Abstract
Background The choice of plates or intramedullary nails for operatively treated humeral shaft fractures remains controversial, since randomized controlled trials have lacked sufficient power. A meta-analysis of existing trials would improve inferences regarding the treatment effect.
Methods We reviewed randomized trials in Medline, Cochrane and SciSearch, along with other sources of published randomized trials from 1969–2000. Of 215 citations identified, only 3 studies were included.
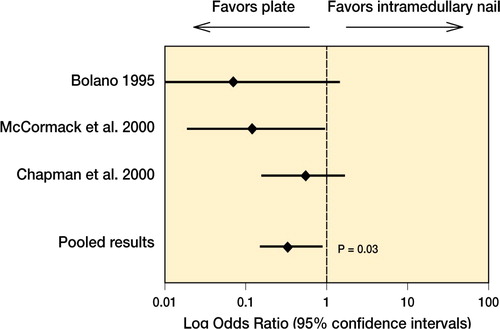
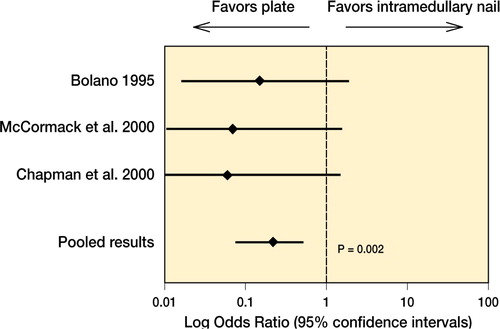
Results The 3 studies (involving 155 patients) were pooled, since they were homogeneous (p > 0.1). Plate fixation gave a lower relative risk of reoperation than intramedullary nailing (RR = 0.26, 95% CI 0.007–0.9, p = 0.03). This translated to a risk reduction of 74% for reoperation when plate fixation was employed. Thus, 1 reoperation could be prevented for every 10 patients treated with plates. Plate fixation also reduced the risk of shoulder problems in comparison to intramedullary nails (RR = 0.10, 95% CI 0.03–0.4, p = 0.002).
Interpretation Plate fixation of humeral shaft fractures may reduce the risk of reoperation and shoulder impingement. The cumulative evidence remains inconclusive, and a larger trial is needed in order to confirm these findings.
Most diaphyseal humerus fractures are managed nonoperatively (Mast et al. Citation1975, Sarmiento et al. Citation1977, Jupiter Citation1994, Balfour and Marrero Citation1995, Wallny et al. Citation1997). Surgery is indicated in non-operative treatment that fails to maintain fracture alignment, associated neurovascular injuries, segmental fractures, pathological fractures, open fractures, floating shoulder or elbow, and multiple trauma (Pollock et al. Citation1981, Bell et al. Citation1985, Brumback et al. Citation1986, Robinson et al. Citation1992, Amillo et al. Citation1993, Foster et al. Citation1993). The best surgical treatment—with either a plate or an intramedullary nail—remains controversial.
Recently, 4 randomized trials have compared plate and intramedullary nail fixation (Bolano Citation1995, Rodriguez-Merchan 1995, Chapman et al. Citation2000, McCormack et al. Citation2000), but all of them had a low number of patients. We conducted a systematic review and meta-analysis of randomized trials in order to assess the effect of plate fixation or intramedullary nailing of diaphyseal fractures of the humerus on rates of reoperation and other secondary outcomes. We reasoned that the statistical pooling of a meta-analysis would improve the precision of the estimates of the relative impact of plates and intramedullary nails and give stronger inferences to guide clinical decisions on the best course of action.
Methods
Eligibility criteria
The following eligibility criteria were used in selecting trials: 1. Target population: individuals with fractures of the humeral diaphysis, 2. Intervention: comparison of plate fixation and intramedullary nail fixation, 3. Primary outcome measure: reoperation (any subsequent humeral surgery following the index procedure resulting from nonunion, infection, nerve palsies, implant failures or impingement), 4. Methodological criteria: prospective, randomized or quasi-randomized controlled trials.
Identification of studies
We conducted a Medline search from 1969 to 2004, identifying the population (humeral shaft fracture), the intervention (fracture fixation and intramedullary and plate) and the methodology (clinical trial). MB and EHS reviewed the titles and identified all papers that might fulfill the eligibility criteria of the study. A search of the Cochrane database was also conducted. If the title suggested any possibility that it might be relevant, the abstract was retrieved. MB and EHS reviewed the abstracts, and chose potentially eligible studies for retrieval. Review of the complete articles included only the Methods sections, and this was carried out blind as to authorship, institutional address, journal, and the results obtained.
One of us (MB) reviewed the reference lists of all key articles for any additional eligible papers, which we then retrieved and reviewed for eligibility. We noted frequently cited articles and conducted a Science Citation Index search (SciSearch) to locate potentially relevant studies that have cited these articles. Additional strategies to uncover relevant studies included: 1) manual searches of tables of contents of 4 major orthopedics journals (Journal of Bone and Joint Surgery (American and British), Journal of Orthopaedic Trauma, Clinical Orthopaedics and Related Research) from 1996 to January 2004, 2) bibliography review of 2 major trauma textbooks in orthopedics (Rockwood and Green: Fractures in Adults, Browner, Jupiter and Swiontkowski: Skeletal Trauma), 3) review of titles of presentations or posters in programmes of 3 major orthopedics meetings (American Academy of Orthopaedic Surgeons, Orthopaedic Trauma Association, Canadian Orthopaedic Association) from 1996 to 2004, and 4) content expert(orthopedic surgeon with expertise in upper extremity fracture care. MDM). We repeated the process of judging study eligibility described above for all potentially relevant studies identified using these additional strategies.
Assessment of methodological quality
We (MB, EHS) abstracted all data and rated each study according to a 21-point study quality assessmentscale (Detsky et al. Citation1992). This scale grades the reporting of studies with respect to eligibility criteria, the adequacy of randomization, description of therapies, the assessment of outcomes, and statistical analysis.
Assessment of agreement between reviewers
Kappa, a measure of chance-corrected agreement, provided most estimates of agreement between reviewers for titles, abstracts and methods sections of potentially relevant articles (Fleiss Citation1975, Donner and Klar Citation1996). For continuous variables, we chose quantitated agreement using an intraclass correlation coefficient. We chose an a priori criterion of k = 0.65 or greater for adequate agreement (Sackett et al. Citation1991).
Data analysis
We pooled data across studies, and calculated relative risks and associated 95% confidence intervals for each outcome using the random effects model of DerSimonian and Laird (Citation1986). This model assumes that the trials included in this review represent a random sample of all the potentially available trials at present and in the future. The Breslow-Day test (1980) provided a test for the consistency or homogeneity of the estimates across studies, with a significance threshold of p < 0.1. We further calculated the The I2 statistic: the per-centage of between-study variability that is due to true differences between studies (heterogeneity) rather than sampling error (chance) can be used to quantify inconsistency among trials (Higgins and Thompson Citation2002). A value greater than 40% can be considered to reflect substantial heterogeneity.
Evaluation of heterogeneity
Prior to analyzing the data, we developed hypotheses regarding potential sources of heterogeneity in reoperation rates. We hypothesized that hetero-geneity may be due to differences in study quality, to whether studies were published or unpublished, and to whether randomization was concealed or not. For each potential determinant of heterogeneity, we compared relative risks across categories (Oxman et al. Citation1994).
Table 1. Study characteristics
Table 2. Results of statistical pooling
Results
Literature search
We identified 215 citations; 210 from Medline, 2 from content expert and 3 from manual searches of major orthopedics journals or meeting programs. The Cochrane database search did not yield any additional studies that were relevant. The weighted kappa (i.e., chance corrected agreement) for eligibility decisions based on the application of study inclusion criteria to abstracts was 0.8 (95% CI 0.7–0.9). 4 studies were included in our meta-analysis review—3 of which had been published (Rodriguez-Merchan 1995, Chapman et al. Citation2000, McCor-mack et al. 2000) and 1 that had not (an abstract: Bolano Citation1995). 1 of these studies (Rodrigues-Merchan Citation1995) was not considered for statistical pooling since flexible intramedullary devices had been used.
Assessment of methodological quality
gives detailed information regarding study methodology which was available in the 3 published studies. Agreement for the overall study quality score was substantial (intraclass correlation coefficient = 0.8, 95% CI 0.7–0.8). We obtained or confirmed data with authors from 2 of the 3 published trials.
Reoperation
The 3 clinical trials randomized a total of 155 patients and the median sample size was 21 patients. The results of the pooled statistical analyses are listed in . The relative risk of reoperation with plates was 0.3 (95% CI 0.07–0.9, p = 0.03) (). This translated into a substantial relative risk reduction of 74%. The difference in risk of reoperation with plates and intramedullary nails was 10% and this indicates that for every 10 patients treated with plates, 1 reoperation might be prevented (i.e. NNT = 10). Sensitivity analyses did not reveal any significant effect of study design, publication status, and nail insertion ().
Shoulder impingement
All 3 trials reported shoulder impingement data. The relative risk of shoulder impingement with plates was 0.1 (95% CI 0.03-–0.4, p = 0.002). This translated to a substantial relative risk reduction of 90%. The difference in risk of reoperation with plates and intramedullary nails (18%) indicated that for every 6 patients treated with plates, 1 shoulder impingement would be prevented (i.e. NNT = 6).
Table 3. Sensitivity analysis—reoperation rates
Nonunion, infection, and radial nerve palsies
Information on secondary outcomes was available in most studies (). Pooling of results across trials was appropriate given the relative homogeneity of the data (test for homogeneity, range of p-values 0.3–0.8). Plate fixation did not incur greater risks of nonunion, infection, or radial nerve palsy from the pooled analysis of studies.
Discussion
This is the first meta-analysis of randomized trials comparing plates and intramedullary nails in the treatment of diaphyseal fractures of the humerus.
Sometimes even the combined data on the main endpoint of interest (eg. reoperation) in an overview is barely sufficient to provide persuasive recommendations. Alternatively, a significant treatmenteffect should also be carefully considered for clinical sense and an underlying biological rationale (Yusuf Citation1987). In both cases, the review of other related outcomes (i.e. nonunions, infections and shoulder impingement) may help to clarify whether such effects are to be believed or not. For example, in those studies comparing plates with intramedullary nails, reoperation rates were significantly reduced with plates (relative risk = 0.3, p = 0.03). This large treatment effect may be an over-estimate, given that studies had small sample sizes and a low number of events. Given that the presenceof a nonunion or shoulder impingement with pain often necessitates a secondary procedure such as bone grafting to promote fracture healing, and implant removal or exchange, it is consistent thatreoperation risk will also be reduced. In general, the results of meta-analyses should be interpreted conservatively. The clinician can gain an indication of the degree of uncertainty of the potential benefit of one treatment over another by calculating standard confidence limits.
Studies avoid bias through random assignment of patients to treatment groups, concealment of ran domization, and blinding of investigators, patients and outcome assessors. Studies that fail to take these precautions tend to report larger estimates of the treatment effect (LeLorier et al. 1997). All the studies we included were randomized. However, the study that did not conceal random allocation (Rodrigues-Merchan Citation1995) reported a greater effect with plate fixation (85% risk reduction vs 55% risk reduction) than the 2 other studies which used envelopes (). Although individual patient information was not available for specific grades of soft tissue injury (only 17 patients with grade III open injuries) or degree of comminution, these overall analyses suggest that plate fixation of diaphyseal humeral fractures will yield more or less the same result in a variety of fracture morphologies.
In our meta-analysis of randomized trials, plate fixation has been observed to reduce the risk of a subsequent surgery by at least 12% and by as much as 93%. These large treatment effects should be interpreted with caution until confirmed by a large randomized trial. To date, only 155 patients have been randomized across 3 small randomized controlled trials. The event rate in the intramedullary nail group was 27%. If we assume a realistic treatmenteffect (a relative risk reduction of 25%), then we would require between 1,150 patients (alpha = 0.05, study power = 80%) and 2,180 patients (alpha = 0.01, study power = 90%) (). Thus, a larger trial is imperative to compare the true effect of plates and intramedullary nails in patients with humeral shaft fractures.
Figure 3. Cumulative meta-analysis assessing the effect of compression plating and intramedullary nailing on the need for reoperation in patients with humeral shaft fractures. The Lan-DeMets (LD) sequential monitoring boundary, which assumes a 27% control event rate (i.e. patients receiving intramedullary nailing) and a 25% relative risk reduction with 80% power and a two-sided alpha of 0.05, has not been crossed—indicating that the cumulative evidence is inconclusive.
No competing interests declared.
Author contributions
MB study design, concept, data collection, analysis and manuscript preparation. PJD study design, analysis and manuscript revision. MMK study design, identification, analysis and manuscript revision. ES study design, study quality assessment, analysis and manuscript revision.
- Amillo S., Barrios R. H., Martinez-Peric R. Surgical treatment of the radial nerve lesions associated with fractures of the humerus. J Orthop Trauma. 1993; 7: 211–5
- Balfour G. W., Marrero C. E. Fracture brace for the treatment of humerus shaft fractures caused by gunshot wounds. Orthop Clin North Am. 1995; 26: 55–63
- Bell M. J., Beauchamp C. G., Kellam J. K., McMurty R. Y. The results of plating humeral shaft fractures in patients with multiple injuries: the Sunnybrook experience. J Bone Joint Surg (Br). 1985; 67: 293–6
- Bolano L. E., Iaquinto J. A., Vasicek V. Operative treatment of humerus shaft fractures: A prospective randomized study comparing intramedullary nailing with dynamic compression plating. Presented at the Annual Meeting of the American Academy of Orthopaedic Surgeons. 1995
- Breslow N. E., Day D. E. Combination of results from a series of 2 x 2 tables; control of confounding. International Agency for research on cancer, LyonFrance. 1980: 136–46, In: Statistical methods in cancer research. Vol. 1. The analysis of case-control studies
- Brumback R. J., Bosse M. J., Poka A., Burgess A. R. Intramedullary stabilisation of humerus shaft fractures in patients with multiple trauma. J Bone Joint Surg (Am). 1986; 68: 960–70
- Chapman J. R., Henley M. B., Agel J., Benca P. J. Randomized prospective study of humeral shaft fracture fixation: Intramedullary nails versus plates. J Orthop Trauma. 2000; 14: 162–6
- DerSimonian R, Laird N. Meta-analysis of clinical trials Cont Clin Trials. 1986; 7: 177–88
- Detsky A. S., Naylor C. D., O'Rourke K., McGeer A. J., L'Abbe K. A. Incorporating variations in the quality of individual randomized trials into meta-analysis. J Clin Epidemiol. 1992; 45: 255–65
- Donner A., Klar N. The statistical analysis of kappa statistics in multiple samples. J Clin Epidemiol. 1996; 9: 1053–8
- Fleiss J. L. Measuring agreement between two judges on the presence or absence of a trait. Biometrics. 1975; 31: 651–9
- Foster R. J., Swiontkowski M. F., Bach A. W. Radial nerve palsy caused by open humeral shaft fractures. J Hand Surg. 1993; 18A: 121–4
- Higgins J. P., Thompson S. G. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–58
- Jupiter J. B. Managing fractures of the humeral shaft and distal humerus. J Musculoskel Med. 1994; 11: 35–44
- Le Lorier J., Gregoire G., Benhaddad A., LaPierre J., Derderian F. Discrepencies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997; 337: 536–42
- Mast J. W., Spiegel P. G., Harvey J. P., Harrison C. Fractures of the humeral shaft. Clin Orthop. 1975; 12: 254–62
- McCormack R. G., Brien D., Buckley R. E., McKee M. D., Powell J., Schemitsch E. H. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail: A prospective randomized trial. J Bone Joint Surg (Br). 2000; 82: 336–9
- Oxman A., Cook D. J., Guyatt G. H. User's guides to the medical literature: How to use an overview. JAMA. 1994; 272: 1367–71
- Pollock A. H., Drake D., Bovill E. G. Treatment of radial neuropathy associated with fractures of the humerus. J Bone Joint Surg (Am). 1981; 63: 239–43
- Robinson C. M., Bell K. M., Court-Brown C. M., McQueen M. M. Locked nailing of humeral shaft fractures. J Bone Joint Surg (Am). 1992; 74: 558–62
- Rodrigues-Merchan E. C. Compression plating versus hackethal nailing in closed humeral shaft fractures failing non-operative reduction. J Orthop Trauma. 1995; 9: 194–7
- Sackett D. L., Haynes R. B., Guyatt G. H., Tugwell P. Clinical epidemiologya basic science for clinical medicine. Little, Brown and Company, Toronto 1991; 30
- Sarmiento A., Kinman P. B., Galvin E. G. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg (Am). 1977; 59: 596–601
- Yusuf S. Obtaining medically meaninigful answers from an overview of randomized clinical trials. Stats Med. 1987; 6: 281–6
- Wallny T., Westermann K., Sagebiel C. Functional treatment of humeral shaft fractures:indications and results. J Orthop Trauma. 1997; 11: 283–7