Abstract
Background We have previously reported that 6 months of oral treatment with clodronate reduced the migration of the NexGen total knee prosthesis during the first postoperative year, as measured by radiostereometry (RSA). We now report the 4-year results.
Methods This was a double-blind randomized study, using RSA with maximal total point motion (MTPM).
Results With analysis according to the “intention to treat” principle, the only remaining difference between the groups at 4 years was reduced rotation around the transverse axis (a secondary variable) in the clodronate group. However, 3 patients (all clodronate) did not take any tablet after surgery. If they are excluded, there was an almost statistically significant difference between the groups at 4 years regarding MTPM from baseline, with the clodronate group showing 25% less migration. From 1 to 4 years, there was no difference in migration rate by MTPM, but there was a continuous increase in rotation around the transverse axis in the controls, which differed from the clodronate group. There were no cases of aseptic loosening. 2 patients had migration of more than 1.3 mm from baseline to 4 years; neither of them had taken clodronate. The others had migration of less than 0.9 mm.
Interpretation Because migration was clearly reduced by clodronate during the first postoperative year, and there was still a difference at 4 years when analyzed per protocol, it appears likely that this treatment can diminish the risk of loosening. The difference in the number of outliers also points in this direction, and may be more relevant than mean migration values.
Late loosening of a total joint prosthesis appears to be closely dependent on initial fixation and early postoperative processes. Postoperative radiolucent zones (Ritter et al. Citation1999)—or even as little as 0.25 mm migration during the second postoperative year (Ryd et al. Citation1995)—increase the risk of late loosening several-fold. One explanation for this link between early stability and lasting success may be that direct contact is established between the implant and the bone. This would prevent generation of fluid pressure and invasion by wear debris particles, both of which have been suggested to cause bone resorption (Aspenberg and Van der Vis Citation1998). When direct contact is not established, a fibrous membrane will be formed. This tissue replaces the bone on which the implant (the cement) was resting directly after insertion. Thus, initial bone resorption is a prerequisite for the formation of a membrane, if surgery has been successfully performed. Thus, inhibition of bone resorption by a bisphosphonate during the postoperative period should facilitate the maintenance of direct bone-implant contact until a mechanically and biologically stable situation has been reached. We have previously tested this hypothesis in a randomized blinded study, using radiostereometry (RSA) as outcome variable (Hilding et al. Citation2000).
The 1-year results of that study were published on condition that longer follow-up would follow. This now follows. Briefly, 50 patients receiving NexGen total knee prostheses because of osteoarthrosis were randomized to receive either placebo or 1.6 g clodronate once daily until 6 months postoperatively. Radiostereometeric analyses after 1 year showed that migration was significantly less in the clodronate group. However, even the controls migrated little. With this small margin for improvement, the mean MTPM could only be diminished from 0.4 mm in the controls, to 0.3 mm. Migration could not be abolished totally. The conclusions were that early migration is at least in part dependent on osteoclastic activity and that it could be reduced by a bisphosphonate.
When we got the results of the previous report, i.e. 1 year postoperatively, two different further developments could be envisaged. Either the initial clodronate treatment might prove to be successful in creating a lasting mechanical contact between bone and the implant, or the effect might wear off, and both groups would then show similar results.
Patients and methods
Patients, inclusion criteria, and radiostereometric methods were described in detail in the previous paper (patients filled in informed consent forms and the study was duly approved by a regional ethical board and the Swedish Drug Agency). Briefly, the inclusion criteria were gonarthrosis stadies 3–5 according to Ahlbäck (Citation1968), and age 60–75 years. Patients with previous bisphosphonate medication, rheumatoid arthritis, or any other systemic illness affecting the skeleton were excluded. The patients were randomized to either clodronate (1.6 g/day) or placebo starting 3 weeks before the operation and continuing for 6 months after the operation. Thus, any deviations in postoperative course or implant position did not influence inclusion.
RSA examinations were done on the first postoperative day, at 6 weeks, 6 months, and 1, 2 and 4 years. The analyses of the radiostereometric radiographs at 4 years were done in Linköping, using the same RSA system. The raw RSA data from the examinations previously analyzed in Lund were reevaluated by the technician in Linköping.
The analysis is based on maximum total point motion (MTPM), i.e. on the tantalum bead inside the prosthesis that has migrated most relative to the bone. Because this is expressed as a scalar representing the length of a vector, it always has a positive value. Even if the implant is absolutely stable, the measuring error will produce a difference between two time points with a positive value, which would then not represent migration. To overcome this, we related all later measurements to the postoperative position. This is the normal procedure in RSA studies, because the errors when comparing two later examinations then tend to even out. The magnitude of the migration will be underestimated, however, because the implant might move from one position to another, both being at similar distances from the postoperative position. We therefore also studied the MTPM from 1–4 years, using the 1-year examination as baseline.
Statistics
The primary endpoint was MTPM from postoperative examination to 4 years.
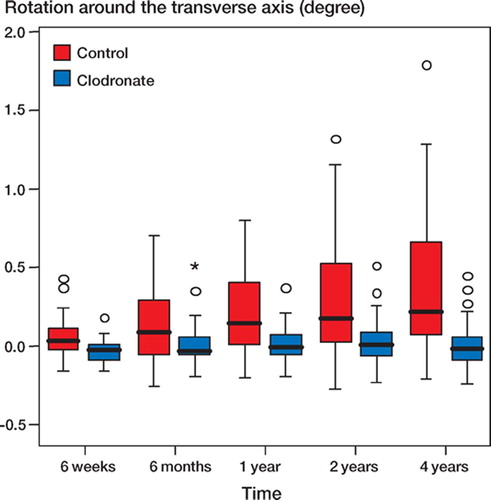
We then analyzed rotation around the transverse axis (forward or backward tilt). Because there was a significant effect of clodronate on this variable in the previous report, its further development was of special interest.
The statistical analysis was done with SPSS. We compared migration at a single time point with t-tests, without assumption of equal variances (Welsh's test). When all time points were analyzed, we used two-way ANOVA for repeated measures using the Greenhouse-Geissler test.
Secondary variables (translation and rotation around the transverse, vertical, and sagittal axes) were tested by t-test (Welsh's test), without multiplicity correction for mass significance. Because rotation may not be more likely to occur in one direction than the other (i.e. one group may have patients with both larger positive and negative rotations, but similar mean value), it may be more relevant to test whether the variation differs between the groups rather than the mean values. We therefore also compared the groups with F-test.
Results
Of the 50 patients included from the start, 1 died before the 1-year follow-up due to unrelated disease. 1 patient missed the 4-year follow-up due to dementia, and one 4-year RSA was technically insufficient. Thus, 3 patients were lost, leaving 47 patients (23 in the clodronate group) at 4 years. 1 clodronate patient had a deep infection, which was cured with antibiotics only. He was not excluded. No patient needed revision.
No difference in MTPM between the groups could be seen at 4 years (t-test, p = 0.1). Repeatedmeasures ANOVA showed an effect of time (p = 0.02) and a trend toward an effect of clodronate treatment (p = 0.06). At the previously reported 1year follow-up, translation or rotation relative to the sagittal, transverse or longitudinal axes were not significantly different between the groups, except for rotation around the transverse axis (backward tilting), which was reduced by clodronate (Hilding et al. Citation2000). At 4 years, rotation around the transverse axis still differed between the groups (p = 0.04).
3 patients (all clodronate) stopped taking the medication due to side effects after a few doses, i.e. well before the operation. One of them also had severe postoperative complications, including deep infection. Because they did not take any tablet at all after surgery, we excluded these 3 patients and performed a new analysis. The results are presented below.
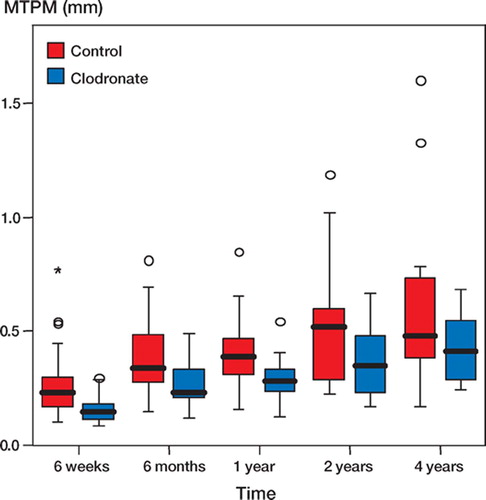
The average migration at 4 years from the postoperative examination was 0.43 (SD 0.14) mm in the clodronate group and 0.58 (SD 0.33) mm in the control group (p = 0.06). The variance in the clodronate group was smaller (p = 0.03). Repeated measures ANOVA showed an effect of time (p = 0.03) and an effect of clodronate treatment (p = 0.02; ). MTPM at 4 years, using the 1-year examination as baseline, showed no group difference (p = 0.3).
Figure 1. MTPM (in mm) for all time points using the postoperative examination as baseline. Controls in red, clodronate in blue. Boxes show interquartile range, whiskers the 90th percentile, and rings show extreme values. The horizontal line inside the box shows the median value. Numerical data are available from the corresponding author on request.
Rotation around the transverse axis (backward tilting) was 0.37° (SD 0.48) in the controls and 0.02° (SD 0.18) in the clodronate group (group difference: p = 0.002; , ). This variable continued to be influenced by the clodronate, even though it was only given for 6 months. Between 1 and 4 years, the tilt had increased by 0.15° (SD 0.25) in the controls (p = 0.02), but only by 0.01° (SD 0.10) in the clodronate group. This change over time differed significantly between the groups (p = 0.01). Sinking of the prosthesis (vertical translation) was also significantly reduced by clodronate (p = 0.03).
Figure 2. Rotation around the transverse axis (in degrees) for all time points using the postoperative examination as baseline. Controls in red, clodronate in blue. Boxes show interquartile range, whiskers the 90th percentile, and rings show extreme values. The horizontal line inside the box shows the median value. Numerical data are available from the corresponding author on request.
Migration from postoperative examination to 4 years. 3 patients who did not take any tablet after the operation have been excluded. X-, y- and z-axes are transverse, vertical and sagittal, respectively
F-test showed less variation in rotation around the transverse axis at 4 years in the clodronate group (p = 0.002).
2 individuals had MTPM values higher than 1.3 mm from baseline to 4 years, both of whom were controls. The others had MTM values below 0.9 mm.
Discussion
At 4 years, there was still a difference between the groups regarding rotation around the transverse axis. This difference also increased between 1 and 4 years. However, our primary outcome variable (MTPM) did not show a significant difference at 4 years (p = 0.06). The migration in both groups was small, but similar to that recently reported in cemented knee prostheses (Carlsson et al. Citation2005). Although desirable, this low degree of migration diminishes the margin for improvement. The effect of clodronate at 1 year shows that osteoclast activity and early fixation are related, but we did not reach our goal of providing total absence of migration from the early postoperative period onward.
An analysis according to protocol is more relevant to this study than the intention to treat principle. It is focused on the effects of delivered treatment at longer follow-up. Today, there are more convenient ways of administering bisphosphonates than in 4 large tablets taken daily (weekly doses, injections or local intraoperative treatment). This would probably increase patient compliance. Thus, we find it justified to exclude the 3 patients who stopped taking their tablets before surgery.
Bisphosphonates preferably bind to remodeling sites, so any binding during the preoperative weeks must have been minimal in comparison to that in the postoperative months, when local remodeling is intense. In similar ongoing studies, we no longer give the bisphosphonate preoperatively.
All our patients were operated by the same surgeon (MH) who had specialized in total knee replacement many years before the study started. It is possible that with less specialized surgeons, the migration would have been greater—which would create more room for a protective effect of bisphosphonate treatment. Hydroxyapatite-coated prostheses that are designed to become osseointegrated have tended to migrate less than cemented prostheses, provided their initially high migration rate has come to a halt (Carlsson et al. Citation2005). With a small degree of migration, differences in mean values between groups may carry less meaningful information than the few outliers that migrate to an ominous degree. There were only 2 such cases in our study, neither of whom had taken clodronate. Indeed, we believe that the distribution pattern for migration (number of outliers) may be more relevant than mean values, but this requires larger studies that are difficult to perform.
Interestingly, the infected patient who took his clodronate did not show any excessive migration. Perhaps bisphosphonates can prevent infec-tion-triggered resorption, thereby contributing to this patient's successful outcome after antibiotic therapy. Several orthopedic conditions might well benefit from bisphosphonate treatment: there is now good evidence that alendronate, at an ordinary osteoporosis dosage, can prevent collapse by blocking resorption after osteonecrosis of the femoral head (Lai et al. Citation2005). Contrary to what we wrote in our previous article (Hilding et al. Citation2000), we now believe that the results with clodronate are likely to be valid for any bisphosphonate. Despite the findings cited regarding osteonecrosis, we would, however, still advocate a high dose.
At 1 year, the patients on clodronate showed migration of 0.3 mm. If all migration is dependent on bone resorption, and if the bisphosphonate treatment had been entirely successful, we should have seen no migration at all at one year and then lasting stability over time. That would indicate osseointegration. It might still be possible to reach that goal with more efficacious bisphosphonate treatment. We know from animal experiments that bone resorption at unstable interfaces requires much higher doses of bisphosphonates than are needed to inhibit a generally increased bone metabolism as in osteoporosis (Åstrand and Aspenberg Citation2002). Thus, in order to provide even better prognosis for total joint replacements, it is possible that they should be combined with either prolonged bisphosphonate treatment at the current dose—or very high local doses of biphosphonate, provided by topical treatment during surgery. We have preliminary unpublished data suggesting that this is efficacious.
We thank Ulf Kallander for RSA analyses. This study was supported by the strategic research project Materials in Medicine, Linköping, Sweden and by the Swedish Research Council.
No competing interests declared.
- Ahlbäck S. Osteoarthritis of the knee. A radiographic investigation. Acta Radiol Scand 1968, Suppl 277: 1–71
- Aspenberg P, Van der Vis H. Migration, particles, and fluid pressure. A discussion of causes of prosthetic loosening. Clin Orthop Relat Res 1998, 352: 75–80
- Åstrand J, Aspenberg P. Reduction of instability-induced bone resorption using bisphosphonates: high doses are needed in rats. Acta Orthop Scand 2002; 73(1)24–30
- Carlsson A, Björkman A, Besjakov J, Önsten I. Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop 2005; 76(3)362–9
- Hilding M, Ryd L, Toksvig-Larsen S, Aspenberg P. Clodronate prevents prosthetic migration: a randomized radiostereometric study of 50 total knee patients. Acta Orthop Scand 2000; 71(6)553–7
- Lai K A, Shen W J, Yang C Y, Shao C J, Hsu J T, Lin R M. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg (Am) 2005; 87(10)2155–9
- Ritter M A, Zhou H, Keating C M, Keating E M, Faris P M, Meding J B, Berend M E. Radiological factors influencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg (Br) 1999; 81(6)982–6
- Ryd L, Albrektsson B E, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77(3)377–83