Abstract
Background Secure healing of soft tissue to bone is a prerequisite for many orthopedic operations. This healing can be achieved either by pressing the tissue against the bone (press fixation) or by suturing the soft tissue to the bone (point fixation).
Experiments and findings We tested the hypothesis that point fixation of soft tissue to bone results in better mechanical properties than press fixation. 10 skeletally mature New Zealand White rabbits were operated on bilaterally at the knees. The medial collateral ligaments were fixated to the bone just above the original insertion on the tibia. Two types of plates were used for this purpose, one with flat undersurface (left knee) and the other one with a pegged undersurface (right knee). The pegged plate was thought to mimic fixation achieved with suture anchors. After 4 weeks, mechanical testing revealed an almost doubled force at failure, stiffness and energy uptake in the knees operated with the pegged plates.
Interpretation Suture anchors or devices with a pegged undersurface are better for soft tissue fixation to bone than devices with a flat surface, such as screws with washers or staples.
The outcome of instability surgery of the shoulder or the knee depends on secure fixation and healing of soft tissue to bone. Traditionally, this can be achieved in two ways: either by pressing the soft tissue against the bone with a staple, screw or tag, or by bone-sutures. Since Goble et al. (1984) introduced suture anchors, it has been much easier to suture soft tissue to bone. Still, little is known about the biomechanical consequences of different fixation techniques.
We got the idea for this study when we reoperated patients who had undergone an open Bankart repair with a screw and washer. In some of these patients, a buttonhole deformity had developed in the anterior capsule-labral complex, leading to recurrent anterior instability. Furthermore, a retrospective study found better anterior stability in a group of patients operated with suture anchor fixation than in a group with the screw technique (Nowak et al. Citation1998). Our study was designed to test the hypothesis that point fixation, as with suture anchors, results in better healing than when the soft tissue is compressed against the bone with a flat surface, e.g. with a screw or staple.
Using a rabbit model, we compared fixation of the medial collateral ligament with two different plates: one with a smooth flat undersurface, and the other one with a pegged undersurface.
Experiment
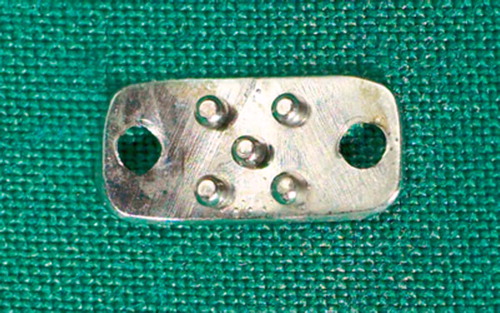
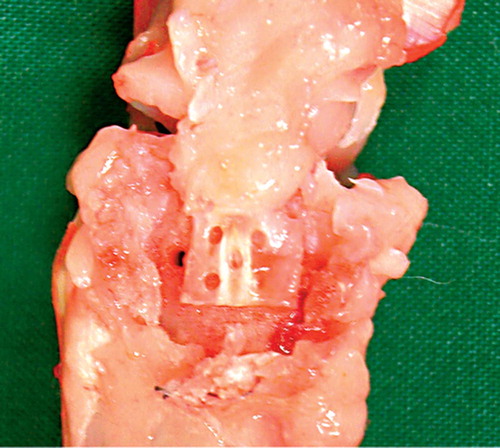
10 skeletally mature New Zealand White rabbits (5 male) weighing 4.4 (4.0–4.8) kg were used. The study was approved by the regional ethics committee. Special plates were designed and made by an instrument maker. The plates were made of stainless steel and shaped to conform to the proximal part of the rabbit tibia, where the medial collateral ligament inserts. The plates were identical in shape, except that half of the plates had 5 pegs of 1 mm height and diameter on the undersurface, resembling point fixation (). The other half had a smooth flat undersurface, resembling fixation with a compression device (). The plates were fixed to the tibia with two 1.5-mm AO cortical screws.
Surgical procedure and treatment
The rabbits were sedated with fentanyl fluanisone (Hypnorm Janssen Pharmaceutica, Beerse, Belgium; 0.1–0.2 mg/kg body weight) subcutaneously. Under general anesthesia using isoflurane gas (Forene; Abbot Scandinavia, Solna, Sweden) and oxygen, the rabbits were operated on both the right and left knee. Surgery was performed under standard aseptic conditions. The skin was shaved, and prophylactic antibiotics (dicloxacillin) and analgesics in the form of 0.015 mg buprenorphine (Temgesic; Schering-Plough, Brussels, Belgium) subcutaneously were given preoperatively.
A 3-cm skin incision was made midway between the medial collateral ligament (MCL) and the patellar tendon insertion. The MCL was exposed, the synovial bursa under the ligament removed and the cortical bone roughened with a rasp proximal to the distal insertion of the ligament. A 3-0 nonabsorbable suture was passed under the ligament and pulled distally as far as possible to mark the insertion on the tibia without compromising it. The ligament portion proximal to the suture and beneath the joint line was then fixed by the plate. The plate was fixed to the bone with two 1.5-mm AO screws, one on each side of the ligament.
The plate with pegs was used on the right side, and on the left side the plate with a flat undersurface was used. The skin was closed with a 4-0 etylon suture intracutanously. Minimal bleeding was observed during the operations.
After the operation, the rabbits were housed 1 per cage (0.5 m2) and activity was allowed only in the cages. They received analgesia with Temgesic, 0.03 mg/kg twice daily for 3 days postoperatively. The condition of each rabbit was documented in an individual rabbit journal on a daily basis.
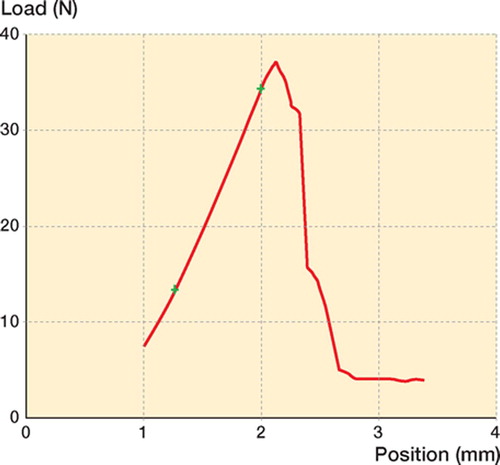
Mechanical results of flat or pegged plates in all rabbits
Evaluation
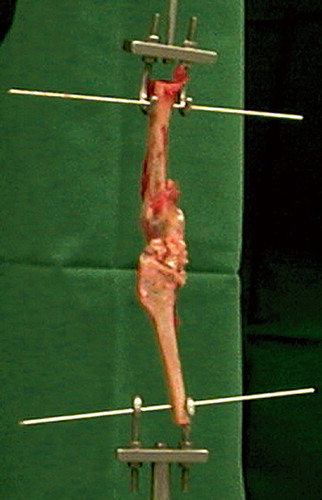
The rabbits were killed 28 days after the operation using an overdose of pentabarbitural injected intravenously. Each knee joint was removed by transecting the femur just below the trochanteric region and the tibia above the ankle. The MCL attached to the femur and the tibia was isolated, and the remaining soft tissue was removed. Before removing the plate, a transverse cut was made through the MCL along the distal border of the plate, proximal to the original insertion point of the MCL (marked with the nonabsorbable suture). This enabled us to test the mechanical properties of the ligament fixation in the area under the plate. The knee was fixed to a materials testing machine (100R; DDL Inc., Eden Praire, MN) using 1.6-mm Kirschner wires inserted into drill-holes made in the femur and tibia. Testing was performed within a few hours of death. In the meantime, the knee was kept cool and wet. A constant distension in the direction of the MCL with a speed of 1 mm/sec was applied until failure. We recorded the peak force at failure, stiffness and energy uptake until the force dropped to 90% of maximum.
Statistics
We used Wilcoxon's signed-rank sum test to compare the flat and pegged sides. Confidence intervals for the median difference between the sides are based on the observations with rank 2 and 9, which yields approximately 90% confidence (Altman Citation1999).
Results
No animals were excluded. All the wounds healed uneventfully and the rabbits loaded their hind limbs immediately postoperatively. Gross inspection of the knee joints at the harvest showed that the plates were covered by fibrous material similar to tendon callus.
Mechanical results (Table)
Rabbit no. 7 was an outlier, probably due to malplacement of one screw through the ligament on the pegged plate side. In the other 9 animals, the force at failure, stiffness and energy uptake were always higher on the side with the pegged plate. Analyzing all 10 animals, the force was 133% higher on the pegged side (range –24 to 342; 90% CI for median 51–322%). Stiffness and energy were increased by 75% and 210%, respectively. (Stiffness: range –22% to 426%; 90% CI for median 8–260%. Energy uptake: range 79% to 659%; 90% CI for median 90–515%).
Discussion
In the classical Bankart repair (Bankart Citation1923), the capsulolabral complex has to heal to the anterior glenoidal rim, and in cuff repair the tendons have to heal to the tuberosities.
Tendon-to-bone healing in a dog model with a bone tunnel shows a progressive increase in the number and organization of collagen fibers between the bone and the tendon (Rodeo et al. Citation1993). The fibers were morphologically identical to the classic description of Sharpey fibers (Sharpey and Ellis Citation1856). In the same model, there was a progressive increase in the strength of the interface during the first 12 weeks after the operation, and this appeared to correlate with the degree of bone ingrowth and maturation of the tissue (Rodeo et al. Citation1993). The values for pullout strength were proportional to the degree of osseous ingrowth into the interfacial gap (Arnoczky et al. Citation1988). In another dog model, an ACL reconstruction was performed using a 4-mm diameter flexor tendon in tunnels with a diameter of 4 or 6 mm in the tibia (Yamazaki et al. Citation2002). The results of both histological and mechanical properties were superior in the group with a 6-mm diameter tunnel at 3 and 6 weeks. In contrast, Rodeo et al. (Citation1993) found that the pullout strength of the tendon from a bone tunnel progressively increased with the obliteration of the space between the tendon and the bone.
In a rabbit model using semitendinosus autograft for reconstruction of the anterior cruciate ligament, the interface between the grafted tendon and the bone tunnel was filled with calcium phosphate cement (CPC) (Tien Citation2004). Histological examination showed that the CPC produced early, diffuse and massive bone ingrowth, leading to increased pullout strength. In another study (Yamazaki et al. Citation2005), the ACL was reconstructed in a dog model with a flexor tendon treated with 2 ng of TGF-β1 mixed with 0.1 mL of fibrin sealant. The pullout strength was increased, and the histology showed that there was rich generation of perpendicular fibers connecting the tendon to bone.
Other studies have focused on the ability to restore the native footprint of the tendon. In a study on shoulders of cadavers, tendon motion relative to the insertional footprint on the greater tuberosity was determined (Ahmad et al. Citation2005). Testing was performed for the intact tendon, a complete supraspinatus tear, a suture anchor repair and a transosseous tunnel repair. The transosseous repair showed less motion between the tendon and the bone at the footprint than the suture anchor repair condition. In a bovine shoulder model, the interface contact pressure between the tendon and bone was evaluated for different rotator cuff repair techniques. A transosseous tunnel technique created more contact and a greater overall pressure distribution over a defined footprint, than did repair with suture anchors with simple or mattress technique (Park et al. Citation2005).
Excessive motion at the tendon-bone interface may disrupt the forming fibrovascular tissue and compromise the healing process. The endobutton linked with tape allows motion of the graft up to 3 mm under cyclic physiological loads (Hoher et al. Citation1999). This longitudinal motion has been associated with tunnel expansion in clinical trials (L'Inslata et al. Citation1997, Nebelung et al. Citation1998).
A controversy exists regarding the optimal fixation technique in rotator cuff surgery. Some studies have reported that suture anchors are weaker than transosseous tunnels (Rossouw et al. Citation1997), while others have reported higher fixation strength with suture anchors (Reed et al. Citation1996). There has been recent interest in improving footprint anatomy by using a double-row suture anchor technique in rotator cuff repair (Fealy et al. Citation2002, Lo and Burkhart Citation2003), a medial mattress and lateral simple suture, and this may improve tendon-to-bone pressure distribution.
Our study addresses tendon healing to a bone surface. This kind of healing is essential in surgery for instability of the shoulder and cuff repair. It can also be expected to be more difficult to achieve, because the bone surface appears less vascularized, and if the periosteum is scraped off, there are probably fewer progenitor cells. However, in a goat model, no difference has been found in the healing process or in the mechanical properties between tendon healing to cortical and cancellous bone (St Pierre and Olsson Citation1995). On the other hand, based on a histological study in 14 rabbit shoulders, it has been advocated that the tendon should be attached to a bleeding surface of cancellous bone (Uthoff Citation2000). In our study the bone surface was roughened, but no attempt was made to create a bleeding surface.
A weak point of our study is that we used a pegged plate instead of suture anchors, because this made it easy to produce a reasonably standardized model for point fixation. Using the pegged plate roughly doubled the mechanical variables. One possible explanation may be that the flat plate compromises the blood supply, leading to tissue necrosis that would impair the healing process. Our results favor the use of suture anchors or other devices that result in point fixation.
We thank Dr Olena Virchenko and Ali Sudeifi for help with operations and technical assistance. This work was funded by “Materials in Medicine” in Linkoping, and by the Swedish Research Council 2031 and Centrum for Idrottsmedicin in Sweden.
No competing interests declared.
Contributions of authors
SK: designed, performed and wrote the article. AF: helped in performance of the study. PA: designed, did the statistic analyses and reviewed the article. HR: designed, helped in writing and reviewed the article.
- Ahmad C S, Stewart A M, Izquierdo R, Bigliani L U. Tendon-bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques. Am J Sports Med 2005; 33: 1667–71
- Altman D G. Practical statistics for medical research. Table B11: Ranks for obtaining a confidence interval for the median. Textbook, Chapman & Hall/CRC, London 1999; 535
- Arnoczky S P, Torzilli P A, Warren R F, Allen A A. Biologic fixation of ligament protheses and augmentation: an evaluation of bone ingrowth in the dog. Am J Sports Med 1988; 16: 106–12
- Bankart A S B. Recurrent or habitual dislocation of the shoulder joint. Br Med J. 1923; 2: 1132–3
- Fealy S, Kingham T P, Altchek D W. Mini-open rotator cuff repair using a two-row fixation technique: outcomes analysis in patients with small, moderate, and large rotator cuff tears. Arthroscopy 2002; 18(6)665–70
- Goble E M, Somers W K, Clark R, Olsen R E. The development of suture anchors for use in soft tissue fixation to bone. Am J Sports Med 1994; 22: 236–9
- Hoher J, Livesay G A, Ma C B, Withrow J D, Fu F H, Woo S L. Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc 1999; 7(4)215–9
- L'Insalata J C, Klatt B, Fu F H, Harner C D. Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc 1997; 5(4)234–8
- Lo I K, Burkhart S S. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy 2003; 19(9)1035–42
- Nebelung W, Becker R, Merkel M, Ropke M. Bone tunnel enlargement after anterior cruciate ligament reconstruction with semitendinosus tendon using Endobutton fixation on the femoral side. Arthroscopy 1998; 14(8)810
- Nowak J, Wintzell G, Moberg A, Wikblad L, Larsson S. A comparative study of fixation techniques in the open Bankart operation using either a cannulated screw or a suture-anchors. Acta Orthop Belg 1998; 64: 150–9
- Park M C, Cadet E R, Levine W N, Bigliani L U, Ahmad C S. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med 2005; 33: 1154–9
- Reed S C, Glossop N, Ogilvie-Harris D J. Full-thickness rotator cuff tears. A biomechanical comparison of suture versus bone anchor techniques. Am J Sports Med 1996; 24(1)46–8
- Rodeo S A, Arnoczky S P, Torzilli P A, Hidaka C, Warren R F. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg (Am) 1993; 75(12)1795–803
- Rossouw D J, McElroy B J, Amis A A, Emery R J. A biomechanical evaluation of suture anchors in repair of the rotator cuff. J Bone Joint Surg (Br) 1997; 79(3)458–61
- Sharpey W, Ellis G V. Elements of anatomy by Jones Quain. Walton and Moberly, London 1856, Ed. 6, vol. 1
- St Pierre P, Olson E J. Tendon-healing to cortical bone compared with healing to a cancellous trough. A biomechanical and histological evaluation in goats. J Bone Joint Surg (Am) 1995; 77: 1858–66
- Tien Y C. Augmentation of tendon-bone healing by the use of calcium-phosphate cement. J Bone Joint Surg (Br) 2004; 86: 1072–6
- Uhthoff H K. Early reactions after reimplantation of the tendon of supraspinatus into bone. A study in rabbits. J Bone Joint Surg (Br) 2000; 82: 1072–6
- Yamazaki S, Yasuda K, Tomita T, Minami A, Tohyama H. The effect of graft-tunnel diameter disparity on intraosseous healing of the flexor tendon graft in anterior cruciate ligament reconstruction. Am J Sports Med 2002; 30: 498–505
- Yamazaki S, Yasuda K, Tomita F, Tohyama H, Minami A. The effect of transforming growth factor-beta1 on intraosseous healing of flexor tendonautograft replacement of anterior cruciate ligament in dogs. Arthroscopy 2005; 21(9)1034–41