ABSTRACT
Introduction: Diagnosing eosinophilic asthma is important, because uncontrolled eosinophilic airway inflammation is associated with reduced response to glucocorticoids and increased risk of severe exacerbations.
Areas covered: Currently, the diagnosis of eosinophilic asthma is based on measurements of sputum eosinophils, which is time consuming and requires specific technical expertise. Therefore, biomarkers such as blood eosinophils, FeNO, serum IgE and periostin are being used as surrogates. These biomarkers can be used separately or in combination, and their accuracy to detect sputum eosinophilia depends on cut-off values. The demonstration of eosinophils in sputum is no guarantee for response to treatment with current biological agents targeting Type 2 inflammation, because several molecular pathways may lead to eosinophilic inflammation. In the near future, the results of large trials using ‘omics’ technologies will certainly identify new, more ‘upstream’ biomarkers of eosinophilic inflammation, that will ultimately lead to the ideal targeted treatment for patients with eosinophilic asthma.
Expert commentary: Of currently used surrogate markers to diagnose eosinophilic asthma, blood eosinophils and FeNO have the highest diagnostic accuracy, in particular if used in combination to rule in or rule out eosinophilic asthma. For patients who cannot be classified by these biomarkers alone, the clinical profile may be of help.
1. Introduction
Traditionally, asthma was considered a single disease, but it has now been recognized that it is a heterogeneous mix of subtypes with distinct clinical, physiological, and inflammatory characteristics [Citation1]. In each asthma subtype, unique pathophysiologic mechanisms drive symptoms, airway smooth muscle contraction and mucosal inflammation, that influence the response to conventional therapies [Citation2]. One subtype that has gained increasing attention in recent times is the ‘eosinophilic asthma’ subtype [Citation3]. Patients with this asthma subtype have evidence of uncontrolled eosinophilic inflammation in the airways, which puts them at risk of asthma exacerbations. Patients in whom eosinophilic airway inflammation persists despite high doses of inhaled corticosteroids (ICSs) typically have severe asthma, with poor symptom control, frequent exacerbations, fixed airflow limitation, and oral corticosteroid dependency [Citation3]. For these patients with severe eosinophilic asthma, new biological agents that block eosinophil specific interleukins (IL) such as IL-5 have recently become available [Citation4]. Treatment with these new biologicals results in a marked reduction in exacerbations, a significant improvement in quality of life [Citation5,Citation6] and the ability to taper or even discontinue chronic prednisolone treatment [Citation6]. Diagnosing eosinophilic asthma at an early stage is important, but not without challenges. Here, we will review the current and upcoming approaches for diagnosing eosinophilic asthma and give our personal view on how it can be improved. We will first address the definition of eosinophilic asthma, and why it is important to diagnose this asthma subphenotype. We will then consider the current diagnostic methods and the use of surrogate biomarkers. Next, we will review the value of combined biomarkers and adding clinical patient characteristics. Finally will give our expert opinion including a diagnostic algorithm and conclude with a 5-year view on how diagnosing eosinophilic asthma will evolve.
2. How is eosinophilic asthma defined?
There exists no exact definition of ‘eosinophilic asthma.’ In the literature, term ‘eosinophilic asthma’ is used in different contexts. First, it is used to describe an asthma phenotype that is distinct from non-eosinophilic asthma. Non-eosinophilic asthma was initially described by Douwes and colleagues in 2002 [Citation7]. They defined non-eosinophilic asthma as symptomatic asthma in the absence of eosinophilic airway inflammation. By reviewing the literature, they found that up to 50% of all asthmatics had no evidence of eosinophilic inflammation, and a proportion had evidence of neutrophilic inflammation. This was confirmed by McGrath and colleagues in a longitudinal study of 995 patients with asthma, showing that about 50% of patients had persistently non-eosinophilic asthma, that did not respond well to ICSs [Citation8]. Eosinophilic asthma, defined as symptomatic asthma in the presence of airway eosinophilia with or without neutrophils, is generally associated with a good response to glucocorticosteroids [Citation9], and asthma management guided by eosinophils in sputum rather than according to asthma control measures results in better outcomes [Citation10,Citation11]. Cowan and colleagues found that the proportion of patients with eosinophilic asthma was influenced by the use of ICSs. After withdrawal from ICSs, 67% of patients had eosinophilic asthma, whereas after treatment with ICSs, only 39% had eosinophilic asthma [Citation12]. This and other factors may explain why the eosinophilic phenotype is not consistent over time in some studies [Citation13].
Second, the term eosinophilic asthma is used to describe a subphenotype of severe asthma, that is, asthma that is characterized by active eosinophilic inflammation, which remains uncontrolled and is associated with active eosinophilic inflammation despite the adequate use of high-dose corticosteroid treatment [Citation14]. Wenzel and colleagues first described this ‘eosinophil high’ severe asthma phenotype when performing bronchial biopsies and showed that it was associated with airway remodeling and risk of near-fatal asthma attacks [Citation15]. Others showed that severe eosinophilic asthma is characterized by frequent exacerbations and often requires systemic corticosteroid treatment for control of the disease [Citation14,Citation16,Citation17]. Persistent airway eosinophilia (with or without neutrophils) is the key characteristic of this asthma subphenotype, which appears to be reasonably stable over time [Citation18]. In the present review, we will use the term ‘eosinophilic asthma’ in both senses.
It is important to acknowledge that airway eosinophilia and/or blood eosinophilia are not exclusively related to asthma. Tissue eosinophilia and peripheral blood eosinophilia are also characteristic for other hypereosinophilic conditions including eosinophilic granulomatosis with polyangiitis allergic bronchopulmonary aspergillosis, eosinophilic pneumonia, hypereosinophilic syndrome (HES), and other rare conditions [Citation19,Citation20]. Typical for eosinophilic asthma is the presence of elevated numbers of eosinophils in airway tissue, in the absence of vasculitis, fungus infection, pulmonary infiltrates, bone marrow abnormalities, and organ involvement other than airway mucosa [Citation21]. These other hypereosinophilic conditions will not be addressed in this review.
3. Why should we diagnose eosinophilic asthma?
Diagnosing eosinophilic asthma is important, both in primary practice and secondary or tertiary care. For the general practitioner, it is important to know whether in a patient with symptoms suggestive of asthma treatment with ICSs should be initiated or not. Patients with symptoms and evidence of eosinophilic inflammation are likely to respond to ICSs [Citation9], but in the absence of airway eosinophilia, patients should not be treated with ever increasing doses of corticosteroids. Also for secondary and tertiary care physicians who deal with patients with difficult-to-treat asthma, it is important to know whether the patient has airway eosinophilia. Those with persistent eosinophilia despite being treated with inhaled or oral corticosteroids are at risk of severe exacerbations and airway remodeling and should therefore be monitored more intensively [Citation11]. In all settings, it is important to use all available resources and information to better predict whether a patient has eosinophilic asthma.
4. Current methods for diagnosing eosinophilic asthma
The diagnosis of eosinophilic asthma relies on the demonstration of eosinophilic inflammation in the airways of patients with asthma, but there is still no standard diagnostic test. Several methods are being used to identify airway eosinophilia in the airways including bronchial biopsies, induced sputum, blood, and exhaled breath. Traditionally, airway biopsies or bronchoalveolar lavage is considered as the gold standard for assessing airway inflammation [Citation15] but this method is too invasive for routine clinical use. Therefore, there has been great interest in methods to assess airway inflammation noninvasively and in a convenient and inexpensive way. The most common and best validated method to diagnose eosinophilic asthma is detection of eosinophils in induced sputum [Citation22]. A recently published meta-analysis on the diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma found that most (88%) of the research on this subject was done with sputum eosinophils as reference standard [Citation23]. Also in the present review, we will use sputum eosinophilia as reference for eosinophilic airway inflammation. Sputum induction is not without risk in patients with severe asthma nor is it always successful [Citation24]. Processing requires time and expertise and results are not readily available. This has led to surrogates to detect airway eosinophilia including blood eosinophils, the fraction of exhaled nitric oxide (FeNO), serum periostin, and serum immunoglobulin E (IgE) [Citation25]. Most of these markers have proven their use in clinical setting. However, the accuracy of these markers is far from ideal [Citation23].
5. Use of surrogate markers for diagnosing eosinophilic asthma
5.1. Blood eosinophils
Complete blood cell counts with differential can be performed at a lower cost and greater accessibility than induced sputum. Therefore, eosinophil counts in peripheral blood have become popular in identifying asthma patients with airway eosinophilia, in particular in studies with anti-IL-5 therapies [Citation5]. However, although there exists a significant association between eosinophils in blood and in sputum, the use of blood eosinophils to identify sputum eosinophilia is still debated because of the relatively high false-negative and false-positive rates [Citation26]. This was illustrated in the 328 patients of the severe asthma research programme (SARP) showing that the accuracy of blood eosinophils to predict sputum eosinophilia was low, leading to considerable misclassification of patients with eosinophilic or non-eosinophilic asthma. This low accuracy might be due to the high variability of blood eosinophil counts in patients with asthma, both in the short (24 h) and in the long (1 year) run [Citation13,Citation27]. So, merely for the diagnosis of ‘eosinophilic asthma,’ one single measurement of blood eosinophils does not seem to be of great value. The most important role for blood eosinophils is probably its role in identifying patients who are likely to respond to treatment with the new biological agents against Type 2 inflammation [Citation25]. However, they seem to be less suitable to monitor treatment response, given the fact that biologicals such as anti-IL-5 strongly reduce blood eosinophils but affect tissue eosinophils to a much lesser extent [Citation28]. This may also explain why anti-IL-5 treatment can effectively reduce exacerbations and systemic corticosteroid requirement but has only little effect on the forced expiratory volume in 1 s (FEV1) [Citation16].
5.2. FeNO
FeNO is being regarded as one of the most practical noninvasive tests to identify eosinophils in sputum from patients with asthma, because it is easy, quick, cheap, and generally available. Still, there are many unresolved questions. After the first observation that FeNO was increased in patients with asthma [Citation29], many studies have suggested that this biomarker could be used as a test to diagnose or monitoring asthma in clinical practice [Citation30]. In particular, for identifying eosinophilic airway inflammation, FeNO was put forward as an ideal noninvasive biomarker [Citation31]. Many studies have shown a positive relationship between FeNO and the number of percentage sputum eosinophils [Citation23,Citation32,Citation33], and one study showed that FeNO measurement could identify the subgroup of patients with severe eosinophilic asthma [Citation34]. However, in the SARP study, a high rate of misdiagnosis was found when using FeNO for diagnosing eosinophilic asthma based on sputum eosinophils ≥2% [Citation26]. One possible explanation for this discrepancy might be that FeNO values in severe asthma can be confounded by many factors [Citation30]. But another, more plausible explanation is that FeNO and blood eosinophils reflect different pathways of Type-2-mediated inflammation. This is illustrated by two trials in which a discrepancy was observed between the treatment response as measured by eosinophils or FeNO. In one trial, mepolizumab, a monoclonal antibody against IL-5 given to patients with eosinophilic asthma, significantly reduced blood and sputum eosinophils but had no effect on FeNO levels [Citation14]. In another trial, lebrikizumab, an anti-IL-13 monoclonal antibody, had no effect on eosinophils but was associated with a significant reduction in FeNO levels and improvement in lung function, in particular in patients with high periostin levels [Citation35]. Apparently, the molecular pathways leading to increased FeNO levels differ from those regulating eosinophil recruitment and activation. Increased FeNO seems to be primarily related to pathways involved in Th2-mediated asthma, whereas blood eosinophils may relate more to type 2 innate lymphoid cell (ILC2)-mediated (severe) asthma [Citation36,Citation37].
These different pathways may also explain why sputum eosinophils can be used to titrate treatment with ICSs in asthma patients with frequent exacerbations [Citation10,Citation11], whereas FeNO values are not adequate for this purpose [Citation38]. Inhaled corticosteroids are known to directly affect inducible nitric oxide synthase, irrespective of their effect on eosinophils, which is very important when interpreting FeNO values [Citation39]. FeNO values are high in patients with allergies, irrespective of blood eosinophils counts, whilst FeNO levels are reduced in asthma patients who smoke or have consumed alcohol [Citation30]. Even age and gender are known to affect FeNO levels, which reduces its value as a biomarker for predicting eosinophilic airway inflammation. Up till now, there is no consensus how and where to use FeNO in clinical practice. In primary care, FeNO might be used as a screening tool to exclude Type 2 inflammation in patients with symptoms of cough and wheeze [Citation40]. Alternatively, for patients with severe asthma who are candidates for the new expensive biologicals directed against Type 2 inflammation, FeNO could be suitable to exclude nonadherence with ICS treatment as the cause of eosinophilia in blood or sputum [Citation41].
5.3. Periostin
Periostin is a relatively new kid on the block for detecting eosinophilic airway inflammation. Several reports have shown significant correlations between periostin in serum and eosinophils in sputum [Citation42,Citation43]. Woodruff et al. were the first to show upregulated periostin gene expression in bronchoalveolar lavage from patients with asthma as compared to normal control subjects, which was associated with increased concentrations of IL-4, IL-5, and IL-13 [Citation44]. These patients also had higher eosinophil counts in lavage fluid, suggesting that increased periostin levels might reflect a Th2-high profile. This fits well with the observed correlation between periostin and specific IgE in sputum [Citation45]. After this initial report, several investigators confirmed the association between periostin and sputum eosinophils, even proposed serum periostin as a biomarker for airway eosinophilia [Citation42]. However, subsequent studies showed that the strength of the correlation between periostin and sputum eosinophilia, although significant, was relatively weak, and that neither serum nor sputum periostin was suitable for use as a surrogate marker of airway eosinophilia [Citation43]. Wagener et al. showed that serum periostin, when compared to blood eosinophils and FeNO, showed the lowest accuracy for distinguishing eosinophilic (sputum eosinophils ≥3%) from non-eosinophilic inflammation in two independent cohorts of patients with asthma [Citation46].
Although the diagnostic accuracy to predict eosinophilic airway inflammation is relatively modest, periostin may have clinical relevance in predicting the response to some of the new biologicals against Type 2 inflammation. This was suggested by the observation that increased serum periostin levels were found in patients with a greater response to therapy with lebrikizumab, a monoclonal antibody against IL-13. In patients with low periostin levels, the response was minimal, suggesting that periostin might identify patients with an IL-13-dependent type 2 inflammation who are likely to benefit from anti-IL-13 therapy [Citation35] although this has yet to be confirmed in prospective studies.
5.4. Total IgE
IgE has an essential role in allergic asthma [Citation47]. Allergic patients produce IgE antibodies specific for antigens such as house dust mite and pollens, which bind to IgE-specific receptors on mast cells and basophils. Cross-linking of IgE molecules causes the release of mediators (histamine, arachidonic acid metabolites) and cytokines (tumor necrosis factor alpha, IL-4, and IL-5) which are responsible for the immediate and late-phase allergic response, and the associated influx of eosinophils in the airway [Citation48]. Several studies have found an association between serum IgE levels and airway eosinophilia in asthma, and treatment with anti-IgE has been shown to be associated with a significant reduction in tissue eosinophils [Citation49]. However, despite these findings, the use of IgE as a biomarker for eosinophilic inflammation is not recommendable. A recent meta-analysis by Korevaar and colleagues showed low accuracy for this biomarker to detect sputum eosinophilia, and inferiority as compared to FeNO [Citation23]. When comparing blood eosinophils with IgE, the results were not conclusive. Remarkably, Westerhof and colleagues, when comparing atopic and non-atopic patients with asthma, found poorer accuracy of total IgE for detecting sputum eosinophilia in atopic patients, suggesting that in these patients IgE has no value in distinguishing between those with or without sputum eosinophilia [Citation50]. Thus, of all currently available biomarkers to detect eosinophilic asthma, IgE seems to be the least useful. This does however not exclude that IgE can be used to identify patients who will likely benefit form anti-IgE therapy, nor that anti-IgE can have a beneficial effect in subgroups of patients with eosinophilic asthma [Citation51].
6. Combinations of blood eosinophils, FeNO, periostin, and IgE
By recognizing that eosinophilic asthma has a complex underlying pathogenesis involving different molecular pathways, it seems illogical to expect to find one perfect biomarker for this phenotype. However, since different biomarkers may represent different pathways of type 2 airway inflammation [Citation23,Citation52], combinations of two or more biomarkers could increase sensitivity and specificity for detection of eosinophilic airway inflammation.
Several clinical trials investigating the effects of monoclonal antibodies against key cytokines of Type 2 inflammation have already taken such approach. For example, the DREAM study evaluating the effect of anti-IL-5 therapy with mepolizumab used FeNO ≥50 parts per billions (ppb) or blood eosinophils ≥0.3 × 109/L to select patients with eosinophilic asthma [Citation16]. A more complex method was used in another trial with and IL-5R-alpha [Citation53]. Here, the ELEN-index was used for stratifying the eosinophilic status of the patient. This index used the absolute ratio between eosinophils and lymphocytes (EL) and the absolute ratio between eosinophils and neutrophils (EN) as a predictor for the presence of sputum eosinophilia [Citation54]. A study with anti-IL-13 used a combination of total serum IgE level and peripheral-blood eosinophil count [Citation35]. Both biomarkers had to be high enough in order to classify the subject as ‘type 2 high.’ Yet, another study investigating whether periostin correlated with type 2 immunity [Citation55] combined blood and sputum eosinophils, FeNO and IgE and created the ‘type 2 immunity composite score.’ Apparently, the authors of all above-mentioned studies assumed that a combination of several biomarkers provided more information than one single biomarker.
Only few studies have specifically looked at the accuracy of a combination of two or more biomarkers to detect eosinophilic airway inflammation [Citation26,Citation46,Citation50]. Unfortunately, the results of these studies are not fully conclusive. One study did not find an improvement in accuracy when combining blood eosinophils, FeNO, and periostin as compared to one of the single biomarkers [Citation46], whereas another study did find a small enhancement in accuracy when combining FeNO and blood eosinophils [Citation50]. Adding IgE to these models did not lead to any improvement of the results. Thus, theoretically the use of a combination of biomarkers could improve the diagnosis of eosinophilic asthma, but there are currently not enough data available to confirm this. Hopefully, the results of the Medical Research Council United Kingdom Refractory Asthma Stratification Programme (RASP-UK) will shed more light on this issue. The RASP-UK Consortium is a large scale research project that aims to explore novel biomarker stratification strategies in severe asthma to improve clinical management and target treatments effectively in patients with severe asthma. This study will examine a novel composite biomarker strategy including FeNO, blood eosinophils, and serum periostin as biomarkers for diagnosing Type 2 inflammation [Citation56].
Up till now, there is a general feeling and some evidence that combining different biomarkers, in particular FeNO and blood eosinophils, might improve the accuracy to diagnose eosinophilic asthma. The role for periostin is unclear and with some certainty it can be concluded that IgE does not provide added value to detect active eosinophilic airway inflammation. However, this does not exclude that using single or combined biomarkers might be helpful to select the right asthma patients for specific targeted treatments.
7. Cutoff points for blood eosinophils, FeNO, periostin, and IgE
One of the problems in defining eosinophilic asthma is lack of consensus regarding biomarker cutoff values. This lack of consensus is reflected in research papers where several different values are being used, even for sputum eosinophilia as the reference standard. In some studies, sputum eosinophilia is defined as ≥2% eosinophils, which is based on the upper limit of the normal range in the healthy population [Citation57], but other studies use higher levels, up to ≥3%. Also values for the surrogate biomarkers vary widely. The cutoff values for blood eosinophils differ between 0.22 and 0.32 × 109/L, for FeNO levels between 10 and 41 ppb, and for IgE 72 and 900 IU/mL [Citation23]. For periostin, a value of 25–50 ng/mL or the median of the study population is mostly used [Citation35,Citation42,Citation58]. These cutoff values are based on the optimal combination of sensitivity and specificity. However, for clinical use of these biomarkers, it might be better to use more than one threshold, so that one can either choose for high specificity OR high sensitivity instead of a suboptimal combination of both. These thresholds can thus be used to rule out (high sensitivity) or rule in (high specificity) eosinophilic inflammation in an asthmatic patient [Citation23].
This principle of using different thresholds was applied in an elegant study in patients with severe asthma [Citation59]. Sputum eosinophils and blood eosinophils were collected and different cutoff points for blood eosinophils (0.15/0.3/0.45 × 109/L) were used to predict ≥2% sputum eosinophilia. The results showed that changing the threshold from 0.3 to 0.45 × 109/L improved the specificity from 84.4% to 97%. From these results, the authors concluded that using a cutoff of 0.45 × 109/L or higher for blood eosinophilia could safely predict airway eosinophilia. Also other studies reported that a blood eosinophil threshold ≥0.4 × 109/L could predict sputum eosinophilia with high probability [Citation8,Citation50]. Westerhof et al. not only found a specificity of 95% for blood eosinophils ≥0.41 × 109/L to rule in, but also a sensitivity of 96% for ≤0.09 × 109/L eosinophils to rule out sputum eosinophilia [Citation50].
This value is in accordance with values used in trials with the anti-IL-5 monoclonal antibody reslizumab, in which the authors have chosen a blood eosinophil threshold of ≥0.4 × 109/L to select patients with a high likelihood of having active eosinophilic airway inflammation [Citation60,Citation61]. This choice was based on a subgroup analysis of a phase 3 trial with this agent, showing that patients with baseline eosinophils <0.4 × 109/L, exhibited no significant improvement in FEV1 after reslizumab treatment compared with placebo [Citation62]. In the subgroup with eosinophils ≥0.4 × 109/L eosinophils, however, treatment with reslizumab was associated with much larger improvements in FEV1, asthma symptoms, rescue medication use and forced vital capacity (FVC) compared with placebo. These findings contrast with those for mepolizumab, another anti-IL-5 monoclonal antibody. In three independent large trials, it was found that a threshold of blood eosinophils ≥0.15 × 109/L predicted treatment response to mepolizumab, in that it reduced the rate of exacerbations and the dose of chronic oral glucocorticoids [Citation5,Citation6,Citation16]. Blood eosinophils 0.15 × 109/L correctly predicted the response sputum eosinophilia ≥3% with a sensitivity of 85% and specificity of 75%, whilst increasing the threshold to 0.3 × 109/L had minimal influence on sensitivity, but decreased specificity substantially [Citation63]. Remarkably, sputum eosinophils did not predict treatment response to mepolizumab, but blood eosinophils counts did [Citation64]. This latter finding suggests that blood eosinophilia, rather than sputum eosinophilia is the ‘gold standard’ for patients to be eligible for mepolizumab treatment. For treatment with reslizumab, another anti-IL-5 monoclonal antibody, the threshold for blood eosinophils was higher, ≥0.4 × 109/L. This difference in thresholds might be explained by the relatively large proportion of patients who were on systemic corticosteroid treatment in the mepolizumab studies. Yet another value for blood eosinophils (0.3 × 109/L was found to be optimal for the selection of patients likely to respond to lebrikizumab, the monoclonal antibody against IL-4R-alpha (dupilumab),and IL-5R-alpha (benralizumab) [Citation53,Citation58,Citation65]. Taken together, the threshold for blood eosinophils to be used for treatment with Type 2 biologicals is variable and depends on medication used and the biological of choice.
Threshold values with high sensitivity or high specificity to detect elevated sputum eosinophils have also been reported for FeNO [Citation8,Citation34,Citation42,Citation50,Citation66–Citation68]. However, these thresholds vary widely depending on the technique that is being used, and the population under study. In steroid naïve asthma patients the presence of sputum eosinophils ≥3% was ruled in at a FeNO level of >41 ppb [Citation68], and ruled out at a levels of ≤21 ppb (sensitivity 97%) [Citation67]. Among ICS users, the sensitivity was considerably lower for the rule-out threshold (sensitivity 81%). Another study in corticosteroid-treated asthma patients showed that sputum eosinophils ≥3% could be ruled out if FeNO levels were ≤12.2 ppb and ruled in if FeNO levels were ≥64.5 ppb [Citation50]. A similar high threshold (>73 ppb) for FeNO to rule in eosinophilic inflammation in patients on corticosteroid treatment was seen when bronchial biopsies were used as the reference standard for eosinophilic airway inflammation [Citation34]. Taken together, in patients with mild asthma FeNO levels of around 40 ppb or higher are associated with airway eosinophilia, whereas in steroid-treated asthma patients higher levels of FeNO (>65–70 ppb) are indicative of persistent airway eosinophilia.
Only one study specifically looked at thresholds for IgE to detect sputum eosinophilia [Citation50]. This study showed that the threshold for total IgE to rule out sputum eosinophilia ≥3% was <13.5 IU/L and to rule in eosinophilia was ≥764 IU/L (sensitivity ≥ 95%). Clearly, these widely spaced thresholds of total IgE do not seem to have much value in clinical practice.
To our knowledge, there are no studies that have looked at thresholds for serum periostin to rule out or rule in airway eosinophilia.
8. Repeated measurements of biomarkers
Although studies have shown that the eosinophilic asthma phenotype is reasonably stable over time [Citation18,Citation69], there is no doubt that sputum inflammatory profiles and their associated biomarkers vary under the influence of many factors, including change in medications, adherence to treatment, exacerbations, pollution, and allergens’ exposure. It is therefore rational to assume that one-off clinic readings may not be the best method of utilizing biomarkers, and that repeated measures are required to obtain reliable phenotyping data on subjects with asthma.
With respect to blood eosinophil measurements, Katz and colleagues showed that using an average of multiple measurements of blood eosinophils spread over a prolonged period of time only marginally increased the sensitivity to detect sputum eosinophils ≥3% [Citation64,Citation70]. Repeated measurements of FeNO, however, do seem to increase the diagnostic accuracy for detecting sputum eosinophilia. Nanda and colleagues showed that an average FeNO measurement over a moving period of 5–7 days gave a better insight into the level of sputum and blood eosinophils than a single measurement [Citation71]. Thus, repeated measurements of blood eosinophils for diagnosis of eosinophilic asthma do not seem to provide additive value, whereas serial measurement of FeNO may do.
9. Added value of clinical features to improve the diagnosis of eosinophilic asthma
In clinical practice, high or low levels of blood eosinophils and FeNO may be used for ruling in or ruling out eosinophilic asthma, but often the levels of these biomarkers are inconclusive. In these patients, the clinical profile may have added value. A recent study looking at the typical clinical profile of adult patients with eosinophilic asthma found that patients with this phenotype differed from patients with non-eosinophilic asthma with respect to a number of distinctive clinical features [Citation72]. As compared to non-eosinophilic asthma patients, those with the eosinophilic phenotype had more often adult-onset asthma, were more often male, and had more often chronic rhinosinusitis with nasal polyposis. In addition, they showed more often persistent airflow limitation and airtrapping, which is typically associated with dyspnea on exertion. Other studies looking at patients with eosinophilic asthma found similar clinical characteristics [Citation18]. So, this typical set of clinical parameters seems point toward an asthma phenotype that is likely to have active eosinophilic airway inflammation. This implies that clinical pattern recognition by the treating physician could improve the diagnosis eosinophilic asthma if combined with biomarkers in blood or serum. Currently, there are no published studies that have examined the diagnostic accuracy of combined clinical characteristics and biomarkers for diagnosing eosinophilic asthma, but it would be worth considering.
10. Future options to improve the diagnosis of eosinophilic asthma
10.1. Volatile organic compounds and other ‘omics’ techniques
A promising new technique for assessing airway inflammation involves the use of volatile organic compound (VOC) patterns in exhaled breath [Citation73]. Exhaled breath contains a complex gas mixture of several thousands of individual VOCs, which are derived from systemic and local metabolic, inflammatory, and oxidative processes. Individual molecular compounds in a VOC mixture can be measured by gas chromatography–mass spectrometry (GC–MS), whereas patterns of different VOCs can be captured by an ‘electronic noses’ (breathomics) [Citation74]. Until now, no single compound has been identified as disease specific, presumably due to overlap of compounds between diseases. However, various research groups demonstrated that VOCs profiles could accurately distinguish patients with a pulmonary disease from healthy controls. The current hypothesis is that pulmonary diseases are characterized by a disease-specific breath-print, as distinct profiles were found in patients with different lung diseases [Citation75]. Exhaled breath has been used in the detection of lung diseases such as lung cancer, tuberculosis, and cystic fibrosis [Citation74], but its most promising application lies in stratification of inflammatory airways disease into different subphenotypes [Citation76]. In asthma, specific exhaled VOCs profiles defined by GC–MS appear to be associated with the eosinophilic phenotype and are associated with disease activity [Citation76]. The distinctiveness of breath prints for inflammatory subtypes was also confirmed in a study with an electronic nose [Citation77]. In accordance, steroid responsiveness in patients could be predicted by the electronic nose with even greater accuracy than sputum eosinophils or FeNO [Citation78].
There are still some hurdles which need to be taken in order to make prints breath applicable in the clinic [Citation74]. But large multicenter trials such as U-BIOPRED study [Citation79] validating this diagnostic ‘biomarker’ are currently underway. U-BIOPRED focusses on several new ‘omics’ techniques such as gene expression (transcriptomics), proteins (proteomics), lipids (lipidomics), and metabolites (metabolomics) in the lungs, blood, and urine [Citation79]. Results of this large study are expected to reveal more accurate biomarkers for identification of all existing asthma phenotypes and endotypes.
10.2. Multiple molecular pathways leading to eosinophilic airway inflammation
Until a few years ago, airway eosinophilia was considered the key characteristic feature of Th2-mediated inflammation. This concept has been challenged by the observation that blocking eosinophil recruitment and activation by a monoclonal antibody against IL-5 had no effect on the Th2-related symptoms, in particular, on the early and late asthmatic response to inhaled allergens [Citation80]. The most likely explanation that has been put forward recently is that multiple mechanisms involving multiple molecular pathways can lead to an eosinophilic inflammatory response [Citation81].
In allergic eosinophilic asthma, Th2 cells are driving the pathobiology of the disease, but there is accumulating evidence that in adult-onset nonallergic eosinophilic asthma, ILC2s may play a more prominent role [Citation36]. Air pollutants, microbes, and glycolipids induce the release of epithelium-derived cytokines that activate ILC2s, which are then able to produce high amounts of IL-5 and IL-13 leading to eosinophilia [Citation82,Citation83]. ILC2s are present in greater numbers in sputum and blood of patients with severe eosinophilic asthma compared to mild allergic asthmatics and produce high levels of IL-5 and IL-13 in sputum [Citation84]. Thus, ILC2s and its cytokines can promote the persistence of airway eosinophilia independent of allergen exposure, which explains the lack of response of anti-IL-5 in the allergen challenge model, and the presence of eosinophilic inflammation in nonallergic asthma [Citation36]. Because of the close association between ILC2s in peripheral blood and sputum eosinophils, ILC2s have even been proposed as novel biomarkers for eosinophilic asthma [Citation85]. It appeared that the diagnostic accuracy of ILC2s, expressed in percentage of lymphocytes (%ILC), was better than that of blood eosinophils and FeNO. Using 0.076% ILC2 as a cutoff value, eosinophilic airway inflammation was detected with a sensitivity of 67.7% and a specificity of 95.3%. With these numbers, %ILC2s can be a promising biomarker to be used in the clinic to rule in eosinophilic asthma and identify patients for anti-IL-5 therapy.
The finding of at least two different pathways with different drivers of eosinophilic inflammation may explain why markers such as blood eosinophilia, FeNO, periostin, and IgE have different predictive value for sputum eosinophilia in several studies. Therefore, it seems sensible to look for a biomarker that is representative of multiple Type 2 pathways. Airway epithelial cells constitute the first physical, chemical, and immunological barrier for all type 2 immune cell stimuli including allergens, pollutants, viruses, and fungi [Citation86]. There is now increasing evidence that in asthma, a dysregulated epithelial responses or barrier function could be the driver of the disease process. Potential markers of such epithelial cell dysregulation are IL-25, IL-33, and thymic stromal lymphopoietin (TSLP), known as epithelial alarmins. These cytokines initiate pathways resulting in the type 2 inflammatory cascade and eosinophilia [Citation86]. TSLP, in particular, has been proposed to play a key role in eosinophilic asthma. This upstream cytokine has convincingly been shown to be driving classical allergen-induced asthma and eosinophil influx into the airways [Citation87] but is also an important component of the innate type 2 immune system. TSLP plays an important role in the inflammation seen in patients with nasal polyposis [Citation88] and is supposed to contribute to the pathogenesis of aspirin induced asthma [Citation89]. It would be interesting to see if serum TSLP or another upstream molecule could be used as a biomarker of the multiple pathways that lead to eosinophilic airway inflammation in allergic, nonallergic, and aspirin-induced asthma. However, the question remains whether a biomarker for diagnosing eosinophilic airway inflammation ‘per se’ would be the best predictor of response to targeted therapies, when compared to specific pathway-related biomarkers like periostin for anti-IL-13 or IgE or for anti-IgE therapy.
10.3. Genetic markers, cell-surface markers, and microbiome
Genetic markers, in particular single-nucleotide polymorphisms (SNPs), have been found to control epithelial barrier function (e.g. filaggrin) and control the production or responsiveness to epithelial cytokines, such as TSLP and IL 1 receptor-like 1 (which encodes the receptor for IL-33). These SNPs are involved in biological pathways leading to eosinophilic airway inflammation and might thus be considered as indirect biomarkers [Citation90].
Surface markers of eosinophils have also been proposed as biomarkers to distinguish between different eosinophilic conditions. For example, Siglec-8 correlates with blood eosinophils and has been identified as a marker for HESs [Citation91]. This protein might even become a target for new therapies as this protein plays a role in apoptosis of eosinophils [Citation92]. Whether this surface marker is useful as biomarker or therapeutic target in eosinophilic asthma needs to be further explored.
Another interesting approach to diagnose eosinophilic asthma may be the microbiome. Recently, it has been shown that the dysbiosis of the lower airway microbiome correlates with clinical characteristics of chronic persistent asthma, including airflow obstruction, use of corticosteroid medications, and presence of airway eosinophilia [Citation93,Citation94]. This suggests that the composition of the airway microbiome may be important in severe eosinophilic asthma, and as such might become a unique biomarker in the future.
11. Expert commentary
The diagnosis of eosinophilic asthma is currently based on sputum eosinophils as the ‘gold standard.’ However, the measurement of sputum eosinophils is time consuming and requires specific technical expertise. Therefore, biomarkers such as blood eosinophils, FeNO, serum IgE, and periostin are being used as surrogates. Blood eosinophils and FeNO have the highest diagnostic accuracy, but to reduce the likelihood of misclassification as much as possible, these biomarkers should be used in the most effective manner. First, repeated measures of biomarkers, in particular FeNO, are likely to reduce misclassification, and combined measures of blood eosinophils and FeNO have been demonstrated to improve diagnostic accuracy. Second, these biomarkers should primarily be used to rule in or rule out eosinophilic asthma by using high and low cutoff values, respectively (). For patients who cannot be classified by these biomarkers alone, the clinical profile may be of help. If the patient exhibits typical features such as adult-onset asthma, chronic rhinosinusitis with nasal polyposis, persistent airflow limitation, and air trapping, the probability will be high that the patient has indeed eosinophilic asthma. If both biomarkers and clinical profile are inconclusive, sputum induction will be necessary to confirm the diagnosis. However, a diagnosis of eosinophilic asthma is no guarantee for response to treatment with biologicals targeting Type 2 inflammation, because several molecular pathways may lead to eosinophilic inflammation. For this purpose, it should be recommended to evaluate the biomarker appropriate for the specific treatment of choice ().
Figure 1. Algorithm to diagnose and treat eosinophilic asthma.
*reference values can be found in the text. ICS: inhaled corticosteroids; FeNO: fraction of exhaled nitric oxide; ppb: parts per billion; GINA: global initiative for asthma; OCS: oral corticosteroids; IgE: immunoglobuline E; IL: interleukin; Rα: receptor alpha.
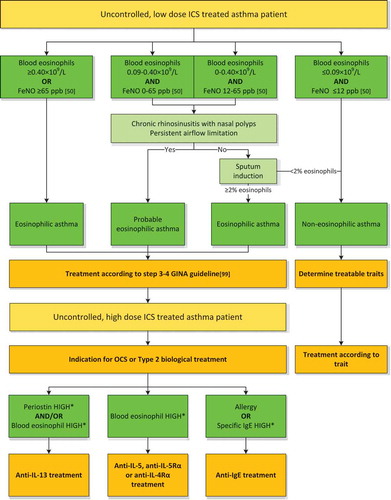
Blood eosinophils, periostin or IgE measurements could be used to select patients for treatment with anti-IL-5, anti-IL-5R-alpha, anti-IL-4R-alpha, anti-IL-13, and anti-IgE, respectively. When the biomarker in question is labeled as ‘high,’ the diagnosis of eosinophilic asthma may not be certain but there will be a chance of success for the chosen treatment, which may be more relevant for the patient.
12. Five-year view
Currently, we are at the tipping point concerning asthma diagnosis. In the next few years, results of large multicenter studies as the IMI-EU sponsored U-BIOPRED study will certainly lead to the discovery and development of new biomarkers for eosinophilic asthma. In the most ideal situation, even a new gold standard will be set. This could be one particular biomarker representing the entire complex Type 2 pathway or a well-defined combination of various biomarkers representing multiple pathways conjointly.
However, the biggest change for asthma will not lie in the area of biomarkers. We believe that the diagnosis of eosinophilic asthma will become less important, but the focus will be on the diagnosis of eosinophilic airway inflammation as a treatable option. The current debate in the asthma and chronic obstructive airways disease (COPD) field emphasizes on changing the current strategy of traditional diagnoses to acknowledging the complexity of chronic airway diseases. Instead of clear-cut disease definitions, the focus is shifting toward features of chronic airway diseases that are amenable to specific therapies. This concept is not entirely new but was the hall mark of the Dutch Hypothesis in the sixties and has also been put forward some years ago by the Leicester asthma research group as the ‘A to E of airway disease’ [Citation95,Citation96]. With the introduction of ‘treatable traits,’ important steps are being made as we speak. Agusti and colleagues [Citation40] have reinforced this fundamental concept and strongly encourage the use of ‘label-free patients.’ This in order to work toward personalized medicine and thereby improving patient’s outcome [Citation97]. These traits can be pulmonary (e.g. airflow limitation, eosinophilic inflammation), extrapulmonary (e.g. obesity, rhino-sinusitis), or behavior/lifestyle risk factors (e.g. smoking, adherence). By defining which treatable traits are present in a patient with airways disease, whether it is asthma or COPD, a tailor-made treatment plan can be used to manage the patient. This approach is still in early stages, and the currently suggested treatable traits will certainly be adapted in the coming years. Nonetheless, there is a high probability that eosinophilic inflammation will be one of the key traits to be targeted. Diagnosing eosinophilic inflammation might be done with the suggested use of biomarkers in this review, and hopefully new biomarkers will be identified and available for daily use in the near future. But most of all, it will be interesting to see if within the next 5 years physicians and researchers are ‘brave enough’ to take the next steps in order to let go of the past and embrace the new era that is in front of us [Citation98].
Key issues
Diagnosing eosinophilic asthma is important, because uncontrolled eosinophilic airway inflammation is associated with reduced response to glucocorticoids and increased risk of severe exacerbations.
The diagnosis of eosinophilic asthma is currently based on the demonstration of elevated numbers of eosinophils in induced sputum, which is a time consuming procedure that requires specific technical expertise.
Surrogate biomarkers of eosinophilic asthma include blood eosinophils, FeNO, serum IgE and periostin, of which blood eosinophils and FeNO as single biomarkers have the highest diagnostic accuracy.
The diagnostic accuracy for detecting eosinophilic asthma can be improved by using high and low cutoff values to rule-in or rule-out eosinophilic airway inflammation. Further improvement might be obtained by combining FeNO and blood eosinophils or combining biomarkers with typical clinical characteristics.
The demonstration of eosinophils in sputum is no guarantee for response to treatment with current biological agents targeting Type 2 inflammation, because several molecular pathways lead to eosinophilic inflammation.
Blood eosinophils, periostin and IgE have proven their use for identifying candidates for treatment with Type 2 biological agents.
Results of large trials using ‘omics’ technologies are about to identify new biomarkers of eosinophilic inflammation, that will ultimately lead to the ideal targeted treatment for patients with eosinophilic asthma.
In the next 5 years our approach to diagnosing and treating airways diseases will change. The focus will shift from disease labeling towards identifying ‘treatable traits’ of which eosinophilic airway inflammation will certainly be amongst the most important.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Additional information
Funding
References
- Martinez FD, Vercelli D. Asthma. Lancet. 2013;382(9901):1360–1372.
- Gauthier M, Ray A, Wenzel SE. Evolving concepts of asthma. Am J Respir Crit Care Med. 2015;192(6):660–668.
- De Groot JC, Ten Brinke A, Bel EHD. Management of the patient with eosinophilic asthma: a new era begins. ERJ Open Res. 2015;1(1):00024–02015.
- Hilvering B, Xue LZ, Pavord ID. Evidence for the efficacy and safety of anti-interleukin-5 treatment in the management of refractory eosinophilic asthma. Ther Adv Respir Dis. 2015;9(4):135–145.
- Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. New Engl J Med. 2014;371(13):1198–1207.
- Bel EH, Wenzel SE, Thompson PJ, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. New Engl J Med. 2014;371(13):1189–1197.
- Douwes J, Gibson P, Pekkanen J, et al. Non-eosinophilic asthma: importance and possible mechanisms. Thorax. 2002;57(7):643–648.
- McGrath KW, Icitovic N, Boushey HA, et al. A large subgroup of mild-to-moderate asthma is persistently noneosinophilic. Am J Respir Crit Care Med. 2012;185(6):612–619.
- Hargreave FE. Induced sputum and response to glucocorticoids. J Allergy Clin Immunol. 1998;102(5):S102–105.
- Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet. 2002;360(9347):1715–1721.
- Jayaram L, Pizzichini MM, Cook RJ, et al. Determining asthma treatment by monitoring sputum cell counts: effect on exacerbations. Eur Respir J. 2006;27(3):483–494.
- Cowan DC, Cowan JO, Palmay R, et al. Effects of steroid therapy on inflammatory cell subtypes in asthma. Thorax. 2010;65(5):384–390.
- Kupczyk M, Dahlen B, Sterk PJ, et al. Stability of phenotypes defined by physiological variables and biomarkers in adults with asthma. Allergy. 2014;69(9):1198–1204.
- Haldar P, Brightling CE, Hargadon B, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. New Engl J Med. 2009;360(10):973–984.
- Wenzel SE, Schwartz LB, Langmack EL, et al. Evidence that severe asthma can be divided pathologically into two inflammatory subtypes with distinct physiologic and clinical characteristics. Am J Respir Crit Care Med. 1999;160(3):1001–1008.
- Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380(9842):651–659.
- Nair P, Pizzichini MM, Kjarsgaard M, et al. Mepolizumab for prednisone-dependent asthma with sputum eosinophilia. N Engl J Med. 2009;360(10):985–993.
- Van Veen IH, Ten BA, Gauw SA, et al. Consistency of sputum eosinophilia in difficult-to-treat asthma: a 5-year follow-up study. J Allergy Clin Immunol. 2009;124(3):615–617.e2.
- Klion AD, Bochner BS, Gleich GJ, et al. Approaches to the treatment of hypereosinophilic syndromes: a workshop summary report. J Allergy Clin Immunol. 2006;117(6):1292–1302.
- Walford HH, Doherty TA. Diagnosis and management of eosinophilic asthma: a US perspective. J Asthma Allergy. 2014;7:53–65.
- Groh M, Pagnoux C, Baldini C, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss) (EGPA) consensus task force recommendations for evaluation and management. Eur J Intern Med. 2015;26(7):545–553.
- In ‘T Veen JCCM, De Gouw HWFM, Smits HH, et al. Repeatability of cellular and soluble markers of inflammation in induced sputum from patients with asthma. Eur Respir J. 1996;9(12):2441–2447.
- Korevaar DA, Westerhof GA, Wang J, et al. Diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(4):290–300.
- Ten Brinke A, De Lange C, Zwinderman AH, et al. Sputum induction in severe asthma by a standardized protocol: predictors of excessive bronchoconstriction. Am J Respir Crit Care Med. 2001;164(5):749–753.
- Berry A, Busse WW. Biomarkers in asthmatic patients: has their time come to direct treatment? J Allergy Clin Immunol. 2016;137(5):1317–1324.
- Hastie AT, Moore WC, Li H, et al. Biomarker surrogates do not accurately predict sputum eosinophil and neutrophil percentages in asthmatic subjects. J Allergy Clin Immunol. 2013;132(1):72–80.
- Spector SL, Tan RA. Is a single blood eosinophil count a reliable marker for “eosinophilic asthma? J Asthma. 2012;49(8):807–810.
- Flood-Page PT, Menzies-Gow AN, Kay AB, et al. Eosinophil’s role remains uncertain as anti-interleukin-5 only partially depletes numbers in asthmatic airway. Am J Respir Crit Care Med. 2003;167(2):199–204.
- Alving K, Weitzberg E, Lundberg JM. Increased amount of nitric oxide in exhaled air of asthmatics. Eur Respir J. 1993;6(9):1368–1370.
- Mummadi SR, Hahn PY. Update on exhaled nitric oxide in clinical practice. Chest. 2016;149(5):1340–1344.
- Dweik RA, Boggs PB, Erzurum SC, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184(5):602–615.
- Berry MA, Shaw DE, Green RH, et al. The use of exhaled nitric oxide concentration to identify eosinophilic airway inflammation: an observational study in adults with asthma. Clin Exp Allergy. 2005;35(9):1175–1179.
- Jatakanon A, Lim S, Kharitonov SA, et al. Correlation between exhaled nitric oxide, sputum eosinophils, and methacholine responsiveness in patients with mild asthma. Thorax. 1998;53(2):91–95.
- Silkoff PE, Lent AM, Busacker AA, et al. Exhaled nitric oxide identifies the persistent eosinophilic phenotype in severe refractory asthma. J Allergy Clin Immunol. 2005;116(6):1249–1255.
- Corren J, Lemanske RF, Hanania NA, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365(12):1088–1098.
- Brusselle GG, Maes T, Bracke KR. Eosinophils in the spotlight: eosinophilic airway inflammation in nonallergic asthma. Nat Med. 2013;19(8):977–979.
- Crespo A, Giner J, Torrejon M, et al. Clinical and inflammatory features of asthma with dissociation between fractional exhaled nitric oxide and eosinophils in induced sputum. J Asthma. 2016;53(5):459–464.
- Petsky HL, Cates CJ, Lasserson TJ, et al. A systematic review and meta-analysis: tailoring asthma treatment on eosinophilic markers (exhaled nitric oxide or sputum eosinophils). Thorax. 2012;67(3):199–208.
- Khanduja KL, Kaushik G, Khanduja S, et al. Corticosteroids affect nitric oxide generation, total free radicals production, and nitric oxide synthase activity in monocytes of asthmatic patients. Mol Cell Biochem. 2011;346(1–2):31–37.
- Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J. 2016;47(2):410–419.
- McNicholl DM, Stevenson M, McGarvey LP, et al. The utility of fractional exhaled nitric oxide suppression in the identification of nonadherence in difficult asthma. Am J Respir Crit Care Med. 2012;186(11):1102–1108.
- Jia G, Erickson RW, Choy DF, et al. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J Allergy Clin Immunol. 2012;130(3):647-654.e10.
- Simpson JL, Yang IA, Upham JW, et al. Periostin levels and eosinophilic inflammation in poorly-controlled asthma. BMC Pulm Med. 2016;16(1):67.
- Woodruff PG, Boushey HA, Dolganov GM, et al. Genome-wide profiling identifies epithelial cell genes associated with asthma and with treatment response to corticosteroids. Proc Natl Acad Sci U S A. 2007;104(40):15858–15863.
- Mouthuy J, Viart S, Ladjemi MZ, et al. Mite allergen-specific IgE is detectable in bronchial secretions of patients with nonatopic asthma and correlates with mucosal expression of periostin. J Allergy Clin Immunol. 2015;136(6):1685-1688e1681-1682.
- Wagener AH, De Nijs SB, Lutter R, et al. External validation of blood eosinophils, FE(NO) and serum periostin as surrogates for sputum eosinophils in asthma. Thorax. 2015;70(2):115–120.
- Froidure A, Mouthuy J, Durham SR, et al. Asthma phenotypes and IgE responses. Eur Respir J. 2016;47(1):304–319.
- Cieslewicz G, Tomkinson A, Adler A, et al. The late, but not early, asthmatic response is dependent on IL-5 and correlates with eosinophil infiltration. J Clin Invest. 1999;104(3):301–308.
- Djukanovic R, Wilson SJ, Kraft M, et al. Effects of treatment with anti-immunoglobulin E antibody omalizumab on airway inflammation in allergic asthma. Am J Respir Crit Care Med. 2004;170(6):583–593.
- Westerhof GA, Korevaar DA, Amelink M, et al. Biomarkers to identify sputum eosinophilia in different adult asthma phenotypes. Eur Respir J. 2015;46(3):688–696.
- Massanari M, Holgate ST, Busse WW, et al. Effect of omalizumab on peripheral blood eosinophilia in allergic asthma. Respir Med. 2010;104(2):188–196.
- Pavord ID, Bafadhel M. Exhaled nitric oxide and blood eosinophilia: independent markers of preventable risk. J Allergy Clin Immunol. 2013;132(4):828–829.
- Castro M, Wenzel SE, Bleecker ER, et al. Benralizumab, an anti-interleukin 5 receptor α monoclonal antibody, versus placebo for uncontrolled eosinophilic asthma: a phase 2b randomised dose-ranging study. Lancet Respir Med. 2014;2(11):879–890.
- Khatry DB, Gossage DL, Geba GP, et al. Discriminating sputum-eosinophilic asthma: accuracy of cutoffs in blood eosinophil measurements versus a composite index, ELEN. J Allergy Clin Immunol. 2015;136(3):812–814.e812.
- Johansson MW, Evans MD, Crisafi GM, et al. Serum periostin is associated with type 2 immunity in severe asthma. J Allergy Clin Immunol. 2016;137:1904-1907.e2.
- Heaney LG, Djukanovic R, Woodcock A, et al. Research in progress: medical research council united kingdom refractory asthma stratification programme (RASP-UK). Thorax. 2016;71(2):187–189.
- Belda J, Leigh R, Parameswaran K, et al. Induced sputum cell counts in healthy adults. Am J Respir Crit Care Med. 2000;161(2 Pt 1):475–478.
- Hanania NA, Noonan M, Corren J, et al. Lebrikizumab in moderate-to-severe asthma: pooled data from two randomised placebo-controlled studies. Thorax. 2015;70(8):748–756.
- Fowler SJ, Tavernier G, Niven R. High blood eosinophil counts predict sputum eosinophilia in patients with severe asthma. J Allergy Clin Immunol. 2015;135(3):822–824.e822.
- Bjermer L, Lemiere C, Maspero J, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil levels: a randomized phase 3 study. Chest. 2016. doi: 10.1016/j.chest.2016.03.032.
- Castro M, Zangrilli J, Wechsler ME, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3(5):355–366.
- Corren J, Weinstein S, Janka L, et al. Phase 3 Study of Reslizumab in Patients with Poorly Controlled Asthma: Effects Across a Broad Range of Eosinophil Counts. Chest. 2016. doi: 10.1016/j.chest.2016.03.018.
- Ortega H, Katz L, Gunsoy N, et al. Blood eosinophil counts predict treatment response in patients with severe eosinophilic asthma. J Allergy Clin Immunol. 2015;136(3):825–826.
- Katz LE, Gleich GJ, Hartley BF, et al. Blood eosinophil count is a useful biomarker to identify patients with severe eosinophilic asthma. Ann Am Thorac Soc. 2014;11(4):531–536.
- Wenzel S, Castro M, Corren J, et al. Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high-dose inhaled corticosteroids plus a long-acting beta agonist: a randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. Lancet. 2016.;388(10039):31–44.
- Hillas G, Kostikas K, Mantzouranis K, et al. Exhaled nitric oxide and exhaled breath condensate pH as predictors of sputum cell counts in optimally treated asthmatic smokers. Respirology. 2011;16(5):811–818.
- Alvarez-Puebla MJ, Rivera JMO, Almudevar E, et al. Cutoff point for exhaled nitric oxide corresponding to 3% sputum eosinophils. J Invest Allerg Clin. 2015;25(2):107–111.
- Schneider A, Schwarzbach J, Faderl B, et al. FENO measurement and sputum analysis for diagnosing asthma in clinical practice. Respir Med. 2013;107(2):209–216.
- Green RH, Pavord I. Stability of inflammatory phenotypes in asthma. Thorax. 2012;67(8):665–667.
- Ortega H, Gleich G, Mayer B, et al. Reproducibility of a single blood eosinophil measurement as a biomarker in severe eosinophilic asthma. Ann Am Thorac Soc. 2015;12(12):1896–1897.
- Nanda CR, Singapuri A, Soares M, et al. Domiciliary exhaled nitric oxide and eosinophilic airway inflammation in adults with asthma. Eur Respir J. 2016;48:242–244.
- De Groot JC, Storm H, Amelink M, et al. Clinical profile of patients with adult-onset eosinophilic asthma. ERJ Open Res. 2016;2(2):00100–02015.
- Boots AW, Bos LD, Van Der Schee MP, et al. Exhaled molecular fingerprinting in diagnosis and monitoring: validating volatile promises. Trends Mol Med. 2015;21(10):633–644.
- Van Der Schee MP, Paff T, Brinkman P, et al. Breathomics in lung disease. Chest. 2015;147(1):224–231.
- Van De Kant KD, Van Der Sande LJ, Jobsis Q, et al. Clinical use of exhaled volatile organic compounds in pulmonary diseases: a systematic review. Respir Res. 2012;13:117.
- Ibrahim B, Basanta M, Cadden P, et al. Non-invasive phenotyping using exhaled volatile organic compounds in asthma. Thorax. 2011;66(9):804–809.
- Plaza V, Crespo A, Giner J, et al. Inflammatory asthma phenotype discrimination using an electronic nose breath analyzer. J Investig Allergol Clin Immunol. 2015;25(6):431–437.
- van der Schee MP, Palmay R, Cowan JO, et al. Predicting steroid responsiveness in patients with asthma using exhaled breath profiling. Clin Exp Allergy. 2013;43(11):1217–1225.
- Wheelock CE, Goss VM, Balgoma D, et al. Application of ‘omics technologies to biomarker discovery in inflammatory lung diseases. Eur Respir J. 2013;42(3):802–825.
- Leckie MJ, Brinke A, Khan J, et al. Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsìveness, and the late asthmatic response. Lancet. 2000;356(9248):2144–2148.
- Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16(1):45–56.
- Yu S, Kim HY, Chang YJ, et al. Innate lymphoid cells and asthma. J Allergy Clin Immunol. 2014;133:943–950.
- Spits H, Artis D, Colonna M, et al. Innate lymphoid cells–a proposal for uniform nomenclature. Nat Rev Immunol. 2013;13(2):145–149.
- Smith SG, Chen R, Kjarsgaard M, et al. Increased numbers of activated group 2 innate lymphoid cells in the airways of patients with severe asthma and persistent airway eosinophilia. J Allergy Clin Immunol. 2016;137(1):75-86.e8.
- Liu T, Wu J, Zhao J, et al. Type 2 innate lymphoid cells: a novel biomarker of eosinophilic airway inflammation in patients with mild to moderate asthma. Respir Med. 2015;109(11):1391–1396.
- Lambrecht BN, Hammad H. Allergens and the airway epithelium response: gateway to allergic sensitization. J Allergy Clin Immunol. 2014;134(3):499–507.
- Gauvreau GM, O’Byrne PM, Boulet LP, et al. Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. N Engl J Med. 2014;370(22):2102–2110.
- Nagarkar DR, Poposki JA, Tan BK, et al. Thymic stromal lymphopoietin activity is increased in nasal polyps of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;132(3):593–600e512.
- Buchheit KM, Cahill KN, Katz HR, et al. Thymic stromal lymphopoietin controls prostaglandin D2 generation in patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2016;137(5):1566–1576e1565.
- Holgate ST. Innate and adaptive immune responses in asthma. Nat Med. 2012;18(5):673–683.
- Na HJ, Hamilton RG, Klion AD, et al. Biomarkers of eosinophil involvement in allergic and eosinophilic diseases: review of phenotypic and serum markers including a novel assay to quantify levels of soluble Siglec-8. J Immunol Methods. 2012;383(1–2):39–46.
- Kiwamoto T, Kawasaki N, Paulson JC, et al. Siglec-8 as a drugable target to treat eosinophil and mast cell-associated conditions. Pharmacol Ther. 2012;135(3):327–336.
- Denner DR, Sangwan N, Becker JB, et al. Corticosteroid therapy and airflow obstruction influence the bronchial microbiome, which is distinct from that of bronchoalveolar lavage in asthmatic airways. J Allergy Clin Immunol. 2016;137(5):1398–1405e1393.
- Zhang Q, Cox M, Liang Z, et al. Airway microbiota in severe asthma and relationship to asthma severity and phenotypes. PLoS One. 2016;11(4):e0152724.
- Pavord ID, Wardlaw AJ. The A to E of airway disease. Clin Exp Allergy. 2010;40(1):62–67.
- Orie NG, Slutter HJ, De V, et al. Chronic nonspecific respiratory diseases. Ned Tijdschr Geneeskd. 1961;105:2136–2139.
- Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015;372(9):793–795.
- Sterk PJ. Chronic diseases like asthma and COPD: do they truly exist? Eur Respir J. 2016;47(2):359–361.
- Global Initiative for Asthma. Global strategy for asthma management and prevention; 2016. Cited 2016 May 31. Available from: www.ginasthma.org
