Abstract
Background Reconstruction of the bone stock and fixation of the implant remain challenging problems in revision surgery. In this retrospective study, we wanted to gain information on initial stability and wear after revision with the Burch-Schneider ring.
Patients and methods Between 1994 and 1998, we performed 70 reconstructions of the acetabulum with a Burch-Schneider ring in revision arthroplasty. 63 patients could be followed up clinically and radiographically. 40 cups were suitable for EBRA measurements whereas migration and wear could not be assessed by this method in 23 cases due to lack of comparability of pelvic radiographs. The mean follow-up time was 4.7 years.
Results 2 cups were re-revised and 14 cups had breakage or changes of position of the screws. 30 cups showed detectable migration and 18 cups detectable wear. The mean migration was 2.8 mm and the mean wear rate was 0.12 mm/year. 16 cups had detectable migration after 1 year; 11 of these 16 continued to migrate and 9 of them had screw breakage. Both re-revisions showed early migration. Early migration correlated with later screw breakage and the overall migration correlated with wear. The only risk factor found for early migration was the wear rate.
Interpretation The Burch-Schneider ring is an established and reliable implant for cup revision with good clinical results, but it seems to be difficult to maintain intraoperative stability. The implants with continuous migration may lead to late clinical failure and require further observation. Wear may contribute to migration and resorption of the bone graft. ▪
A reinforcement ring can be used to protect the bone graft and to fix the cup when a loose acetabular component is revised. The defect is filled with bank bone or autologous bone from the iliac crest. The mid-term results are promising (Berry and Muller Citation1992, Cabanela Citation1998, Bohm and Banzhaf Citation1999, Schatzker and Wong Citation1999, Perka and Ludwig Citation2001, Winter et al. Citation2001).
Very little data on migration and wear after such a reconstruction are available. There is controversy regarding the initial stability. Some authors report no migration as assessed by conventional methods (Winter et al. Citation2001) but RSA studies have found significant migration for almost all cups revised with the Burch-Schneider ring (Snorrason and Kärrholm Citation1990) and with impacted bone grafting (Ornstein et al. Citation1999).
In this retrospective study, we wanted to obtain more information on the in vivo behavior of acetabular reconstruction with the Burch-Schneider ring, concentrating especially on assessment of migration and wear of the implant. Measurements were made with the EBRA method, which has been shown previously to be more accurate than standard methods (Ilchmann Citation1997, Stockl et al. Citation1997).
Patients and methods
In the years 1994 and 1995, 70 acetabular reconstructions with a Burch-Schneider ring were performed at our hospital due to aseptic loosening of the cup. 1 patient died postoperatively due to an anesthetic complication and 1 died of causes not related to the operation. 3 patients could not be traced and were lost to follow-up and 2 patients declined further examination and were excluded. The remaining 63 patients had regular clinical and radiographic follow-up examinations. All patients had at least 4 radiographs of the pelvis. In 23 hips, migration and wear could not be assessed with the EBRA software due to a lack of comparability of the pelvis radiographs, as this would have compromised measurement accuracy (Krismer et al. Citation1995). 40 cups (patients) remained for complete measurements of migration and wear. The mean follow-up was 4.7 (2.3−6.9) years and on average 7.8 (4−19) radiographs per patient wereanalyzed.
The primary diagnosis for hip replacement was osteoarthrosis in 35 cases, trauma in 3 and others in 2. The mean age at revision was 70 (36–81) years. 11 of the 40 patients were male and 11 hips were left-sided. All hips were revised due to aseptic loosening at a mean of 12 (2–21) years after the last operation. 33 of the primary implants were cemented. The others were various kinds of cementless implants and 6 cups were revised for the second time.
In 26/40 hips only the cup was revised, 14 of which had a temporary extraction of the stem during the operation to facilitate the approach to the cup. 14 hips had a revision of both components.
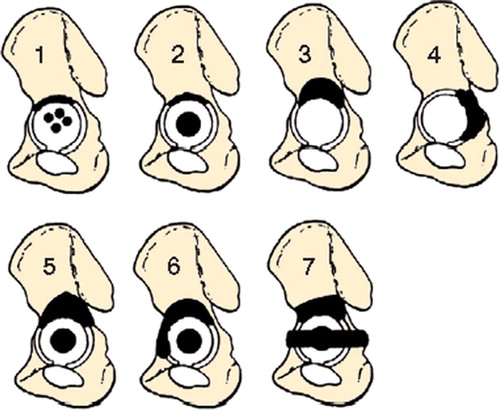
Rings were only used in cases of severe bone loss as judged by the operating surgeon. Type and extent of the acetabular deficiency were determined from the preoperative radiographs and the intraoperative findings. They were classified according to Bettin and Katthagen (Citation1997): 24 had unisegmental defects and 16 had bi- or trisegmental defects ().
Figure 1. Defect classification according to Bettin and Katthagen (Citation1997). Type 1 is a cavity. Types 2–4 are unisegmental defects. Type 5 is bisegmental, type 6 is trisegmental, and type 7 is a discontinuity of the pelvis.
The loose implant, residual cement, any granulomas and all membranes were removed and the remaining vital bone was exposed. The defect was filled with hand-made bone chips of about 5–10 mm in size. In 33 hips frozen allogenic bone from the bone bank was used, and for 7 hips autologous bone from the iliac crest was harvested and frozen in a first operation some weeks before the revision. A small-sized ring was implanted into 18 patients and 22 patients were given the large-sized ring. 2–5 screws were used for fixation of the cranial flange and 0–2 screws for the caudal flange.
All patients with cup revision alone were mobilized after 1 week of bed rest with 20 kg of weight bearing for 6 weeks. The patients with additional stem revision had 1–2 weeks of bed rest and 20 kg of weight bearing for 6–12 weeks, depending on the bone stock at the femoral site.
The position of the reconstructed centre of rotation was controlled. In the cases of unilateral hip disease, the contralateral side served for estimation of the optimal position, using the Nunn lines as reference (Nunn et al. Citation1989). In the other cases, the center of rotation was estimated using the method of Ranawat et al. (Citation1980).
On the follow-up radiographs, any breakage or changes of position of the screws and osteolysis were recorded. Migration was measured as proposed by Nunn et al. (Citation1989). Furthermore, migration and wear were measured with the EBRA method. Before starting the analysis, the measurement accuracy was verified by repeated measurements of single radiographs and series of radiographs. For some hips, the contour of the contrast wire of the cup was difficult to detect as it was partially covered by the ring. Using special software for contrast enhancement, the contour of all components could be defined in a satisfactory way. As in previous EBRA investigations, migration of more than 1 mm and wear of more than 0.5 mm were regarded as significant (Ilchmann Citation1997).
Statistics
We used the Mann-Whitney U-test, Fisher’s exact test and Pearson’s coefficient of correlation. The Kolmogorov-Smirnov test was applied to test the assumption of normally distributed data. A normally distributed variable was compared between two groups with student’s t-test for independent groups. The homogeneity of variances was analyzed with the Levene test. Correlations for not normally distributed data were calculated with Spearman’s rank coefficient, rho. The significance level, alpha, was set to 5% for each test.
Results
At the latest follow-up, the mean Harris hip score was 72 (33–100) points. All patients were able to walk and none were interested in further surgery. On the postoperative radiographs, the center of rotation was placed mean 8.3 (−16–40) mm cranially and 8.7 (−13–38) mm laterally relative to the ideal position. There was no correlation between the preoperative bone defect (unisegmental vs. defect with larger extent) and the postoperative position of the center of rotation (Mann-Whitney U-test, p = 0.7).
Obvious osteolysis could not be seen in any case. Broken screws were found in 12 hips, and 2 hips had a screw dislocation without breakage (). 2 cups were re-revised due to aseptic loosening of the Burch-Schneider ring after 3 and 5 years; all screws were broken or severely dislocated (). Screw breakage was observed after a mean time of 3 (0.7–6) years. The incidence of screw breakage did not depend on the number of screws (p = 0.8, Mann-Whitney U-test), the size of the preoperative bone defect (unisegmental vs. bi- or trisegmental, p = 1, Fisher’s exact test) and postoperative lateral position (p = 0.7, Fisher’s exact test) or cranial position (p = 0.7, Fisher’s exact test). Of the 23 patients excluded from EBRA analysis, no cup was re-revised.
Figure 2. A 28-year-old man had a hip replacement because of a posttraumatic osteonecrosis of the femoral head. After 8 years, the cup was revised due to symptomatic aseptic loosening. After 3.5 years, he had no pain and a regular function of his revised hip. There was a change of position of 2 screws without breakage. The migration was 3.2 mm, and the wear 0.7 mm.

Figure 3. A 67-year-old woman received a hip replacement for primary osteoarthrosis. After 6 years, the cup was revised because of recurrent dislocation and symptomatic aseptic loosening. After 3.7 years, she had experienced increasing pain. There was a severe dislocation of the Burch-Schneider ring; two screws were broken. The migration was 18 mm, and the wear 0.81 mm. The cup had to be re-revised.

Migration measurement with the Nunn method showed a migration of more than 3 mm in 7 cups and all but 1 had broken screws. 5 of these cups had a migration exceeding 5 mm; all had broken screws. The two re-revised cups had the highest amount of migration (11 and 19 mm). Mean migration was 3.0 (0.6–19) mm and the main direction of migration was craniomedial.
With EBRA, 30 cups had a migration of more than 1 mm, the mean direction of migration being craniomedial (). Mean migration in the medial direction was 0.1 (−13–4.2) mm, and mean migration in the cranial direction was 1.9 (−1.7–12) mm. The cup with the maximum amount of lateral migration (13 mm) was situated 7 mm laterally from the calculated center of rotation and had developed a lateral dislocation of the caudal flange; this cup was re-revised (). 13 of 14 cups with broken or dislocated screws showed significant migration. 1 cup had a slight movement of one screw but the ring showed no detectable migration. For the 14 cups with screw changes, the mean medial migration was 0.1 (−13–4.2) mm and the mean cranial migration was 4.0 (−0.9–12) mm. 10 cups had a migration exceeding 3 mm, and 9 of them had broken or dislocated screws. 4 cups had a migration of more than 5 mm; all had broken screws, 2 of which were re-revised. There was a correlation between changes in the screws and migration (r2 = 0.27, p < 0.001). For the 14 cases with changes in the screws, the mean total migration was 5.0 mm, whereas the 26 cases without changes in the screws had a significantly lower mean migration of 1.5 mm (p = 0.001, Mann-Whit-ney U-test).
Figure 4. With EBRA, 30 cups had a significant migration of more than 1 mm (inner circle) and 10 cups migrated more than 3 mm. The main direction of migration was craniomedial (mean 71°, SD 67.9°). The 2 cups with the maximal migration have since been re-revised, the main direction of migration being craniolateral.
The incidence of migration did not depend on the preoperative bony defect (p = 0.71, Fisher’s exact test) or a postoperative cranial (p = 0.5) or lateral (p = 0.3) cup position. There was no difference in the incidence of migration between autologous or homologous bone-grafts (p = 1, Fisher’s exact test). The 26 patients with an isolated revision of the cup showed slightly more migration (mean 3.2 mm, SD 3.9) than the patients with revision of both components (mean 2.0 mm, SD 1.2) (p = 0.6, Mann-Whitney U-test).
16 hips had detectable migration after 1 year (early migration), with 5 of the 16 cups showing no further progression of the initial migration. These 5 cups had no screw changes and a lower wearrate than the 11 cups with continuous migration. Early and continuous migration increased the risk of screw changes (p < 0.001, Fisher’s exact test) which were seen in 9 of the 11 cups, 2 of which were re-revised. There were statistically significant positive correlations between early migration and the migration-rate (r2 = 0.29, p < 0.001), the total migration (r2 = 0.28, p < 0.001) and the wear-rate (r2 = 0.20, p = 0.004). The cups with early migration showed more migration at two (r2 = 0.42, p < 0.001) and three (r2 = 0.26, p < 0.001) years of follow-up than the other cups ().
Figure 5. Mean migration and standard deviation for the 16 cups with detectable migration at one year (early migration) and for the 24 cups without early migration. Most of the cups with early migration continued to migrate. Both re-revised cups had early migration. The cups with no early migration remained stable; they showed little increase in total migration with time.
The 18 cups with a medial direction of migration showed less migration (mean 2.8, range 0.6–8.9 mm) than the 8 cups with lateral migration (mean 5.4, 1.5–18 mm), but the difference was not significant (p = 0.2, Mann-Whitney U-test).
In 17 hips, the center of rotation was reconstructed more than 5 mm laterally relative to the ideal position. They even were placed more cranially (p = 0.02, Fisher’s exact test). There was no significant difference in defect size (p = 0.5, Fisher’s exact test), in incidence of screw changes (p = 0.7, Fisher’s exact test), in the amount of migration (p = 0.4, Mann-Whitney U-test) or in wear (p = 0.3, Mann-Whitney U-test) as compared to the other rings.
18 cups had detectable wear, the mean wear being 0.51 (0.1–1.6) mm and the mean wear rate being 0.12 (0.03–0.32) mm/year. The mean direction of wear was craniolateral. There was a significant positive correlation between the total wear and the total migration (p = 0.004, Spearman’s rho = 0.44).
Patients with revision of the cup alone showed significantly more linear wear (mean 0.57 mm, SD 0.32) than patients with revision of both components (mean 0.38 mm, SD 0.17; p = 0.02, t-test for independent groups).
The 22 cups without detectable wear had migrated to a significantly lesser extent (mean 2 mm, SD 1.0) than the 18 cups with detectable wear (mean 4.2 mm, SD 4.4; p = 0.008, Mann-Whitney U-test). There was a positive correlation between the wear rate and the migration rate (p = 0.001, Spearman’s rho = 0.61). Hips without stem revision had a mean wear rate of 0.13 (SD 0.07) mm/year. With stem revision, the mean wear rate was 0.10 (SD 0.06) mm/year (p = 0.1, t-test.).
Discussion
The Burch-Schneider ring is recommended for the reconstruction of multisegmental defects, as it is thought to provide good primary stability because of the cranial and caudal flanges and the additional screws for fixation. It is intended to protect the grafted bone from high mechanical stress or micromovements which might lead to bone resorption and poor remodeling of the defects. Satisfying mid-term results can be expected for this system (Perka and Ludwig Citation2001, Winter et al. Citation2001).
Filling of extended defects with solid allografts and cementing of the new cup is controversial (Snorrason and Kärrholm Citation1990, Gross et al. Citation2002a, Paprosky and Martin Citation2002). Impacted morselized bone grafting seems to achieve a better incorporation of the bone and better mid-term results. The smaller bony chips become sufficiently integrated and replaced by vital bone (Schreurs et al. Citation1994, Buma et al. Citation1996, Slooff et al. Citation1996, van der Donk et al. Citation2002). It does, however,appear to be difficult to achieve a rigid bony bed in the case of severe central defects, and the use of reinforcement rings is recommended especially for extended defects (Schatzker and Wong Citation1999, Winter et al. Citation2001, Gross et al. Citation2002b).
Assessment of migration gives objective data on the initial stability, and it has been demonstrated that early migration is of prognostic value for primary hip replacements (Walker et al. Citation1995, Krismer et al. Citation1996, Freeman Citation1997). For cup revisions, initial stability is inferior to that for primary arthroplasties and a high rate of migration has been reported in the use of cages (Snorrason and Kärr-holm Citation1990, Nivbrant et al. Citation1996, Van Koeveringe and Ochsner Citation2002) and in impacted bone grafting for cemented and uncemented cups (Franzen et al. Citation1993, Nivbrant et al. Citation1996, Ornstein et al. Citation1999). We found a high percentage of cup migration and screw breakage in revisions with the Burch-Schneider ring.
In a previous study from our institution, Winter et al. (Citation2001) found no migration in 38 cups after an average of 7 years. All had been operated in an earlier period (1988–1994) by the same surgeon using the technique mentioned above. The level of significance for assessment of migration was not stated, and the absence of migration may have been due to a lower methodological accuracy—but changes in the screws were not noted either. In the present series of patients, we found significant migration of 7 cups with the Nunn method and changes in screws for one third of the cups. With EBRA, 30 of 40 cups showed significant migration; early migration was found for 16 cups and 11 had continuous migration. This early migration was associated with increased total migration, screw breakage and wear. Even in the cases without significant migration, it is difficult to prove the osseointegration of the ring with the methods used. Initial stability is very important in order to reduce the risk of migration and loosening, but it is difficult to maintain intraoperative stability in case of revision (Mjöberg Citation1997). The use of the ring seems to provide limited additional stability as compared to bone grafting alone (Gill et al. Citation1998, Gross et al. Citation2000), and the patients should have regular radiographic follow-up—even in cases where there is good clinical function.
We could not detect radiolucencies and bone graft resorption, not even in cups with severe migration. Because of the irregular shape of the grafted defects and the radiographic contrast of the implant and cement, radiolucent lines might be difficult to detect. Radiographic healing does not correlate with histological ingrowth (Hooten et al. Citation1996). In the case of cranio-medial migration, the Burch-Schneider ring may come in closer contact with the opening plane of the acetabulum. Further migration of the implant and compression of the grafted bone might be prevented, explaining the lower migration rate for cups migrating in the medial direction. For implants with lateral migration, a gap between the implant and the reconstructed bone might be expected, but could not be observed on the radiographs. Cups with lateral migration had a higher migration rate; both re-revised cups had migrated laterally. It seems less probable that cups with lateral migration become osseointegrated; clinical failure may become evident when the center of rotation has migrated too much in a lateral direction. We could not find risk factors for lateral migration; also, some medially placed cups had migrated laterally. The direction of migration is difficult to assess, and there is a high error of measurement for hips with little migration, which might explain the absence of risk factors. Neutral reconstruction of the centre of rotation is to be recommended, however (Nivbrant et al. Citation1996).
The wear rate did not differ from that seen in primary implants. Wear depends on the activity of the patient and use of the implant (Schmalzried et al. Citation2000). After a revision, it can be expected that the patients will be less mobile than after a primary replacement. Thus, a lower wear rate might be expected (Robinson et al. Citation1999). On the other hand, bone or cement debris from the revision, scratches on the femoral head in the case of isolated cup revision with non-modular femoral implants, and the use of 32-mm heads might increase the wear rate of revision implants. Patients with isolated cup revision may maintain a higher level of activity. Furthermore, the risk of wear may be increased by damage to the head during the revision operation. The head must be carefully protected during the operation and has to be changed in modular systems. We found a positive correlation between the wear rate and the migration of the cups. The polyethylene debris may cause further damage to the remaining or transplanted bone, and efforts should be made to keep the wear rate low. This might be achieved by the use of smaller heads, ceramics or metal-on-metal surfaces.
No competing interests declared.
Author contributions
TI: concept of the study, supervision, discussion, writing. JPG: patient management, measurements, data handling. EW and KW: concept of the study, discussion, writing.
- Berry D J, Muller M E. Revision arthroplasty using an antiprotrusio cage for massive acetabular bone deficiency. J Bone Joint Surg (Br) 1992; 74: 711–5
- Bettin D, Katthagen B D. The German Society of Orthopedics and Traumatology classification of bone defects in total hip endoprostheses revision operations. Z Orthop Ihre Grenzgeb 1997; 135: 281–4
- Bohm P, Banzhaf S. Acetabular revision with allograft bone. 103 revisions with 3 reconstruction alternatives, followed for 0.3–13 years. Acta Orthop Scand 1999; 70: 240–9
- Buma P, Lamerigts N, Schreurs B W, Gardeniers J, Versleyen D, Slooff T J. Impacted graft incorporation after cemented acetabular revision. Histological evaluation in 8 patients Acta Orthop Scand 1996; 67: 536–40
- Cabanela M E. Reconstruction rings and bone graft in total hip revision surgery. Orthop Clin North Am 1998; 29: 255–62
- Franzen H, Mjöberg B, Önnerfalt R. Early migration of acetabular components revised with cement. Clin Orthop 1993, 287: 131–4, A roentgen stereophotogrammetric study
- Freeman M A. Acetabular cup migration: prediction of aseptic loosening. J Bone Joint Surg (Br). 1997; 79: 342–3
- Gill T J, Sledge J B, Muller M E. The Burch-Schneider antiprotrusio cage in revision total hip arthroplasty: indications, principles and long-term results. J Bone Joint Surg (Br) 1998; 80: 946–53
- Gross A E, Wong P, Saleh K J. Grafts and cages: managing massive bone loss. Orthopedics. 2000; 23: 973–4
- Gross A E, Blackley H, Wong P, Saleh K, Woodgate I. The role of allografts in revision arthroplasty of the hip. Instr Course Lect 2002a; 51: 103–13
- Gross A E, Wong P, Saleh K J. Don't throw away the ring: indications and use. J Arthroplasty 2002b; 17: 162–6
- Hooten J P, Jr., Engh C A, Heekin R D, Vinh T N. Structural bulk allografts in acetabular reconstruction. J Bone Joint Surg (Br) 1996; 78: 270–5, Analysis of two grafts retrieved at post-mortem
- Ilchmann T. Radiographic assessment of cup migration and wear after hip replacement. Acta Orthop Scand (Suppl 276) 1997; 1–26
- Krismer M, Bauer R, Tschupik J, Mayrhofer P. EBRA: a method to measure migration of acetabular components. J Biomech 1995; 28: 1225–36
- Krismer M, Stockl B, Fischer M, Bauer R, Mayrhofer P, Ogon M. Early migration predicts late aseptic failure of hip sockets. J Bone Joint Surg (Br) 1996; 78: 422–6
- Mjöberg B. The theory of early loosening of hip prostheses. Orthopedics 1997; 20: 1169–75
- Nivbrant B, Kärrholm J, Onsten I, Carlsson A, Snorrason F. Migration of porous press-fit cups in hip revision arthro-plasty. J Arthroplasty 1996; 11: 390–6, A radiostereometric 2-year follow-up study of 60 hips
- Nunn D, Freeman M A, Hill P F, Evans S J. The measurement of migration of the acetabular component of hip prostheses. J Bone Joint Surg (Br) 1989; 71: 629–31
- Ornstein E, Franzen H, Johnsson R, Sandquist P, Stefansdottir A, Sundberg M. Migration of the acetabular component after revision with impacted morselized allografts: a radiostereometric 2-year follow-up analysis of 21 cases. Acta Orthop Scand 1999; 70: 338–42
- Paprosky W G, Martin E L. Structural acetabular allograft in revision total hip arthroplasty. Am J Orthop 2002; 31: 481–4
- Perka C, Ludwig R. Reconstruction of segmental defects during revision procedures of the acetabulum with the Burch-Schneider anti-protrusio cage. J Arthroplasty 2001; 16: 568–74
- Ranawat C S, Dorr L D, Inglis A E. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg (Am) 1980; 62: 1059–65
- Robinson A H, Palmer C R, Villar R N. Is revision as good as primary hip replacement? A comparison of quality of life. J Bone Joint Surg (Br) 1999; 81: 42–5
- Schatzker J, Wong M K. Acetabular revision. Clin Orthop 1999, 369: 187–97, The role of rings and cages
- Schmalzried T P, Shepherd E F, Dorey F J, Jackson W O, dela R M, Fa'vae F, McKellop H A, McClung C D, Martell J, Moreland J R, Amstutz H C. The John Charnley Award. Wear is a function of use, not time. Clin Orthop 2000, 381: 36–46
- Schreurs B W, Buma P, Huiskes R, Slagter J L, Slooff T J. Morsellized allografts for fixation of the hip prosthesis femoral component. A mechanical and histological study in the goat Acta Orthop Scand 1994; 65: 267–75
- Slooff T J, Buma P, Schreurs B W, Schimmel J W, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop 1996, 324: 108–15
- Snorrason F, Kärrholm J. Early loosening of revision hip arthroplasty. A roentgen stereophotogrammetric analysis J Arthroplasty 1990; 5: 17–29
- Stockl B, Beerkotte J, Krismer M, Fischer M, Bauer R. Results of the Muller acetabular reinforcement ring in revision arthroplasty. Arch Orthop Trauma Surg 1997; 116: 55–9
- van der Donk S, Buma P, Slooff T J, Gardeniers J W, Schreurs B W. Incorporation of morselized bone grafts: a study of 24 acetabular biopsy specimens. Clin Orthop 2002, 396: 131–41
- Van Koeveringe A J, Ochsner P E. Revision cup arthroplasty using Burch-Schneider anti-protrusio cage. Int Orthop 2002; 26: 291–5
- Walker P S, Mai S F, Cobb A G, Bentley G, Hua J. Prediction of clinical outcome of THR from migration measurements on standard radiographs. A study of cemented Charnley and Stanmore femoral stems J Bone Joint Surg (Br) 1995; 77: 705–14
- Winter E, Piert M, Volkmann R, Maurer F, Eingartner C, Weise K, Weller S. Allogeneic cancellous bone graft and a Burch-Schneider ring for acetabular reconstruction in revision hip arthroplasty. J Bone Joint Surg (Am) 2001; 83: 862–7