Abstract
Background and purpose — Elderly patients may benefit from a dislocation low-risk dual-mobility (DM) articulation in total hip arthroplasty, but the best cup fixation method is unknown. We compared cup migration for cemented and cementless DM cups using radiostereometry.
Patients and methods — In a patient-blinded randomized trial, 60 patients (33 female) with osteoarthritis were allocated to cemented (n = 30) or cementless (n = 30) Avantage DM cup fixation. Criteria were age above 70 years, and T-score above –4. We investigated cup migration, periprosthetic bone mineral density (BMD), and patient-reported outcome measures (PROMs) until 24 months postoperative follow-up.
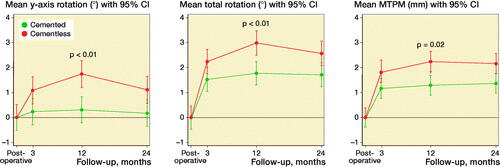
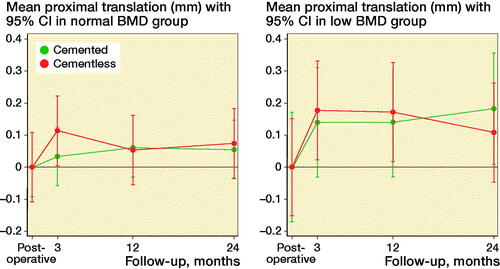
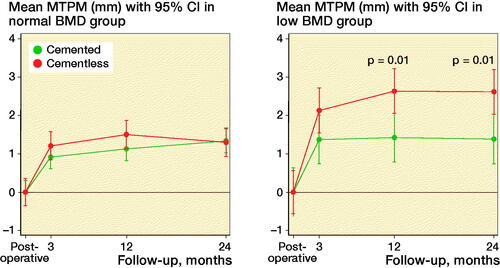
Results — At 24 months mean proximal cup migration was 0.11 mm (95% CI 0.00–0.23) for cemented cups and 0.09 mm (CI –0.09 to 0.28) for cementless cups. However, cementless cups generally migrated more than cemented cups at 12 and 24 months. Cemented cups had no measurable migration from 3 months’ follow-up, while cementless cups had not yet stabilized at 24 months in all rotations. Cementless cups showed statistically significantly more maximum total point motion (MTPM) at 12- and 24-month follow-up compared with cemented cups in patients with low systemic BMD (p = 0.01). Periprosthetic BMD changes did not statisticially significantly correlate to proximal migration in either cup fixation group (p > 0.05). PROMs improved similarly in both groups.
Interpretation — Cemented cups were well fixed at 3 months. The cementless cups migrated more in patients with low BMD, showed an inconsistent pattern of migration, and migrated in different directions during the first and second year without tendency to stabilization. Cemented fixation of the Avantage DM cup seems safer in elderly patients
The most common indication for revision of a conventional primary total hip arthroplasty (THA) is aseptic loosening of the components (SHAR 2016, NJR 2017, DHAR 2018).
Implant fixation method (i.e., cemented or cementless) in primary THA seems mainly based on the surgeon’s preference and national trends. The Danish Hip Replacement Registry report shows a decrease in the use of cemented cup fixation in osteoarthrosis (OA) patients above 70 years (DHAR 2018). This trend has also been described in the United Kingdom (UK) and Australian Joint Registries, while in Sweden and Norway cemented cup fixation is still the preferred fixation method in elderly patients (SHAR 2016, NAR 2017, NJR 2017).
The dual-mobility (DM) concept, with 2 articulation surfaces and increased jump distance, may decrease the dislocation rate and increase range of motion compared with standard single mobility (SM) THAs. The long-term survival and the best fixation method of the newer Avantage Reload DM cup in elderly patients is currently unknown but retrospective studies on other types of primary DM THAs suggest acceptable survival rates (Batailler et al. Citation2017) .
Excessive early (2-year) implant micromotion measured with radiostereometric analysis (RSA) is a strong predictor for later implant loosening and poor survival (Karrholm et al. Citation1997, Nieuwenhuijse et al. Citation2012, Pijls et al. Citation2012), and our primary aim was to investigate the early RSA-measured migration of cemented and cementless Avantage DM cups in elderly (> 70 years old) OA patients until 24 months’ follow-up. Secondary endpoints included systemic and periprosthetic bone mineral density (BMD) measurements, and clinical outcome scores.
Patients and methods
Design and patients
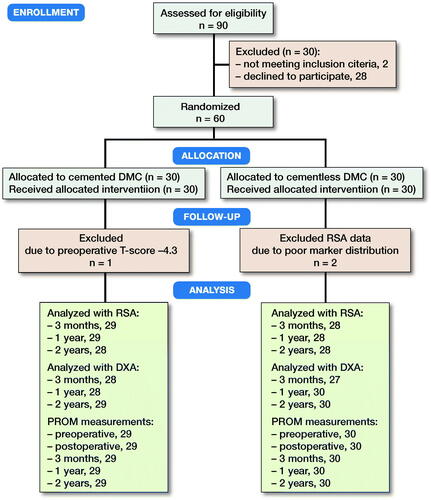
Between November 2014 and January 2018, we performed a Level I prospective, randomized, patient-blinded, parallel group trial at Regional Hospital West Jutland, Holstebro, Denmark. Inclusion criteria were primary osteoarthrosis, age above 70 years, informed consent, and only 1 hip operated and with adequate bone quality for insertion of a cementless acetabular component as judged by the surgeons on radiographs and intraoperatively. Exclusion criteria were vascular or neuromuscular disease in the operated leg, fracture sequelae, avascular necrosis of the femoral head, alcohol abuse, and severe osteoporosis (T-score ≤ –4.0). 60 patients (33 female) were included and block randomized (using a computerized algorithm) to either cemented (n = 30) or cementless (n = 30) cup fixation (). There is no “acceptance limit” for “low systemic BMD/T-score.” We arbitrarily chose a T-score limit of –4.0 and thus excluded patients with severe osteoporosis.
Prosthesis, surgery, and rehabilitation
The Avantage Reload cemented and cementless DM cup (ZimmerBiomet, Warsaw, IN, USA) has been commercially available since 2005. The external surface of the cemented Avantage Reload metal shell has a bright polish (Ra max 0.4 µm), and the inner articulate surface is highly polished. Vacuum-mixed Palacos R + G bone cement (Heraeus Medical, Wehrheim, Germany) was used for cemented fixation. The cementless Avantage Reload metal shell has a double coating with a projection vacuum plasma (VPS) titanium coating (Ra > 15 µm) and synthetic hydroxyapatite (HA) (150 ± 50 µm) to create a rough surface finish (Ra > 11 µm). Exeter highly-polished stems (Stryker Corporation, Kalamazoo, MI, USA) with vacuum mixed Palacos R + G bone cement (Heraeus Medical, Wehrheim, Germany) were used in all patients. A 28-mm chrome-cobalt femoral head was used in all cases. Vitamin E-infused highly cross-linked polyethylene liner (GUR 1050) was used in both cemented and cementless cups. All liners were vacuum-packed and gamma sterilized with a minimum of 25 kGy.
All patients were operated by 1 of 2 highly experienced orthopedic hip surgeons. The sequentially numbered sealed envelopes were hidden from investigators until directly prior to surgery to prevent bias. On the day of surgery, a sealed randomization envelope was opened to allocate the patient to either cemented or cementless cup fixation. Prophylactic cefuroxime 1.5 g was administrated intravenously before surgery and twice postoperatively with an 8-hour interval. After bone preparation, 6–8 tantalum beads (1 mm) were inserted into the periacetabular bone during surgery. All patients were operated by a posterolateral approach and received the same rehabilitation program, allowing full weight-bearing immediately after surgery.
Radiostereometric analysis
Stereoradiographs were obtained within the first postoperative 2 days (mean 1.1, range 1–14) and at 3, 12, and 24 months after surgery. All examinations were performed with the patient in a supine position with a uniplanar calibration box (Carbon Box 19, RSAcore, Leiden, The Netherlands) located underneath the examination table. The anatomical axis of the leg was parallel to the y-axis of the calibration box. Cup migration was evaluated on all 3 follow-up stereoradiographs with the postoperative stereoradiograph as the baseline reference.
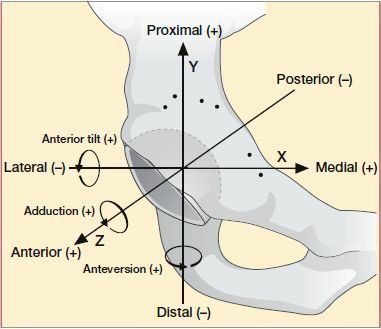
The radiostereometric analysis was performed with Model-Based RSA version 4.10 software (RSAcore, Leiden, The Netherlands) using computer-aided design (CAD) implant models provided by the manufacturer (ZimmerBiomet, Warsaw, IN, USA). We measured cup migration (center of 3D model points) in the coordinate system of the calibration box as described in the Guidelines for RSA of Implants (Valstar et al. Citation2005) (). Total translation (TT) and total rotation (TR) were both calculated using Pythagoras’ theorem (sqrt (x2 + y2 + z2). The mean condition number (CN) of the bone marker model was 83 (SD 47) and the rigid body error (ME) was mean 0.24 (SD 0.06). A minimum of 3 bone markers was accepted and the cut-off points for CN and ME were maintained at 150 and 0.35, respectively (Valstar et al. Citation2005).
All patients were subject to double examinations at the 3-month RSA examination according to guidelines (, see Supplementary data) (Valstar et al. Citation2005).
Table 1. RSA measurement error based on double-examination stereoradiographs
The position of the fitted implant CAD model on the postoperative stereoradiograph pose-estimation served as inclination and anteversion estimates and were read from the Model-Based RSA software (RSAcore, Leiden, The Netherlands).
Dual-energy X-ray absorptiometry (DXA) scans
Preoperatively all patients underwent spine and dual hip DXA scan to determine systemic BMD and T-score. The mean time from preoperative DXA scan to surgery was 20 days (14–71). Postoperatively (within 4 days after surgery) and at 3, 12, and 24 months after surgery, quantitative measurements of the periprosthetic BMD (g/cm2) was acquired with DXA scans using a GE Lunar iDXA scanner (General Electric, Chicago, IL, USA), and analyses were performed using enCORE version 16 software (https://www.encore.com/). Patients were placed in supine position with the body parallel to the examination table and the feet fixed to a device that kept the halluces pointing straight up. Analysis was performed according to Wilkinson 4 regions of interest (ROI) and precision ranged from 3% to 13% in cemented cup fixation and 3% to 6% in cementless cup fixation (, see Supplementary data) (Wilkinson et al. Citation2001). A template was applied to the baseline scan, and the ROIs were subsequently copied to align with the bone-border on follow-up scans. ROI 2 and 3 were adjusted in height on the baseline scan depending on the cup size (each ROI was 1 half cup height) and ROIs 1 and 4 had fixed sizes ().
Figure 3. Wilkinson regions of interest (ROI) 1–4. Only the bone areas within yellow lines are included in the analysis.
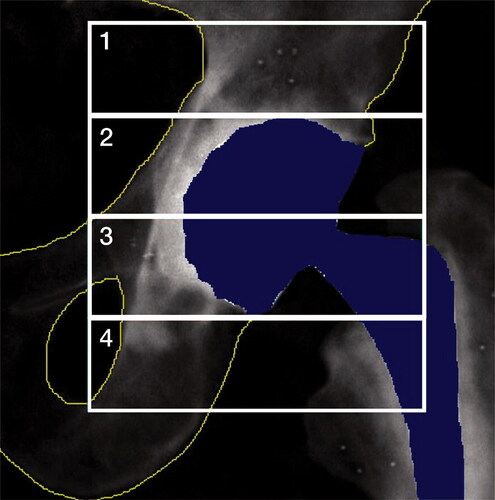
Table 2. DXA (g/cm2) measurement error based on 3-month double-examination DXA scans for cemented and cementless cup fixation
Clinical outcome measures and complications
Clinical outcome measures were assessed by Harris Hip Score (HHS), Oxford Hip Score (OHS) (Paulsen et al. Citation2012), patient-reported quality of life (EQ-5D) (Brooks Citation1996), and visual analog scale (VAS) for hip pain preoperatively and at 3, 12, and 24 months after surgery.
Statistics and sample size
The primary endpoint was proximal cup migration at the 24-month follow-up (Pijls et al. Citation2012). Linear mixed-effect models were used to determine whether cup fixation and BMD had a significant effect on cup migration at 3-, 12-, and 24-month follow-up. This was used as it takes the correlation of measurements on the same patient into account and includes all patients/missing values effectively. The analysis was modelled as a function of fixation with the interaction of time and fixation as fixed effects. Bonferroni correction was applied to migration data (primary end-point), when linear mixed models showed significant p-values. Model estimates are reported as means with 95% confidence intervals (CI). The secondary endpoints were measurements of periprosthetic BMD, clinical outcomes of HHS, OHS, and EQ-5D, and VAS (rest and activity) for pain. Subgroup analyses (mixed model) were performed between cup fixation (cemented/cementless) and cup migration when stratified to normal (T-score ≥ –1.0) or low (T-score < –1.0) preoperative BMD. Student’s t-test was used for normally distributed data. When data were not normally distributed according to a Shapiro–Wilks test, a non-parametric (Mann–Whitney) test was used. Data were analyzed as of the date of the last data collection (January 2018).
Proximal cup acceptance migration thresholds at 24 months’ follow-up was assessed according to Pijls et al. (Citation2012).
There are no previous migration data for the Avantage DM cup that could be used for sample size calculation. The pilot study included both cemented and cementless cups in patients (n = 5) older than 70 years. A pre-study sample size calculation using 2-sample mean test for a minimal relevant proximal cup migration difference of 0.2 mm (Pijls et al. Citation2012) with a mean cup migration of 0.2 mm (SD 0.27) (pilot study), power 80%, alpha 0.05, estimated 29 patients in each group. 30 patients per group were included to account for dropout. Statistical significance was set at 0.05. Stata version 13.1 (StataCorp, College Station, TX, USA) was used for statistical analysis.
Ethics, funding, and potential conflicts of interest
The study was conducted in accordance with the Helsinki Declaration. Patients gave informed consent before entering the study. The study was approved by the Central Danish Regional Committees on Biomechanical Research Ethics (Journal no. 1-10-72-209-14) and the study was registered with ClinicalTrials.gov (NCT02404727). ZimmerBiomet Inc. and The Danish Rheumatism Association supported the study financially but had no influence on the manuscript or publication. The authors have no conflicts of interest.
Results
The baseline demographics of all patients are presented in .
Table 3. Descriptive baseline characteristics of the patients, implants, and surgery. Values are mean (range) unless otherwise specified
Radiostereometric analysis
Translations and rotations, including TT, TR, and MTPM (mean and CI), are presented in , and statistically significant migrations are presented in . Cemented cups showed no statistically significant translation (p > 0.3) or rotation (p > 0.2) during the 24-month follow-up time. Cementless cups had no statistically significant translations (p > 0.20) during 24-month follow-up, but showed rotation about all orthogonal axes and in TR during the 24-month follow-up (). Cemented cups migrated 0.54 (CI 0.44–0.65) and cementless cups migrated 1.08 (CI 0.71–1.46) MTPM between 12 months and 24 months with a mean difference of –0.54 (CI –0.94 to –0.14, (p = 0.01).
Table 4. Translations along and rotations about the x-, y-, and z-axis for cemented and cementless cups presented as mean (95% CI)
Table 5. Cup rotations and MTPM between follow-ups within each cup fixation group presented as mean difference (95% CI)
By 24 months, 21/28 of the cemented cups showed proximal cup migration < 0.2 mm, 7/28 were between 0.2 and 1.0 mm, and no cemented cups had proximal cup migration > 1.0 mm. By 24 months, 18/28 of the cementless cups showed proximal cup migration < 0.2 mm, 9/28 were between 0.2 and 1.0 mm, and 1/28 cementless cup showed > 1.0 mm proximal cup migration. When stratifying patients into 2 subgroups based on preoperative systemic BMD (normal and low BMD), we found no within-subgroup difference in proximal cup migration between cemented and cementless cup fixation at any follow-up (p > 0.3; , see Supplementary data). The mean 24-month proximal cup migration in the normal BMD group was 0.05 mm (CI –0.08– 0.18) for cemented cups and 0.07 mm (CI –0.17–0.32) for cementless cups (, see Supplementary data). Mean 24-month proximal cup migration in the low BMD group was 0.18 mm (CI 0.05–0.31) for cemented cups and 0.11 mm (CI –0.07–0.29) for cementless cups (, see Supplementary data).
The postoperative inclination angle was higher in cemented cups compared with cementless cups (p = 0.01) (). The postoperative anteversion angle did not differ between the two fixation methods (p = 0.9) ().
Further analyses on BMD groups showed that MTPM was statistically significantly higher at 12- and 24-month follow-up in cementless cups compared with cemented cups in the low BMD group (p = 0.01, ), which could be explained by a higher cup migration in x-translation (p = 0.04 at 24 months), y- rotation (p < 0.001, p = 0.03, at 12 and 24 months respectively), and z-rotation (p = 0.04 at 24 months). Likewise, TT and TR was higher for cementless cups compared with cemented cups in the low BMD groups at 12 and 24 months (all p < 0.03).
Percentage change in periprosthetic BMD
Percentage BMD changes are presented in . We did not find a statistically significant correlation between percentage BMD change and proximal cup migration in cemented or cementless cups during follow-up (p > 0.06). However, this does not imply that there is no true correlation between percentage BMD change and proximal cup migration. The strongest correlation between proximal cup migration and percentage BMD was found at 24 months in the cementless group in ROI 4 (CI –0.68–0.00, p = 0.06).
Table 6. BMD change in the 4 ROIs around the acetabular component presented as mean (95% CI) percentage change from the baseline values at 3, 12, and 24 months
Clinical outcome measures and complications
Clinical results (HHS, OHS, EQ-5D, VAS) were similar between the 2 fixation groups during 24-month follow-up (, see Supplementary data). The 2 groups showed similar clinical improvement from preoperative to 24-month follow-up. The biggest difference between fixation groups was found in VAS at activity, mean diff = 1.0 (CI 0.02–2.1, p > 0.07).
Table 7. Mean (SD) scores for the HHS, OHS, EQ-5D, and VAS for pain
1 patient (cementless cup) underwent revision surgery (liner and femoral head exchange) 3 months after the index surgery due to an intraprosthetic dislocation. 2 weeks after revision, the patient underwent a 1-stage debridement, washout, femoral head and liner exchange, and antimicrobial treatment for 6 weeks due to deep infection (Staphylococcus aureus). Hereafter, the patient had a well-functioning hip and continued regular RSA follow-up. There were no large articulation dislocations in either fixation group during the follow-up period.
Discussion
To our knowledge, this is the first RSA study of the DM articulation concept in elderly OA patients comparing cemented and cementless cup fixation in a randomized study. The key findings were similar proximal cup migration between fixation groups, but cementless cups migrated more on absolute measures, migrated more in patients with low BMD, and had not stabilized at 24 months, whereas cemented cups were stable from 3 months.
Radiostereometric analysis
The association between early high proximal cup migration and the elevated risk of aseptic cup loosening and later revision have previously been described (Nieuwenhuijse et al. Citation2012, Pijls et al. Citation2012). In relation to Pijls’ (2012) thresholds for proximal cup migration, we identified 7 cemented cups (range 0.23–0.71 mm) and 9 cementless cups (range 0.2–0.75 mm) “at risk” of later revision in our study, but we observed no cemented cups and 1 cementless cup (1.16 mm) with “unacceptable” proximal migration (Pijls et al. Citation2012). In relation to Nieuwenhuijse’s definition we observed no cups exceeding 1.76 mm proximal migration and 1 cementless cup (6.39°) with abduction (z-axis) above 2.53° (Nieuwenhuijse et al. Citation2012).
Cementless cups are inserted by under-reamed technique, and the initial rim-fit may be lost over time resulting in a final bottoming in the acetabulum (Rohrl et al. Citation2004). However, we saw 1 cementless cup with large proximal migration, and in general no measurable translation over time in the cementless group. Cementless cups did, however, have more rotation overall, over time, and in opposite directions before and after 12 months, as compared with cemented cups. A clinical significance level in relation to rotation measures has not been established. The difference in cup y-rotation was evident at 3 months and was probably an effect of final osseointegration.
Cemented cups were inserted with significantly higher inclination angle compared with cementless cups, which may be explained by surgeons’ preference for free-hand insertion of cemented Avantage DM cups due to affection of the cup–cement interface before cement curing with disconnection of the cup-guide. However, our findings suggest that bone fixation of cemented cups is less sensitive to increased cup angulation compared with cementless cups. This is also in line with a study on all-poly cemented and cementless cups (Kadar et al. Citation2012).
RSA evaluations of elderly patients with OA treated with a primary THA are scarce. Direct comparisons with previous RSA reports are difficult due to alternative ways of presenting data, methods of fixation, marked differences in patient demographics, implant design, surgical approach, and follow-up time. Based on 24-month proximal migration as an indicator for primary stability our findings for cemented and cementless fixation methods are comparable, and in many cases lower than reported in other studies on cemented and cementless cup fixation in primary THA (Lazarinis et al. Citation2014, Salemyr et al. Citation2015, Finnila et al. Citation2016).
Radiostereometric analysis and preoperative BMD status
Cementless ceramic-on-ceramic THA has shown statistically significantly and clinically relevant higher proximal migration and migration until 12-month follow-up in women with low BMD (lower T-score limit of –3.5) compared with women with normal BMD at 24-month follow-up (Finnila et al. Citation2016). These findings are inconsistent with the present study where we observed similar proximal migration in the normal BMD and low BMD groups and no migration within fixation groups of the BMD subgroups during follow-ups. The mean 24-month proximal migration in our cementless group with low BMD of 0.11 mm (CI –0.07 to 0.29) was lower than reported in the study by Finnilä et al. (2016) of 0.29 mm (CI 0.20–0.39), suggesting early initial proximal cup stability with Avantage DM cups, even in the low BMD group, and in both cemented and cementless cup fixation. However, in the low BMD group, cementless cups showed statistically significantly more migration in MTPM, x-axis translation, y-axis rotation, TT and TR compared with cemented cups, suggesting that cementless cup fixation is not preferable in patients with preoperative low BMD. Only 1 study reports proximal cup migration in cemented cups with stratification to normal and low BMD but unclear definition of osteoporosis makes direct comparison troublesome (Digas et al. Citation2004).
Periprosthetic BMD measurements
Differences in BMD change in cemented and cementless fixation may be a result of different load transfer mechanisms leading to different bone remodeling profile (Digas et al. Citation2006). In cementless cups, forces are transmitted sideways to the periphery, rather than proximally, which leads to reduced load transfer in the most cranial/proximal area (Digas et al. Citation2006, Lazarinis et al. Citation2014) with local bone resorption caused by stress-shielding. This might explain the greater bone loss observed in ROI 1 and 2 of cementless cups compared with cemented cups in our study. Conversely, the increased BMD in ROI 3 and lesser BMD reduction in ROI 4 in cementless cups compared with cemented could be due to the increased traction forces in cementless cups acting as a stimulus for preservation of bone or even increase in BMD (Salemyr et al. Citation2015). The percentage BMD changes in the 2 cup fixation methods did not correlate to proximal cup migration.
Clinical outcome measures
There was no statistically significant difference in postoperative clinical evaluations (quality of life measured by EQ-5D, or hip status measured by HHS and OHS) between cemented and cementless cup groups. The 2-year clinical evaluations of cemented and cementless fixation translates to either very good or excellent end-results (Nilsdotter and Bremander 2011).
Cup fixation method in the elderly
There is no clear consensus on the choice of the cemented or cementless cup fixation method in elderly patients, and registry reports from the UK, Australia, Sweden, Norway, and Denmark reveal no clear overall tendency regarding cup fixation methods in the elderly (SHAR 2016, NAR 2017, NJR 2017, DHAR 2018). While many registries report a tendency towards more cups being inserted with cementless fixation, their superiority is not supported in the literature (Troelsen et al. Citation2013, Makela et al. Citation2014).
Limitations and strengths
The strength of this study is the patient-blinded randomized controlled study design and a large group available for migration analysis. RSA is a validated surrogate measure of later implant loosening, but other complications, i.e., wear-induced osteolysis or fractures in the cement mantle, may not be detected with early RSA (Nieuwenhuijse et al. Citation2012). Linear mixed-model analysis enabled us to use all the available data. A high number of radiographs were available for analysis, and the number of patients with available 24-month RSA measurements was equal in both fixation groups. Only 2 patients in the cementless group were excluded due to poor marker distribution. In the cemented group 1 patient was excluded due to a mistake in identification of severe preoperative osteoporosis (preoperative T-score of –4.3) and the 24-month follow-up RSA radiographs of 1 patient were accidentally lost. BMD is typically higher around cemented cups due to opacity of the cement and therefore net BMD measurements are not direct comparable between cementless and cemented cups, and for this reason we compared percentage BMD changes (Jayasuriya and Wilkinson Citation2014). The high inclusion rate improves the external validity of our study, but results can be generalized only to patients older than age 70 years with a T-score above –4.
Conclusion
At minimum 2 years’ follow-up cemented and cementless DM cups had similar proximal mean migration below the recommended acceptance threshold, yet more cups in the cementless group migrated above the acceptance levels, which is of clinical importance. The cementless cups migrated more in patients with low BMD, showed an inconsistent pattern of migration, and migrated in different directions during the first and second year without tendency to stabilization. On the other hand, cemented cups were well fixed at 3 months. Cemented fixation of the Avantage DM cup seems safer in elderly patients; however, long-term studies are warranted.
Supplementary data
, and are available as supplementary data in the online version of this article, http://dx.doi.org/ 10.1080/17453674.2020.1720978
ST-J, TBH, and MS designed the study and validated the methods. ST-J performed all the follow-up examinations. SBM and ST-J performed the statistical analyses. ST-J wrote the initial manuscript, and all authors revised it.
Note: All product names are for identification purposes only, and may be trademarks of their respective owners.
Acta thanks Søren Kold and Johan Kärrholm for help with peer review of this study.
Supplemental Material
Download PDF (70.7 KB)- Batailler C, Fary C, Verdier R, Aslanian T, Caton J, Lustig S. The evolution of outcomes and indications for the dual-mobility cup: a systematic review. Int Orthop 2017; 41(3): 645–59.
- Brooks R. EuroQol: the current state of play. Health Policy 1996; 37(1): 53–72.
- DHAR. The Danish Hip Arthroplasty Registry. National annual report 2018; 2018.
- Digas G, Thanner J, Anderberg C, Karrholm J. Bioactive cement or ceramic/porous coating vs. conventional cement to obtain early stability of the acetabular cup: randomised study of 96 hips followed with radiostereometry. J Orthop Res 2004; 22(5): 1035–43.
- Digas G, Karrholm J, Thanner J. Different loss of BMD using uncemented press-fit and whole polyethylene cups fixed with cement: repeated DXA studies in 96 hips randomized to 3 types of fixation. Acta Orthop 2006; 77(2): 218–26.
- Finnila S, Moritz N, Svedstro M E, Alm J J, Aro H T. Increased migration of uncemented acetabular cups in female total hip arthroplasty patients with low systemic bone mineral density: a 2-year RSA and 8-year radiographic follow-up study of 34 patients. Acta Orthop 2016; 87(1): 48–54.
- Jayasuriya R L, Wilkinson J M. Pelvic periprosthetic bone mineral density measurement around cemented vs cementless acetabular prostheses. J Clin Densitom 2014; 17(1): 116–20.
- Kadar T, Furnes O, Aamodt A, Indrekvam K, Havelin L I, Haugan K, Espehaug B, Hallan G. The influence of acetabular inclination angle on the penetration of polyethylene and migration of the acetabular component: a prospective, radiostereometric study on cemented acetabular components. J Bone Joint Surg Br 2012; 94(3): 302–7.
- Karrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses: review of methodology and clinical results. Clin Orthop Relat Res 1997; (344): 94–110.
- Lazarinis S, Milbrink J, Mattsson P, Mallmin H, Hailer N P. Bone loss around a stable, partly threaded hydroxyapatite-coated cup: a prospective cohort study using RSA and DXA. Hip Int 2014; 24(2): 155–66.
- Makela K T, Matilainen M, Pulkkinen P, Fenstad A M, Havelin L, Engesaeter L, Furnes O, Pedersen A B, Overgaard S, Karrholm J, Malchau H, Garellick G, Ranstam J, Eskelinen A. Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. BMJ 2014; 348: f7592.
- NAR. Norwegian National Registry for Arthroplasty annual report 2017; 2017.
- Nieuwenhuijse M J, Valstar E R, Kaptein B L, Nelissen R G. Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups: results from ten years of follow-up with Roentgen stereophotogrammetric analysis (RSA). J Bone Joint Surg Am 2012; 94(10): 874–80.
- Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken) 2011; 63(Suppl 11): S200–S7.
- NJR. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Annual report 2017; 2017.
- Paulsen A, Odgaard A, Overgaard S. Translation, cross-cultural adaptation and validation of the Danish version of the Oxford hip score: assessed against generic and disease-specific questionnaires. Bone Joint Res 2012; 1(9): 225–33.
- Pijls B G, Nieuwenhuijse M J, Fiocco M, Plevier J W, Middeldorp S, Nelissen R G, Valstar E R. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survival studies. Acta Orthop 2012; 83(6): 583–91.
- Rohrl S M, Nivbrant B, Strom H, Nilsson K G. Effect of augmented cup fixation on stability, wear, and osteolysis: a 5-year follow-up of total hip arthroplasty with RSA. J Arthroplasty 2004; 19(8): 962–71.
- Salemyr M, Muren O, Eisler T, Boden H, Chammout G, Stark A, Skoldenberg O. Porous titanium construct cup compared to porous coated titanium cup in total hip arthroplasty: a randomised controlled trial. Int Orthop 2015; 39(5): 823–32.
- SHAR. The Swedish Hip Arthroplasty Register annual report 2016; 2016.
- Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res 2013; 471(7): 2052–9.
- Valstar E R, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76(4): 563–72.
- Wilkinson J M, Peel N F, Elson R A, Stockley I, Eastell R. Measuring bone mineral density of the pelvis and proximal femur after total hip arthroplasty. J Bone Joint Surg Br 2001; 83(2): 283–8.