Abstract
Purpose
The purpose of this study was to clarify whether the novel lateral transfer assist robot facilitates easier transfers compared with a wheelchair in post-stroke hemiparesis patients.
Methods
This cross-sectional study enrolled 20 post-stroke hemiparesis patients, and the task difficulty of transfers was compared between a wheelchair and lateral transfer assist robot. All participants were asked to transfer from either wheelchair or lateral transfer assist robot to a platform table and back. The primary outcome was the transfer score of the Functional Independence Measure. The secondary outcome was the time required for transfer.
Results
The transfer score of the Functional Independence Measure was significantly higher with lateral transfer assist robot than with wheelchair (p < .001). The transfer times from these devices to a platform table and back showed no significant differences (to device from platform table: 7.8 s, lateral transfer assist robot vs 7.6 s, wheelchair, p > .05: device to platform table: 7.1 s, lateral transfer assist robot vs 8.0 s, wheelchair, p > .05).
Conclusions
Transfer with a lateral transfer assist robot is easier than with wheelchair and facilitates independence in post-stroke hemiparesis patients.
Transfer skill influences the functional independence and quality of life of a wheelchair user
A novel structural mobility device—the lateral transfer assist robot (LTAR)—can facilitate transfers
The LTAR could improve the degree of independence for transfers than the wheelchair, without any time loss, in post-stroke hemiparesis patients
The LTAR could potentially reduce the risk for falls in various medical and care facilities
IMPLICATIONS FOR REHABILITATION
Introduction
Stroke is one of the most common neurological disorders. In 2019, the American Heart Association reported that approximately 800,000 people experience a stroke in the United States every year [Citation1]. Stroke patients are unable to fully recover from hemiparetic motor and sensory deficits even after rehabilitative treatment. Many stroke survivors live in the community with prolonged long-term disability in daily life after hospital discharge [Citation2,Citation3]. Therefore, one of the crucially important purposes of the rehabilitative approach in stroke patients is to reduce the amount of assistance they require in fulfilling the activities of daily living.
Stroke patients with a gait disorder usually use a wheelchair for daily mobility. The wheelchair is an excellent mobility assistive device, although transferring from a wheelchair proves difficult for these patients because of the high burden on the upper limbs and risk of falls. Nonetheless, for wheelchair users, transferring from the wheelchair to another surface is an indispensable and essential factor for maintaining independence in daily life. Most wheelchair user performs approximately 15 transfers per day [Citation4]. The transfer skill influences the functional independence and quality of life of a wheelchair user [Citation5]. However, transfer is ranked as one of the most difficult factors among all wheelchair-related activities [Citation6,Citation7] and is the most frequently mentioned activity to have been undertaken at the time of a fall [Citation8,Citation9].
A common transfer method is the squat/stand pivot transfer, wherein patients lift themselves to raise their buttock over some obstacle (e.g., wheelchair armrest) and then rotate their buttock onto the desired surface during transfer while ensuring no contact of their buttock on those obstacles. However, many patients need caregiver assistance for lifting and rotating their buttocks during transfer [Citation10]. The difficulty level of these transfers is affected by differences in height, width of gap (>8.9 cm), and presence of an obstacle (e.g., armrest or wheels) between the transfer surfaces [Citation11].
We demonstrated that a novel approach of lateral transfer, which is defined as transferring laterally between surfaces without any height differences, gaps, or obstacles, and without using the flip-up-armrest and transfer-board, can facilitate independent transfers and decrease the need for transfer assistance in post-stroke hemiparesis patients [Citation12]. In combination with the abovementioned approach, a novel structural mobility device—the lateral transfer assist robot (LTAR)—has been proposed to facilitate transfers [Citation13]. In healthy participants, a previous study showed that the extent of vertical movement of the centre of mass of users was decreased with LTAR compared to that with the wheelchair [Citation14].
We hypothesised that LTAR can contribute to easier transfers and higher degree of independence among post-stroke hemiparesis patients. The aim of this study was to test whether LTAR is easier to transfer than WC among hemiparetic stroke patients.
Methods
Study design, setting and participants
The present study used a cross-sectional design for convenience sampling among inpatients in the subacute recovery phase in a rehabilitation ward at a university hospital. The study included 20 hemiparesis patients, with a mean age of 65.4 years (standard deviation [SD] 16.9; 15 men, 5 women), after a subacute stroke who were using a standard wheelchair for activities of daily living. The exclusion criteria were the presence of bilateral, cerebellar, and/or brain-stem lesions; severe upper-extremity pain and/or injury; severe injury of the lower extremity on the non-paretic side; other neuromuscular disease; and pressure sores. The study protocol was approved by the institutional ethics committee (approval no. HM16-311). All patients provided written informed consent prior to study participation. This study was performed in accordance with the principles of the Declaration of Helsinki and its later amendments.
Experimental setup
The experimental setup consisted of a platform table and two mobility devices: the standard wheelchair and LTAR. The seat of the wheelchair and that of the LTAR was adjusted to the same height as that of the platform table. In preparation for transfer from/to the wheelchair, the footrest was removed. In the starting position, the wheelchair was set close to the platform table at a 20–45° angle to the non-paretic side of the participant. On the other side, the LTAR was placed in close contact with the other side of the platform table. All wheels of the devices were locked in place. Both soles of the participants’ feet were placed on the floor during the squat/stand on the wheelchair or LTAR.
All participants were asked to perform two transfer methods using the specified devices. For the wheelchair transfer, the participants were asked to carry out a squat/stand-pivot transfer in a similar manner to what they do in daily living. For the LTAR transfer, the participants were asked to perform a lateral transfer, as described in previous studies [Citation12–14]. In every trial, an occupational therapist closely supervised the patients to prevent a fall during the transfers. Based on the patient’s transfer ability, an occupational therapist supported the lifting and/or rotating of participants’ buttocks with minimal assistance for both methods. All participants were allowed to rest for a few minutes between transfers of the wheelchair and LTAR based on their fatigue levels.
Lateral transfer assist robot
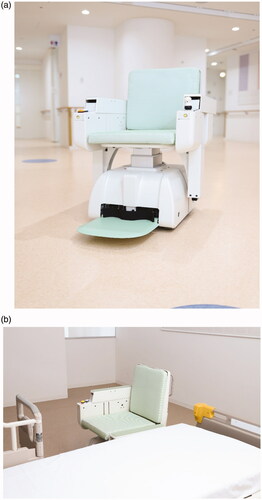
The LTAR () has been previously described in some reports [Citation13,Citation14]. Briefly, the LATR is a novel mobility device that raises and lowers the footrest and armrest on the side of transfer. The seat is raised and lowered to the same level as the transfer surface. The wheels are retracted under the seat to ensure that these do not interfere with the user’s movement. These key features achieve a setting wherein there are no height differences, gaps or obstacles (e.g., armrests or wheels) between the transfer surfaces, and no complicated brake operations are required during the transfer. As another feature, the LTAR has 360° manoeuvrability for facilitating easy movement close to the transfer surface because of the mecanum wheels, which have free rollers with axes tilted at 45° from the wheel plane to the outer circumference of each wheel.
Figure 1. Latest lateral transfer assist robot. a) Oblique front view of the lateral transfer assist robot (LTAR). The joystick is placed in the armrest on the left side and can be placed on the right side depending on the user’s preference. b) The preparatory state of the LTAR before transfer. When the armrest covers are closed on the transfer side prior to the transfer, the height of the seat and armrest increase or decreases until it is at the same height as the transfer surfaces. At the same time, the footrest moves down to lie flat at the floor level.
Assessment
An item of the bed-transfer—Functional Independence Measure (FIM)—was used as a primary outcome [Citation15,Citation16]. The FIM transfer score represents the amount of physical assistance and level of independence during transfers based on an ordinal scale from 1 (maximum assistance) to 7 (independent). The secondary outcome was the amount of time required for transfers to assess the temporal efficiency between two transfer methods. All transfers were video-recorded for assessment by three occupational therapists (including the therapist who supervised or assisted the transfer). Disagreements between the raters were resolved by discussion until a consensus was obtained.
Statistical analysis
The Wilcoxon signed rank test was used to compare the transfer score of the FIM for squat/stand-pivot transfer and lateral transfer using the wheelchair and LTAR, respectively. Performance times for transfers were compared between the wheelchair and LTAR transfers using paired t-test and were analysed based on the transfer direction: 1) from the platform table to the wheelchair or LTAR and 2) from the wheelchair or LTAR to the platform table. To eliminate the effect of degree of assistance, patients who needed assistance during the transfer were excluded from the analysis of the secondary outcome. All statistical analyses were performed with R (version 3.4.3; Institute of Statistical Mathematics, Tokyo, Japan). The statistical significance level was set at a p-value of .05.
Results
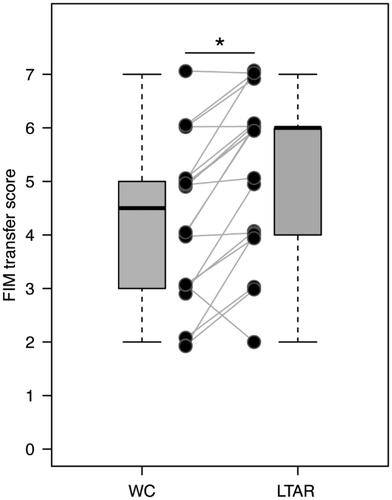
The transfer score of the FIM for each device is shown in . The transfer score was higher for the LTAR than for the wheelchair in almost all patients (p = .0003). Moreover, 10 and 13 patients did not need any physical assistance during transfers with the wheelchair and LTAR, respectively.
Figure 2. Functional Independence Measure (FIM) transfer scores for the wheelchair (WC) and lateral transfer assist robot (LTAR). The figure shows the difference in the FIM transfer scores of each participant (line plot) and for all participant (boxplot). The central lines of the boxplot represent medians; the box limits comprise the interquartile range from 25% and 75%. The boxplot whiskers extend to 1.5 times the interquartile range from the first and third quartiles.
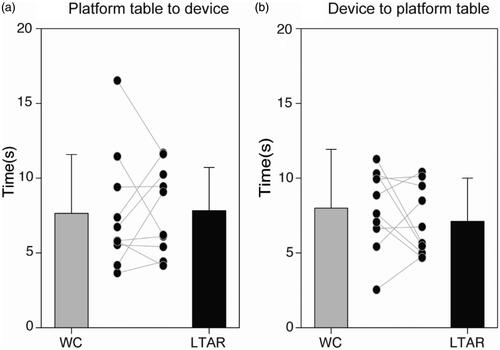
For an evaluation of the performance time, 10 patients who could independently transfer with both methods were included in the further analysis of the secondary outcome. The mean performance time in the LTAR was 7.8 s (from the platform table) and 7.1 s (to the platform table), whereas that in the wheelchair was 7.6 s (from the platform table) and 8.0 s (to the platform table) (). There was no statistical difference in the performance times between the two devices, regardless of the transfer direction. All patients performed all transfers without any adverse events.
Figure 3. Transfer performance time. A boxplot shows the mean transfer performance time: a) from the platform table to the wheelchair (WC) or to the lateral transfer assist robot (LTAR), and b) from the WC or LTAR to the platform table. The vertical axis shows time in seconds. The solid line-plot represents the performance time of transfers for each patient.
Discussion
This study showed that LTAR could better improve the degree of independence for transfers than the wheelchair in post-stroke hemiparesis patients. In addition, there was no difference in the transfer time between the two devices.
A previous report showed that the transfer score of the FIM was strongly associated with balance function [Citation17]. Other studies have reported that the lower limbs play an important role in truncal support and control of sitting balance during forward movements, particularly with regard to the centre of gravity in a sitting position that occurs during wheelchair transfer [Citation18,Citation19]. With regard to the difference in the degree of independence for transfers, one of the main reasons might be that the lateral transfer method does not require a high balancing ability or application of pedal force for interrupting the forward momentum of the body mass to prevent a fall in the forward direction during transfer. In the typical squat/stand-pivot transfer, patients must lift their buttocks to avoid hitting the armrest and wheel of the wheelchair to perform the transfer from a wheelchair to another surface [Citation10,Citation20–25]. However, for LTAR, patients do not need to raise their centre of gravity and shift their centre of gravity mainly laterally along a horizontal plane [Citation12–14].
With regard to the performance time required for a transfer with the two methods, there was no difference between the two transfer methods. This finding is a crucially important factor of relevance in hospitals and nursing homes because of the limited amount of care-time per patient. Several transfer-assistive devices (i.e., mechanical lifts and power-assisted systems) have been developed, although these previously developed devices require more time from patients or caregivers to perform transfers than with a wheelchair. Alamgir et al reported that transfers with ceiling lift-type transfer-assistive device require 52.1 s (wheelchair to bed) and 57.9 s (bed to wheelchair), excluding the preparatory time, in a long-term care facility [Citation26]. For a floor lift-type device, transfers require 104.6 s (wheelchair to bed) and 100.6 s (bed to wheelchair) [Citation26]. In contrast, the results of this study showed that the mean performance time for transfers with the LTAR was 7.1 s (from the platform table) and 7.8 s (to the platform table).
Transfers between the wheelchair and desired surface have to surmount several barriers (e.g., the height difference, armrest, and wheel). To overcome these barriers, various older low-tech devices have included transfer boards, slides, and slings [Citation25,Citation27,Citation28]. Despite the advantage of low cost with those devices, they require greater effort from participants to operate them and are incapable of completely reducing participants’ load [Citation14,Citation29]. Based on the findings of the present study, the LTAR might have a clinical benefit as a novel transfer assistive device that completely eliminates these barriers while maintaining performance times that are equal to those for the wheelchair.
One of the most important aspects of rehabilitative care is to ensure safe independence in the activities of daily living. Falls are one of the most frequent complications in community-dwelling stroke survivors [Citation9,Citation30–32]. Consequences of falls can cause further physical complications in community-dwelling stroke survivors (e.g., soft tissue injuries [Citation33], lumbar compression fracture [Citation8], and hip fracture [Citation34,Citation35]). Therefore, this newly developed mobility assistive device might facilitate reduction in the risk of falls because of improved level of independence for transfers.
The present pilot study had some limitations. First, the degree of participants’ disability severity only ranged from 2 to 7 in the FIM transfer score. For patients who require maximal assistance for transfer, it is unclear whether the extent of assistance needed would decrease when caregivers use the LTAR. This point should be clarified in further studies among patients who require maximal assistance for transfers. Second, this study only examined the effectiveness and efficiency of LTAR with regard to the difficulty of transfer and transfer performance time. Further research should examine the effectiveness of LTAR with regard to various outcomes (e.g., reduction of the risk of falls, decrease in caregiver burden, and usability within the home environment) to identify the target populations where LTAR has the most efficacy.
In conclusion, LTAR transfer is easier than wheelchair transfer, without any time loss, in post-stroke hemiparesis patients. Therefore, the LTAR could improve the transfer ability in post-stroke hemiparesis patients and potentially reduce the risk for falls.
Acknowledgements
We are grateful to the medical staff at our university hospital for their contribution to this study.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528.
- Scrutinio D, Lanzillo B, Guida P, et al. Development and validation of a predictive model for functional outcome after stroke rehabilitation: the Maugeri Model. Stroke. 2017;48(12):3308–3315.
- Reistetter TA, Graham JE, Deutsch A, et al. Utility of functional status for classifying community versus institutional discharges after inpatient rehabilitation for stroke. Arch Phys Med Rehabil. 2010;91(3):345–350.
- Pentland WE, Twomey LT. Upper limb function in persons with long term paraplegia and implications for independence: part I. Paraplegia. 1994;32(4):211–218.
- Nyland J, Quigley P, Huang C, et al. Preserving transfer independence among individuals with spinal cord injury. Spinal Cord. 2000;38(11):649–657.
- Tsuji T, Sonoda S, Domen K, et al. ADL structure for stroke patients in Japan based on the functional independence measure. Am J Phys Med Rehabil. 1995;74(6):432–438.
- Linacre JM, Heinemann AW, Wright BD, et al. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75(2):127–132.
- Wada N, Sohmiya M, Shimizu T, et al. Clinical analysis of risk factors for falls in home-living stroke patients using functional evaluation tools. Arch Phys Med Rehabil. 2007;88(12):1601–1605.
- Weerdesteyn V, de Niet M, van Duijnhoven HJ, et al. Falls in individuals with stroke. J Rehabil Res Dev. 2008;45(8):1195–1213.
- Hess JA, Kincl LD, Mandeville DS. Comparison of three single-person manual patient techniques for bed-to-wheelchair transfers. Home Healthcare Now. 2007;25(9):577–579.
- Toro ML, Koontz AM, Cooper RA. The impact of transfer setup on the performance of independent wheelchair transfers. Hum Factors. 2013;55(3):567–580.
- Koyama S, Tanabe S, Saitoh E, et al. Comparison of two methods of bed-to/from-wheelchair transfer in patients with hemiparetic stroke. Fujita Medical Journal. 2020;6(3):81–86.
- Tanabe S, Saitoh E, Koyama S, et al. Designing a robotic smart home for everyone, especially the elderly and people with disabilities. Fujita Medical Journal. 2019;5(2):31–35.
- Tatemoto T, Saitoh E, Tanabe S, et al. Lateral transfer assist robot (LTAR): development of a proof-of-concept prototype. Technol Health Care. 2020;28(2):175–183.
- Keith RA, Granger CV, Hamilton BB, et al. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18.
- The Data Management Service of the Uniform Data System for Medical Rehabilitation and the Center for Functional Assessment Research. Guide for use of the uniform data set for medical rehabilitation, Version 3.0. State University of New York Buffalo; 1990.
- Fujita T, Sato A, Ohashi Y, et al. Amount of balance necessary for the independence of transfer and stair-climbing in stroke inpatients. Disabil Rehabil. 2018;40(10):1142–1145.
- Dean C, Shepherd R, Adams R. Sitting balance I: trunk-arm coordination and the contribution of the lower limbs during self-paced reaching in sitting. Gait Posture. 1999;10(2):135–146.
- Dean CM, Shepherd RB. Task-related training improves performance of seated reaching tasks after stroke. A randomized controlled trial. Stroke. 1997;28(4):722–728.
- Koontz A, Toro M, Kankipati P, et al. An expert review of the scientific literature on independent wheelchair transfers. Disabil Rehabil Assist Technol. 2012;7(1):20–29.
- Koontz AM, Kankipati P, Lin YS, et al. Upper limb kinetic analysis of three sitting pivot wheelchair transfer techniques. Clin Biomech (Bristol, Avon.). 2011;26(9):923–929.
- Koontz AM, Tsai CY, Hogaboom NS, et al. Transfer component skill deficit rates among Veterans who use wheelchairs. J Rehabil Res Dev. 2016;53(2):279–294.
- Krishnan RH, Pugazhenthi S, editors. Development of a self-transfer robotic facility for elderly and disabled. Proceedings of the 2015 International Conference on Robotics, Automation, Control and Embedded Systems (RACE); 2015 Feb 18–25; Chennai, India.
- Rice LA, Smith I, Kelleher AR, et al. Impact of the clinical practice guideline for preservation of upper limb function on transfer skills of persons with acute spinal cord injury. Arch Phys Med Rehabil. 2013;94(7):1230–1246.
- Tsai CY, Boninger ML, Hastings J, et al. Immediate biomechanical implications of transfer component skills training on independent wheelchair transfers. Arch Phys Med Rehabil. 2016;97(10):1785–1792.
- Alamgir H, Li OW, Yu S, et al. Evaluation of ceiling lifts: transfer time, patient comfort and staff perceptions. Injury. 2009;40(9):987–992.
- Gruis KL, Wren PA, Huggins JE. Amyotrophic lateral sclerosis patients' self-reported satisfaction with assistive technology. Muscle Nerve. 2011;43(5):643–647.
- Kjellberg K, Lagerstrom M, Hagberg M. Work technique of nurses in patient transfer tasks and associations with personal factors. Scand J Work Environ Health. 2003;29(6):468–477.
- Sivakanthan S, Blaauw E, Greenhalgh M, et al. Person transfer assist systems: a literature review. Disabil Rehabil Assist Technol. 2019;12(1748–3115):1–10.
- Chin LF, Wang JY, Ong CH, et al. Factors affecting falls in community-dwelling individuals with stroke in Singapore after hospital discharge. smedj. 2013;54(10):569–575.
- Hwang S, Woo Y, Kim KH, et al. Effects of falls experience on cognitive functions and physical activities in community-dwelling individuals with chronic stroke. Int J Rehabil Res. 2013;36(2):134–139.
- Xu T, Clemson L, O'Loughlin K, et al. Risk factors for falls in community stroke survivors: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(3):563–573, e5.
- Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ. 1995;311(6997):83–86.
- Ramnemark A, Nilsson M, Borssén B, et al. Stroke, a major and increasing risk factor for femoral neck fracture. Stroke. 2000;31(7):1572–1577.
- Salehi Omran S, Murthy SB, Navi BB, et al. Long-term risk of hip fracture after ischemic stroke. Neurohospitalist. 2019;50(Suppl_1):1941874419859755.
