Abstract
Background Acetabular screw cups seem to give high primary stability. We analyzed the migration and loosening behavior of a first-generation screw cup in a longterm follow-up.
Patients and methods We examined 92 uncemented titanium alloy conical screw cups prospectively. Implant migration was assessed with a digital high-precision method (EBRA) with an accuracy of 1.0 mm.
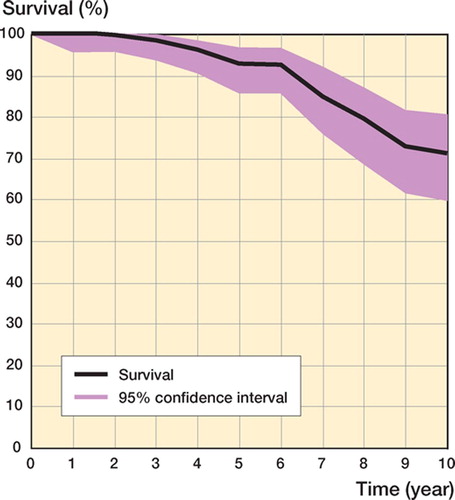
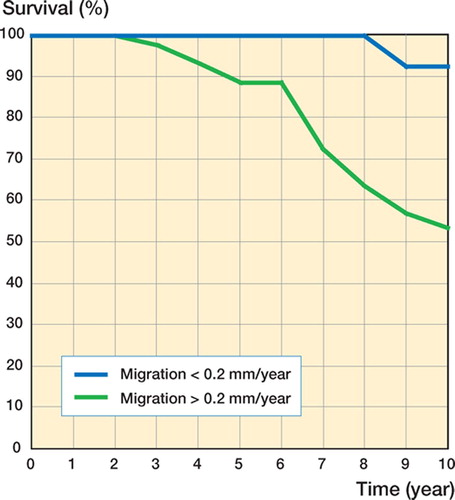
Results After mean 11 (0.5–18) years, 87 patients were available for examination and 5 patients had died. 32 implants had been revised and 7 cases showed radiographic evidence of loosening. The 10-year survival rate was 71%. Migration of more than 1 mm occurred in 53 hips. Implant survival was strongly associated with an annual migration of greater than 0.2 mm.
Interpretation The long-term behavior of this cup is not satisfactory. In spite of extraordinarily high primary implant stability, secondary osseointegration of this cup often fails. The annual migration rate represents a valid parameter for prediction of implant survival.
Acetabular screw cups give the intraoperative impression of high primary stability and have been widely used in Europe (Lord and Bancel Citation1983, Parhofer and Ungethum Citation1984, Refior et al. Citation1988, Thabe et al. Citation1993, Blasius et al. Citation1994). The disadvantages of some screw-in cup systems became evident at the end of the eighties, however (Apel et al. Citation1989, Engh et al. Citation1990, More et al. Citation1992, Seral et al. Citation1992, Gouin et al. Citation1993, Fox et al. Citation1994, Seelen et al. Citation1995, Fernandez-Gonzalez et al. Citation1997, Volkmann et al. Citation1999, Bizot et al. Citation2000, Kubo et al. Citation2001). In a meta-analysis of the literature prior to 1992, a higher loosening rate (3.8%) was found for the first-generation screw sockets than for spherical press-fit cups (1.4%) and cemented cups (1.6%) (Yahiro et al. Citation1995).
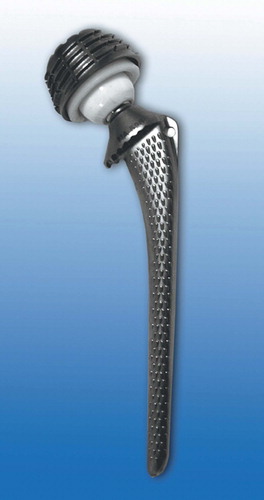
In this series we used a Parhofer-Monch (PM)-type screw cup (Aesculap, Tuttlingen, Germany) between 1982 and 1991 (). Its conical body is made of a titanium-aluminum-vanadium alloy with a smooth surface. In Europe, the system was used in more than 60,000 patients. After good early results (Parhofer and Ungethum Citation1984, Krodel and Refior Citation1988, Wolf et al. Citation1988), the mid-term results turned out to be moderate at best (Reichelt and Botterer Citation1993, Dickob and Martini Citation1996, Karches et al. Citation1996) with a 6-year survival rate of 88%.
Figure 1. The Parhofer-Monch (PM) prosthesis. The conical threaded cup is made of titanium-aluminum-vanadium alloy with a smooth surface, resembling a typical design of the first generation of screw-rings.
Our long-term follow-up of this cup allows for characterizing its loosening mechanism. An analysis of 20 loosened Bi-Metric cups has shown initial radiolucencies at the tip of the acetabular thread prior to the appearance of continuous radiolucent lines, and implant migration measurable on conventional radiographs (Tallroth et al. Citation1993). In contrast, in one radiostereometry (RSA) study concerning screw sockets, a migration of 1 mm was found in all 20 patients examined for a Link type-V implant after a follow-up time of 2 years (Snorrason and Kärrholm Citation1990). Our knowledge concerning the migration behavior of screw cups over longer periods is limited. We have documented clinical results of the PM cup using a prospectively registered patient group. We used a digital measuring system with high accuracy (Ein-Bild-Roent-gen-Analyse; EBRA) to analyze the relationship between the migration behavior and implant survival over a 10-year period.
Patients and methods
Patients
From 1982 through 1991, we prospectively registered 81 patients who had had an uncemented PM conical screw cup (Aesculap, Tuttlingen, Germany) implanted in combination with 32-mm ceramic heads and conventional polyethylene liners. Inclusion criteria were age less than 60 years, normal life expectancy, absence of systemic bone disease (i.e. osteoporosis), place of living within a range of 50 km, and informed consent. In order to measure acetabular cup migration, at least 4 radiographs were needed. 11 other patients were added retrospectively because they had followed the study control intervals in our department on a volunteerly basis and thus had a sufficient number of radiographs. There was no selection bias operating here. Thus, 92 patients with an average age of 53 (33–60) were available for the study (53 males). The average BMI was 26 (19–35). The diagnoses were primary osteoarthritis (n = 60), dysplasia (n = 10), avascular necrosis (AVN) of the femoral head (n = 14), and other (n = 8).
Follow-up examinations
All patients were examined clinically and radiographically after an average postoperative time of 10.5 (0.5–18) years. The Harris hip score was determined. All patients were examined with a pelvic overview radiograph and a Lauenstein projection. Radiolucent lines and enhanced subchondral sclerosis surrounding the cup were assessed using the 3 zones of DeLee and Charnley (Citation1976).
Definition of loosening
Implants were classified radiographically as being stable or loosened using the criteria of Engh et al. (Citation1990). A prosthesis was considered to be loose when revision surgery had taken place, or when there were clear radiographic indications of migration. Clinical criteria for loosening were increasing pain in the groin and limp. Radiographic criteria of loosening were continuous radiolucencies around the cup in 2 of the 3 zones, progressive radiolucencies indicating probable instability, or measurable component migration of either 3 mm, a tilt of 8°, or a fracture of the implant. All cups defined as loose had clear signs of radiographic loosening. Infection was ruled out in these cups by a normal CRP or a negative aspiration of the joint.
Ein-Bild-Roentgen-Analyse (EBRA)
We used pelvic radiographs obtained 2 weeks postoperatively as the baseline radiographs for measurements. 491 pelvic overview radiographs (mean 5.3 images/implant) were measured. The radiographs were digitized using a 12-bit CCD scanner (256 shades of gray) and measured on the DiagnostiX 2048-base station (Pace-Systems, Freiburg, Germany). The maximum resolution was 2.5 line pairs/mm for a matrix size of 2048 × 2048. The digitized radiographs were saved as TIF data files and measured using the EBRA digital software, release 1999 (Dept. of Geometry, University of Innsbruck, Austria). The numerical results of cup migration in the x- and y-directions over time and their graphical representation were displayed using the program modules EBRAGRAF and SIMULGRAF (Dept. of Geometry, University of Innsbruck, Austria). EBRA accepts only pelvic radiographs within a range of 9° tilting in the ydirection and 6° in the x-direction. Using these parameters, a measurement accuracy of better than ± 1 mm has been reported (Ilchmann et al. Citation1992, Ilchmann Citation1997, Phillips et al. Citation2002). Thus, implant migration was defined as a change in implant position of more than 1 mm in the horizontal or vertical direction. Migration rates were calculated by dividing the amount of maximum migration by the observation time in years.
Statistics
All statistical analyses were done with SPSS for Windows version 10.0. The survival rate was determined with the help of life tables based on annual examinations. Comparison of the survival rates between the groups was carried out with the nonparametric log-rank test and confidence intervals were calculated according to Murray et al. (Citation1993). The Mann-Whitney U-test was performed to compare the migration of fixed and loosened implants at different time intervals. A p-value of < 0.05 was considered significant.
In order to determine the influence of several factors and variables, a Cox regression was performed. The following variables were included: sex, age, BMI, diagnosis, migration, and acetabular protrusion. The variables sex, diagnosis, migration, and acetabular protrusion were marked as categorial. The endpoint of the regression model was revision or loosening.
Results
Fate of the prostheses
At the time of our last evaluation 5 patients had died. In 1 of these, a revision of both components of the prothesis had been performed. In the 87 surviving patients, a revision of the acetabular component had been performed in 31 cases. 7 additional implants met the radiographic criteria for loosening. Revision surgery was recommended to all these patients. The remaining 53 patients showed no signs of loosening, based on radiographic or clinical criteria.
Clinical examination
The Harris score for the complete group improved from 48 ±(SD 13) points to an average of 74 (SD 5.8) points (range 24–100). Those patients who were not revised had a slightly higher Harris score of 78 (SD 4.9) points (p < 0.1). At their last examination, 79 of the 92 patients stated that they were satisfied with the result of the operation.
Radiographic examination
In DeLee and Charnley zone I (lateral segment of the cup), 45 cups showed no radiolucent lines and 47 components showed a radiolucent line of mean 0.8 (SD 0.2) mm. In zone II (central segment), 43 components showed no radiolucent line, while the radiolucent line in those demonstrating radiolucencies was 0.6 (SD 0.1) mm on average. 53 acetabular components had no radiolucent line in zone III (medial segment), while the other cups had a line of 0.8 (SD 0.2) mm on average. A continuous radiolucent line of 2 or 3 mm was observed in 2 implants with suspected loosening. An enhanced sclerosis could be seen for 30 implants in zone I, for 37 in zone II, and for 5 in zone III.
Survival analysis
The 10-year survival rate was 71% ().
EBRA
Analysis with the EBRA method could be performed in 81 of the 92 cases (88%) ().
Table 1. Loosening and migration of conical screw cups
Horizontal and vertical migration
Implant migration of fixed and loosened cups was compared at 2 and 10 years (). After 2 years, a mean migration of 0.3 (SD 0.3) mm in the horizontal (x-) direction was seen for stable cups while the loosened cups showed a migration of 0.7 (SD 0.8) mm (p = 0.05). For the vertical (y-) direction, the mean migration was 0.1 (SD 0.5) mm for the fixed implants and 1.2 (SD 2.9) mm for the loosened cups (p = 0.01). After 10 years, fixed implants had migrated 1.0 (SD 0.8) mm in the x-direction and loosened cups 1.8 (SD 1.0) mm (p < 0.001). In the y-direction, fixed implants showed a migration of 0.6 (SD 1.3) mm, and loosened cups migrated 3.8 (SD 5.8) mm (p < 0.001).
Figure 3. Bar diagram showing the horizontal and vertical implant migration (upper and lower panels, respectively). The migration (in mm) is depicted on the y-axis, and the results for fixed and loosened cups after 2 and 10 years are shown. The error bars represent one standard deviation. In both directions, significant differences between fixed and loosened cups can be traced.
Survival rate and implant migration
In order to evaluate the correlation between implant migration and loosening for both the migrated and non-migrated implant groups, we performed a survival analysis. The 10-year survival rate of the migrated implants was 61% and that of the nonmigrated implants was 89% (p = 0.002).
Survival rate and migration rate
The 10-year survival rate of the cups that migrated over 0.2 mm/year was 54%, while the survival of implants that migrated less than 0.2 mm/year was 93% (p < 0.001) ().
Cox regression
With the limited data available for the variables included in the Cox regression analysis, only migration showed a significant influence on the endpoint revision or loosening ().
Table 2. Cox regression with the endpoint revision or loosening
Discussion
For clinical screw cups, the 10-year survival rate of 71% must be regarded as poor even when considering the young patient age (mean 53 years) in this study. We measured migration by the EBRA method, which can be regarded as the most accurate measuring system using conventional radiographs. Different authors have found an accuracy of between ± 0.82 and 1.0 mm (Phillips et al. Citation2002), or between ± 0.27 and 0.39 mm compared to RSA (Ilchmann et al. Citation1992).
Tallroth et al. (Citation1993) found that radiolucent lines at the tips of the threads followed by circumferential radiolucent lines always appeared before a conventionally measured migration on plain radiographs of over 2 mm or a tilt of 4° was demonstrable. In contrast, Snorrason and Kärrholm (Citation1990) showed that all 20 Link type-V cups measured by RSA migrated over 1 mm within the first 2 years. Thus, migration is probably the same as late detection of early migration because of the use of conventional methods with lower sensivity. Implant migration is considered to be the consequence of deficient initial stability (Kärrholm et al. Citation1997).
Our results confirm that the high primary stability breaks down within the first 2 years. The radiolucent lines observed by Tallroth et al. (Citation1993) surrounding the threads and the whole implant should be considered a consequence of the migration of the implant rather than its cause. Also, in an animal model using a screw implant, the absence of definite osseointegration could be observed within the first 3 months postoperatively (Tooke et al. Citation1988).
Generally, early implant migration is thought to indicate poor long-term survival of a cup system. In a prospective study performed by Krismer et al. (Citation1996), it was shown that cups with a migration of over 1 mm within the first 2 years had a significantly higher rate of loosening in the course of 7 years. The predictive value of a migration of over 1 mm within 24 months for loosening after 7 years was stated to be over 70%. Also, our study confirms the predictive value of implant migration analysis. All the implants that had migrated within the first 2 years had also been revised within our observation period. This corresponds to the observations made for other cup systems (Stocks et al. Citation1995, Kärrholm et al. Citation1997, Stockl et al. Citation1999).
While a migration of 1 mm within the first 2 years appears to indicate poor osseointegration, there were also implants whose migration could not be detected before 2 years postoperatively. Even in the group with the stable, non-migrated implants, intraoperative loosening was found in 2 cases. In these 2 cases, however, revision surgery had not been performed until 108 months after primary surgery.
We found a highly significant correlation between migration and loosening. The 10-year survival rate of the migrated implants was 6%, while that of the non-migrated implants was 89%. This difference is impressive if one takes the annual migration of over 0.2 mm as a basis. Those implants migrating over 0.2 mm/year had a 10-year survival rate of 54%, and those migrating up to 0.2 mm/year had a 10-year survival of 93% (p < 0.001). Also, in the Cox regression, the variable “migration” had an influence on loosening and/or revision. With the limited number of datasets available, however, we cannot exclude the possibility that in a larger cohort, additional variables might also have an influence on loosening.
Due to the poor long-term results with the PM cup, it has been replaced successively (since 1987) by the Harris-Galante cup, which shows excellent long-term results (Clohisy and Harris Citation1999) and a low implant migration rate (Hendrich et al. Citation1997).
Contributions of author
CH: team leader. DA, US, HS: data collection and EBRA. SK, JMM: EBRA and statistics.
No competing interests declared.
- Apel D M, Smith D G, Schwartz C M, Paprosky W G. Threaded cup acetabuloplasty Early clinical experience. Clin Orthop 1989, 241: 183–9
- Bizot P, Banallec L, Sedel L, Nizard R. Alumina-on-alumina total hip prostheses in patients 40 years of age or younger. Clin Orthop 2000, 379: 68–76
- Blasius K, Weber U, Weiss M, Cotta H. Clinical and radiological results with the spherical Mecring as acetabulum prosthesis in hip joint diseases. Aktuelle Traumatol 1994; 24: 180–3
- Clohisy J C, Harris W H. The Harris-Galante porous-coated acetabular component with screw fixation. An average ten-year follow-up study. J Bone Joint Surg (Am) 1999; 81: 66–73
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 20–32
- Dickob M, Martini T. The cementless PM hip arthroplasty. Four-to-seven-year results. J Bone Joint Surg (Br) 1996; 78: 195–9
- Engh C A, Griffin W L, Marx C L. Cementless acetabular components. J Bone Joint Surg (Br) 1990; 72: 53–9
- Fernandez-Gonzalez J, Canosa S R, Garcia-Araujo C. Cementless total hip arthroplasty with a threaded acetabular cup. Int Orthop 1997; 21: 327–31
- Fox G M, McBeath A A, Heiner J P. Hip replacement with a threaded acetabular cup. A follow-up study. J Bone Joint Surg (Am) 1994; 76: 195–201
- Gouin F, Fechoz F, Passuti N, Sentucq-Rigal J, Bertrand O, Bainvel J V. Acetabulum without cement. Short-term results of a series of 112 threaded cups. Int Orthop 1993; 17: 65–72
- Hendrich C, Bahlmann J, Eulert J. Migration of the uncemented Harris-Galante acetabular cup: results of the einbildroentgenanalyse (EBRA) method. J Arthroplasty 1997; 12: 889–95
- Ilchmann T. Radiographic assessment of cup migration and wear after hip replacement. Acta Orthop Scand 1997, Suppl 276: 1–26
- Ilchmann T, Franzen H, Mjöberg B, Wingstrand H. Measurement accuracy in acetabular cup migration. A comparison of four radiologic methods versus roentgen stereophotogrammetric analysis. J Arthroplasty 1992; 7: 121–7
- Karches C, Hendrich C, Kramer C, Eulert J. Langzeitergebnisse zementfreier Hüftendoprothesen. Orthopädische Praxis 1996; 32: 228–32
- Kärrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop. 1997, 344: 94–110
- Krismer M, Stockl B, Fischer M, Bauer R, Mayrhofer P, Ogon M. Early migration predicts late aseptic failure of hip sockets. J Bone Joint Surg (Br) 1996; 78: 422–6
- Krodel A, Refior H J. Radiologic changes of the bones following cement-free implantation of hip joint prosthesis in inflammatory rheumatic diseases. Z Orthop Ihre Grenzgeb 1988; 126: 387–93
- Kubo T, Inoue S, Maeda T, Arai Y, Hirakawa K, Wu Y, Suehara H, Ogura T, Hirasawa Y. Cementless Lord total hip arthroplasty: cup loosening common after minimum 10year follow-up of 103 hips. Acta Orthop Scand 2001; 72: 585–90
- Lord G, Bancel P. The madreporic cementless total hip arthroplasty. New experimental data and a seven-year clinical follow-up study. Clin Orthop 1983, 176: 67–76
- More R C, Amstutz H C, Kabo J M, Dorey F J, Moreland J R. Acetabular reconstruction with a threaded prosthesis for failed total hip arthroplasty. Clin Orthop 1992, 282: 114–22
- Murray D W, Carr A J, Bulstrode C. Survival analysis of joint replacements. J Bone Joint Surg (Br) 1993; 75: 697–704
- Parhofer R, Ungethum M. Experiences with hip joint endoprosthesis model PM for cement free implantation. Z Orthop Ihre Grenzgeb 1984; 122: 790–7
- Phillips N J, Stockley I, Wilkinson J M. Direct plain radiographic methods versus EBRA-Digital for measuring implant migration after total hip arthroplasty. J Arthroplasty 2002; 17: 917–25
- Refior H J, Parhofer R, Ungethum M, Blomer W. Special problems of cementless fixation of total hip-joint endoprostheses with reference to the PM type. Arch Orthop Trauma Surg 1988; 107: 158–71
- Reichelt A, Botterer H. The PM-prosthesis. Z Orthop Ihre Grenzgeb 1993; 131: 532–8
- Seelen J L, Bruijn J D, Kingma L M, Bernoski F P, Bloem J L. Radiographic loosening of cementless threaded acetabular cups. No additional diagnostic value of arthrography in 30 patients. Acta Orthop Scand 1995; 66: 415–7
- Seral F, Villar J M, Esteller A, Vivar F G, Abad I, Martinez G M, Jorda E, Espinar E. Five-year follow-up evaluation of the noncemented press-fit titanium hip-joint endoprosthesis. Clin Orthop 1992, 283: 49–56
- Snorrason F, Kärrholm J. Primary migration of fully-threaded acetabular prostheses. A roentgen stereophotogrammetric analysis. J Bone Joint Surg (Br) 1990; 72: 647–52
- Stockl B, Sandow M, Krismer M, Biedermann R, Wimmer C, Frischhut B. Migration of the Duraloc cup at two years. J Bone Joint Surg (Br) 1999; 81: 51–3
- Stocks G W, Freeman M A, Evans S J. Acetabular cup migration. Prediction of aseptic loosening. J Bone Joint Surg (Br) 1995; 77: 853–61
- Tallroth K, Slätis P, Ylinen P, Paavolainen P, Paavilainen T. Loosening of threaded acetabular components. Radiographic manifestations. J Arthroplasty 1993; 8: 581–4
- Thabe H, Wolfram U, Schill S. Medium-term results using the cement-free link endoprosthesis Ribbed shaft V socket. Z Orthop Ihre Grenzgeb 1993; 131: 568–73
- Tooke S M, Nugent P J, Chotivichit A, Goodman W, Kabo J M. Comparison of in vivo cementless acetabular fixation. Clin Orthop 1988, 235: 253–60
- Volkmann R, Schneider M A, Bretschneider C, Weise K. More failures of uncemented acetabular screw-rings than of cemented polyethylene cups in total hip arthroplasties. Int Orthop 1999; 23: 138–9
- Wolf T, Reichelt A, Schlepckow P. Clinical results using the PM type of hip endoprosthesis. Z Orthop Ihre Grenzgeb 1988; 126: 637–42
- Yahiro M A, Gantenberg J B, Nelson R, Lu H T, Mishra N K. Comparison of the results of cemented, porous-ingrowth, and threaded acetabular cup fixation. A meta-analysis of the orthopaedic literature. J Arthroplasty 1995; 10: 339–50