Case report
2 years after a first episode of lumbosciatica, pain recurred in a 57-year-old man who now had a positive Trendelenburg sign, lack of ankle jerk, impaired foot dorsiflexion, L5 and S1 paresthesias, and a Lasègue sign at 30° with positive Bragard manoeuvre on the right side.
MRI of the complete neural axis showed a tumor posterior in the L5 vertebral body extending mediolaterally into the spinal canal, compressing the right L5 and S1 nerve roots (). The most probable radiological diagnosis was a chordoma. As the patient refused major surgery (spondylectomy), both the epidural mass and the vertebral tumor were totally removed by microsurgery through bilateral laminotomies at L4/L5 and L5/ S1. The tumor was completely encapsulated. It had not penetrated the posterior longitudinal ligament. Apart from the foot paresis and S1 hypesthesia, the patient recovered fully. The histological diagnosis was a chordoma.
Figure 1. Sagittal (A) and axial (B) MRI after intravenous application of gadolinium. The L5 tumor protruded into the epidural space where it compressed the right L5 nerve root.
6 months after surgery, MRI showed recurrence of the tumor. It was confined to the vertebral body; however, posteriorly it was in contact with the thecal sac (). The patient now agreed to undergo spondylectomy. Angiography of the tumor revealed only slight vascularization; even so, it was embolized before surgery.
Figure 2. Sagittal (A) and axial (B) T2-weighted MRI images showing tumor recurrence (arrow) after posterior resection.
Total L5 spondylectomy
The gastrointestinal tract was completely washed. A uretheral catheter was introduced to monitor the patient and to facilitate exposure. Perioperative antibiotics were given. We did not use a cell saver to avoid tumor dissemination. Under general anesthesia, the patient was put prone with physiological lumbar lordosis. Using microtechniques, we performed an L5 laminectomy with complete pedicle resection down to the vertebral body, and resection of the superior and inferior L5 facets and the transverse processes. After complete exposure of neural structures, the epidural part of the chordoma was removed. Its surface within the vertebral body was continuously covered with bone wax to prevent dissemination of tumor cells (Abe et al. Citation2000). Finally, the posterior longitudinal ligament was horizontally transsected twice. A bony bridge was created between the inferior articular processes of L4 and the superior one of S1 on both sides, using two autologous co rtico-cancellous bone grafts (posterior iliac crest). The right graft was anchored with a screw, whereas the left one was firmly jammed in between the articular processes without instrumentation. Thereafter, we performed internal L4 to S1 fixation by use of pedicle screws and rods (titanium). Two transverse devices—one in compression and one in distraction—were used to reinforce the construct (Cotrel-Dubousset (CD) Horizon; Sofamor Danek, Memphis TN) ().
Figure 3. Anteroposterior (A) and lateral (B) radiographs showing circular reconstruction after L5 total spondylectomy.
The patient was put supine with abducted legs. Through a lower midline incision, a retroperitoneal approach to the lumbosacral angle was created as previously described (Markwalder et al. Citation2003, Wenger et al. Citation2006). The great vessel’s bifurcations were retracted cephalad. Total discectomies of L4/L5 and L5/S1 were performed. We detached the psoas muscles bilaterally, resulting in complete isolation of the L5 vertebral body. During extraction of the L5 VB, a small laceration of the left iliac vein occurred, which was sutured. Thereafter, a lordotic telescope-cage (X-tenz; DePuy-AcroMed, Leeds, UK) filled with a mixture of cancellous bone (posterior iliac crest) and homologous bone graft (DynaGraft; GenSci, OrthoBiologics Inc., Irvine, CA) was put in place. It was elongated until there was firm contact between the cage and the lower endplate of L4 and the upper endplate of S1. Prior to introduction of the cage, both endplates were scratched until smooth bleeding of the cortical layer occurred to facilitate subsequent bony fusion.
The operation lasted 11 h. Most blood loss was due to epidural bleeding. 10 Ec units, 10 units of fresh frozen plasma and 1 unit of thrombocytes were substituted. Extubation was delayed because of low core temperature.
A postoperative thrombosis of the left leg (vascular retraction during surgery and/or laceration of the vein) was treated by anticoagulation. The patient wore a removable rigid plastic corset for 4 months and resumed work after 5 months. After 6 months, we found ossification within the cage and thus solid bony interbody fusion in physiological lordosis ().
Third operation and radiation therapy
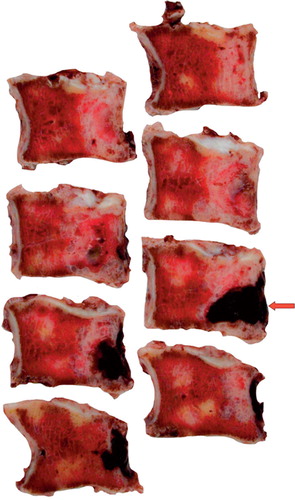
6 months after spondylectomy, MRI showed recurrence of the tumor in the epidural space between the right CD rod and the cage (). Radiographs of the lungs and a 99mTc-DPD-scintigraphy of the skeleton revealed no signs of metastasis. Using microtechniques, this mass was completely removed through a posterior approach (). 2 months later, percutaneous radiation therapy was initiated (66 Gy (protron beam) within 6 weeks) (Thieblemont et al. Citation1995, Boriani et al. Citation1996, Cheng et al. Citation1999, Baratti et al. Citation2003). 1.5 years after the third operation, the patient continued to suffer from foot paresis and S1 hypesthesia. He had no signs of tumor recurrence or dissemination.
Discussion
Chordomas have a high propensity for local recurrence and may also give rise to metastases (Markwalder et al. Citation1979, Bjornsson et al. Citation1993, Bergh et al. Citation2000). Only a wide resection of a chordoma within the vertebral body is associated with a reasonable chance of cure (Cheng et al. Citation1999, Boriani et al. Citation1996, Bosma et al. Citation2001). We involuntarily contribute to this opinion because our patient, who initially refused major surgery, experienced local recurrence shortly after posterior resection. Even (delayed) total L5 spondylectomy was followed by a local recurrence. However, after the third operation and radiation therapy, he remains free of disease (3 years after diagnosis).
In our opinion, the handling of the great vessels and avoidance of blood loss through epidural (Bosma et al. Citation2001) and small vessels within the psoas muscle attachments are the most important challenges when doing a spondylectomy. After clip ligation and transsection of the sacralis mediana artery and vein, a combination of sharp and blunt dissection in the caudad to cephalad direction along or even under the anterior longitudinal ligament is required to allow retraction of the vessels. This has to be done in a more extensive manner than in monosegmental anterior lumbar interbody fusion or total disc arthroplasty procedures (Wenger et al. Citation2005) because the L5 body (the largest vertebral body) has to be removed altogether. After total L4/L5 and L5/S1 discectomies with transsection of the posterior longitudinal ligament, clipping of segmental vessels and bilateral detachment of the psoas muscles, the L5 VB is completely isolated and extracted.
Anterior vertebral body reconstructions are often a “tinkering around” with different implants. In recent years the following have been used: bicortical iliac crest grafts (Benoit et al. Citation1990), allograft and anterior Goutallier plate (Boriani et al. Citation1996), fibular allograft (Tomita et al. Citation1997), tricortical iliac crest grafts (Bosma et al. Citation2001), chest tube filled with methylmethacrylate (Marmor et al. Citation2001) or an apatite-wollastonite glass ceramic vertebral prosthesis or a titanium mesh cage filled with iliac bone chips and augmented with Zielke or Kaneda instrumentation (Abe et al. Citation2000, Citation2001), and mesh cages which have to be cut to obtain physiological regional lordosis. These devices are mostly not designed for L5 reconstruction and do not provide reliable primary stability. We believe that telescopic lordotic cages are the most reliable and easy-to-use implants (alternatives: Synex System from Synthes GmbH, Oberdorf BL, Switzerland, and LIFT VB from Sofamor Danek, Memphis TN, both of which must be filled with bone and/or its substitute to induce bony fusion). Due to the exact adjustment of height, the lordosis angle and the broad design, they provide primary stability in correct alignment. This is why we did not incorporate additional levels in the posterior osteosynthesis. In our patient, solid fusion in the anterior and posterior weight bearing axes allowed resection of the second recurrence without further destabilization.
Total L5 spondylectomy is a surgical challenge. However, as surgeons increasingly perform anterior lumbar interbody fusions and total disc arthroplasties, their experience of this type of major surgery will grow significantly. We strongly advocate primary total spondylectomy for solitary vertebral body chordoma.
Contributions of authors
MW assisted in the operation and wrote the article. JT assisted in the operation and gave writing advice. RM performed all the pathological examinations and gave writing advice. T-MM senior author who performed the operation and gave writing advice.
- Abe E, Sato K, Tazawa H, Murai H, Okada K, Shimada Y, Morita H. Total spondylectomy for primary tumor of the thoracolumbar spine. Spinal Cord 2000; 38: 146–52
- Abe E, Kobayashi T, Murai H, Suzuki T, Chiba M, Okuyama K. Total spondylectomy for primary malignant, aggressive benign, and solitary metastatic bone tumors of the thoracolumbar spine. J Spinal Disord 2001; 14: 237–46
- Baratti D, Gronchi A, Pennacchioli E, Lozza L, Colecchia M, Fiore M, Santinami M. Chordoma: natural history and results in 28 patients treated at a single institution. Ann Surg Oncol 2003; 10: 291–6
- Benoit J, Videcoq P, Hardy P, Durigon M. Spinal chordoma. A case report on chordoma of the L3 vertebra. Rev Rhum Mal Osteoartic 1990; 57: 557–61
- Bergh P, Kindblom L G, Gunterberg B, Remotti F, Ryd W, Meis-Kindblom J M. Prognostic factors in chordoma of the sacrum and mobile spine. A study of 39 patients. Cancer 2000; 88: 2122–34
- Bjornsson J, Wold L E, Ebersold M J, Laws E R. Chordoma of the mobile spine. A clinicopathologic analysis of 40 patients. Cancer 1993; 71: 735–40
- Boriani S, Chevalley F, Weinstein J N, Biagini R, Campanacci L, De Iure F, Piccill P. Chordoma of the spine above the sacrum. Treatment and outcome in 21 cases. Spine 1996; 21: 1569–77
- Bosma J J, Pigott T J, Pennie BH, Jaffray D C. En bloc removal of the lower lumbar vertebral body for chordoma. Report of two cases. J Neurosurg (Spine 2) 2001; 94: 284–91
- Cheng E Y, Özerdemoglu R A, Transfeldt E E, Thompson R C, Jr. Lumbosacral chordoma. Prognostic factors and treatment. Spine 1999; 24: 1639–45
- Markwalder T M, Markwalder R V, Robert J L, Krneta A. Metastatic chordoma. Surg Neurol 1979; 12: 473–8
- Markwalder T M, Wenger M, Elsig J P, Laloux E. The Wilhelm Tell technique for anterior lumbar interbody fusion. Technical note. J Neurosurg (Spine2) 2003; 98: 222–5
- Marmor E, Rhines L D, Weinberg J S, Gokaslan Z L. Total en bloc lumbar spondylectomy. Case report. J Neurosurg (Spine2) 2001; 95: 264–9
- Thieblemont C, Biron P, Rocher F, Bouhour D, Bobin J Y, Gerard J P, Blay J Y. Prognostic factors in chordoma: role of postoperative radiotherapy. Eur J Cancer 1995; 31A: 2255–9
- Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine 1997; 22: 324–33
- Wenger M, Markwalder T M. A novel surgical treatment of lumbar disc herniation in patients with long-standing degenerative disc disease. J Neurosurg Spine 2005; 2: 515–20
- Wenger M, Vogt E, Markwalder T M. Double-segment Wilhelm Tell technique for anterior lumbar interbody fusion in unstable isthmic spondylolisthesis and adjacent segment discopathy. J Clin Neurosci 2006; 13: 265–9