral ligaments. Any fracture extensions into the columns were temporarily stabilized with appropriate methods. A trial prosthesis was then inserted. The stability of this prosthesis depends on intact ligament structures. Thus, the correct positioning of the prosthesis in an isometric position relative to the collateral ligaments is of utmost importance, not only for stability but also for functional elbow flexion.
After the appropriate trial prosthesis had been selected, the definitive implant was cemented in a correct rotational position, e.g. 5–7° of internal rotation. All column fractures were stabilized with K-wires which were inserted while the cement was still soft. After reconstruction of the triceps using osteosutures, the wound was closed in layers. Active exercises were started within 48 h, supervised by a physiotherapist. A splint was worn between exercise sessions for the first four weeks after the operation, and flexion beyond 120° and extension against resistance was not allowed to protect the triceps repair. In the 3 patients with column fractures, active flexion/extension exercises were postponed to 6 weeks postoperatively.
Results
All incisions healed uneventfully. At follow-up after an average of 10 (3–14) months, all patients were back in their homes and living independently. None had pain at rest or when using the extremity for daily activities. 2 patients reported a slight reduction in muscle force. According to the Mayo elbow performance score (Morrey Citation2000), 3 had excellent outcome and 1 had good outcome (Table).
Motion (degrees) on follow-up
Discussion
Nonoperative treatment of these fractures often results in a healed fracture with extension/flexion contracture or nonunion (Zagorski et al. Citation1986), whereas open reduction and internal fixation carry a high risk of complications and inferior function, particularly in elderly patients with a complex fracture and poor bone stock (Frankle et al. Citation2003). TEA has proven to be an attractive solution in older patients with this type of fracture (Cobb and Morrey Citation1997, Garcia et al. Citation2002, Frankle et al. Citation2003).
Parsons et al. (Citation2005) described the use of a specially designed humeral prosthesis in a series of 11 patients. 4 of these were acute fractures and the preliminary results were encouraging. However, 3 patients developed symptomatic hardware from the osteotomy tension band, requiring removal, and 1 was considered for conversion to a total elbow arthroplasty due to ulnohumeral osteoarthrosis. The youngest patient in their series was 46 years old. The authors concluded that an HA is perhaps a better alternative than TEA in young patients with non-reconstructable distal humerus fractures, the main reason being the risk of aseptic loosening from polyethylene wear. We do not fully agree with these conclusions but would rather consider an HA in an elderly patient with low to moderate functional demands, and consequently a low anticipated risk of future revisions. The design of the Kudo humeral component is, however, not ideal and may lead in the long term to ulnohumeral erosions. However, this complication and the need for revision among these elderly patients with low to moderate functional demands are probably unlikely. Furthermore, a hemiarthroplasty should not be considered unless ligament stability can be achieved either by preservation or reconstruction.
We do not recommend this technique for younger patients. In our experience, the development of modern fracture stabilization implants (O'Driscoll Citation2004) has made it possible to provide stable internal fixation and early mobilization in most complex fractures in younger patients.
- Cobb T K., Morrey B F. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. J Bone Joint Surg (Am) 1997; 79(6)826–32
- Frankle M A, Herscovici D, DiPasquale T G, Vasey M B, Sanders R W. A comparison of open reduction and internal fixation and primary elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 66. J Orthop Trauma 2003; 17: 473–80
- Garcia J A, Mykula R, Stanley D. Complex fractures of the distal humerus in the eldery. The role of total elbow replacement as a primary treatment. J Bone Joint Surg (Br) 2002; 84(6)812–6
- Gramstad G D, King G J W, O'Driscoll S W, Yamaguchi K. Elbow arthroplasty using a convertible implant. Tech Hand and Upper Extrem Surg 2005; 9(3)153–63
- Kamieni S, Morrey B F. Distal humeral fractures treated with noncustom total elbow replacement. J Bone Joint Surg (Am) 2004; 86: 940–7
- Morrey B F. The elbow and its disorders. Philadephiathird ed., W B Saunders, 2000; 82
- O'Discoll S W. Optimizing stability in Distal humerus fracture fixation. J Shoulder Elbow Surg 2004, Suppl 1: 14
- Parsons M, O'Brien R, Hughes J. Elbow hemiarthroplasty for acute and salvage reconstruction of intra-articular distal humerus fractures. Tech Hand and Upper Extrem Surg 2005; 6(2)87–97
- Sanches-Sotelo J, Torchia M E, O'Driscoll S W. Principle-based internal fixation of distal humerus fractures. Tech Hand and Upper Extrem Surg 2001; 5: 179–87
- Shifrin P G. Elbow arthroplasty with 20-years follow-up study. A case report and literature review. Clin Orthop 1990, 254: 128–33
- Swoboda B, Scott R D. Humeral hemiarthroplasty of the elbow joint in young patients with rheumatoid arthritis; a report on 7 arthroplasties. J Arthriplasty 1999; 14: 553–9
- Zagorski J B, Jennings J J, Burkhalter W E, Uribe J W. Comminuted intraarticular fractures of the distal humeral condyles. Surgical vs. nonsurgical treatment. Clin Orthop 1986, 202: 197–204