Abstract
Purpose
We aimed to identify assistive technologies that are promising for addressing loneliness in people living with dementia in long-term care.
Materials and methods
A scoping review was conducted. EBSCO, PubMed, Cochrane Library, and ProQuest were searched from 2000 to 2020. The included studies were selected by three independent researchers and summarised, compared, and categorized according to technology type. Publications were eligible for inclusion when they reported on psychosocial interventions aiming to reduce loneliness and/or social isolation in people with dementia in long-term care settings.
Results
Twenty-four papers were included (20 original research papers and four reviews). Most studies were conducted in Australia and Europe. The studies aimed to investigate two different types of assistive technology: social robots, and multimedia computer systems. Most studies focussed on behaviour, engagement, and mood as primary outcomes. Only one study directly aimed to alleviate loneliness.
Conclusions
Even though only one study addressed loneliness directly, it became clear that assistive technologies used to apply psychosocial interventions have the potential to impact loneliness in people with dementia in long-term care. However, it remains unclear why loneliness was not included as an outcome and how loneliness could become a key outcome in evaluating assistive technologies.
Loneliness among older adults is associated with health risks, such as the development of dementia, depression, and increased mortality.
Ambient Assisted Living (AAL) technologies have been studied to address loneliness for older adults; however people with dementia are often excluded from such studies.
This diverse group of technologies is shown to have a promising impact on outcomes, such as social engagement, quality of life, and mood, but loneliness was studied less often.
More research is needed to discover the potential of assistive technologies for people with dementia living in long-term care.
IMPLICATIONS FOR REHABILITATION
Introduction
Ageing brings various challenges, as it often affects physical, psychological, and social functioning. One of the pressing issues among older adults is loneliness [Citation1,Citation2]. Loneliness is often defined “as a subjective feeling state of being alone, separated or apart from others and is an imbalance between desired and actual social contacts” [Citation3]. In the literature, the terms “loneliness” and “social isolation” are often used interchangeably [Citation4–6]. Social isolation is typically defined as social disconnectedness, presenting as a lack of social relationships and low levels of participation in social activities [Citation7].
Loneliness among older adults is associated with further health risks [Citation8], self-neglecting behaviours [Citation9], and increased mortality rates [Citation10,Citation11]. Loneliness among older adults may also add to the progression of symptoms of dementia and mild cognitive impairment (MCI) [Citation12]. The predictive power of loneliness on the progression of dementia and MCI was found comparable to some biological measures, such as higher cortical amyloid burden [Citation13], genetics, diabetes, and vascular diseases [Citation14].
It is common for people with dementia to move from home to long-term care (LTC) facility as the disease progresses [Citation15]. The move to LTC exacerbates the likelihood of loneliness, social isolation, and depression [Citation16]. The prevalence of moderate loneliness in older adults living in LTC facilities is high, ranging from 31 to 100%, and the prevalence of severe loneliness ranges from 9 to 81%, although studies have not reported dementia-specific numbers [Citation5].
Loneliness and social isolation among older adults are often addressed by several psychosocial interventions, e.g., telephone befriending or horticultural therapy [Citation17]. Psychosocial interventions in dementia were defined as physical, cognitive, or social activities that may help people cope with their dementia and maintain or improve their functioning, interpersonal relationships, and well-being [Citation18]. However, the experience of loneliness is largely subjective. As there is no one-size-fits-all approach to address loneliness, the need to tailor interventions to suit the needs of individuals is growing [Citation17]. It has been suggested that future research should focus on identifying evidence-based [Citation17], sophisticated [Citation19], and theory-driven [Citation20] interventions for people living with dementia (PlwD).
In the past two decades, there was enormous growth in research into assistive technologies in dementia care [Citation21]. Assistive technologies for PlwD can be defined as “any item, piece of equipment, product or system driven by electronics, whether acquired commercially, off-the-shelf, modified or customized, that is used to help persons with dementia in dealing with the consequences of dementia” [Citation22]. Assisted living technologies based on this model are called ambient assisted living (AAL) tools [Citation23].
The potential of technologies to support PlwD and their caregivers in different care settings is of interest to policymakers and governments. In fact, the benefits of AAL are visible in many areas of life for PlwD [Citation24]. In addition to positive effects, ethical concerns are raised, such as the impact of the social robot on the quality of care and human relations [Citation24].
However, only a few technologies in dementia care are targeted at LTC facilities [Citation25]. Therefore, we performed a scoping review to provide an overview of studies that used AAL technologies to impact loneliness for PlwD living in LTC. The following research questions were applied: (1) what is the function and impact of AAL technologies in addressing the loneliness of PwlD living in LTC settings? (2) Which AAL device(s) could be used to provide psychosocial interventions that are the most promising for impacting loneliness among PlwD living in LTC settings?
Methods
A scoping review approach was chosen, as the topic of assistive technologies for people with dementia in LTC settings for loneliness is novel and was not fully examined. The review mapped out the empirical evidence on the use of assistive technology and psychosocial interventions that have been proposed to impact loneliness or social isolation in people with dementia living in LTC. The conduct of this scoping review was based on PRISMA frameworks and principles [Citation26].
For the purposes of this review, an LTC facility was defined as any established setting providing long-term care to older adults in a residential care facility and/or nursing home. We applied a broad definition of loneliness [Citation3], which allowed us to include studies that did not necessarily focus directly on loneliness but on related concepts, such as social interaction, communication, engagement, and social behaviour.
The inclusion criteria were as follows: studies with any design and research method that reported on psychosocial and health promotion interventions delivered by technology aimed to elicit change in loneliness and/or social isolation, investigated any outcomes related to the concept of loneliness, included persons with all types and stages of dementia (not necessarily clinically diagnosed) living in LTC and were published in English. Given recent advances in technology, studies published between 2000 and 2020 were included.
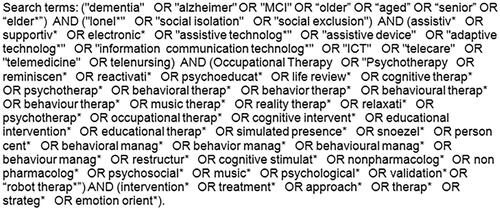
The exclusion criteria were as follows: mixed cohort studies, unless the results for study participants with dementia were distinguishable from the results for other participants; studies focussed on technologies without their own computing capacity, for example, rails, wheelchairs, or hearing aids; studies with no outcomes related to the concept of loneliness, such as improvement in cognition or frequency of falls; and studies published in a language other than English. Conference proceedings, letters, news, study protocols, or publications without an abstract were also excluded. The search string is displayed in .
The search terms were adapted for each database: EBSCO, PubMed, Cochrane Library, and ProQuest. All reference lists of the included studies were hand-searched to identify any additional potentially relevant studies. EndNote 9 [Citation27], and COVIDENCE [Citation28] were used for data management, screening, and data extraction. The first author (BB) conducted the initial title/abstract screening. G.A. and V.H. then worked independently of each other to screen all remaining studies by title and abstract. Studies that did not meet the eligibility criteria were excluded. The full texts of the remaining studies were assessed independently by three members of the research team (B.B., G.A., and V.H.). Any disagreement about study inclusion was solved in a discussion within the author team. Key information, including the year, country, design, aim, type of technology, type of intervention, outcome measures, and key findings, was extracted from the included publications. The studies were summarised, grouped, and compared for similarities and differences. In particular, the studies were compared according to the aim, type of technology used, key findings, and proposed mechanisms for the potential impact of technology on loneliness. Definitions of terms in interventions, outcome measures, dementia symptoms, and assessment methods were compared. Based on the AAL technologies evaluated in the included studies categories of AAL compared by function and effect of AAL in the included papers were analyzed, thus categories of AAL in this paper were decided.
The following sections will present our findings categorized first by the research question, second by activities, and third by type of technology, i.e., findings on studies involving social robots and multimedia computer programs. These sections will present findings from both original research and review papers, with a specific focus on the function these devices served and the impact they achieved.
Results
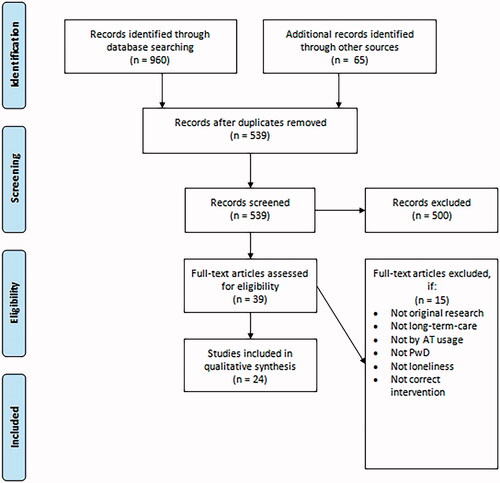
In this section, we first provide information on the characteristics of the studies before moving on to outcomes. In this review, 20 original research papers and four reviews were identified for inclusion (see the PRISMA flowchart in ). Most studies were conducted in Australia (n = 10) or Europe (n = 9), and the others were performed in New Zealand (n = 2), the USA (n = 2), and Japan (n = 1). The included studies reported a broad variety of primary outcomes: loneliness (n = 1) [Citation29,Citation30], perceptions (n = 1) [Citation31], physical fitness (n = 1) [Citation32], acceptability of AAL technology (n = 3) [Citation33–35], quality of life (n = 3) [Citation29,Citation36,Citation37], agitation (n = 3) [Citation37–39], mood (n = 4) [Citation33,Citation36,Citation40,Citation41], engagement (n = 5) [Citation30,Citation32,Citation38,Citation42,Citation43], and behaviour changes (n = 9) [Citation36,Citation38,Citation39,Citation44–49]. Only one paper reported secondary outcomes: engagement (n = 1) [Citation39], mood states (n = 1) [Citation39], and agitation (n = 1) [Citation39].
The studies investigated two different types of AAL technology: social robots (n = 18) [Citation29,Citation30,Citation33,Citation35–42,Citation45–47,Citation50–52], including robotic animals (n = 14) [Citation29,Citation31,Citation35–39,Citation41,Citation42,Citation45,Citation47,Citation50,Citation51,Citation53], humanoid robots (n = 1) [Citation46], and telepresence robots (n = 3) [Citation33,Citation51,Citation52]; and multimedia computer systems (n = 6) [Citation32,Citation34,Citation43,Citation44,Citation48,Citation49]. Furthermore, the original studies assessed the effect of technologies (n = 16) [Citation29,Citation31,Citation32,Citation36–40,Citation43–50], the function of technologies (n = 3) [Citation33–35], or both (n = 1) [Citation30], whereas the included reviews addressed heterogeneous outcomes. The papers reported results for people living with dementia at different stages of the disease. However, one study compared results across different stages of dementia [Citation47]. The sample sizes ranged from 4 to 415 participants. In the qualitative and mixed methods studies (n = 11) [Citation31–33,Citation37,Citation40,Citation44–48,Citation50], most (n = 8) [Citation29,Citation32,Citation34–40,Citation43–50] focussed solely on the perspectives of persons with dementia in their findings, while the rest examined family, staff and mixed perspectives. The other papers took the perspectives of staff and families into account. In the mixed methods studies, both standardized measures for loneliness and related outcomes, as well as qualitative analyses of interviews, were used. Some studies measured changes in factors related to QoL, mood states, behaviours, and care relationships with questionnaires or explored the perspectives of participants, families, or staff through the qualitative synthesis of interview data. The key data of the included papers are summarised in (original research papers) and (reviews).
Table 1. Key findings from original research.
Table 2. Key findings from review articles.
Based on the included studies, we identified one AAL device directly aimed at alleviating the loneliness of people with dementia living in LTC settings and 14 AAL devices that are promising for the provision of psychosocial interventions impacting loneliness among people with dementia living in LTC settings.
AAL technologies addressing loneliness as a primary outcome
In a study from New Zealand, PARO—a therapeutic companion robotic seal—was tested in non-facilitated group interactions; the results of these interactions were compared with those of semi-structured group interactions with residents without a robot intervention [Citation29,Citation30]. This was the only study included in our review in which loneliness was directly targeted for intervention using AAL technology. This study reported that the use of PARO significantly improved loneliness in people with dementia living in LTC as measured by the UCLA Loneliness Scale [Citation54]. Comparing PARO interactions to group interactions, PARO had no significant effect on QoL and depression [Citation29]. Most participants chose to actively engage with PARO, speaking to it, touching it, and talking about it to others. Of the 20 participants initially involved in the study, six refused to engage with the robot to any significant degree; they thought the robot was a “silly toy” and did not wish to play with PARO or quickly lost interest in it. Those who did not want to interact with the robotic animal did not receive some of the benefits that the other participants reported, such as comfort and relaxation from patting it, yet they may still have benefitted from increased social contact with other residents [Citation29,Citation30].
Family members were particularly interested in the benefits of PARO for emotional and social engagement and a reduction in loneliness. Additionally, family members mentioned that it did not seem to matter whether the robot was a seal or a dog, as long as the resident perceived it to be real [Citation30,Citation31]. Families were keen on the idea of their relatives using a social robot that moved and engaged with them, perceiving it to improve mood, reduce agitation, and provide comfort and opportunity for communication for their relatives [Citation30,Citation31].
AAL technologies that are promising in providing psychosocial interventions to impact loneliness
Based on the AAL technologies evaluated in the 24 included studies, we defined three categories of activities: (a) communication and interaction with social robots, including the activities in the aforementioned PARO study [Citation29]; (b) robotic pet therapy; and (c) leisure and creative activities. AAL technologies were tested in either individual or group interactions, with or without facilitation, and in a structured or non-structured way. Except for the study of Robinson et al., the studies did not directly aim to impact loneliness (not defined it as an outcome), but we determined that there is potential for these AAL technologies to deliver psychosocial interventions targeting loneliness.
Communication and interaction with social robots
Ten of the 18 studies on robotics investigated PARO, an interactive baby seal robot. The remaining three studies on robotics examined (1) “Giraff”, a telepresence robot facilitating video conferencing between a person with cognitive impairment and his or her family; (2) a teddy bear robot called CuDDler; and (3) two humanoid robots, “Sophie” and “Jack”, used to facilitate leisure activities.
In a randomized control trial (RCT) from Australia, PARO was incorporated in daily activities as a therapeutic companion robotic seal, and the PARO group was compared to an interactive reading group [Citation36]. The researchers found that PARO significantly impacted QoL, anxiety, and depression scores [Citation36]. In another study, Moyle et al. tested non-facilitated sessions with PARO in comparison to the use of a plush toy and to usual care [Citation39]. Video data showed that PARO was more effective than usual care in improving pleasure; however, PARO was no different than the plush animal in reducing neutral emotional affect. The group that interacted with PARO was significantly more verbally and visually engaged with PARO than the plush toy group was with the toy. On the other hand, comparing PARO interactions and the use of the plush toy with usual care, the researchers observed increased levels of anger in the PARO and plush toy groups. Video data analysis indicated that the observed anger was not directed at PARO or the plush toy but was due to various reasons in a small group of participants (e.g., PARO or the plush toy interrupted their current activity). Although significantly more effective than usual care, PARO was found to have a similar effect on mood and agitation as plush animals. Compared with usual care, PARO demonstrated effectiveness in reducing agitated behaviour, but this effect was not observed when measured with a standard scale, such as the Cohen-Mansfield Agitation Inventory (CMAI) [Citation39].
In another study evaluating the effect of PARO on mood and pain perception in people with dementia [Citation40], the participants had positive attitudes towards PARO and acknowledged the therapeutic benefits of PARO on mood improvement and pain relief. Staff members mentioned the limitations of PARO regarding its weight, voice, and characteristics [Citation40]. Takayanagi et al. tested PARO in individual, non-structured interactions with residents [Citation47]. Compared with residents who interacted with a plush toy lion, residents in moderate and severe dementia groups who interacted with PARO had a greater frequency of talking to PARO, more often showed positive emotional expressions, and tended to laugh during their interactions with PARO [Citation47].
Another robot, Giraff, a telepresence robot, was tested in structured video calls between families and people with dementia in LTC [Citation33]. Giraff was found to be acceptable and feasible for implementation within LTC facilities and to be able to engage families and people with dementia [Citation33]. Giraff was viewed positively by families regarding its ability to provide an enhanced alternative to phone talks and to facilitate conversations with persons with reduced verbal communication skills [Citation33].
CuDDler, an interactive robotic teddy bear, was tested in engagement activities supported by a facilitator to identify its effect on agitation [Citation38]. The researchers found that CuDDler significantly increased joy and improved engagement in people with dementia. Although the CMAI scores indicated slightly increased agitation, the participants seemed to interact more and even reminisce about previous pets [Citation38]. While CuDDler had differing effects, such as frustration or affection, among five participants, it was also clear that CuDDler provided the opportunity for the participants to engage in social interaction. Even when CuDDler had technical problems, such as being slow to react, the participants continued to speak to CuDDler and/or the facilitator. Therefore, CuDDler provided a platform for social interaction; however, over time, the facilitator became the source of engagement [Citation38]. Another study found that people with dementia had positive interactions with the humanoid robots “Sophie” and “Jack”, which were designed to increase interaction and communication, leading to an improvement in their social capabilities, such as engagement in group activities [Citation46].
Robotic animals utilized to provide pet therapy
Three studies investigated robotic animals, i.e., (1) a robot dog, AIBO; (2) a robot cat, JustoCat; and (3) a pair of unnamed cat and dog robots in providing pet therapy. Robotic animals have been reported to be a promising alternative to therapy with live pets [Citation36]. Interacting with robotic animals seems to improve communication and interaction and reduce stress responses and medication use in people with dementia. Despite their cognitive decline, they talked about previous pets and asked questions, complemented, and talked directly to the robotic dog-related stimuli, with the majority of their verbalizations being appropriate for the situation. In another study, both a real dog and a robot dog were received positively by residents with dementia; however, they engaged longer with the live dog than the robot dog [Citation50]. Although the three real dogs evoked the highest number of spoken comments by the residents, the residents also made comments about the robotic dog and the puppy video. In contrast, the study participants in the control group made only a few comments [Citation50]. On the contrary, in the study with AIBO, the robotic dog, participants were more interested in the robotic dog than a real dog [Citation45].
The JustoCat intervention resulted in positive effects, including increased interaction, communication, stimulation, relaxation, peace, and comfort, for individuals with dementia [Citation37]. JustoCat improved QoL for persons with dementia in LTC [Citation37]. While the robot increased agitation scores for most residents with dementia in LTC [Citation37], interestingly, a professional caregiver interpreted increased this agitation to be a positive sign, with higher scores viewed as awakening moments in the residents’ otherwise introverted lives [Citation37].
Robotic pets were found to be acceptable in the LTC environment, as an alternative in the face of a range of constraints, such as hygiene and phobias [Citation35]. Furthermore, robotic animals were able to support conversation with a resident with dementia by providing a common focus of interest to talk about [Citation35,Citation38,Citation45].
Leisure and creative activities via multimedia computer systems
In this scoping review, five multimedia computer systems providing leisure and/or creative activities were identified: (1) CIRCA, a multimedia touchscreen computer system comprising different content categories, such as photographs, music, and videos [Citation43,Citation49]; (2) The Chitchatters (CC), a technology-based leisure activity using a radio, television, telephone and treasure box [Citation44]; (3) Digital Life Storybooks, a software program used in the dyadic approach to create a video of an individual’s life for reminiscence therapy [Citation34]; (4) VENSTER, an interactive touch screen art installation [Citation48]; and (5) Nintendo Wii, a gaming console that can be used for well-being activities [Citation32].
CIRCA was studied regarding its impact on engagement [Citation43]. It was found that even when professional caregivers used the touchscreen, their actions and the response of the system helped persons with dementia remain engaged and focussed on the task [Citation49]. The results from this study suggested that the dyads of professional caregivers and persons with dementia were able to establish joint attention much more easily in the CIRCA sessions than in traditional reminiscence sessions, which failed to achieve joint attention at all [Citation43]. CIRCA was shown to be able to partially restore the ability of a resident with dementia to carry out a satisfying conversation with a relative, caregiver, or friend [Citation49]. All participating caregivers positively reported their experience with CIRCA and its ease of use [Citation49]. In comparison to traditional reminiscence sessions, CIRCA also appeared to support relationships between caregivers and people with dementia by scaffolding a conversation [Citation43].
In a study investigating the effect of CC on social behaviour, the frequencies of “comments” and “talking to oneself” significantly increased [Citation44]. CC could stimulate communication and empathy, which Nijhof et al. interpreted as an indicator of improved well-being [Citation44].
Digital Life Storybooks was used in The Life Storybook Study [Citation34] to deliver reminiscence therapy; the study showed that compared to the participants who used conventional life storybooks, most participants who used Digital Life Storybooks improved their QoL and autobiographical memory. All participants showed improvement or stability in their depression scores. Digital Life Storybooks were considered a tangible aid with therapeutic value to residents living with dementia [Citation34]. Multiple case studies showed that in all but one instance, Digital Life Storybooks was linked to significantly increased QoL [Citation34].
VENSTER elicited a range of responses, from verbal reactions to active physical engagement, and thus illustrated the potential of interactive artwork within reminiscence therapy in the LTC environment [Citation48]. The research found that content that triggered memories or recognition helped initiate a conversation [Citation48]. Incomplete memory or recognition prompted residents to ask others, mostly care providers, for more information or confirmation. VENSTER encouraged participants to reminisce and interact with staff [Citation48]. By providing an interesting topic to talk about, it triggered social interaction [Citation48].
Nintendo Wii is a gaming console system used with residents with dementia living in LTC facilities primarily for physical fitness [Citation32]. The system proved feasible for use in supervised physical training sessions for various groups of older adults aged 62–89 with or without dementia and with or without physical impairment [Citation32]. Researchers measured social interaction by background and participatory observations. Later in semi-structured group interviews, participants remarked that they talked, laughed, and cheered for each other during the exercises [Citation32]. Participants with dementia found the experience to be socially engaging since it facilitated social interaction. However, the competition created motivation and demotivation when participants had to disclose their weight and age for the game. Interaction with the game resulted in more endurance and a generally positive trend in physical improvement for the participants while they engaged in the game [Citation32].
Reviews included
Four reviews were included in our scoping review.
The key finding of Neal et al. was that the potential of technology to impact meaningful engagement did not lie in the technologies used in the studies themselves but rather in the opportunities the technologies provided to facilitate connection and belonging [Citation51].
Pu et al. evaluated the role of robots in the context of agitation and dementia [Citation42]. They identified two categories of robotics: social robots and robotic animals. No significant effect of social robots on agitation was found [Citation42].
Bemelmans et al. also investigated two types of robotics with the same categorization, within a non-dementia-specific review: social robots and robotic animals [Citation41]. They reported that the generally positive effects reported indicating the need for further research into the effects and potential use of socially assistive robotics in older adult care, as the methodological quality of the studies included in their review was low. Furthermore, they stated that outcomes linked to loneliness were not investigated as the main outcome in the included studies [Citation41].
Moyle et al. investigated telepresence robots and found that all reviewed studies reported positive aspects of the use of videoconferencing to facilitate the social connection between persons with dementia and their family and friends [Citation52]. They further speculated that the benefits of telepresence systems are expected to outweigh any technical issues [Citation52]. On the other hand, staff and relatives considered the guide robot to be too complicated for people with dementia to use, particularly for those with language impairments. Participants positively regarded the CompanionAble robot, specifically its movement and location of the user, which was similar for Giraff. However, in general, telepresence robots were considered expensive in all studies, despite their significant benefits for persons with dementia since they did not have to learn specific skills to use them [Citation52].
Discussion
This scoping review, to the best of our knowledge, is the first to investigate the potential impact of assistive technologies providing psychosocial interventions on loneliness in older adults with dementia in LTC. Most of the social robot studies (n = 9 out of 15) were conducted in Australia or New Zealand, whereas all multimedia systems studies were conducted in Europe (n = 6). This finding opens the way to be interpreted as a difference between the understandings and preferences of care technologies among countries.
The focus of our review was on alleviating loneliness; however, only one paper [Citation29] out of 24 papers was identified that directly aimed to address loneliness, revealing a shortage of research on this topic. Most studies reported varying degrees of positive impacts of the studied technologies; however, most studies either did not measure loneliness explicitly or measured it only in a limited capacity. Of the studies that measured behaviours (e.g., participating in social activities with AAL technologies), five used standard measurement tools, most of which were developed by researchers.
Communication and interaction through robotic animals, such as PARO and JustoCat have been shown to have the potential to improve QoL for people with dementia [Citation36,Citation37], but with mixed results [Citation29]. Beridze et al. showed that loneliness and social isolation are associated with QoL but that the association is context-dependent (e.g., variation in QoL based on where people with dementia live) [Citation55]. Thus, interventions aiming to influence QoL can be seen as interventions with the potential to alleviate loneliness. Interaction with robotic animals, such as PARO, AIBO, and CuDDler improves engagement and communication [Citation38,Citation39,Citation50], which holds the potential to reduce loneliness in people with dementia. The results suggest that residents with advanced dementia might benefit more from a PARO intervention than from the use of other robots. This finding might be taken with a grain of salt because PARO is the most researched robotic animal within the scope of this review. However, barriers were also found in the use of PARO, e.g., cost and workload, infection concerns, and stigma and ethical issues [Citation56]. Hung et al. concluded in their scoping review that future research should focus on how to overcome barriers to the adoption of PARO [Citation56].
A bioethics committee in Austria expressed ethical concerns regarding the design of robots, such as which aspects of human life can be robotized and whether social robots enable older adults to retain their skills and avoid potential deception and infantilization in people with dementia [Citation57]. Hung et al. also raised the concern that the use of social robots could lead to infantilizing and dehumanizing care [Citation56]. Furthermore, a “mismatch between needs and solutions offered by the robot, usability, and lack of experience with technology, was seen as the most important barriers for social robot adoption” [Citation58].
Our review indicated that telepresence robots are regarded positively by residents with dementia, staff, and family members as they provide an enhanced alternative to phone conversations. People with dementia valued the self-initiating function of telepresence robots, while families enjoyed the ability to carry on a conversation with residents with reduced verbal communication skills, in particular when families could not visit in person. During the COVID-19 pandemic, it became evident that “social isolation is detrimental on not only an emotional and psychosocial level, but may also cause long-lasting cognitive damage” [Citation59]. Thus, increased use of tele-video conferences was observed to alleviate loneliness in residents with dementia [Citation59].
All robotic animals facilitated better communication, and therefore, they may contribute to an effect on loneliness. In most studies, robotic animals, such as AIBO, PARO, and JustoCat were regarded usable and considered as an alternative to living animals for pet therapy [Citation35–37,Citation50]. Robotic animals also provided the opportunity for people to reminiscence their previous pets, and they gave people with dementia comfort and reduces their anxiety [Citation31]. Furthermore, some studies reported a sense of responsibility that robotic animals inspired in residents, providing another reason to interact with others, e.g., ask how to feed the puppy [Citation30]. However, research also indicated aspects of aversion [Citation30] and feelings of infantilization [Citation38] in regard to robotic animal interventions. The findings suggest that the potential of technology to impact loneliness lies mostly in the perceptions of people with dementia and how they can relate to those perceptions. Mordoch et al. concluded in their literature review that pet robots “affect regulation, social interactions, and decreases in psychological stress reactions” [Citation60].
In one study, the robotic animal intervention generated more pleasure and joy for some participants than any individual or group activity ever did in the participating LTC facility [Citation38]. In some cases, residents felt anxious and misunderstood when surrounded by people but exhibited a very positive response to social robots [Citation38]. It can be suggested that social robots in the LTC environment have the potential to alleviate loneliness by facilitating interaction with other residents, providing company for residents when they feel down, and providing an opportunity for staff to better communicate with residents [Citation29]. Whelan et al. concluded in their literature review that acceptability can be improved with humanlike communication, personalized responses to users, and addressing issues of trust and control of the robot [Citation61].
Multimedia computer systems were found to improve engagement and communication [Citation32,Citation43,Citation49]. Multimedia computer systems acted as cognitive prosthetics to aid people with dementia in carrying out conversations [Citation49]. Nintendo Wii facilitated social engagement and, despite physical and technical limitations, people with dementia were able to use the technology and improve their physical fitness [Citation32]. Li et al. concluded in their systematic review that in general, exergames can enhance social well-being and reduce loneliness; unfortunately, persons with dementia have often been excluded from these studies. We, therefore, assume that more research is needed to understand the impact of multimedia computer systems on persons with dementia [Citation62].
Robotic animals allow residents with dementia to reminisce about their previous pets, and they thus bring joy and pleasure beyond improved social engagement. Telepresence robots bring a face to a phone conversation, making it easier for families to communicate with their relatives and impacting well-being.
Similar to a previous review [Citation51], our review showed that AAL technology holds the potential to impact loneliness by facilitating social interaction. However, there is a need to clarify the terms relating to loneliness and social isolation [Citation6].
Strengths and limitations of the review
This scoping review was conducted in line with recognized methods [Citation26]. Although efforts were made to minimize the likelihood of overlooking potentially relevant studies, there is the possibility that the search terms and eligibility criteria did not capture the extent of the research available. However, the examination of MeSH headings, review of recent reviews on similar topic areas, and hand-searching of reference lists reduced this likelihood. Another limitation is that our scoping review did not include a detailed critical appraisal of the included studies, as this was not our purpose. The aim was to summarise the current evidence on a topic and provide future directions for research.
Conclusions
The current review showed that loneliness is seldom studied as a primary outcome measure of psychosocial interventions delivered via AAL technologies for people with dementia in LTC. Despite the limitations of this review, we conclude that assistive technologies hold the potential to impact loneliness in people with dementia. AAL technologies have been shown to have positive effects, such as improvement in social engagement and the potential to impact loneliness in residents with dementia living in LTC. From the results of our scoping review, it can be concluded that these AAL technologies can improve the general well-being of residents with dementia and enhance communication with others.
Implications for future research
This study suggests the need for further research on the effect of AAL technologies on loneliness compared to that of traditional psychosocial interventions, such as (living) pet therapy. Research has identified the need for effective comparison of interventions with assistive technologies to traditional interventions. Additionally, the working mechanism of the potential effect of assistive technologies on loneliness needs to be analyzed. More consistency in the measurement of behavioural outcomes related to loneliness is needed. Finally, the effectiveness of telepresence robots and PARO needs to be further investigated to determine whether connecting people with dementia to their loved ones or supporting interaction with others in facilities better alleviates loneliness.
Author contributions
All authors were involved in designing the review. B.B. conducted the literature search, data collection, and extraction. B.B., G.A., and V.H. conducted Ti/Ab screening and data extraction. B.B. primarily wrote the paper. M.R., F.L.U., and F.M. supervised the whole process. S.T. and S.F. contributed to the development of the search strategy.
Disclosure statement
The authors have no conflict of interest to declare.
Additional information
Funding
References
- Freedman A, Nicolle J. Social isolation and loneliness: the new geriatric giants. Can Fam Physician. 2020;66(3):176–182.
- Chen Y-RR, Schulz PJ. The effect of information communication technology interventions on reducing social isolation in the elderly: a systematic review. J Med Internet Res. 2016;18(1):e18.
- Ernst JM, Cacioppo JT. Lonely hearts: psychological perspectives on loneliness. Appl Prev Psychol. 1999;8(1):1–22.
- Golden J, Conroy RM, Bruce I, et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int J Geriatr Psychiatry. 2009;24(7):694–700.
- Gardiner C, Laud P, Heaton T, et al. What is the prevalence of loneliness amongst older people living in residential and nursing care homes? A systematic review and meta-analysis. Age Ageing. 2020;49(5):748–757.
- Prohaska T, Burholt V, Burns A, et al. Consensus statement: loneliness in older adults, the 21st century social determinant of health? BMJ Open. 2020;10(8):e034967.
- Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50(1):31–48.
- Jaremka LM, Fagundes CP, Glaser R, et al. Loneliness predicts pain, depression, and fatigue: understanding the role of immune dysregulation. Psychoneuroendocrinology. 2013;38(8):1310–1317.
- Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol. 2009;28(3):354–363.
- Steptoe A, Shankar A, Demakakos P, et al. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013;110(15):5797–5801.
- Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237.
- Sutin AR, Stephan Y, Luchetti M, et al. Loneliness and risk of dementia. J Gerontol B Psychol Sci Soc Sci. 2020;75(7):1414–1422.
- Donovan NJ, Okereke OI, Vannini P, et al. Association of higher cortical amyloid burden with loneliness in cognitively normal older adults. JAMA Psychiatry. 2016;73(12):1230–1237.
- Tilvis RS, Kähönen-Väre MH, Jolkkonen J, et al. Predictors of cognitive decline and mortality of aged people over a 10-year period. J Gerontol. 2004;59(3):268–274.
- Sury L, Burns K, Brodaty H. Moving in: adjustment of people living with dementia going into a nursing home and their families. Int Psychogeriatr. 2013;25(6):867–876.
- Tsai HH, Cheng CY, Shieh WY, et al. Effects of a smartphone-based videoconferencing program for older nursing home residents on depression, loneliness, and quality of life: a quasi-experimental study. BMC Geriatr. 2020;20(1):27.
- Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health. 2020;20(1):129.
- Moniz-Cook E, Vernooij-Dassen M, Woods B, et al. Psychosocial interventions in dementia care research: the INTERDEM manifesto. Aging Ment Health. 2011;15(3):283–290.
- van Mierlo LD, Dröes RM, Meiland FJM, et al. Personalized psychosocial interventions in dementia care: evaluation and implementation. Amsterdam: Vrije Universiteit Amsterdam; 2015.
- Akhter-Khan SC, Au R. Why loneliness interventions are unsuccessful: a call for precision health. Adv Geriatr Med Res. 2020;2(3):e200016.
- Asghar I, Cang S, Yu H. Assistive technology for people with dementia: an overview and bibliometric study. Health Info Libr J. 2017;34(1):5–19.
- Meiland F, Innes A, Mountain G, et al. Technologies to support community-dwelling persons with dementia: a position paper on issues regarding development, usability, effectiveness and cost-effectiveness, deployment, and ethics. JMIR Rehabil Assist Technol. 2017;4(1):e1.
- Ienca M, Fabrice J, Elger B, et al. Intelligent assistive technology for Alzheimer's disease and other dementias: a systematic review. J Alzheimers Dis. 2017;56(4):1301–1340.
- Bennett B, McDonald F, Beattie E, et al. Assistive technologies for people with dementia: ethical considerations. Bull World Health Organ. 2017;95(11):749–755.
- Lorenz K, Freddolino PP, Comas-Herrera A, et al. Technology-based tools and services for people with dementia and carers: mapping technology onto the dementia care pathway. Dementia. 2019;18(2):725–741.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
- The EndNote Team. EndNote. EndNote X9 ed. Philadelphia (PA): Clarivate; 2013.
- Covidence systematic review software. Melbourne: Veritas Health Innovation; 2019.
- Robinson H, Macdonald B, Kerse N, et al. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14(9):661–667.
- Robinson H, Broadbent E, MacDonald B. Group sessions with Paro in a nursing home: structure, observations and interviews. Australas J Ageing. 2016;35(2):106–112.
- Moyle W, Bramble M, Jones CJ, et al. “She had a smile on her face as wide as the great Australian bite”: a qualitative examination of family perceptions of a therapeutic robot and a plush toy. Gerontologist. 2019;59(1):177–185.
- Aarhus R, Grönvall E, Larsen SB, et al. Turning training into play: embodied gaming, seniors, physical training and motivation. Gerontechnology. 2011;10(2):110–119.
- Moyle W, Jones C, Cooke M, et al. Connecting the person with dementia and family: a feasibility study of a telepresence robot. BMC Geriatr. 2014;14(1):7.
- Subramaniam P, Woods B. Digital life storybooks for people with dementia living in care homes: an evaluation. Clin Interv Aging. 2016;11:1263–1276.
- Campbell A. Dementia care: could animal robots benefit residents? Nursing and Residential Care. 2011;13(12):602–604.
- Moyle W, Cooke M, Beattie E, et al. Exploring the effect of companion robots on emotional expression in older adults with dementia: a pilot randomized controlled trial. J Gerontol Nurs. 2013;39(5):46–53.
- Gustafsson C, Svanberg C, Mullersdorf M. Using a robotic cat in dementia care: a pilot study. J Gerontol Nurs. 2015;41(10):46–56.
- Moyle W, Jones C, Sung B, et al. What effect does an animal robot called CuDDler have on the engagement and emotional response of older people with dementia? A pilot feasibility study. Int J Soc Robot. 2016;8(1):145–156.
- Moyle W, Jones CJ, Murfield JE, et al. Use of a robotic seal as a therapeutic tool to improve dementia symptoms: a cluster-randomized controlled trial. J Am Med Dir Assoc. 2017;18(9):766–773.
- Pu L, Moyle W, Jones C. How people with dementia perceive a therapeutic robot called Paro in relation to their pain and mood: a qualitative study. J Clin Nurs. 2020;29(3–4):437–446.
- Bemelmans R, Gelderblom GJ, Jonker P, et al. Socially assistive robots in elderly care: a systematic review into effects and effectiveness. J Am Med Dir Assoc. 2012;13(2):114–120.e1.
- Pu L, Moyle W, Jones C, et al. The effectiveness of social robots for older adults: a systematic review and meta-analysis of randomized controlled studies. Gerontologist. 2019;59(1):e37–e51.
- Astell AJ, Ellis MP, Bernardi L, et al. Using a touch screen computer to support relationships between people with dementia and caregivers. Interact Comput. 2010;22(4):267–275.
- Nijhof N, van Hoof J, van Rijn H, et al. The behavioral outcomes of a technology-supported leisure activity in people with dementia. TAD. 2013;25(4):263–273.
- Kramer SC, Friedmann E, Bernstein PL. Comparison of the effect of human interaction, animal-assisted therapy, and AIBO-assisted therapy on long-term care residents with dementia. Anthrozoös. 2009;22(1):43–57.
- Chu M-T, Khosla R, Khaksar SMS, et al. Service innovation through social robot engagement to improve dementia care quality. Assist Technol. 2017;29(1):8–18.
- Takayanagi K, Kirita T, Shibata T. Comparison of verbal and emotional responses of elderly people with mild/moderate dementia and those with severe dementia in responses to seal robot, Paro. Front Aging Neurosci. 2014;6:257.
- Luyten T, Braun S, Jamin G, et al. How nursing home residents with dementia respond to the interactive art installation ‘VENSTER’: a pilot study. Disabil Rehabil Assist Technol. 2018;13(1):87–94.
- Alm N, Dye R, Gowans G, et al. A communication support system for older people with dementia. IEEE Comput. 2007;40(5):35–41.
- Marx MS, Cohen-Mansfield J, Regier NG, et al. The impact of different dog-related stimuli on engagement of persons with dementia. Am J Alzheimers Dis Other Demen. 2010;25(1):37–45.
- Neal I, Du Toit SH, Lovarini M. The use of technology to promote meaningful engagement for adults with dementia in residential aged care: a scoping review. Int Psychogeriatr. 2020;32(8):913–923.
- Moyle W, Arnautovska U, Ownsworth T, et al. Potential of telepresence robots to enhance social connectedness in older adults with dementia: an integrative review of feasibility. Int Psychogeriatr. 2017;29(12):1951–1964.
- Bemelmans R, Gelderblom GJ, Jonker P, et al. How to use robot interventions in intramural psychogeriatric care; a feasibility study. Appl Nurs Res. 2016;30:154–157.
- Russell DW. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40.
- Beridze G, Ayala A, Ribeiro O, et al. Are loneliness and social isolation associated with quality of life in older adults? Insights from northern and southern Europe. Int J Environ Res Public Health. 2020;17(22):8637.
- Hung L, Liu C, Woldum E, et al. The benefits of and barriers to using a social robot Paro in care settings: a scoping review. BMC Geriatr. 2019;19(1):232.
- Bioethics Commission. Robots in the care of older people. Vienna: Federal Chancellery Republic of Austria; 2018.
- Pino M, Boulay M, Jouen F, et al. Are we ready for robots that care for us?” attitudes and opinions of older adults toward socially assistive robots. Front Aging Neurosci. 2015;7:141.
- Donovan NJ, Blazer D. Social isolation and loneliness in older adults: review and commentary of a national academies report. Am J Geriatr Psychiatry. 2020;28(12):1233–1244.
- Mordoch E, Osterreicher A, Guse L, et al. Use of social commitment robots in the care of elderly people with dementia: a literature review. Maturitas. 2013;74(1):14–20.
- Whelan S, Murphy K, Barrett E, et al. Factors affecting the acceptability of social robots by older adults including people with dementia or cognitive impairment: a literature review. Int J Soc Robot. 2018;10(5):643–668.
- Li J, Erdt M, Chen L, et al. The social effects of exergames on older adults: systematic review and metric analysis. J Med Internet Res. 2018;20(6):e10486.