Abstract
Background and purpose — Femoral neck fractures are commonly treated with cemented or uncemented hemiarthroplasties (HA). We evaluated differences in mortality and revision rates in this fragile patient group.
Patients and methods — From January 1, 2007 until December 31, 2016, 22,356 HA procedures from the Dutch Arthroplasty Register (LROI) were included. For each HA, follow-up until death, revision, or end of follow-up (December 31, 2016) was determined. The crude revision rate was determined by competing risk analysis. Multivariable Cox regression analyses were performed to evaluate the effect of fixation method (cemented vs. uncemented) on death or revision. Age, sex, BMI, Orthopaedic Data Evaluation Panel (ODEP) rating, ASA grade, surgical approach, and previous surgery were included as potential confounders.
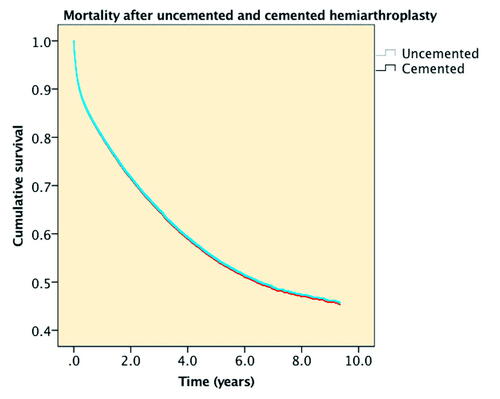
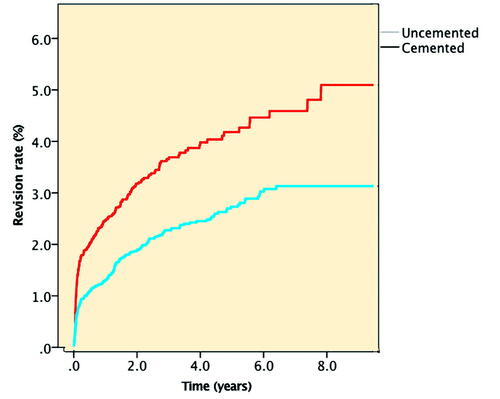
Results — 1-year mortality rates did not differ between cemented and uncemented HA. 9-year mortality rates were 53% (95% CI 52–54) in cemented HA compared to 56% (CI 54–58) in uncemented HA. Multivariable Cox regression analysis showed similar mortality between cemented and uncemented HA (HR 1.0, CI 0.96–1.1). A statistically significantly lower 9-year revision rate of 3.1% (CI 2.7–3.6) in cemented HA compared with 5.1% (CI 4.2–6.2) in the uncemented HA was found with a lower hazard ratio for revision in cemented compared with uncemented HA (HR 0.56, CI 0.47–0.67).
Interpretation — Long-term mortality rates did not differ between patients with a cemented or uncemented HA after an acute femoral neck fracture. Revision rates were lower in cemented compared with uncemented HA.
The number of hemiarthroplasties (HA) after displaced femoral neck fracture increases as a result of global aging, and inferior results and high risk of reoperation after internal fixation. Although the literature on the decision to use cemented or uncemented HA may favor a cemented implant, both techniques are currently used. The use of bone cement is associated with bone cement implantation syndrome (BCIS) characterized by hypoxia, hypotension, loss of consciousness around the time of bone cementation, and intraoperative death (Olsen et al. Citation2014, Rutter et al. Citation2014). More intraoperative complications including intraoperative death were found in cemented HA in the Norwegian register (Gjertsen et al. Citation2012, Talsnes et al. Citation2013). However, no differences in mortality were found after 1 week (Costain et al. Citation2011, Yli-Kyyny et al. Citation2014). More studies including randomized controlled trials (Deangelis et al. Citation2012, Taylor et al. Citation2012) and registry studies (Costa et al. Citation2011, Ekman et al. Citation2019) did not show differences in mortality between cemented and uncemented HA. Randomized controlled trials (Taylor et al. Citation2012, Langslet et al. Citation2014, Inngul et al. Citation2015) and register studies (Gjertsen et al. Citation2012, Yli-Kyyny et al. Citation2014) have shown that the use of uncemented implants could result in a higher risk of periprosthetic fractures. A meta-analysis by Li et al. (Citation2013) concluded that differences in several outcome parameters indicated cemented hemiarthroplasty to be superior to the uncemented counterpart. However, a serious flaw in this analysis is that several studies were included using an outdated stem like the Austin Moore (Sonne-Holm et al. Citation1982, Emery et al. Citation1991, Parker et al. Citation2010) and the experimental uncemented Thomson stem (Sadr and Arden Citation1977). The use of a prosthesis without Orthopaedic Data Evaluation Panel (ODEP) rating > 3A could influence outcome and is therefore discouraged (Grammatopoulos et al. Citation2015). A recent review by Rogmark and Leonardsson (Citation2016) included 5 randomized studies comparing modern uncemented and cemented hemiarthroplasties. They found no differences in mortality, but more periprosthetic fractures in uncemented cases. We compared cemented and uncemented HA after an acute hip fracture with primary outcome mortality and revision rate. Data from the Dutch Arthroplasty Register (LROI) were used and the cohort of cemented HAs was compared with uncemented HAs, accounting for the ODEP rating and other confounders.
Patients and methods
The Dutch Arthroplasty Register (LROI) is a nationwide population-based register that includes information on arthroplasties in the Netherlands since 2007. It covers 100% of Dutch hospitals and has a completeness of reporting of 70% for primary orthopedic HAs in 2013 to 88% in 2016 (Van Steenbergen et al. Citation2015).
The LROI database contains information on patient, procedure, and prosthesis characteristics registered by registrars from each hospital. For each component a product number is registered to identify the characteristics of the prosthesis. Vital status of all patients was obtained actively on a regular basis from Vektis, the national insurance database on health care in the Netherlands, which records all deaths of Dutch citizens. The LROI requires the informed consent of patients and uses an opt-out system in this respect.
For this study, we included all HA procedures in patients with an acute femoral neck fracture registered by orthopedic surgeons in the LROI from January 1, 2007 until December 31, 2016 (N = 22,351). All femoral stems were classified as ODEP rating 3A or other/no rating by checking the prosthesis in the ODEP database (http://www.odep.org.uk). Prostheses that were not available in the ODEP database were manually explored by the researchers. When these prostheses were not found as ODEP rating ≥ 3A, they were classified as “no ODEP 3A rating.” Other parameters such as age, sex, BMI, ASA classification, and previous surgery on the affected hip were used from the LROI database. BMI and smoking have only been available in the LROI since 2014. Closed reductions after a dislocation or incision and drainage for infection were not included in the LROI, as in these procedures no component exchange was performed. The median follow-up was 1.8 years (0–10).
Statistics
Kaplan–Meier survival analysis was performed to examine the survival rates of the patients over time. A multivariable Cox proportional hazard analysis was performed to examine the effect of fixation type (i.e., cemented vs. uncemented) on death after HA. Demographic variables such as age, sex, ASA classification, BMI, and smoking habit were included as covariates. Age and BMI with impossible values were excluded.
Survival time for revision was calculated as the time from primary HA to the first revision arthroplasty for any reason, death of the patient, or the end of the study follow-up (December 31, 2016). Cumulative crude incidence of revision was calculated using competing risk analysis where death was considered to be the competing event (Lacny et al. Citation2015, Wongworawat et al. Citation2015). Multivariable Cox proportional hazard analyses were performed to examine the effect of fixation type on revision. Demographic variables and possible risk factors including approach, ODEP rating (> 3A vs. other/no rating), and previous surgery on the affected hip were included as covariates.
Furthermore, the reasons for revision were compared between cemented and uncemented HA. Finally, multivariable logistic regression analyses were performed on the revisions (n = 517) to examine independent risk factors for revision due to dislocation, infection, femoral loosening, periprosthetic fracture, or other reasons for revision. Demographic variables and possible risk factors were included as covariates in the multivariable logistic regression analysis. All confidence intervals (CI) are defined as 95%. For the CI, we assumed that the number of observed cases followed a Poisson distribution.
Ethics, funding, and potential conflicts of interest
Ethical approval was not required for this study. Our Foundation for Orthopedic Research, Care and Education (FORCE) receives money from Zimmer-Biomet, Stryker, and Mathys not directly related to this study. SB is a consultant for Stryker.
Results
Patients and procedure characteristics are given in .
Table 1. Patient characteristics of cemented (n = 14,736) and uncemented (n = 7,615) hemiarthroplasties in the Netherlands 2007–2016. Values are number (%) unless otherwise specified
Mortality
1-week mortality was 2.1% (CI 1.8–2.3) in the cemented HA group compared with 1.8% (CI 1.6–2.2) in the uncemented HA group. 1-month mortality was 6.0% (CI 5.6–6.4) in the cemented HA group compared with 5.4% (CI 4.9–6.0) in the uncemented HA group. 1-year mortality was 19.7% (CI 19.1–20.4) in the cemented HA group compared with 19.5% (CI 18.6–20.4) in the uncemented HA group. 9-year mortality rates were 53% (CI 52–54) in the cemented HA group compared with 56% (CI 54–58) in the uncemented HA group (). Univariable Cox regression analysis showed no statistically significant difference in mortality between patients with a cemented and an uncemented HA (HR 0.99, CI 0.95–1.04). Multivariable Cox regression analysis showed an HR of 1.00 (CI 0.96–1.05) adjusted for age at surgery, sex, and ASA classification. In a subset from 2014 to 2016 that included also BMI and smoking, no statistically significant difference in mortality in cemented and uncemented HA was found (HR 1.06, CI 0.97–1.15).
Revision
Competing risk analysis showed a lower crude revision rate at 1 month (0.5%, CI 0.4–0.7), 1 year (1.3%, CI 1.1–1.5), and 9 years (3.1%, CI 2.7–3.6) in cemented HA compared with the revision rate at 1 month (1.1%, CI 0.9–1.4), 1 year (2.5%, CI 2.1–2.9), and 9 years (5.1%, CI 4.2–6.2) in uncemented HA (). Multivariable Cox regression revealed a lower hazard ratio for revision (HR 0.56, CI 0.47–0.67) in cemented compared with uncemented HA, adjusted for confounders including sex, age, ASA classification, approach, ODEP rating, and previous surgery on the affected hip. These findings were persistent after adjusting also for BMI and smoking in the subset from 2014 to 2016.
Reasons for revision
Dislocation, infection, femoral loosening, and periprosthetic fractures were the most common reason for revision of HA (). Multivariable logistic regression analysis showed that the risk for dislocation was lower in direct lateral approach (HR 0.37, CI 0.24–0.56) and anterolateral approach (HR 0.32, CI 0.16–0.66) compared with posterolateral approach.
Table 2. Reasons for revision of cemented and uncemented hemiarthroplasty
Risk for revision because of infection was statistically significantly higher in patients with previous surgery (HR 4.0, CI 1.3–13). Femoral stem loosening was less often the reason for revision in the cemented HA group compared with the uncemented HA group (HR 0.21, CI 0.12–0.36) and more often in patients aged 60– 80 compared with those aged > 80 years (HR 2.2, CI 1.3–3.8). The risk for revision because of a periprosthetic fracture was less in cemented HA compared with cemented HA (HR 0.07, CI 0.04–0.13).
Discussion
In this study with more than 22,000 hemiarthroplasties for acute femoral neck fracture from the Dutch Arthroplasty Register, we found comparable 9-year mortality rates between cemented and uncemented HA. The 9-year revision rate was lower in cemented HA compared with uncemented HA. Dislocation, infection, femoral stem loosening, and periprosthetic fractures were the most common reasons for revision.
The register data show that in the Netherlands one-third of hemiarthroplasties are performed with an uncemented stem. One of the reasons for choosing an uncemented stem may be the assumed risk for BCIS when using a cemented stem in the fragile patient. We found a difference in early mortality rates in favor of the uncemented group. This might indicate the presence of BCIS, although this cannot be proven from a register study and could also be the result of selection bias. Our 1-month mortality rate was lower in the uncemented HA group. However, the difference was small and the 1-month mortality rate in the cemented HA was comparable to mortality rates of 5–8% previously found in the literature (Costain et al. Citation2011, Olsen et al. Citation2014). From these results, in patients with high risk for BCIS, an uncemented HA may be a good option to improve the earliest outcome. Olsen et al. (Citation2014) showed an incidence of 21%, 5.1%, and 1.7% of BCIS grades 1, 2, and 3 respectively with a 1-month mortality of 9.3%, 35%, and 88% respectively.
BCIS could also influence morbidity due to hypoxia and hypotension leading to a higher mortality during follow-up. An increased mortality in the cemented HA group was, however, not observed compared with the uncemented HA group at 1- and 9-year follow-up. This effect may be due to a higher revision rate in the uncemented group. Our 1-year mortality rate of 20% is comparable to results from the Norwegian and the Swedish Registry (Leonardsson et al. Citation2012, Gjertsen et al. Citation2017). Our 9-year mortality rates of 53% and 56% are in line with the mortality rate of 45% found in the Swedish Registry after 7 years’ follow-up (Jawad et al. Citation2019). A recent study of the Norway Registry showed a higher mortality of about 90% at 9 years’ follow-up (Kristensen et al. Citation2019). This could be due to patient selection, as Kristensen et al. selected only patients of 70 years of age or older, whereas in the current study and in the study of the Swedish Registry no age selection was performed.
Our findings of a lower revision rate after cemented HA, compared with uncemented HA, is supported by other register studies (Gjertsen et al. Citation2012, Jameson et al. Citation2013, Yli-Kyyny et al. Citation2014, Kristensen et al. Citation2019). We have no data on reoperations other than revision procedures in the Dutch register. Other studies showed a reoperation rate of 7–11% at 5–19 years’ follow-up (Parker et al. Citation2010, Viberg et al. Citation2013). These reoperation rates cannot be compared with our revision rates as reoperations do not always include a revision. Surprisingly, ODEP rating > 3A did not influence revision rate in our study. Although individual prosthesis brands could in theory influence revision rate, the data on individual prosthesis brands were not available for this study.
Dislocation, infection, femoral stem loosening, and periprosthetic fractures were the most common reasons for revision. The posterolateral approach was an independent risk factor for dislocation as shown earlier (Leonardsson et al. Citation2012, Rogmark et al. Citation2014, Moerman et al. Citation2018). The posterolateral approach could be considered as surgical approach in HA because functional outcome including pain, walking without mobility aids, and patient-reported outcome measures have been shown to be in favor of the posterolateral approach (Kristensen et al. Citation2017, Hongisto et al. Citation2018). We could not measure the functional outcome. Mukka et al. (Citation2017) did not find any differences in functional outcome between direct lateral and posterolateral approach. We found an uncemented HA as independent risk factor for femoral loosening and periprosthetic fracture as previously shown (Leonardsson et al. Citation2012, Rogmark et al. Citation2014, Moerman et al. Citation2018), which could also be influenced by a lower threshold to revise an uncemented stem when compared with a cemented implant.
The strength of this population-based registry study is the large study population of over 22,000 patients with follow-up of up to 9 years and the inclusion of several potential confounders such as patient, procedure, and prosthesis characteristics, like type of fixation and ODEP rating. A limitation of our study is the observational nature of the data. Therefore, causal relationships cannot be identified. To minimize selection bias, confounders including age, sex, ASA classification, BMI, previous surgery, and smoking habit were added to the multivariable regression analysis. However, potential residual confounding like socioeconomic factors and alcohol consumption could still be present. Severely ill elderly patients could have received internal fixation or non-operative treatment instead of HA. Also, “young old” patients could receive HA rather than THA or internal fixation. Both regimes would lower the mortality after HA. Furthermore, the Dutch Arthroplasty Register does not allow for comparison of individual prosthesis brands. Reoperations like debridement of the wound or Vancouver B1 fracture fixation without prosthesis component replacement are not registered in the Dutch Arthroplasty Register. This may influence the view on fracture rates in our cohort. In addition, closed reduction for a dislocated hip and acetabular erosion as reason for revision are not registered in the LROI database and are therefore not included in this study. Because of these reoperations without revision of the prosthesis, reoperation rate will be higher than revision rate.
An uncemented HA may be considered for the patient with high risk for BCIS with short life expectancy. Regular use of an uncemented stem does not seem to offer benefit to patients. We found no evidence that cemented HA leads to higher mortality in the longer term. In summary, based on the outcome of this study and earlier findings in the literature, in which long-term mortality rates were similar between cemented and uncemented HA for displaced femoral neck fracture and revision rates were lower in cemented HA, we recommend the use of a cemented HA for patients with an acute femoral neck fracture.
Conception of the study: BD, KK, and SB. Data analysis: BD, KK, LS, and SB. Preparation and final approval of the manuscript: BD, KK, LS, and SB.
Acta thanks Jan-Erik Gjertsen and Cecilia Rogmark for help with peer review of this study.
- Costa M L, Griffin X L, Pendleton N, Pearson M, Parsons N. Does cementing the femoral component increase the risk of peri-operative mortality for patients having replacement surgery for a fracture of the neck of femur? Data from the National Hip Fracture Database. J Bone Jt Surg—Ser B 2011; 93(10): 1405–10.
- Costain D J, Whitehouse S L, Pratt N L, Graves S E, Ryan P, Crawford R W. Perioperative mortality after hemiarthroplasty related to fixation method. Acta Orthop 2011; 82(3): 275–81.
- Deangelis J P, Ademi A, Staff I, Lewis C G. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma 2012; 26(3): 135–40.
- Ekman E, Laaksonen I, Isotalo K, Liukas A, Vahlberg T, Mäkelä K. Cementing does not increase the immediate postoperative risk of death after total hip arthroplasty or hemiarthroplasty: a hospital-based study of 10,677 patients. Acta Orthop 2019; 90(3): 270–4.
- Emery R J, Broughton N S, Desai K, Bulstrode C J, Thomas T L. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck: a prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br 1991; 73(2): 322–4.
- Gjertsen J E, Lie S A, Vinje T, Engesaeter L B, Hallan G, Matre K, Furnes O. More re-operations after uncemented than cemented hemiarthroplasty used in the treatment of displaced fractures of the femoral neck: an observational study of 11 116 hemiarthroplasties from a national register. J Bone Joint Surg Br 2012; 94(8): 1113–19.
- Gjertsen J E, Dybvik E, Furnes O, Fevang J M, Havelin L I, Matre K, Engesaeter L B. Improved outcome after hip fracture surgery in Norway: 10-year results from the Norwegian Hip Fracture Register. Acta Orthop 2017; 88(5): 505–11.
- Grammatopoulos G, Wilson H A, Kendrick B J L, Pulford E C, Lippett J, Deakin M, Andrade A J, Kambouroglou G. Hemiarthroplasty using cemented or uncemented stems of proven design: a comparative study. Bone Joint J 2015; 97-B(1): 94–9.
- Hongisto M T, Nuotio M S, Luukkaala T, Väistö O, Pihlajamäki H K. Lateral and posterior approaches in hemiarthroplasty. Scand J Surg 2018; 107(3): 260–8.
- Inngul C, Blomfeldt R, Ponzer S, Enocson A. Cemented versus uncemented arthroplasty in patients with a displaced fracture of the femoral neck: a randomised controlled trial. Bone Joint J 2015; 97-B(11): 1475–80.
- Jameson S S, Jensen C D, Elson D W, Johnson A, Nachtsheim C, Rangan A, Muller S D, Reed M R. Cemented versus cementless hemiarthroplasty for intracapsular neck of femur fracture: a comparison of 60,848 matched patients using national data. Injury 2013; 44(6): 730–4.
- Jawad Z, Nemes S, Bülow E, Rogmark C, Cnudde P. Multi-state analysis of hemi- and total hip arthroplasty for hip fractures in the Swedish population: results from a Swedish national database study of 38,912 patients. Injury 2019; 50(2): 272–7.
- Kristensen T B, Vinje T, Havelin L I, Engesaeter L B, Gjertsen J E. Posterior approach compared to direct lateral approach resulted in better patient-reported outcome after hemiarthroplasty for femoral neck fracture. Acta Orthop 2017; 88(1): 29–34.
- Kristensen T B, Dybvik E, Kristoffersen M, Dale H, Engesaeter L B, Furnes O, Gjertsen J-E. Cemented or uncemented hemiarthroplasty for femoral neck fracture? Data from the Norwegian Hip Fracture Register. Clin Orthop Relat Res 2019; Epub ahead of print.
- Lacny S, Wilson T, Clement F, Roberts D J, Faris P D, Ghali W A, Marshall D A. Kaplan–Meier Survival Analysis Overestimates the Risk of Revision Arthroplasty: A Meta-analysis. Clin Orthop Relat Res 2015; 473(11): 3431–42.
- Langslet E, Frihagen F, Opland V, Madsen J E, Nordsletten L, Figved W. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res 2014; 472(4): 1291–9.
- Leonardsson O, Kärrholm J, Åkesson K, Garellick G, Rogmark C. Higher risk of reoperation for bipolar and uncemented hemiarthroplasty. Acta Orthop 2012; 83(5): 459–66.
- Li T, Zhuang Q, Weng X, Zhou L, Bian Y. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in elderly patients: a meta-analysis. PLoS One 2013; 8(7): e68903.
- Moerman S, Mathijssen N M C, Tuinebreijer W E, Vochteloo A J H, Nelissen R G H H. Hemiarthroplasty and total hip arthroplasty in 30,830 patients with hip fractures: data from the Dutch Arthroplasty Register on revision and risk factors for revision. Acta Orthop 2018; 89(5): 509–14.
- Mukka S, Knutsson B, Majeed A, Sayed-Noor A S. Reduced revision rate and maintained function after hip arthroplasty for femoral neck fractures after transition from posterolateral to direct lateral approach. Acta Orthop 2017; 88(6): 627–33.
- Olsen F, Kotyra M, Houltz E, Ricksten S E. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and effect on outcome. Br J Anaesth 2014; 113(5): 800–6.
- Parker M I, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br 2010; 92(1): 116–22.
- Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J 2016; 98-B(3): 291–7.
- Rogmark C, Fenstad A M, Leonardsson O, Engesaeter L B, Kärrholm J, Furnes O, Garellick G, Gjertsen J E. Posterior approach and uncemented stems increases the risk of reoperation after hemiarthroplasties in elderly hip fracture patients. Acta Orthop 2014; 85(1): 18–25.
- Rutter P D, Panesar S S, Darzi A, Donaldson L J. What is the risk of death or severe harm due to bone cement implantation syndrome among patients undergoing hip hemiarthroplasty for fractured neck of femur? A patient safety surveillance study. BMJ Open 2014; 4(6): e004853.
- Sadr B, Arden G P. A comparison of the stability of Proplast-coated and cemented Thompson prostheses in the treatment of subcapital femoral fractures. Injury 1977; 8(3): 234–7.
- Sonne-Holm S, Walter S, Jensen J S. Moore hemi-arthroplasty with and without bone cement in femoral neck fractures: a clinical controlled trial. Acta Orthop Scand 1982; 53(6): 953–6.
- Van Steenbergen L N, Denissen G A W, Spooren A, Van Rooden S M, Van Oosterhout F J, Morrenhof J W, Nelissen R G H H. More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86(4): 498–505.
- Talsnes O, Vinje T, Gjertsen J E, Dahl O E, Engesaeter L B, Baste V, Pripp A H, Reikerås O. Perioperative mortality in hip fracture patients treated with cemented and uncemented hemiprosthesis: a register study of 11,210 patients. Int Orthop 2013; 37(6): 1135–40.
- Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am 2012; 94(7): 577–83.
- Viberg B, Overgaard S, Lauritsen J, Ovesen O. Lower reoperation rate for cemented hemiarthroplasty than for uncemented hemiarthroplasty and internal fixation following femoral neck fracture: 12- to 19-year follow-up of patients aged 75 years or more. Acta Orthop 2013; 84(3): 254–9.
- Wongworawat M D, Dobbs M B, Gebhardt M C, Gioe T J, Leopold S S, Manner P A, Rimnac C M, Porcher R. Editorial: Estimating survivorship in the face of competing risks. Clin Orthop Relat Res 2015; 473(4): 1173–6.
- Yli-Kyyny T, Sund R, Heinänen M, Venesmaa P, Kröger H. Cemented or uncemented hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthop 2014; 85(1): 49–53.