ABSTRACT
In this editorial we try to summarise how we, in 2021, understand mental disorders in general, and psychoses in particular. We have tried to write it in a language that is understandable for our readers, including patients, relatives, students and professionals, without reducing its scientific validity or basis. During the last decade we have gained new insight in these disorders, and most textbooks are outdated and convey an old-fashioned understanding of the causes, the possible courses and the treatments needed for serious mental suffering.
Editor’s note:
Dr Jan Olav was President of ISPS from 2001 to 2006 and 2015 to 2019, and President of the Norwegian Psychiatic Association from 2006 to 2011. He is an Assoicate Editor of this journal. In this Editorial he, and his esteemed colleague for many years at Stavanger University Hospital, Dr Inge Joa, present their own perspectives, via a Norwegian lens, of developments in how psychosis should be understood and responded to.
Introduction
The past decade has seen a significant development in our understanding of psychosis. We have come to recognize a clearer logic in the development of mental disorders through stages and phases, and we understand better how mental disorders develop gradually, and as a result of perceived stress. We have gained new knowledge about stress reactions, mental and physical, and we now understand more our mental experiences as internal imprints of external events. We further understand how the stress and immune systems interrelate, as a result of external stresses and life events, both in the past and present
And how we understand mental illness is crucial for how clinical services are designed, what content they provide, and what treatment approaches we give priority to. This understanding has varied throughout history; the two extremes are those who understand mental illness as exclusively environmental and those who, on the other hand, understand mental illness as biological hereditary diseases in line with many somatic disorders. If one considers psychosis as a biological disorder, where the psychosis breakthrough is almost inevitable, in line with, for instance, Chorea Huntington, the emphasis will be on biological treatment approaches and care. If, however, one considers mental illness and psychotic disorders to be linked to environmental factors, the emphasis will be on correction of the external environment, relational aspects and prevention.
In the 40s through the 60s, our understanding was way over on the environmental side, while the pendulum swung over into a biological understanding in the 70s and into the 90s. In the 2000s, the pendulum swung back again, much thanks to new research and knowledge about epidemiology, psychological trauma, genes and epigenetics.
The breakthrough in epigenetics, the understanding that gene expression is also influenced by the environment, by human experiences, has been crucial for modern understanding of causation in mental disorders. We furthermore know that the epigenetic development works over several generations (Jiang et al., Citation2019).
Moreover, it seems that the significance of the genetic risk is much less than we previously assumed, perhaps as little as 5–6% of the risk (Bassett et al., Citation2017; Goes & Sawa, Citation2017) .
Leboyer & Schurhoff (Citation2014) state in an article in the Schizophrenia Bulletin: “Until very recently, schizophrenia and bipolar disorder have been conceived as two separate conditions. This distinction is still taught in medical and graduate studies, is maintained in diagnostic classifications, and relied upon by regulatory bodies, drug companies, researchers, clinical care and research funding agencies, and advocacy groups. Psychiatrists know that between these diagnostic entities, there are not only symptom, diagnostic, and treatment overlap, but also shared genetic and environmental risk factors”.
So, many of the genetic findings to overlap between different mental disorders, suggesting that there may be a relatively large element of common underlying causes
We now know that we are actually treating mental states, transient states with changing signs and symptoms. No human fits fully into a particular diagnosis; we warn against “silo thinking” and now view mental disorders more and more in a transdiagnostic perspective.
In the following, we will present a modern understanding of psychosis, where much of this has not yet been included into present day textbooks, based on a dimensional understanding of what mental disorders really are.
What studies of the incidence of mental illness reveals
Psychotic disorders involve a major burden of stress for those affected and for their families. Overall, neuropsychiatric disorders were accounted as the main cause of burden in high-income countries, especially in those aged 15–24 years (Gore et al., Citation2011). Psychotic disorders, moreover, have a pronounced socio-economic significance. This has to do with the fact that the disorders start early, sometimes last a long time, and sometimes involve a long-term loss of function. 75% of all diagnosed mental disorders start before the age of 25 (Kessler et al., Citation2007), of which most people are diagnosed with mental disorders at the age of 20. Prior to this, those who develop more severe mental disorders such as major depression, bipolar disorder, anorexia and non-affective psychoses will have had symptoms such as anxiety, depression and concentration problems, for perhaps as much as up to 5 years. 50% of all mental health problems are established at the age of 14 years. Anxiety disorders are nowadays often referred to as “a gateway disorder” for other, more serious disorders (Ginsburg et al., Citation2014)
Most textbooks still state that the incidence of psychotic disorders are fairly stable and similar throughout the world. This is not the case. There is a huge variation in the incidence of psychosis between different geographical areas, including the most serious diagnosis, schizophrenia. A multi-centre study published in 2018 (Jongsma et al., Citation2018) found a 10-fold variation in the crude incidence of first episode psychosis (FEP) between different countries, and within different countries. A Danish study showed a significant incidence increase by 1.4 of non-affective psychosis (f20-f29) from 2000–2012, and a two-fold incidence increase for women age 19–24 (F20) (Kühl et al., Citation2016). Another, recently published register-study (Christensen et al., Citation2021) from Denmark shows the same development, with significant incidence increases for schizophrenia spectrum disorders, bipolar affective disorders and recurrent depression in the years 2000–2013.
So what is psychosis?
Psychosis essentially signifies a serious mental breakdown. In Norwegian, we would call psychosis a state of confusion, where mental and emotional chaos has arisen, and where the most important characteristic is a reduced ability or inability to distinguish between oneself and the reality around oneself.
Mental disorders develop in phases
The severe psychoses are considered to be dynamic processes that develop in phases. In modern research and clinical practice, it will be crucial to define which phase one is facing in the psychotic disorder. Considering mental disorders as disorders with a significant overlap between the different diagnostic groups is, as previously mentioned, is called a dimensional perspective. This is in contrast to the so-called categorical perspective, where the various diagnostic categories are regarded as separate states with separate, and more biological, causal relationships (Bentall, Citation1993).
Over the past few years, we have gained more knowledge about neurophysiology, neuropsychological mechanisms and neuroimmunology. This knowledge leads us on the trail of important etiological factors, such as unfortunate life events, traumas etc., and indicates that the existing diagnostic categories may be an obstacle to developing a more comprehensive and integrated understanding of mental ill health. Based on this recognition, an alternative approach to the conceptualization of mental disorders, called The Research Domain Criteria (RDoC) (Insel et al., Citation2010), has been developed in the United States. The RDoC matrix was developed by The National Institute of Mental Health (NIMH) and represents a radical break, almost a paradigm shift, with existing research categories within mental health. The following factors are central to the model: first, dimensions are emphasized by the description of symptoms and personality, not categories. Secondly, one does not start with existing diagnoses – the starting point should be connections between neurobiology and behaviour, which can then be linked to clinical phenomena. Thirdly, attempts have been made to define models (constructions), such as fear, loss, perception and cognition. McGorry et al have emphasized the importance of the timing of initiating treatment versus diagnostic specificity. They have proposed a clinical staging model describing the various dimensions and development of possible psychopathology and prevention aspects (McGorry et al., Citation2006).
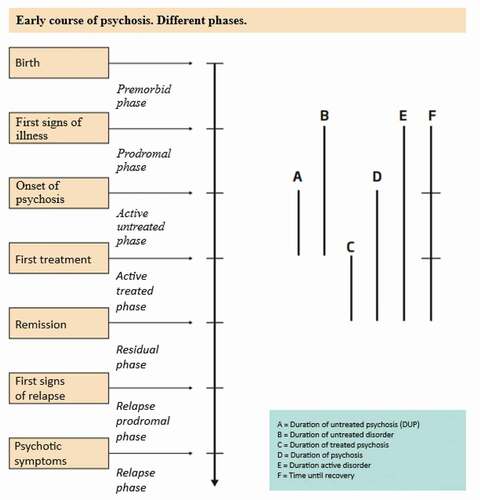
In below, attempts have been made to illustrate the various phases of disorder development. The premorbid phase means the phase before the disorder itself breaks out, prodromal means “warning phase”, and means that one may spot the first signs of illness, though then most often as non-specific signs (e.g. anxiety symptoms and symptoms of depression). The psychosis phase will be discussed in detail later, the most important sign in this phase is an impaired reality-testing ability (sense of reality).
about here
As the figure (McGlashan & Johannessen, Citation1996) shows, we talk about an “active untreated phase” and about the “duration of untreated disorder”. These are phases that should be as short as possible.
The stress-vulnerability model
This model integrates various psychological models with possible biological explanatory models for vulnerability to developing psychosis (Zubin & Spring, Citation1977). A low threshold for psychotic breakdown may be due to either biological or psychological conditions, or both at the same time. The proposed traumagenic neurodevelopmental model may be a good example of integrating bio and psycho-social mechanisms (Read et al., Citation2014).
Various risk factors related to heredity and the environment are the subject of extensive research and include genetic and other biological markers, conditions during pregnancy, birth, childhood, and conditions of physical and psychological nature. It is now apparent that environmental factors are important. Both growing up in big cities, migration, drug use and adverse life events, including trauma, are risk factors for psychosis (A. Morrison et al., Citation2005; Read et al., Citation2008).
No definite association has been found between the incidence of schizophrenia and social class, but the prognosis is worse for patients from lower social classes (Hastings et al., Citation2020; Anglin et al., Citation2021). Furthermore, poverty is a powerful predictor of who develops psychosis (Read, Citation2010). A poorer prognosis is probably due to the presence of several risk factors. There is a dose-response increased risk connected to child adversity events (Trauelsen et al., Citation2015).
Psychosis and stress
It is important to remember that we are talking about emotional, psychological problems in people, reactions that may affect anyone, if the pressure is great enough. When emotions overwhelm us, so that our psychological coping apparatus breaks down, we can all expereince this breakdown called psychosis.
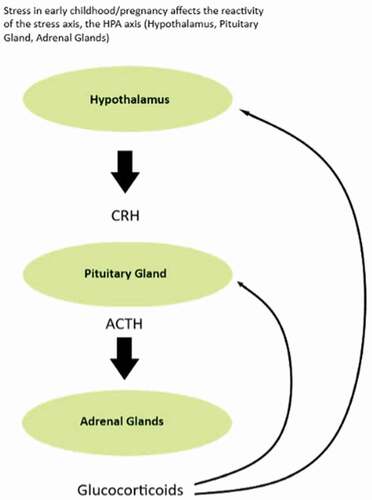
Our ability to withstand different types of stress in adolescence and early adulthood varies. The stress systems in the body are largely hormonal, and the reactivity in our stress axis is affected by the stress we experience during pregnancy and the first years of life, . “Stress” actually means two things, an external pressure and the bodily reaction to this pressure. Stress in the form of childhood trauma has been shown to be associated with many different mental disorders, such as PTSD, sleep disorders, anxiety, depression, bipolar disorder, hallucinations, personality disorders, substance abuse, eating disorders and many more.
The term we use today to explain this increased vulnerability is “adverse life events”. Unfortunate life events embrace everything from pure bad luck and coincidences in life, to abuse and other detectable traumatic events (Varese et al., Citation2012).
Thus, we must never, in meeting with people diagnosed as having a mental illness, think in stereotypes. We must recognize each individual as unique, and in order to help, we must know the life of the other, perhaps better than they know it themselves. It is an essential part of the therapist’s task. We can all make use of an outside perspective on our lives, on our life history
Put another way: mental illness must begin somewhere, have a starting point. We are all different when it comes to the formation of our personality. We have, and develop, our strengths and weaknesses, and we are different in the way we manage stress.
Such a state of confusion does not arise from nothing or by itself. The confusion, or breakdown if you will, is almost always preceded by a shorter or longer period of time with general signs of mental issues, triggered by subjective stress experiences. The collapse is often preceded by sensory impressions being altered and amplified. Noises can become uncomfortably loud, the room feels smaller, etc. Most people will have experienced this at some point in their lives during particularly stressful periods.
Over time, the mental pressure can increase until we eventually experience a total breakdown, with confusion or psychosis as the next stage. Yet, what is stressful to you is not stressful to me, and vice versa, and how we deal with different types of stress depends on the individual’s personality and previous life experiences.
In November 2019 (Volume 213), an epoch-making edition of the highly renowned journal Schizophrenia Research was published, in which all the articles discussed the relationship between stress and psychosis: “Stress and Schizophrenia” This is fairly new knowledge, and these articles describe a paradigm shift in our understanding of severe mental illness, including psychotic disorders. In an article in this journal, “Advances in the Neurobiology of Stress and Psychosis”, Mittal and Walker (Citation2019) describe developments since the “Stress-Vulnerability Model” was introduced. They write:
“The central thesis of this article (Zubin & Spring, Citation1977) is that ““challenges elicit a crisis in all humans, but depending on the intensity of the elicited stress and the threshold for tolerating it, that is, one’s vulnerability, the crisis will either be contained homeostatically or lead to an episode of disorder”.. Then they add: “Assumptions about socioenvironmental and biological etiologic factors were no longer considered incompatible”.
They further write: “It is of interest that the following words did not appear in the article by Zubin and Spring: hypothalamus, pituitary gland, cortisol (or other hormones), HPA axis (stress axis), the brain, neurotransmitter. The absence of these concepts reflects our limited understanding of stress biology in 1977, and of the interaction between environment and biology in relation to the development of psychopathology. Since the 1970s, our scientific understanding of these conditions has increased dramatically” (Mittal & Walker, Citation2019).
Psychoimmunology: the psyche and the immune system
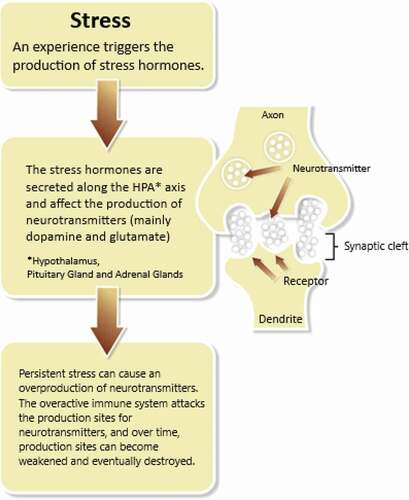
In the last 5 years, we have witnessed new, but not yet conclusive, research and knowledge about the immune system’s interaction with the stress axis and its role in relation to the brain’s neurotransmitters. Until quite recently, it was assumed that the various markers of the immune system did not cross the blood-brain barrier to any significant degree. This has now changed; we know that the immune system acts over the blood-brain barrier. We have tried to illustrate this in the figure above. A hypothesis that seems to be supported in recent research is that the immune system responds to the brain’s compensatory “overproduction” of neurotransmitters such as dopamine and glutamine in stress-related conditions such as psychosis, and that this is normalized when stress levels are lowered. If, on the other hand, stress levels remain high over time, it may appear that this reversal becomes more difficult, with the risk of more permanent changes in the brain’s synaptic systems. If this is the case, then this is another strong argument for early intervention in severe mental illness, and for “the inner being an imprint of the outer”, i.e. that life events leave an imprint in the body, including the brain. It then becomes crucial to reduce the stressors in young people’s lives when they develop psychotic, or psychotic, states (Calcia et al., Citation2016; Howes et al., Citation2016; Malmqvist et al., Citation2019; Pillinger et al., Citation2019)
The role of emotions, psychological coping apparatus and psychotic disorders
To understand what a mental disorder really is, one must have some knowledge of developmental psychology, i.e. how human psychological “apparatus” develops, and knowledge of the function of emotions, i.e. why humans are endowed with emotions, “the sensory apparatus of the soul”.
Feelings (emotions, temperament, affects) can be described both simply or in a more complex fashion. Some writers define 100 different emotional qualities; most still summarize the most important to be fear/anxiety, anger, sadness, joy and shame. It is important to understand that we have been given these feelings for a purpose, namely that they will help us manoeuvre through life, a life that will offer great joys and great sorrows. Emotions should help us in our mental and relational world. Anxiety should lead us to withdraw, anger to do something about a threatening situation, and while grief and sadness are feelings we would rather avoid, sometimes this is not possible. We call it the “adaptive” function of the emotions, i.e. that they should help us meet the changing challenges of life, functioning as a “thermometer of the soul”. The same goes for the phenomena of hallucinations, which present on a continuum where a substantial minority of otherwise normal individuals in the developed world report hearing voices to voices on a level reported by individuals diagnosed with psychosis (Romme & Escher, Citation1989). Richard Bentall addresses this when he claims that psychotic behavior is comprehensible and thus more obviously related to ordinary behaviors and experiences (Bentall, Citation1993).
But, in a complicated modern world, it is not as simple as just registering our emotions then following them blindly. We are tied up in relations, privately and professionally, and the feelings that should be of help can sometimes quickly become a burden. At this point, we move inwards into the area of neurosis, where most of us are. If the emotional tension increases, our psychological coping apparatus (psychological defence) may break down, and we may enter into a psychosis.
Development of psychological coping mechanisms
To understand how mental disorders arise and develop, one must also know a little about how human psychological coping mechanisms/psychological defence mechanisms/ resistance mechanisms arise and develop.
All human beings are by nature endowed with certain hereditary characteristics; we usually call them abilities and facilities. When we are born into the world, these abilities and faculties, in interaction with the environment we grow up in, will shape us as human beings and together cause us to become the unique individuals we later appear to be. It is impossible to ultimately distinguish between what is hereditary and what are environmental characteristics.
Around 20 years of age, our personality will be fairly formed. At this point, we emerge as the unique person we are, each with our own coping mechanisms. In a psychological sense, this is also called “the psychological defences”. When we are required to change, this defence will appear as a kind of psychological resistance. It is then important to remember that we acquired our coping mechanisms through a changeable childhood. These coping mechanisms will vary from person to person and may not be as well suited to the stresses we face later in life. In many ways, it is these coping mechanisms that establish the personality’s ability to cope with life stress, and to cope with life’s changing challenges.
Prevention
It is of utmost importance that people who develop, or are at risk of developing, a psychosis, are quickly examined and treated. The duration of untreated psychosis (DUP), from the first sign of psychosis until treatment is given, is typically between one up four years in the Western world. Together with an early phase/risk phase (prodromal phase), often with an average duration of one year, this means that young people who develop a psychosis often go untreated for two to three years, and frequently longer than that, before they receive adequate help for their issues. With the help of extensive information campaigns, one can reduce the duration of untreated psychosis in a society from up to several years to just a few weeks or a few months, as shown in the Norwegian-Danish TIPS Project (Early Intervention in Psychosis) (Melle et al., Citation2004).
Early treatment of a short duration on untreated psychosis provides a better prognosis and reduces the risk of suicide (Melle et al., Citation2006). It seems evident that one can achieve secondary prevention by offering adequate treatment early in the development of the disorder.
Several research projects have further shown that it may be possible to achieve primary prevention of the development of psychotic disorders by intervening in the so-called risk/prodromal phase. It is too early to say whether these research results can be transferred to normal clinical practice. The ongoing Norwegian primary Prevention of Psychosis (POP) study is addressing this (Joa et al., Citation2015).
The TIPS study has contributed significantly to this new and important knowledge (Hegelstad et al., Citation2012; Johannessen et al., Citation2001). The results of the TIPS study, after 10 years of follow-up, show that the chance of achieving recovery, as judged by strict criteria, is more than twice as great when one comes from a place with early detection strategies and short DUP, compared to places with longer DUP. This is true even if the differences in DUP were not large (4.5 weeks, median versus 16 week, median). Several studies show that, at group level, there is an increasing degree of unfortunate disorder course alongside an increased duration of untreated psychosis. Studies show that the course gets worse when DUP is over 3 months.
The school plays an important role in detecting possible development of psychosis in young people. This is especially true in high school and at college/university. Teachers and counsellors need knowledge of what the early signs of possible psychosis development are, and they must learn to take such signs seriously. Teachers may find that “something is not right” in a student and working together with the family they may consider contacting the health services for follow-up.
Information and information programs are a prerequisite for being able to detect psychosis in young people. Such programs should be developed in close collaboration with user organisations. Relevant target groups for these information strategies are the general public, patients and relatives, the school (counsellors, class teachers and students), GPs, public psychologists, nurses, social wellfare services and the specialist health services.
More specifically about diagnoses
Through a thorough and accurate diagnosis, one tries to define different mental states or disorders and to distinguish these from each other. The aim of this is, among other things, to contribute to a more tailored treatment and to lay the foundation for increased knowledge about these disorders through research and method development. The diagnoses are a language, a terminology, that facilitates communication within professional environments and between different parties within the service apparatus. It is important to be aware that diagnoses in mental health care are constructed consensus-based units, and not absolute truths.
Diagnosis is furthermore fraught with disadvantages, and in mental health care one must therefore pay special attention to possible unfortunate aspects of diagnoses. The most important disadvantage is the danger of reducing the person to the diagnosis, so that one forgets to see the person behind the diagnosis. Diagnoses can also be stigmatising and contribute to self-stigma. Self-stigma means that the patient thinks of himself or herself as the disorder he/she has, instead of seeing himself or herself as a whole and complete human being with opportunities for development. The diagnoses may have advantages too; they can, e.g. help to explain and give meaning to phenomena and symptoms that the patient and relatives have had difficulty understanding.
Diagnoses should be useful in clinical work. However,many diagnoses in psychiatry have a relatively low utility value from a clinical standpoint. This is due to a significant overlap between the so-called mental “illnesses”. Diagnosis have low reliability (“accuracy”), and moreover provide a poor basis for saying something about prognosis. Diagnosis of psychotic disorders may furthermore be particularly challenging due to potentially complicated differential diagnostic assessments and many concomitant disorders. For those who are to treat these disorders, sufficient experience with this patient group, both in quantity and breadth, is important to capture this complexity.
Consequences for structure and content of services
Again, mental disorders are disorders of the young. Young people often find it difficult to put into words, and understand, the emotions they experience. The mental health care of the future must therefore, to a far greater extent, have conscious, national information and education strategies, and training- and antistigma- strategies, aimed at special target groups such as young people, schoolchildren and at-risk groups.
In order to achieve early intervention, available services must have a low threshold, and be easily accessible, preferably in places where children and young people spend time, in a non-stigmatising environment. In Australia, this has been put into a system through the easy-acess “headspace” youth friendly center model (Rickwood et al., Citation2019). A headspace centre will offer an early intervention approach, intergrating primary care services such as educational advice, legal advice, employment offices, GPs and specialist services in the local community.
The artificial age boundaries between child psychiatry, adolescent psychiatry and adult psychiatry, with a distinction at the age of 18, must be removed and/or redefined. The time is long overdue to ensure that the services aimed at young people and young adults are coordinated, e.g. so we have a treatment service from 0–12, and from13-25 years. Ideally, we should introduce a 0–100 perspective. Recent strategies for research and long-term follow-up recommend just that.
Up until 2021, Norway has developed good guidelines for the assessment, treatment and follow-up of various mental disorders. Common to these is that they have a multi- level service perspective; they try to facilitate so-called seamless services across management levels. Everyone emphasises the importance of continuity in treatment, and at this we are not talking about continuity to a Community mental health clinic or an outpatient clinic or to a treatment team, but to a committed human inter -relationship. These guidelines have later been laid down into a structured assessement and treatment system (Packages of Care) for psychosis, which is intended to ensure one’s treatment and the patient’s right to proper treatment for psychiatric disorders and near-psychotic conditions.
The clincal guidelines for treatment of psychosis in Norway (Helsedirektoratet, Citation2013) place great emphasis on the psychosocial, non-biological treatment approaches. This is not necessarily instead of drug treatment, but we must realize that today’s drugs for the most serious mental disorders are not as effective as one might hope. It becomes all the more important that we use documented effective forms of treatment, such as talking-therapies like cognitive behavioural therapy (CBT) (Morrison et al., Citation2004, Citation2020), psychodynamic psychotherapy (Rosenbaum et al., Citation2013), family treatment (McFarlane, Citation2016), milieu therapy (Thorgaard, Citation2006), focus on protecting physical health (Firth et al., Citation2019), music therapy (Gold et al., Citation2009) and other forms of art therapy. Individual placement and support (IPS) in relation to work and school life is now well documented as one of the most important measures we can implement (Moe et al., Citation2020). These are expensive forms of treatment and measures, much more expensive than medication, and forms of treatment that require time, but all economic calculations show that society saves large sums of money in a life perspective through evidence-based early intervention strategies and tailor-made treatment plans. Time to be together, to build relations, is probably the most important ingredient in good psychiatric treatment – time and continuity. Both these factors have suffered in recent decades during the restructuring of our mental health care, even though the road to where we are now has been paved with the best of intentions.
For the development of mental health care of the future, these two values must be the ones that show the way, and the ones which our health care structures reflect.
The design of clinical services should also reflect the disorder- or disease-panorama which society encounters, in the form of the number of people who need such services each year, the incidence of these, and which illness they present themselves with. In other words, which diagnostic groups they represent and how large the different groups are. This is our “terrain”. Then the “map”, or the offer of services, must be designed accordingly.
As stated earlier many of those who work in mental health services, our owners in the state and municipality, our politicians, do not know the mental health care treatment results. Overall, mental disorders are disorders with a good prognosis, if the right treatment is given at the right time, and if the patient actively participates in the treatment and avoids the unwise use of illegal drugs. For the most serious disorders, it is sometimes a question of treatment for several years, which is especially challenging for young people.
At the same time, patients and relatives must be invited to provide positive structured feedback to mental health care, the caregivers, on both patient-reported goals and satisfaction with the treatment offered. This is perhaps the main challenge of our time with regard to how we deploy available resources, especially considering that for example, in Norway about 80% of the resources in mental health care today are spent on treating psychotic disorders, even though these are initially few in scope.
These are difficult challenges, and they are further complicated by the fact that we, in the clinic, to a limited extent treat specific disorders. Instead we treat people with various troublesome symptoms and signs, where no one really fits one hundred percent into any diagnosis category.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Anglin, D. M., Ereshefsky, S., Klaunig, M. J., Bridgwater, M. A., Niendam, T. A., Ellman, L. M., DeVylder, J., Thayer, G., Bolden, K., Musket, C. W., Grattan, R. E., Lincoln, S. H., Schiffman, J., Lipner, E., Bachman, P., Corcoran, C. M., Mota, N. B., & Van Der Ven, E. (2021, July 1). From womb to neighborhood: A racial analysis of social determinants of psychosis in the United States. American Journal of Psychiatry, 178(7), 599–610. https://doi.org/https://doi.org/10.1176/appi.ajp.2020.20071091
- Bassett, A. S., Lowther, C., Merico, D., Costain, G., Chow, E. W. C., van Amelsvoort, T., McDonald-McGinn, D., Gur, R. E., Swillen, A., Van Den Bree, M., Murphy, K., Gothelf, D., Bearden, C. E., Eliez, S., Kates, W., Philip, N., Sashi, V., Campbell, L., Vorstman, J., Cubells, J., & .Marshall, C. R. (2017, November 1). Rare genome-wide copy number variation and expression of schizophrenia in 22q11.2 deletion syndrome. American Journal of Psychiatry, 174(11), 1054–1063. https://doi.org/https://doi.org/10.1176/appi.ajp.2017.16121417
- Bentall, R. P. (1993, January 1). Deconstructing the concept of ‘schizophrenia’. Journal of Mental Health, 2(3), 223–238. https://doi.org/https://doi.org/10.3109/09638239309003768
- Calcia, M. A., Bonsall, D. R., Bloomfield, P. S., Selvaraj, S., Barichello, T., & Howes, O. D. (2016). Stress and neuroinflammation: A systematic review of the effects of stress on microglia and the implications for mental illness. Psychopharmacology (Berl), 233(9), 1637–1650. https://doi.org/https://doi.org/10.1007/s00213-016-4218-9
- Christensen, T. N., Wallstrøm, I. G., Eplov, L. F., Laursen, T. M., & Nordentoft, M. (2021). Incidence rates and employment trends in schizophrenia spectrum disorders, bipolar affective disorders and recurrent depression in the years 2000–2013: A Danish nationwide register-based study. Nordic Journal of Psychiatry, 1–8. https://doi.org/https://doi.org/10.1080/08039488.2021.1952304
- Firth, J., Siddiqi, N., Koyanagi, A., Siskind, D., Rosenbaum, S., Galletly, C., Allan, S., Caneo, C., Carney, R., Carvalho, A. F., Chatterton, M. L., Correll, C. U., Curtis, J., Gaughran, F., Heald, A., Hoare, E., Jackson, S. E., Kisely, S., Lovell, K., Maj, M., & Stubbs, B. (2019, August 1). The Lancet psychiatry commission: A blueprint for protecting physical health in people with mental illness. The Lancet Psychiatry, 6(8), 675–712. https://doi.org/https://doi.org/10.1016/S2215-0366(19)30132-4
- Ginsburg, G. S., Becker, E. M., Keeton, C. P., Sakolsky, D., Piacentini, J., Albano, A. M., Compton, S. N., Iyengar, S., Sullivan, K., Caporino, N., Peris, T., Birmaher, B., Rynn, M., March, J., & Kendall, P. C. (2014). Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry, 71(3), 310–318. https://doi.org/https://doi.org/10.1001/jamapsychiatry.2013.4186
- Goes, F. S., & Sawa, A. (2017, November 1). Psychosis beyond the 22q11.2 deletion: Do additional genetic factors play a role? American Journal of Psychiatry, 174(11), 1027–1029. https://doi.org/https://doi.org/10.1176/appi.ajp.2017.17080910
- Gold, C., Solli, H. P., Krüger, V., & Lie, S. A. (2009, April). Dose-response relationship in music therapy for people with serious mental disorders: Systematic review and meta-analysis. Clinical Psychology Review, 29(3), 193–207. https://doi.org/https://doi.org/10.1016/j.cpr.2009.01.001
- Gore, F. M., Bloem, P. J. N., Patton, G. C., Ferguson, J., Joseph, V., Coffey, C., Sawyer, S. M., & Mathers, C. D. (2011). Global burden of disease in young people aged 10–24 years: A systematic analysis. The Lancet, 377(9783), 2093–2102. https://doi.org/https://doi.org/10.1016/S0140-6736(11)60512-6
- Hastings, P. D., Serbin, L. A., Bukowski, W., Helm, J. L., Stack, D. M., Dickson, D. J., Ledingham, J. E., & Schwartzman, A. E. (2020). Predicting psychosis-spectrum diagnoses in adulthood from social behaviors and neighborhood contexts in childhood. Development and Psychopathology, 32(2), 465–479. https://doi.org/https://doi.org/10.1017/S095457941900021X
- Hegelstad, W. T., Larsen, T. K., Auestad, B., Evensen, J., Haahr, U., Joa, I., Johannesen, J. O., Langeveld, J., Melle, I., Opjordsmoen, S., Rossberg, J. I., Rund, B. R., Simonsen, E., Sundet, K., Vaglum, P., Friis, S., & McGlashan, T. (2012, April 1). Long-term follow-up of the TIPS early detection in psychosis study: Effects on 10-year outcome. American Journal of Psychiatry, 169(4), 374–380. https://doi.org/https://doi.org/10.1176/appi.ajp.2011.11030459
- Helsedirektoratet. (2013). Nasjonal faglig retningslinje for utredning, behandling og oppfølging av personer med psykoselidelser [National guidelines for assessment, treatment and follow-up of peope with psychosis]. Helsedirektoratet.
- Howes, O. D. M. P. D. M., McCutcheon, R. M., Owen, M. J. P. F., & Murray, R. F. R. S. D. (2016). The role of genes, stress and dopamine in the development of schizophrenia. Biological Psychiatry, 81(1), 9–20. https://doi.org/https://doi.org/10.1016/j.biopsych.2016.07.014
- Insel, T., Cuthbert, B., Garvey, M., Heinssen, R., Pine, D. S., Quinn, K., Sanislow, C., & Wang, P., & National Institute of Mental Health, Bethesda, Md. (2010). Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 167(7), 748–751. https://doi.org/https://doi.org/10.1038/nature09552
- Jiang, S., Postovit, L., Cattaneo, A., Binder, E. B., & Aitchison, K. J. (2019, November 8). Epigenetic modifications in stress response genes associated with childhood trauma [Review]. Frontiers in Psychiatry, 10(808). https://doi.org/https://doi.org/10.3389/fpsyt.2019.00808
- Joa, I., Gisselgard, J., Bronnick, K., McGlashan, T., & Johannessen, J. O. (2015, April 22). Primary prevention of psychosis through interventions in the symptomatic prodromal phase, a pragmatic Norwegian ultra high risk study. BMC Psychiatry, 15(1), 89. https://doi.org/https://doi.org/10.1186/s12888-015-0470-5
- Johannessen, J. O., McGlashan, T. H., Larsen, T. K., Horneland, M., Joa, I., Mardal, S., Kvebaek, R., Friis, S., Melle, I., Opjordsmoen, S., Simonsen, E., Ulrik, H., & Vaglum, P. (2001, August 1). Early detection strategies for untreated first-episode psychosis. Schizophrenia Research, 51(1), 39–46. [pii]. https://doi.org/https://doi.org/10.1016/S0920-9964(01)00237-7
- Jongsma, H. E., Gayer-Anderson, C., Lasalvia, A., Quattrone, D., Mulè, A., Szöke, A., Selten, J.-P., Turner, C., Arango, C., Tarricone, I., Berardi, D., Tortelli, A., Llorca, P.-M., de Haan, L., Bobes, J., Bernardo, M., Sanjuán, J., Santos, J. L., Arrojo, M., Del-Ben, C. M., Kirkbride, J. B. (2018). Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatry, 75(1), 36–46. https://doi.org/https://doi.org/10.1001/jamapsychiatry.2017.3554
- Kessler, R. C., Amminger, G. P., Aguilar-Gaxiola, S., Alonso, J., Lee, S., & Ustun, T. B. (2007, July). Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry, 20(4), 359–364. https://doi.org/https://doi.org/10.1097/YCO.0b013e32816ebc8c
- Kühl, J. O. G., Laursen, T. M., Thorup, A., & Nordentoft, M. (2016, October 1). The incidence of schizophrenia and schizophrenia spectrum disorders in Denmark in the period 2000–2012. A register-based study. Schizophrenia Research, 176(2), 533–539. https://doi.org/https://doi.org/10.1016/j.schres.2016.06.023
- Leboyer, M., & Schurhoff, F. (2014, September). Searching across diagnostic boundaries. Schizophrenia Bulletin, 40(5), 946–948. https://doi.org/https://doi.org/10.1093/schbul/sbu112
- Malmqvist, A., Schwieler, L., Orhan, F., Fatouros-Bergman, H., Bauer, M., Flyckt, L., Cervenka, S., Engberg, G., Piehl, F., & Erhardt, S. (2019). Increased peripheral levels of TARC/CCL17 in first episode psychosis patients. Schizophrenia Research, 210(August 2019), 221–227. https://doi.org/https://doi.org/10.1016/j.schres.2018.12.033
- McFarlane, W. R. (2016, September). Family interventions for schizophrenia and the psychoses: A review. Family Process, 55(3), 460–482. https://doi.org/https://doi.org/10.1111/famp.12235
- McGlashan, T. H., & Johannessen, J. O. (1996). Early detection and intervention with schizophrenia: Rationale. Schizophrenia Bulletin, 22(2), 201–222. https://doi.org/https://doi.org/10.1093/schbul/22.2.201
- McGorry, P. D., Hickie, I. B., Yung, A. R., Pantelis, C., & Jackson, H. J. (2006, August). Clinical staging of psychiatric disorders: A heuristic framework for choosing earlier, safer and more effective interventions. Australian & New Zealand Journal of Psychiatry, 40(8), 616–622. ANP1860 [pii]. https://doi.org/https://doi.org/10.1111/j.1440-1614.2006.01860.x
- Melle, I., Johannesen, J. O., Friis, S., Haahr, U., Joa, I., Larsen, T. K., Opjordsmoen, S., Rund, B. R., Simonsen, E., Vaglum, P., & McGlashan, T. (2006, May). Early detection of the first episode of schizophrenia and suicidal behavior. American Journal of Psychiatry, 163 (5), 800–804. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16648319
- Melle, I., Larsen, T. K., Haahr, U., Friis, S., Johannessen, J. O., Opjordsmoen, S., Simonsen, E., Rund, B. R., Vaglum, P., & McGlashan, T. (2004, February). Reducing the duration of untreated first-episode psychosis: Effects on clinical presentation. Archives of General Psychiatry, 61(2), 143–150. 61/2/143 [pii]. https://doi.org/https://doi.org/10.1001/archpsyc.61.2.143
- Mittal, V., & Walker, E. (2019). Advances in the neurobiology of stress and psychosis. Schizophrenia Research, 213(November 2019), 1–5. https://doi.org/https://doi.org/10.1016/j.schres.2019.08.030
- Moe, C., Brinchmann, B., McDaid, D., Killackey, E., Rinaldi, M., & Mykletun, A. (2020, January). Approaches to implementing individual placement and support in the health and welfare sectors: A scoping review protocol. JBI Evid Synth, 18(1), 170–177. https://doi.org/https://doi.org/10.11124/jbisrir-d-19-00035
- Morrison, A., Read, J., & Turkington, D. (2005). Trauma and psychosis: Theoretical and clinical implications. Acta Psychiatrica Scandinavica, 112(5), 327–329. https://doi.org/https://doi.org/10.1111/j.1600-0447.2005.00644.x
- Morrison, A. P., French, P., Walford, L., Lewis, S. W., Kilcommons, A., Green, J., Parker, S., & Bentall, R. P. (2004, October). Cognitive therapy for the prevention of psychosis in people at ultra-high risk: Randomised controlled trial. British Journal of Psychiatry, 185(4), 291–297. https://doi.org/https://doi.org/10.1192/bjp.185.4.291
- Morrison, A. P., Pyle, M., Maughan, D., Johns, L., Freeman, D., Broome, M. R., Husain, N., Fowler, D., Hudson, J., MacLennan, G., Norrie, J., Shiers, D., Hollis, C., James, A., Morrison, A. P., Pyle, M., Maughan, D., Johns, L., Freeman, D., Broome, M. R., & James, A. (2020, September 1). Antipsychotic medication versus psychological intervention versus a combination of both in adolescents with first-episode psychosis (MAPS): A multicentre, three-arm, randomised controlled pilot and feasibility study. The Lancet Psychiatry, 7(9), 788–800. https://doi.org/https://doi.org/10.1016/S2215-0366(20)30248-0
- Pillinger, T., Osimo, E. F., Brugger, S., Mondelli, V., McCutcheon, R. A., & Howes, O. D. (2019). A meta-analysis of immune parameters, variability, and assessment of modal distribution in psychosis and test of the immune subgroup hypothesis. Schizophrenia Bulletin, 45(5), 1120–1133. https://doi.org/https://doi.org/10.1093/schbul/sby160
- Read, J. (2010, 2015-03-22). Can poverty drive you mad? ‘Schizophrenia’, socio-economic status and the case for primary prevention. New Zealand Journal of Psychology (Online), 39 (2), 7–19. https://www.psychology.org.nz/journal-archive/NZJP-Vol392-2010-2-Read.pdf
- Read, J., Fink, P., Rudegeair, T., Felitti, V., & Whitfield, C. (2008, October 1). Child maltreatment and psychosis: A return to a genuinely integrated bio-psycho-social model. Clinical Schizophrenia & Related Psychoses, 2(3), 235. https://doi.org/https://doi.org/10.3371/CSRP.2.3.5
- Read, J., Fosse, R., Moskowitz, A., & Perry, B. (2014, February 2014-03-27). The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry, 4(1), 65–79. https://doi.org/https://doi.org/10.2217/npy.13.89
- Rickwood, D., Paraskakis, M., Quin, D., Hobbs, N., Ryall, V., Trethowan, J., & McGorry, P. (2019). Australia’s innovation in youth mental health care: The headspace centre model. Early Intervention in Psychiatry, 13(1), 159–166. https://doi.org/https://doi.org/10.1111/eip.12740
- Romme, M. A. J., & Escher, A. D. M. A. C. (1989). Hearing voices. Schizophrenia Bulletin, 15(2), 209–216. https://doi.org/https://doi.org/10.1093/schbul/15.2.209
- Rosenbaum, B., Martindale, B., & Summers, A. (2013). Supportive psychodynamic psychotherapy for psychosis. Advances in Psychiatric Treatment, 19(4), 310–318. https://doi.org/https://doi.org/10.1192/apt.bp.111.009142
- Thorgaard, L. (2006). Dynamisk psykoseforståelse og dynamisk relationsbehandling. Hertervig forlag.
- Trauelsen, A. M., Bendall, S., Jansen, J. E., Nielsen, H. G., Pedersen, M. B., Trier, C. H., Haahr, U. H., & Simonsen, E. (2015, June). Childhood adversity specificity and dose-response effect in non-affective first-episode psychosis. Schizophrenia Research, 165(1), 52–59. https://doi.org/https://doi.org/10.1016/j.schres.2015.03.014
- Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., Read, J., Van Os, J., & Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661–671. https://doi.org/https://doi.org/10.1093/schbul/sbs050
- Zubin, J., & Spring, B. (1977). Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology (1965), 86(2), 103–126. https://doi.org/https://doi.org/10.1037//0021-843X.86.2.103