Abstract
Purpose
To provide normative data on swallowing capacity (mL/s) in people older than 60 years using the Timed Water Swallow Test (TWST), stratified by sex. Intra- and inter-rater reliability for swallowing time in TWST was further investigated.
Method
A total of 165 participants, aged 60 years and above, were included in the study. The time taken to consume 150 mL of tap water and the swallowing capacity (mL/s) was observed in a clinical context using the TWST. Video recordings of the performances were collected for 118 of the 165 participants for inter-rater reliability testing, of which a random set of 25 performances were assessed for intra-rater reliability. Analysis of the agreement between TWST rated by an in-person clinician and rated from a video recording was further evaluated.
Result
There were significant age and sex effects observed for swallowing capacity. The average reduction in swallowing capacity in the investigated age range (60–92 years) was 8.8 and 7.3 mL/s, for women and men respectively. The results showed high inter-and intra-rater reliability and agreement between the clinical assessment and the video recording.
Conclusion
The presented measurements indicate a clear effect of age on swallowing capacity and that women may be expected to have lower capacity scores than men when tested using TWST. The provided norms can be used as reference points in the clinical identification of people at risk of dysphagia in the older population.
Introduction
Oropharyngeal dysphagia (i.e. swallowing dysfunction) is a prevalent condition in the older population and refers to swallowing difficulties in the oral cavity and the pharynx (Baijens et al., Citation2016; Serra-Prat et al., Citation2011). Furthermore, oropharyngeal dysphagia is a growing problem among older people due to age-related diseases and age-related changes that affect the swallowing function and can cause severe complications (Baijens et al., Citation2016; Smithard et al., Citation1996). The main complications of oropharyngeal dysphagia include malnutrition, dehydration, respiratory infections, and aspiration pneumonia (Cabre et al., Citation2010; Rofes et al., Citation2010; Serra-Prat et al., Citation2012; Smithard et al., Citation1996). The most accurate way to identify oropharyngeal dysphagia is by using instrumental assessments such as flexible endoscopic evaluation of swallowing (FEES) or videofluoroscopic swallowing study (VFSS) (Langmore, Citation2003). However, the availability of FEES and VFS varies across countries due to social and economic conditions and the existing health policies, and requires trained personnel in performing these gold standard assessment (Baijens et al., Citation2016). To minimise potential complications of oropharyngeal dysphagia, a first step is thus to establish screening methods that can identify patients at risk of dysphagia. Most screening tools assess the activity of swallowing water to identify patients at risk of oropharyngeal dysphagia and by observing clinical signs of swallowing dysfunction such as cough or wet/gurgly voice while swallowing (Bours, Speyer, Lemmens, Limburg, & de Wit, Citation2009; DePippo, Holas, & Reding, Citation1992; Kertscher, Speyer, Palmieri, & Plant, Citation2014; Martino et al., Citation2009; Perry, Citation2001).
One common screening tool used to identify people at risk of oropharyngeal dysphagia is the Timed Water Swallow Test (TWST) (Hughes & Wiles, Citation1996; Nathadwarawala, McGroary, & Wiles, Citation1994; Nathadwarawala, Nicklin, & Wiles, Citation1992). The TWST is a bedside screening tool aimed to assess swallowing capacity (mL/s) as a quantitative indicator of oropharyngeal dysphagia in patients with a neurogenetic diagnosis (Nathadwarawala et al., Citation1992). The authors concluded that swallowing capacity was a reliable and valid index for screening those at risk of dysphagia or its complications and monitoring therapy (i.e. as a quantitative measure before and after swallowing training). A swallowing capacity below 10 mL/s was suggested to be a valid index to identify swallowing difficulties, and this cut-off has been given further support by other studies using instrumental assessments; Wu, Chang, Wang, and Lin (Citation2004) observed that 47 out of 49 participants with a swallowing capacity below 10 mL/s on the TWST had swallowing dysfunction in VFSS, and approximately 50% had an impaired swallowing safety. Hägglund et al. (Citation2020) similarly observed that all investigated participants in the sub-acute phase of stroke (n = 32) with a swallowing capacity <10 mL/s had a swallowing dysfunction in VFSS, 53% had a reduced swallowing safety (i.e. misdirected swallowing with material entering the larynx or the trachea), and 78% had impaired swallowing efficacy (i.e. pharyngeal retention). Thus, a reduced swallowing capacity in screening can be considered predictive of a reduced swallowing function in instrumental assessments.
Further findings of the normative data collected in the original study indicated that swallowing capacity was slowing with age and that women had a slower swallow than men (Nathadwarawala et al., Citation1992). The normative data were, however, only based on a few participants (15 women; 5 men) over the age of 70, making them difficult to use as a clinical reference for many neurological patient groups. While stronger sets of normative reference values have been provided for younger people in subsequent reports (Hughes & Wiles, Citation1996; Sarve, Krishnamurthy, & Balasubramanium, Citation2021), normative data for older people are still lacking.
The TWST has also previously demonstrated high inter-and intra-rater and test-retest reliability (Hughes & Wiles, Citation1996; Nathadwarawala et al., Citation1992). It has further recently shown good to excellent inter-rater reliability when assessed asynchronously from tele-evaluations on patients with suspected dysphagia, indicating it can be reliably measured via telehealth in clinical practice (Borders, Sevitz, Malandraki, Malandraki, & Troche, Citation2021). However, the agreement of TWST performances has not been evaluated from a) video on healthy older individuals or b) the rating of TWST by an in-person clinician compared with ratings from video recordings. Thus, it would be beneficent to evaluate whether an in-person clinician's rating is similar to ratings directly assessed from video recording without pausing to understand the TWST's transference and clinical compliance from the clinic into potential application in telehealth.
Purpose
The present study aimed to establish additional normative data on swallowing capacity (mL/s) for healthy people 60 years and older, stratified by sex. A secondary aim was to evaluate the agreements between TWST swallowing time rated by an in-person clinician and rated from a video recording by a separate clinician, and inter-and intra-rater reliability in assessments from video recordings of TWST.
Method
Participants and settings
This normative study of swallowing capacity using the TWST in people 60 years and older was performed at the general university hospital or a participant's location. We included 165 healthy participants with no report of dysphagia, neurological or gastroenterological disorders, head and neck injuries/surgeries, major neurocognitive disorders, history of intubation, or oral disorders that could affect the swallowing function. The participants were recruited from the general public (e.g. social groups, personal contacts, senior university, and retirement homes) and were all oriented to person, time, and space, which was tested verbally before inclusion. Two recruitment efforts were made; the first (118 participants) assessments were performed by two raters, and the data collection was later expanded to the full set of 165 participants in a renewed effort. The participants were stratified by sex (). This study was conducted in accordance with the Helsinki declaration and was approved by the (Swedish) Ethical Review Authority (Case number 2020-04817) and by the (Faculty of Medicine, Umeå University (FS 1.1.1072-17)). Written informed consent was obtained from all participants.
Table I. An overview of the age and sex distribution of included participants.
Materials
A 100 mL vessel was used to measure 150 mL of water, and a glass that could hold 150mL water was used for the TWST. Also, a 5 ml vessel was used to measure the amount of water a participant could not drink (residual volume). A Canon PowerShot S90 was used when video recording tests were performed.
Data collection
The participants were asked to be seated in an upright position on a chair. Before the TWST was carried out, the participants were given three teaspoons of water to verify that they could swallow a small amount of water without signs of dysphagia. The participants were then given 150 mL of cold tap water in a glass and instructed to drink the water as quickly as possible and stop if any difficulty arose. The participants were asked to put the glass against the lower lip and start drinking on the starting signal. The swallowing time was measured by an external timer from when the water touched the lips until the larynx returned in the rest position (i.e. as seen exteriorly by the thyroid cartilage movement). The time in seconds (s) and any residual volume (mL) were noted on the test protocol. The swallowing capacity (mL/s) was calculated by subtracting any residual volume from 150 mL and dividing the difference by time (s). Each participant performed a single TWST trial.
Inter-rater reliability was assessed by two raters timing a video recording of the TWST performance for the 118 participants who were requited in the initial data collection effort. The agreement between the in-person rating of the TWST performance with a separate clinician’s rating from video recording was further compared. The two raters rated 59 participants each in-person and 59 participants from video. The raters were not allowed to stop the video or use frame-by-frame methods when assessing the TWST performances from the video. This approach was chosen to resemble the information that can be obtained via telehealth, except for the ability of the clinician to provide instructions or feedback to the patient before testing. Intra-rater reliability was further assessed on 20% (n = 25) of the collected video samples. The video recording of the performance was collected using a camera placed at a distance that made the lateral area of the nose and the collarbone of the participant visible, including a clear view of the larynx.
Statistical analysis
Normative data were established for participants’ swallowing capacity and time taken during the TWST, stratified by sex, as mean and 95% confidence interval (CI). The primary statistical analysis of effects on swallowing capacity and time was performed using an ANCOVA, with age (as continuous variable) and sex as independent factors. Type III sums of squares were used in the testing of effects of age and sex in the unbalanced ANCOVA.
Inter-rater reliability for the two raters assessing the performances from video recording was analysed using intraclass correlation (ICC); two-way random effects model analysis. Intra-rater analysis for two raters was further assessed from a random set of 25 TWST performances (i.e. 20% of the sample) and analysed using a two-way mixed, single score, absolute agreement intra-class coefficient (ICC(3,1)). Further, the agreement in swallowing time obtained in the clinical assessment by an in-person clinician and the time obtained from video recording was assessed using two-way random, single measure, absolute intra-class correlation (ICC(2,1)).
Result
Participants
In total, 165 healthy individuals between 60 and 92 years of age (mean age 74 years (SD±7.6)) performed the TWST, of whom 81 were women (mean age 74.5 ± 7.8) and 84 were men (mean age 73.7 ± 7.5), see .
Swallowing capacity
Normative data (mean and 95% CI) for the time used during the TWST and the swallowing capacity (mL/s), stratified by sex and age, are shown in displayed in . The mean swallowing capacity for the participants was above 10 mL/s, regardless of age or sex (). Of the 165 participants, 20 (15 women; 5 men) across the investigated age range (60–92 years) failed to show a swallowing capacity >10 mL/s. The average reduction in swallowing capacity over the investigated age range was 8.8 mL/s for women and 7.3 mL/s for men, with a reduction of 0.276 mL/s and 0.227 mL/s per year, for women and men respectively. The raw data of the participants’ performances of TWST are made available as Supplementary Material.
Figure 1. Locally fitted regression lines indicating the estimated mean swallowing performance, with 95% confidence interval, as a function of age and sex of the participant. The performance is indicated as the time taken to swallow 150 mL of water (top) and the computed swallowing capacity of the participants (in mL/s, bottom).
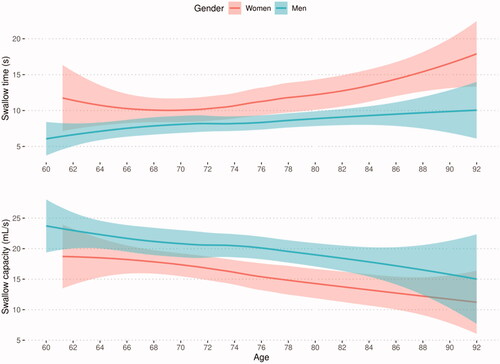
Table II. An overview of the mean and 95% confidence interval obtained for swallowing performance when using the TWST, stratified by age and sex.
Age and sex effect
The age and sex effect on swallowing capacity (mL/s) and swallowing time (s) are shown in . An ANCOVA confirmed a significant effect of participant age (F(1,161)=16.3, p= <0.001, η2p = 0.10) and sex (F(1,161)=21.3, p < 0.001, η2p = 0.11; ) on swallowing capacity. The interaction effect of age and sex was shown not to reach an overall statistical significance (F(1,161)=1.42, p = 0.234, n.s; ).
Table III. Summary of the effects of age and sex on TWST outcome measures (swallowing time and capacity) obtained through ANCOVA.
Reliability
Agreement between TWST rating by an in-person clinician and ratings from video recording were, on average, within 0.15 ± 0.62s of the time obtained from the video recording (0.13 ± 0.61s and 0.18 ± 0.62s, respectively for the two assessors), resulting in a high inter-rater agreement between the TWST rating by an in-person and from video recording: rater one and the in-person clinician [ICC(2,1)=0.992, 95% CI = 0.987––0.994]; and rater two and the in-person clinician [ICC(2,1)=0.992, 95% CI = 0.989–0.995]. Two assessments by the same rater from a video recording showed excellent agreement (ICC(3,1) between 0.99 and 1.00) for the two raters.
Discussion
This study provides normative data on swallowing capacity for healthy people 60 years and older using the TWST (Hughes & Wiles, Citation1996; Nathadwarawala et al., Citation1992). Swallowing capacity was observed to be reduced with age for both men and women, and women swallowed more slowly than men. In the study cohort the mean swallowing capacity was above 10 mL/s. The inter- and intra-rater assessment and the comparison between TWST rated by an in-person clinician versus video recordings also indicate that TWST has high reliability, which is an early indication that TWST could potentially be used to assess swallowing in telehealth. Specific considerations related to factors influencing the TWST testing are discussed below.
Sex and age effect
The sex of the participants influenced the time taken to swallow 150 mL of water, and consequently, the measured swallowing capacity of participants. Men had a higher swallowing capacity than women, which agrees well with previous findings (Alfonsi et al., Citation2015; Hughes & Wiles, Citation1996). Swallowing capacity further showed a similar but not identical rate of decrease with age for healthy men and women of 0.276 and 0.227 mL/s per year, respectively. The age related decline in swallowing capacity may have several underlying causes. Age is known to reduce swallowing function by prolonging the oral phase of the swallowing (Dodds, Citation1989; Yoshikawa et al., Citation2005), introducing a slight delay in triggering the pharyngeal swallowing (Robbins, Hamilton, Lof, & Kempster, Citation1992; Tracy et al., Citation1989; Yoshikawa et al., Citation2005), and an increased frequency of penetration (i.e. food and liquid leaking into the larynx, but not below the vocal folds (Daggett, Logemann, Rademaker, & Pauloski, Citation2006). All participants in this study were 60 years or older; thus, an ageing effect might be expected. Other factors can also impact the swallowing function that were not accounted for in this study, such as sarcopenia (Maeda & Akagi, Citation2016), snoring (Lee, Ko, & Chuang, Citation2000; Lee, Tse, Tsze, & Kwok, Citation2004; Shaheen et al., Citation2008), and polymedication or specific medication such as antipsychotic, antidepressant, and sedatives that reduce cough reflex and/or cause xerostomia (i.e. dry mouth) (Cabre et al., Citation2010; Carrion et al., Citation2015; Ney, Weiss, Kind, & Robbins, Citation2009; Stoschus & Allescher, Citation1993). These factors remain not controlled for in the current investigation, and whether, and to what extent they may have reduced the swallowing capacities showed by a particular participant requires further research.
The mean swallowing capacity observed for all participants, regardless of age or sex, was greater than 10 mL/s. Previous studies have concluded that a swallowing capacity of less than 10 mL/s is, at least for people under the age of 70, an indicator of dysphagia (Hughes & Wiles, Citation1996; Nathadwarawala et al., Citation1992). Additionally, other studies have found that when patients have a swallowing capacity of less than 10 mL/s, they also have a swallowing dysfunction present on VFS (Wu et al., Citation2004; Hägglund et al., Citation2020). Our findings indicate that healthy individuals even older than 70, on average, have a swallowing capacity above 10 mL/s. The 10 mL/s cut-off as an indicator of risk of dysphagia might thus also be applicable among older individuals. However, to understand whether the proposed cut-off indicator for risk of dysphagia (Hughes & Wiles, Citation1996; Nathadwarawala et al., Citation1992) is applicable even among older people we further need to compare healthy older individuals’ TWST results directly with functional outcomes visualised on instrumental assessments (i.e. by VFSS or FEES). Especially since our data also show that some healthy individuals (15 women and 5 men) across the age continuum in the current study showed a swallowing capacity of less than 10 mL/s.
Normative data of swallowing capacity for men and women, especially those older than 70, is highly requested. The prevalence of dysphagia increases with age, and a low swallowing capacity or a capacity that deviates from the normative data may alert clinicians further to investigate the person’s swallowing function with instrumental assessment and thus avoid potential respiratory complications.
Reliability
This study indicates that TWST performance, on an extensive data set of healthy older individuals, has a high inter- and intra-rater agreement when rated asynchronous from video. Previous studies have shown that TWST have both high inter- and intra-rater and test-retest reliability when rated by an in-person clinician on healthy individuals and patients with suspected dysphagia (Hughes & Wiles, Citation1996; Nathadwarawala et al., Citation1992), and asynchronously from video on patients with movement disorders and suspected dysphagia (Borders et al., Citation2021).
Our findings also indicate that TWST can be reliably used in telehealth; the time obtained directly by an in-person clinician and asynchronously from video recordings on the same participants were highly agreeable. This finding indicates that TWST results do not significantly differ depending on the context where the TWST is performed (face-to-face in the clinic or over telehealth). This finding further illustrates that TWST might both be suitable for telehealth and that it might be possible for a non-clinician (e.g. family member/nursing staff) to record the TWST performance and later upload it to a clinician for evaluation. However, the latter needs further evaluation on whether a non-clinician can reliably administrate the TWST (i.e. provide water administration, instructions, and camera placement for a visible view of the mount, throat, and larynx). Overall, TWST seems to be a valid and reliable, simple screening test that can easily be carried out to identify people at risk of dysphagia or monitor therapy in clinics and over telehealth.
Limitations
We did not include the number of swallows in the assessment as included in the original version of TWST. The number of swallows was not accounted for in the present study since clinicians do not commonly use it as a reference for abnormal swallowing or indicator for further instrumental assessment. Furthermore, we did not account for snoring, medication, or sarcopenic dysphagia in this study, which might impact the swallowing capacity. Future studies should compare TWST’s performance of healthy older individuals and patients with suspected oropharyngeal dysphagia with an instrumental assessment of their swallowing function to further evaluate the proposed cut-off of 10mL/s. The TWST should also be evaluated when administrated by a non-clinician (e.g. family member/nursing staff) compared with a trained clinician to evaluate its utility, efficacy, and reliability regardless of administrator.
Conclusion
We have presented sex-stratified normative data for swallowing capacity in people older than 60 years. The effect of age and sex provided an evident influence on swallowing capacity. However, all participants had on average a swallowing capacity above 10 mL/s, regardless of age and sex. The TWST also indicated a high inter- and intra-rater agreeability and that the test might be performed both in a clinical situation and in telehealth with good agreeability.
Supplementary_Material_TASL-2021-0064.xlsx
Download MS Excel (16.2 KB)Declaration of interest
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed at https://doi.org/10.1080/17549507.2022.2096925.
References
- Alfonsi, E., Cosentino, G., Mainardi, L., Schindler, A., Fresia, M., Brighina, F., … Sandrini, G. (2015). Electrophysiological investigations of shape and reproducibility of oropharyngeal swallowing: Interaction with bolus volume and age. Dysphagia, 30, 540–550. doi:10.1007/s00455-015-9634-1
- Baijens, L.W., Clave, P., Cras, P., Ekberg, O., Forster, A., Kolb, G.F., … Walshe, M. (2016). European Society for Swallowing Disorders – European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clinical Interventions in Aging, 11, 1403–1428. doi:10.2147/CIA.S107750
- Borders, J.C., Sevitz, J.S., Malandraki, J.B., Malandraki, G.A., & Troche, M.S. (2021). Objective and subjective clinical swallowing outcomes via Telehealth: Reliability in outpatient clinical practice. American Journal of Speech-Language Pathology, 30, 598–608. doi:10.1044/2020_AJSLP-20-00234
- Bours, G.J., Speyer, R., Lemmens, J., Limburg, M., & de Wit, R. (2009). Bedside screening tests vs. videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. Journal of Advanced Nursing, 65, 477–493. doi:10.1111/j.1365-2648.2008.04915.x
- Cabre, M., Serra-Prat, M., Palomera, E., Almirall, J., Pallares, R., & Clave, P. (2010). Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing, 39, 39–45. doi:10.1093/ageing/afp100
- Carrion, S., Cabre, M., Monteis, R., Roca, M., Palomera, E., Serra-Prat, M., … Clave, P. (2015). Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clinical Nutrition, 34, 436–442. doi:10.1016/j.clnu.2014.04.014
- Daggett, A., Logemann, J., Rademaker, A., & Pauloski, B. (2006). Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia, 21, 270–274. doi:10.1007/s00455-006-9051-6
- DePippo, K.L., Holas, M.A., & Reding, M.J. (1992). Validation of the 3-oz water swallow test for aspiration following stroke. Archives of Neurology, 49, 1259–1261. doi:10.1001/archneur.1992.00530360057018
- Dodds, W.J. (1989). Physiology of swallowing. Dysphagia, 3, 171–178. doi:10.1007/BF02407219
- Hägglund, P., Hägg, M., Levring Jäghagen, E., Larsson, B., & Wester, P. (2020). Oral neuromuscular training in patients with dysphagia after stroke: a prospective, randomized, open-label study with blinded evaluators. BMC Neurol, 20, 405. doi:10.1186/s12883-020-01980-1
- Hughes, T.A., & Wiles, C.M. (1996). Clinical measurement of swallowing in health and in neurogenic dysphagia. Quarterly Journal of Medicine, 89, 109–116. doi:10.1093/qjmed/89.2.109
- Kertscher, B., Speyer, R., Palmieri, M., & Plant, C. (2014). Bedside screening to detect oropharyngeal dysphagia in patients with neurological disorders: an updated systematic review. Dysphagia, 29, 204–212. doi:10.1007/s00455-013-9490-9
- Langmore, S.E. (2003). Evaluation of oropharyngeal dysphagia: which diagnostic tool is superior? Current Opinion in Otolaryngology and Head and Neck Surgery, 11, 485–489. doi:10.1097/00020840-200312000-00014
- Lee, H.C., Ko, W.C., & Chuang, Y.C. (2000). Tetanus of the elderly. J Microbiol Immunol Infect, 33, 191–196. https://www.ncbi.nlm.nih.gov/pubmed/11045384
- Lee, J.S., Tse, S.L., Tsze, S.C., & Kwok, T. (2004). Protein malnutrition is adversely associated with swallowing recovery in tube-fed older people. Journal of American Geriatric Society, 52, 1588–1589. doi:10.1111/j.1532-5415.2004.52430_9.x
- Maeda, K., & Akagi, J. (2016). Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatrics & Gerontology International, 16, 515–521. doi:10.1111/ggi.12486
- Martino, R., Silver, F., Teasell, R., Bayley, M., Nicholson, G., Streiner, D.L., & Diamant, N.E. (2009). The Toronto Bedside Swallowing Screening Test (TOR-BSST): Development and validation of a dysphagia screening tool for patients with stroke. Stroke, 40, 555–561. doi:10.1161/STROKEAHA.107.510370
- Nathadwarawala, K.M., McGroary, A., & Wiles, C.M. (1994). Swallowing in neurological outpatients: Use of a timed test. Dysphagia, 9, 120–129. doi:10.1007/BF00714599
- Nathadwarawala, K.M., Nicklin, J., & Wiles, C.M. (1992). A timed test of swallowing capacity for neurological patients. Journal of Neurology. Neurosurgery and Psychiatry, 55, 822–825. doi:10.1136/jnnp.55.9.822
- Ney, D.M., Weiss, J.M., Kind, A.J., & Robbins, J. (2009). Senescent swallowing: Impact, strategies, and interventions. Nutrition in Clinical Practice, 24, 395–413. doi:10.1177/0884533609332005,
- Perry, L. (2001). Screening swallowing function of patients with acute stroke. Part one: Identification, implementation and initial evaluation of a screening tool for use by nurses. Journal of Clinical Nursing, 10, 463–473. doi:10.1046/j.1365-2702.2001.00501.x
- Robbins, J., Hamilton, J.W., Lof, G.L., & Kempster, G.B. (1992). Oropharyngeal swallowing in normal adults of different ages. Gastroenterology, 103, 823–829. doi:10.1016/0016-5085(92)90013-O
- Rofes, L., Arreola, V., Romea, M., Palomera, E., Almirall, J., Cabre, M., … Clave, P. (2010). Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterology & Motility, 22, 851–858, e230. doi:10.1111/j.1365-2982.2010.01521.x
- Sarve, A.R., Krishnamurthy, R., & Balasubramanium, R.K. (2021). The timed water test of swallowing: Reliability, validity, and normative data from Indian population. International Journal of Health Sciences, 15, 14–20. https://www.ncbi.nlm.nih.gov/pubmed/33708040
- Serra-Prat, M., Hinojosa, G., Lopez, D., Juan, M., Fabre, E., Voss, D.S., … Clave, P. (2011). Prevalence of oropharyngeal dysphagia and impaired safety and efficacy of swallow in independently living older persons. Journal of American Geriatric Society, 59, 186–187. doi:10.1111/j.1532-5415.2010.03227.x
- Serra-Prat, M., Palomera, M., Gomez, C., Sar-Shalom, D., Saiz, A., Montoya, J.G., … Clave, P. (2012). Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in independently living older persons: A population-based prospective study. Age Ageing, 41, 376–381. doi:10.1093/ageing/afs006
- Shaheen, N.J., Madanick, R.D., Alattar, M., Morgan, D.R., Davis, P.H., Galanko, J.A., … Vaughn, B.V. (2008). Gastroesophageal reflux disease as an etiology of sleep disturbance in subjects with insomnia and minimal reflux symptoms: A pilot study of prevalence and response to therapy. Digestive Diseases and Science, 53, 1493–1499. doi:10.1007/s10620-007-0057-1
- Smithard, D.G., O'Neill, P.A., Park, C., Morris, J., Wyatt, R., England, R., & Martin, D.F. (1996). Complications and outcome after acute stroke. Does dysphagia matter? Stroke, 27, 1200–1204. doi:10.1161/01.STR.27.7.1200
- Stoschus, B., & Allescher, H.D. (1993). Drug-induced dysphagia. Dysphagia, 8, 154–159. doi:10.1007/BF02266997
- Tracy, J.F., Logemann, J.A., Kahrilas, P.J., Jacob, P., Kobara, M., & Krugler, C. (1989). Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia, 4, 90–94. doi:10.1007/BF02407151
- Wu, M.C., Chang, Y.C., Wang, T.G., & Lin, L.C. (2004). Evaluating swallowing dysfunction using a 100-ml water swallowing test. Dysphagia, 19, 43–47. doi:10.1007/s00455-003-0030-x
- Yoshikawa, M., Yoshida, M., Nagasaki, T., Tanimoto, K., Tsuga, K., Akagawa, Y., & Komatsu, T. (2005). Aspects of swallowing in healthy dentate elderly persons older than 80 years. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 60, 506–509. doi:10.1093/gerona/60.4.506
