Abstract
Purpose
The healthcare experience is a multifaceted and varied process, particularly for people living with complex conditions such as primary progressive aphasia (PPA). Different experiences influence pathways through the health system, impacting client outcomes. To our knowledge, no previous studies have directly explored the healthcare experiences of people with PPA and their families. This study aimed to explore the experiences of people living with PPA from the perspective of both the person with PPA and their families during diagnostic and post-diagnostic phases, and to identify factors influencing service access and perceptions of quality of care.
Method
The study followed an Interpretive Phenomenological Analysis (IPA) approach. In-depth, semi-structured interviews were completed with three people with PPA and their primary care partner, and two further care partners of people with PPA.
Result
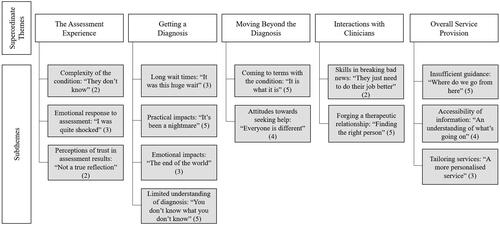
Five superordinate themes were identified: characterising the assessment experience, getting a diagnosis, moving beyond the diagnosis, participant interactions with clinicians, and overall service provision. The five superordinate themes comprised 14 subthemes.
Conclusion
The study provides preliminary insights into the complexity of the PPA healthcare journey, and the need for increased accessibility of information and supports following diagnosis. The findings inform recommendations for improving quality of care and the development of a PPA service framework or care pathway.
Introduction
The healthcare experience is a multifaceted and varied process, particularly for people living with complex or rare medical conditions such as primary progressive aphasia (PPA; Samsi et al., Citation2014). Different experiences influence the pathway taken through the health system and consequently the quality of care and outcomes achieved (Prorok et al., Citation2013). It is not uncommon for people living with PPA and their families to express concerns regarding the amount of information and support received following a diagnosis, as well as challenges in locating health professionals who understand their condition and evolving support needs (Beales et al., Citation2019; Davies & Howe, Citation2020). Identifying factors influencing satisfaction with services is important to optimise healthcare experiences. To our knowledge, no previous studies have directly explored how people with PPA and their families experience the healthcare system.
PPA is a neurodegenerative syndrome that results in declining language due to the degradation of the language networks of the brain (Mesulam, Citation2013). There is limited information internationally on the prevalence of PPA, however, one study in the UK estimated the prevalence to be between 3 and 4/100,000 people (Coyle-Gilchrist et al., Citation2016). There are three main PPA subtypes, namely, the semantic, non-fluent, and logopenic variants (Gorno-Tempini et al., Citation2011). Based on consensus criteria, each variant is characterised by a specific profile of language impairment and relative strengths (Gorno-Tempini et al., Citation2011). The underlying pathology is heterogenous and people with PPA may present with symptoms overlapping with other dementia subtypes such as the amnestic variant of Alzheimer’s disease, or motor speech disorders such as apraxia of speech (Henry & Grasso, Citation2018). While memory and other cognitive difficulties emerge and increase over time, the language symptoms typically remain the most salient throughout the course of PPA (Foxe et al., Citation2021; Mesulam, Citation2013).
The onset of PPA in most individuals occurs before the age of 65, such that it is recognised as a form of younger onset dementia (Mesulam, Citation2013). Due to the younger age of onset and prominent language symptoms, individuals with PPA are frequently faced with a unique set of social, personal, financial, and/or emotional issues (Rogalski & Khayum, Citation2018). For instance, premature retirement from work can result in financial strain and have practical implications for families (Kaiser & Panegyres, Citation2007). Furthermore, the time between onset and diagnosis can be longer for individuals with younger onset PPA due to language symptoms being dismissed as stress- or depression-related, rather than associated with emerging dementia (Davies & Howe, Citation2020). A prolonged diagnostic search may require an individual to consult multiple specialists before PPA is recognised (Prorok et al., Citation2013). Delayed diagnosis can result in uncertainty, as well as anxiety and distress, given that people with PPA are often acutely aware of the emerging language changes and seek solutions in response to their concerns (Samsi et al., Citation2014).
Diagnosis of PPA
First contacts with the health system typically involve the person with PPA approaching their general practitioner (GP) or a medical specialist with concerns relating to language (Prorok et al., Citation2013). Once initiated, the diagnostic assessment process usually involves a battery of tests, neuroimaging, and a series of other medical investigations (Nickels & Croot, Citation2014). For an accurate clinical diagnosis to be made, neuropsychological assessments are often recommended in conjunction with comprehensive language assessment and the medical team is then tasked with delivering diagnostic and prognostic information to the client (Volkmer et al., Citation2020). People with dementia and their families have raised concerns about how diagnostic information is conveyed, resulting in uncertainty about the future and lack of direction regarding where to go next (Quinn et al., Citation2008). In a study on prognostication in post-stroke aphasia, Cheng et al. (Citation2020) highlighted the sensitivity required in communicating prognostic information and considering a person’s current and evolving needs. In the context of PPA, prognostication can be particularly challenging due to the variable and complex nature of the syndrome (Henry & Grasso, Citation2018; Volkmer et al., Citation2023). Although several studies have investigated evidence-based guidance and support for prognostication in post-stroke aphasia and the broader dementia literature, to our knowledge, such guidelines are not available in the context of PPA. The way in which diagnoses are communicated, however, is critical in setting up subsequent healthcare trajectories (Cheng et al., Citation2020).
The assessment experience
Assessment is a key part of diagnosing PPA and tracking the evolution of the clinical syndrome and its functional impact over time (Foxe et al., Citation2021; Sapolsky et al., Citation2011). As such, the phenomenon of being assessed should be understood as a critical component of the healthcare experience of people with PPA. Keady and Gilliard (Citation2002) explored the assessment experience from the perspectives of people with dementia and their supporters, revealing that they often felt uncomfortable and disempowered during the assessment process. Interestingly, the assessment process was equated with "playing a game" (p.16), where the rules of participation had not been made clear, resulting in the person with dementia feeling "trapped" during assessment tasks where the required "moves" were not known (Keady & Gilliard, Citation2002). Such experiences were associated with emotional reactions, including fear, distress, and anxiety, as well as a desire to disengage or retreat from the assessment process, all responses that would likely impact the therapeutic relationship and quality of information gathered. These findings highlight the need for more person-centred and supportive approaches to assessment, which have been discussed in dementia, post-stroke aphasia, and PPA literature (Hersh et al., Citation2013; Keady & Gilliard, Citation2002; Volkmer et al., Citation2023).
In the speech-language pathology field, there has been a shift towards more dynamic and collaborative assessment processes that focus on the identification of strengths, resources, and support needs of individuals and their families, congruent with the World Health Organization’s International Classification of Functioning, Disability and Health Framework (World Health Organization, Citation2001). In doing so, the focus is shifted from simply looking at linguistic changes or symptoms to considering the broader impact of PPA on an individual’s communication, interpersonal relationships, daily activities, and life roles (Davies & Howe, Citation2020). Consistent with a life participation approach to assessment, this allows collection of information about impairment to inform differential diagnosis, while ensuring assessment moves beyond diagnosis to inform proactive and responsive care planning (Henry & Grasso, Citation2018).
While person-centred assessment processes pave the way for personalised management and intervention, as well as informing prognostication, counselling, and tailored education across the continuum of care (Henry & Grasso, Citation2018; Volkmer et al., Citation2023), it is not clear whether individuals with PPA and their family members perceive the assessment process to be of benefit beyond receiving a diagnosis. To our knowledge, no previous studies have directly explored the assessment experience of people with PPA, despite this being an essential component of the healthcare journey.
Post-diagnostic support
The onset of PPA can be physically and emotionally demanding for an individual and the people around them, impacting quality of life and psychosocial wellbeing (Ruggero et al., Citation2019). Studies have shown, however, that following diagnostic assessment and first contacts with the health system, individuals with PPA and other types of dementia are not routinely offered proactive post-diagnostic support, including referral to speech-language pathology services (Volkmer et al., Citation2020), leading to feelings of confusion, frustration, and prolonged uncertainty (Davies & Howe, Citation2020). Better access to comprehensive and well coordinated post-diagnostic support is being increasingly advocated for by individuals with PPA and other types of dementia (Low et al., Citation2018).
As language difficulties are the most prominent feature of PPA, speech-language pathology services are often a priority for individuals and their families. In accordance with the framework of person-centred healthcare, empowering individuals to understand their condition, including the nature of language and communication support needs, can build the capacity to solve problems as they emerge, and engage individuals and families in care planning (Khayum et al., Citation2012; Molony et al., Citation2018). Previous qualitative studies have highlighted the benefits of early access to education and rehabilitation-focused strategies for people with PPA and their family members (Beales et al., Citation2019; Kaiser & Panegyres, Citation2007). Not all clients, however, receive such services due to a lack of clear care pathways in the healthcare system (Beales et al., Citation2019). Previous research by Prorok et al. (Citation2013) has explored how people with dementia experience healthcare services in Australia (Prorok et al., Citation2013), identifying themes of uncertainty and difficulty accessing services and support. The experiences of people with PPA were not examined specifically, such that it remains unclear whether individuals with PPA perceive the diagnostic and post-diagnostic services they receive to be person-centred and responsive to their needs, as well as easily accessible. Understanding these experiences may inform the development of a care pathway for PPA that offers clarity and continuity of care. Clearly defined care pathways have been advocated for in the broader dementia literature to act as navigational aids and promote integrated care between health professionals (Samsi & Manthorpe, Citation2014).
Aims of the study
The aims of this study were to explore the diagnostic and post-diagnostic healthcare experiences from the perspectives of people living with PPA and their families, and their experiences of being assessed by health professionals across the continuum of care. The study sought to identify factors influencing satisfaction with healthcare experiences to inform strategies to enhance the healthcare journey of people living with PPA.
Method
Research design
This study followed a qualitative research design guided by the principles of Interpretative Phenomenological Analysis (IPA) to explore the lived experiences of participants (Smith et al., Citation2009). The IPA approach allowed exploration and discussion of findings with regard to how they may relate to current service provision, rather than focusing on testing a theory or hypothesis (Smith et al., Citation2009). The study focused on the healthcare experiences of people diagnosed with PPA and their family members, including the experience of being assessed by health professionals. This study was conducted in Perth, Western Australia. In-depth, semi-structured interviews were utilised to facilitate rich insights into the participants’ perceptions of healthcare services received and their interactions with health professionals.
Participants
Eight participants took part in this research, with five interviews completed. Three interviews were conducted with people with PPA alongside their primary care partners, and two interviews were conducted individually with the care partners of people with PPA. IPA studies require small sample sizes of 15 or fewer participants to ensure individual voices and experiences are sufficiently represented in the analysis (Scantlebury et al., Citation2018; Smith et al., Citation2009). Previous IPA studies exploring the experiences of people with early-stage dementia have reported similar sample sizes of seven to eight participants (Frazer et al., Citation2012; Lee et al., Citation2022).
Participants were recruited through purposeful sampling via four different private health professionals with experience working with people with PPA (e.g. neurologists, speech-language pathologists). Each participant’s diagnosis of PPA and their capacity to provide informed consent was confirmed by the treating specialist prior to recruitment. Standardised language assessments were not completed as part of the study, however, all participants had undergone comprehensive diagnostic evaluation, including brain imaging with their neurologist and in accordance with international consensus criteria (Gorno-Tempini et al., Citation2011). For context, in the research location multi-disciplinary diagnostic services are available in the public health system through a specialised neurosciences unit, as well as neurology and memory clinics attached to tertiary and secondary hospitals. Diagnostic services can also be accessed through the private system with a small number of neurologists identifying expertise and interest in PPA and other rare, younger onset dementias. Most of the diagnostic services provide annual reviews, however, ongoing management is more commonly provided through private speech-language pathology services. Some public outpatient services offer time-limited individual and group based intervention services for people with PPA, however, at the time of this study there was not a consistent pathway of care. Participant demographic information is set out in . For participants to be included in the study, they were required to have a diagnosis of any variant of PPA and to speak conversational English. Exclusion criteria were the presence of severe expressive and receptive language difficulties, as determined by the treating speech-language pathologist, that would prevent the individual from understanding and responding to interview questions.
Table I. Participant demographic data.
P1 and F1
P1 was a man diagnosed with non-fluent variant PPA a year prior to the study. He presented to his GP with concerns about his speech and was seen by three different neurologists to confirm his diagnosis. P1 was interviewed with his partner, F1, at their home. P1 responded to questions appropriately, with relative strengths in auditory comprehension. He presented with non-fluent, hesitant, and effortful speech production, and evidence of apraxia of speech. P1’s responses were typically short (e.g. "It’s… that’s… never stop learning. That’s the g… goal.") and he frequently deferred to his partner during the interview, who consistently checked that he agreed with her reflections on their healthcare experiences.
P2 and F2
P2 was a man diagnosed with logopenic variant PPA four years prior to the study. P2 first noticed there was a problem with his language when he was at work, which led him to see a GP for assessment. He was referred to a neurologist who diagnosed PPA. P2 was interviewed together with his wife, F2, in their home. P2 contributed actively to the interview and was able to follow the questions. He occasionally sought repetition or clarification for longer questions. P2 required additional time to formulate his responses due to word finding difficulties and the concentration needed to hold onto and organise his thoughts (e.g. "I don’t generally know lots of… it wasn’t sort of… um… what would you say? Hardest to get my words out and so I just found it…").
P3 and F3
P3 was a woman diagnosed with semantic variant PPA five years prior to the study, after raising concerns about language loss and difficulty finding words to her GP. P3 was interviewed together with her husband, F3, in their home. P3 presented with fluent speech that lacked specific meaning with prominent word finding difficulties. Her word comprehension difficulties resulted in frequent requests for clarification of specific words and formulation of off-topic responses (e.g. "Process? Yeah, crazy George!"). Supported conversation techniques (e.g. using Google images and gestures to show or demonstrate word meanings, writing keywords down, and re-stating questions with alternative words) were used to help P3 understand questions and specific words during the interview. P3 wrote words down in a notebook during the interview, such as topics of conversation and words she did not recognise, to support her comprehension and to keep track of information.
F4
F4 was a man whose wife was diagnosed with non-fluent variant PPA four years prior to the study. He requested to be interviewed outside the home, as his wife was not able to participate in the study due to being unable to provide informed consent. His wife’s treating speech-language pathologist confirmed that she was non-verbal due to severe apraxia of speech and would find it difficult to respond to the interview questions, despite having relative strengths in auditory comprehension. F4 and his wife had consulted neurologists, psychologists, and speech-language pathologists across their journey with PPA. In the early stages, they had seen multiple medical specialists with no diagnosis given. Approximately five years into this process, brain scans were carried out at the request of a neurologist and a diagnosis of PPA was made.
F5
F5’s husband was diagnosed with semantic variant PPA approximately nine years prior to the study. Her husband first became aware of his language changes and sought a referral to a neurologist. F5 attended the initial appointments, however, her husband progressed through the diagnostic assessment process on his own. The interview was completed in the couple’s home. Only F5 was present and participated in the interview due to her husband being unable to provide informed consent. His treating speech-language pathologist confirmed that due to severe word comprehension and word finding difficulties, he would not have been able to participate in the interview.
Materials
A Sony Handycam and tripod were used to video record interviews for later transcription with participants who consented to be videoed. For participants who did not consent to being video recorded, audio was recorded using a digital voice recorder. NVivo (QSR International Pty Ltd, 2020) was used in the coding of interview transcripts.
Procedure
In-depth, semi-structured interviews were conducted by the first author who was an Honours student in the final year of an undergraduate speech-language pathology degree. Interview training was provided, noting the interviewer had prior experience working with people with aphasia and their families. Additional strategies, information specific to PPA, and ongoing support throughout the data collection process were provided by the final author, a speech-language pathologist with extensive clinical and research experience in the PPA field. The interview framework was guided by previous studies involving people with PPA (Beales et al., Citation2019) and post-stroke aphasia (Luck & Rose, Citation2007), as well as published recommendations for conducting qualitative interviews (Tong et al., Citation2007). Open-ended questions were used and supported by prompts listed in the interview guide (see Supplementary Material), encouraging a detailed and rich description of the participants’ healthcare experiences. These questions included a combination of descriptive, evaluative, and narrative-type questions.
Interviews took on average 73 minutes (range 55–98 minutes) to complete. All interviews were completed in the participant’s own home, with the exception of F4 who requested that the interview be completed at a location away from their home given that his wife was unable to participate. The interview with F4 was completed in a private and quiet university meeting room. Where the individual with PPA and their partner were interviewed together, the interviewer addressed questions to the person with PPA first, before asking for input from their care partners. Supported communication strategies, such as sentence starters and yes/no question probes, were utilised when required, and understanding of questions and responses was frequently checked. Prior to each interview, a positive relationship was established with the interviewer using relational strategies to create a safe space for participants to share their thoughts and experiences openly.
Data analysis
Interviews were transcribed verbatim by the first author. Transcripts were de-identified and potential sources of identification were removed. Analysis of transcripts was guided by the IPA process described by Smith et al. (Citation2009) to extract appropriate depth and detail from the interviews. Transcripts were read multiple times before free textual analysis commenced, and superordinate themes and subthemes were derived. Individual transcripts were analysed first to ensure a deep understanding of each experience before integration across transcripts. Regular meetings were held between members of the research team throughout coding and analysis to reach a consensus and ensure the process was grounded in the data. Finally, a summary of superordinate themes and subthemes identified in each interview was sent to the respective participants for review and member checking, with examples and dot points to explain each theme. No changes were requested. The IPA approach followed is provided as supplementary information.
Qualitative rigour
The topic guide was informed by recommendations from the qualitative literature (Tong et al., Citation2007) and credibility was achieved by documenting the research process, including notes and transcripts. Bracketing of prior experiences and preconceptions was considered and discussed as a research team. Each interview was coded carefully to capture as far as possible the experiences discussed by the couple before moving to the next one. The interviewer kept a reflexive journal throughout data collection and analysis, noting initial reflections and other information gathered during the interview, and discussed key ideas with other members of the research team on a regular basis. The interviewer had not previously met any of the participants. Four of the five individuals with PPA involved in this study were known to the last author, which may have influenced how they talked about their experiences with speech-language pathology services. The final author was not, however, involved in the interview process and the participants were aware that their comments would not affect their care or be identifiable in any way. Further, the interviews were intended to convey their full experience of services across the journey of care. The participants indicated a willingness to share their experiences and to give their feedback in a respectful context so that other people with PPA and their families may benefit in the future. Dependability was facilitated by members of the research team with experience in the IPA process, who reviewed the analysis and codes for consistency and accuracy (Luck & Rose, Citation2007). Coding of individual transcripts were each revised twice and superordinate themes across all transcripts were revised four times, informed by reflexivity and continued discussions with the research team. Confirmability was ensured throughout the interview process, with the interviewer seeking clarification where responses were unclear and to check that what was recorded was what participants meant. Transcripts were regularly revisited, ensuring accurate interpretations of responses. Confirmability was further achieved through the member checking process, with participants having the opportunity to validate interview findings.
Result
Analysis of the five interviews produced five superordinate themes and 14 subthemes. An overview of the superordinate themes and subthemes is set out in . Each superordinate theme is expanded into subthemes and discussed in detail. Illustrative quotes are included to help define each subtheme.
The assessment experience
This first theme related to participant accounts of their assessment experiences. Participants did not speak specifically about assessment sessions with speech-language pathologists but instead recounted assessment experiences that were associated with diagnostic and review appointments with their neurologist or medical specialist.
Complexity of the condition: “They don’t know”
Complexity associated with the PPA syndrome was described in four of the interviews and was perceived to influence the assessment experience. Participants reported seeing multiple doctors for assessment before PPA was diagnosed. P1 recalled that initially their GP told them to wait and see, however, as they were concerned about P1’s language symptoms, they visited another GP who prompted the initial diagnostic evaluation. F1 recalled the second GP’s response, "…he said, no you don’t let it go, we investigate further".
Due to the rare and complex nature of PPA, participants reported that they faced uncertainty from the medical specialists whom they saw during the assessment process. F4 recounted, "…they thought it might be psychological, some issue", failing to identify the neurodegenerative cause of his wife’s language changes. He and his wife later met with a group of neurologists in a grand round setting, but they were unable to reach a clear conclusion regarding the diagnosis, "so we had all these professional neurologists sitting around and didn’t know what it was… it’s pretty uncommon apparently".
The complexity of PPA also meant that the diagnosis could change over time. For example, P1 and F1 relayed that although they were under the management of a neurologist well-versed in PPA they faced a changing diagnosis, being initially told that P1 had the non-fluent variant of PPA and subsequently Alzheimer’s disease. Upon further review by the same neurologist, P1’s diagnosis was revised back to non-fluent PPA, with F1 recounting, "…then they came back and said no, Alzheimer’s is not the next step, and it’s two different diseases". The diagnostic confusion was described as a significant source of distress for P1 and his family, prompting them to seek the opinion of another neurologist who confirmed the original diagnosis.
Emotional response to assessment: “I was quite shocked”
Participants who spoke directly about the process of being assessed expressed a range of different feelings and emotions. For example, F3 reported that assessments exposed deficits in his wife that he had not previously noticed, recalling, "I didn’t realise until she was tested in front of me, with images, of camels or something. P3 did really badly. She hardly knew anything; I was quite shocked". For some people with PPA, the diagnostic assessment process was overwhelming which was, in turn, difficult for family members to witness. F5 recounted, "I’ve seen him get a bit like, looks as if he’s cornered in a questioning, you know, interview kind of situation". This perspective was corroborated by F2 who explained, "…because he came out of there quite, almost distressed". P2 recounted the experience, "I just… I just… do what you gotta do, just tell me. I don’t know what’s happening really", expressing a lack of control during the assessment process.
Perceptions of trust in assessment results: “Not a true reflection”
Two of the care partners repeatedly stated that the assessments conducted did not accurately reflect the abilities of the person with PPA, given the manner in which the assessments were conducted. For example, F2 recalled, "whatever that assessment, whatever that was, that was not a true reflection of P2" and "whatever they did, whatever the results were, would not have been true results". F2 and P2 identified a range of factors that influenced assessment performance, including unfamiliarity of the assessor, failing to establish rapport prior to test administration, and where the purpose of the assessment task was not explained. F5 felt that similar factors impacted her husband’s performance during assessment sessions, reporting, "He might have done better if he had understood" and "I saw him sort of… kinda retreat? Just not try or bother".
Getting a diagnosis of PPA
The second superordinate theme related to participants' accounts of receiving the diagnosis of PPA, elaborated in four separate subthemes.
Long wait times: “It was this huge wait”
Three participants reported long wait times before they were able to see a specialist to get a diagnosis. P1 recalled, "it was this huge wait" and "it was over a year to see a specialist, from the time they first noticed an issue". Likewise, F2 reported that while they were given the diagnosis at their second appointment, this had been preceded by a lengthy wait, "…which was like I said about eleven months later". Participants reported that knowing something was not right but not being able to put a name to it was a source of frustration.
Practical impacts: “It’s been a nightmare”
All participants described how the onset and diagnosis of PPA had disrupted their lives in some way. For example, F4 reported, "…because of her condition she can’t do anything. So I do everything. Every single thing, um which is unfortunate". F4 reported that the reduced independence as a result of the progression of the disease was a major change in their lives and their relationship. Care partners also described the impact of PPA on the person’s ability to continue work, requiring a range of financial and logistical decisions to be made. F1 recounted, "it’s been a nightmare for us" and "we’ve just spent all of 2020 and to now trying to figure out how to get [P1] out of the business, how do we sell the business, um how do we keep the business going?". Likewise, F3 reported that P3 "…had to give up work and all those sorta things so that was difficult for her too". F5 recalled that her husband continued to work even after the diagnosis but qualified this by stating, "my daughters and I used to look at him and think ‘how, how is he managing?'".
Emotional impacts: “The end of the world”
All participants talked about the profound emotional and psychological impact of receiving a diagnosis of PPA. Three participants recounted the emotional ramifications on the person with PPA, as well as the people around them. F2 recalled, "he was extremely depressed. Um he stopped ringing people, talking to people, just basically, [P2] shut down. Like really badly". F2 reported feeling "…quite worried, scared, concerned for him". Similarly, F3 recalled, "it was all a bit of a shock and um I think we got a bit tearful".
F1 was initially told that he had Alzheimer’s disease and recounted, "so when we left that appointment, it was like the end of the world". The uncertainty and prospect of losing his memory took a toll on P1, noting that this change in diagnosis had made P1 "…even more upset" and more confused about his prognosis. When the diagnosis was reverted to non-fluent PPA they indicated that this was met with some relief.
The diagnosis and uncertainty about the future had an impact on other family members. F1 brought up the emotional impact of the diagnosis on their son, stating "his whole year 7 year 8 and first semester of year 9 has just been a downward spiral and his grades have just totally gone off the cliff", as the whole family had to come to terms with the situation and the lifestyle changes it would bring. Similarly, F3 stated, "it’s been very hard on the kids", seeing how their mother had been impacted by PPA.
Limited understanding of diagnosis: “You don’t know what you don’t know”
Participants highlighted how, after receiving a diagnosis, there was a lack of information conveyed to them about the condition and how it might progress. All participants reported being unsure of what to expect in the future. F1 stated, "we were a bit confused as to what, what does this mean". Similarly, F2 explained, "because you also have to understand, that you don’t know what you don’t know". She recounted that their knowledge was limited, which resulted in them not knowing what questions to ask to get information they would need.
In the case of F4, he perceived that the various healthcare professionals they saw also had a limited understanding of the condition. F4 reported, "it would have been nice to understand that at the start, but no one knew [shrugs]". Further, F4 recalled that the speech-language pathologists provided services for some time, however, they reached a point where they were not able to offer anymore, referring them on or turning them away.
Participants expressed that they needed more information to understand the diagnosis. F5 reported, "I want to optimise. I want to make the most of opportunity, I want information". Participants often looked to the internet for answers. F2 recalled, "but once he got his diagnosis because he didn’t know anything about his diagnosis. He did get on to Google and ask doctor Google". F3 also looked for information online, stating, "I don’t know. I read up a lot of these things and then I stopped reading", finding it overwhelming.
Moving beyond the diagnosis
The third superordinate theme encapsulated moving beyond the diagnosis, incorporating participants’ reactions to the diagnosis, as well as different attitudinal positions adopted by the participants in seeking support.
Coming to terms with the condition: “It is what it is”
All participants talked about their feelings towards and eventual acceptance of the PPA diagnosis. F1 reported, "it is what it is, it’s not good, but it is what it is, and just get on with it". P2 echoed this sentiment, stating "it is what it is, we can’t do anything about it, so, move on!". F5 also said, "you know, there’s nothing you can do! So just get on with it". Participants acknowledged that the condition would inevitably change their lives and chose to keep moving forward. Similarly, F4 said "but it is what it is, you know. We couldn’t… we knew we couldn’t…well we didn’t know but we understood we couldn’t do anything about it.… we knew we couldn’t get back". F3 spoke in a similar manner, highlighting acceptance of the incurable nature of PPA, saying, "I suppose um that was one of the difficulties, to accept that there’s no treatment, except for a few lifestyle [changes]". It was evident that some participants came to terms with the diagnosis once they had reached a sound understanding of the condition. For example, F1 recalled, "we knew what the diagnosis was and so we knew we were in for probably the long haul".
Attitudes towards seeking help: “Every case is different”
Participants had different attitudes towards seeking support in their PPA journey, reflecting the complexity of the healthcare experience. As F2 aptly put it, "every case is different". Some participants had a more proactive approach to help seeking. F5 recounted, "I would initiate phone calls. Every four or five months" and "without a referral, I looked her up and tracked her down". F5 attributed this to "…want[ing] to make the most of opportunity, I want information". P1 and F1 took a similar approach and called up speech-language pathologists for appointments, stating, "so I suppose that we just felt that we were being proactive and were happy with that". P3 recognised the need to seek help with management of the condition, recalling, "it took a while I think for it to sink in that we had to start thinking about that she’s gonna need some services". Another participant had a more independent outlook. F2 reported, "…very much, I don’t need this. I don’t need other people’s help. I’m fine".
Participants felt that they needed to take initiative to obtain relevant information and self-advocate. F5 recalled, "we’ve kinda done it on our own… I’m resourceful. We have resources". For F1, the ability to self-advocate and become more assertive developed over time, emphasising, "we’ll sit down and we’ll ask them direct. Answer that question, that’s all we want. And then we can go from there". Being proactive was not easy for everyone; F3 reported, "you don’t understand what you need to ask. To be able to understand what it is that they expect you to know".
Interactions with clinicians
The fourth superordinate theme set out the participants’ perspectives on interactions with health professionals throughout their healthcare journey and how these contributed to satisfaction, or dissatisfaction.
Skills in breaking bad news: “They just need to do their job better”
Three participants recounted health professionals’ skills in breaking bad news and their perceptions of bedside manner. Two participants felt that specialists were too blunt when delivering diagnostic and prognostic information. F1 suggested, "they just have to do their job better. That’s all. They are dealing with people’s lives". P1 reported, "just that careless, you know, just that careless few words". F1 also emphasised that the way the specialist broke the news to them left much to be desired and "…could have set [P1] up on a much better journey moving forward, and it’s just ruined everything for him".
Similarly, F3 recalled, "well so one thing that she probably remembers is that she was told that she was gonna die [laughs]". P3 recounted that she "…felt a bit stressed with her [neurologist]" due to her "…saying to me that I was going to die straight away. She said that". The way in which the news was broken to them had a lasting impact.
Forging a therapeutic relationship: “Finding the right person”
Participants brought up the importance of being able to connect with the health professional and finding the right fit. For example, P1 reported, "you can go a decade going to one counsellor, one psychologist to another before you find someone you connect with. And [P1] connected with him straight away". Similarly, P2 said, "…and it’s like finding the right person, to go with the person. And it just works, and there is no reason, it just works". F2 highlighted the importance of forging a relationship with the clinician prior to commencing clinical procedures, such as diagnostic assessments, stating "you need a few minutes of talking to someone to allow them to… assess you".
Four participants emphasised the importance of health professionals showing empathy, being positive, and having time to listen. F1 said, "I think you like her because she is so positive". P1: "Yeah [nods], yeah. Lovely person". F4 valued leaving appointments and not feeling "shortchanged". Participants also valued honesty of clinicians, with F3 reporting, "…so, I think having that honest opinion has been important".
Conversely, poor communication from health professionals posed a detriment to the therapeutic relationship. F1 recalled instances where their expectations of the session were not met, stating "I didn’t understand the purpose of that meeting, it didn’t go the way I thought it would". On another occasion, "it was just going there, and they asked how he was and if he had any questions. And that was it". F1 also stated, "…cos there’s no treatment, it’s like there is no hope, they don’t offer, it’s just like when you come in, how are you, do you have any questions? No, I don’t have any questions". F1 and P1 had hoped that the specialist would give them more direction or concrete actions to take. F2 shared a similar sentiment, reporting, "look, this sounds really nasty, my attitude towards it is… ‘okay, how are you doing? Bye, 320 bucks, thanks!’". In some cases, appointments were described as a "…complete waste of time" (F1).
Service provision
The final superordinate theme of service provision captured participants’ perspectives on information and support given from health services throughout their journey, what they valued, and what could have been improved upon.
Insufficient guidance: “Where do we go from here”
Participants expressed needing more guidance throughout their journey. F1 stated,
“if it could come together and have someone to contact if you wanted to know something, if we wanted to know what are the services that are available, well we wouldn’t know who to ask that" and "I think it would be better if there was some sort of… if it worked in unison somehow”.
Similarly, F2 recounted:
“For me to ask him on more than one occasion, where do we go to from here? And be basically to be told, you do know it has no cure, is about as useful as an ashtray on a motorbike! It ain’t much damn use!”
They could direct you in the… in the right direction. [mimes diverging of paths]. They could say well you don’t need to go to a psychologist and spend thousands of bucks seeing him. You should go to a speech therapist and spend thousands of bucks seeing her! [chuckles].
Accessibility of information: “An understanding of what’s going on”
Participants found accessing information challenging. F1 reported,
“it would be good if all those resources would be in one spot which you could call up and you could get some information”.
F2 suggested,
“there needs to be a place for the people that are going through it to get real information”
and
“I suppose what I’m trying to get across is, there needs to be a, an information pack. Not for them to read right then, but for them to be able to access. Even if it’s to take it home and read it later”.
Participants felt that having a centralised source of reliable information would increase ease of access and facilitate timeliness. Although there was information on PPA online, the sheer quantity was overwhelming. F2 recounted, “he did get on to Google and ask doctor Google. And I think that was part of the reason that he was in such a shitful depression. Such a shitful depression”. Moreover, not all information was relevant to them. F3 reported, “…particularly in Australia, a lot more in America, I noticed, for PPA. Massive amounts of… more information”. F3 also reported having to sift through a large quantity of information online before he could find something useful.
Tailoring services: “A more personalised service”
Participants valued being offered services they felt were tailored to them. F1 reported, “I just wish we could go back to [neurologist one]. Because he just got a small practice and he… it would be a more personalised service” compared to the larger service they attended. However, they did not always feel like they had a choice, as they were directed to the recognised specialists in the field. At the larger service, F1 and P1 recalled feeling that that they were “…very much a number that will not be remembered the next time you come round”.
Participants valued being given activities tailored to the individuals’ personality and unique needs. F1 recalled, “I think [the speech-language pathologist] understood how much [P1] liked to tell his stories. So, she changed the sessions that they have”. Activities that were not perceived to be suited to the participant were not perceived positively. F2 recalled, “I think she was more geared towards children because it was young children’s work”. This led P2 and F2 to seek the services of another speech-language pathologist who they felt used a treatment approach more tailored to F2, with P2 reporting that he “looks forward to” those sessions.
F5 reported dissatisfaction with being offered an online appointment, stating “[he]can barely talk when he’s in the room! Zoom’s not gonna work, thank you very much, no thank you. And we’ve never been back”. P1 and F1 also mentioned preferring face-to-face appointments over telehealth appointments, reflecting the need for personalised services extending to modes of service delivery.
Discussion
This study explored the healthcare experiences of people living with PPA and their families, as well as factors influencing perceptions of quality of care around the diagnostic and post-diagnostic process. The rich insights coalesced into five superordinate themes relating to the assessment experience, getting a diagnosis, moving beyond the diagnosis, interactions with clinicians, and service provision. The findings highlighted that while people with PPA and their care partners have significant support needs, they can experience a range of barriers to accessing and receiving quality healthcare calling for clearer care pathways and better access to supportive and personalised post-diagnostic services.
Healthcare experiences
The healthcare experiences of individuals with PPA and their families were characterised by complexity and emotional upheaval, with a range of factors influencing healthcare access and quality. Long wait times, extended periods of uncertainty, and confusion were described, associated with the rare nature of PPA and lack of awareness of the condition. Consistent with previous research, the participants experienced changing diagnoses, as well as misdiagnosis, with early language symptoms associated with a psychological cause or dismissed as work-related stress, rather than emerging dementia (Kaiser & Panegyres, Citation2007; Samsi et al., Citation2014). The findings highlight the need for more streamlined and coordinated services, with a focus on identifying and responding to individual expectations and support needs at particular points in time. Greater transparency and signposting are required to help people with PPA and their families make sense of the referral and diagnostic process while providing direction and options regarding where to go next. Changes are required at the level of the healthcare provider and healthcare system, raising awareness of PPA and articulating care pathways and resources that facilitate timely diagnosis and access to support services, to help people respond proactively to the practical and emotional impacts of PPA that have been consistently described here and in the broader PPA literature (Davies & Howe, Citation2020; Kaiser & Panegyres, Citation2007; Ruggero et al., Citation2019).
Assessment experiences
Being assessed is a critical component of the PPA healthcare experience, to both inform diagnosis and track progression over time. The participants in this study associated the process of assessment with their neurology appointments and were less inclined to recall specific assessment experiences with their speech-language pathologists or other allied health professionals. Similar to the findings of Keady and Gilliard (Citation2002), assessments were not recalled positively but rather were associated with lack of control, unmasking of difficulties, and feeling ‘cornered’ during the assessment process. Given the way assessments were conducted, the participants did not always feel that they provided a true reflection of the individuals’ capabilities. Participants reported that expectations around assessment were not always made clear and that assessments were not routinely administered, even when they were seeking objective information about the progression of symptoms. It was also evident that people attached different meanings to the various dementia syndromes, particularly those that are less familiar. This was highlighted in the case of P1 who described a sense of relief when his diagnosis of Alzheimer’s disease was reverted to non-fluent variant PPA and further related to the theme You don’t know what you don’t know. The findings highlight the need for more person-centred assessment frameworks, with greater transparency during the assessment process, for example being explicit about wait times, openly discussing the purpose of assessment, and providing feedback and supported interpretation of results at each step of the process (Samsi et al., Citation2014). Such assessment approaches have been advocated for in the PPA, dementia, and post-stroke aphasia literature (Hersh et al., Citation2013; Molony et al., Citation2018; Rogalski & Khayum, Citation2018; Volkmer et al., Citation2020), however, they were not evident in the routine care described through this research.
Healthcare interactions
Healthcare experiences were further impacted by the nature of interactions with health professionals and interpersonal factors, highlighting that even brief negative interactions can have a significant and lasting impact on subsequent healthcare trajectories. Considering the emotional distress and practical impacts that individuals with PPA and their care partners experience, healthcare professionals must take care not to add to this stress through healthcare interactions. Individuals with PPA and their care partners valued healthcare interactions that were positive and encouraging. Further, they valued efforts to tailor support and recommendations to their unique needs and concerns, consistent with person-centred care (Rogalski & Khayum, Citation2018; Volkmer et al., Citation2023; Weiss & Swede, Citation2019).
Healthcare system and practice implications
The findings of this study highlight that structural and process elements of healthcare need to be addressed to improve how satisfied people with PPA and their care partners are with both their healthcare experiences and interactions with health professionals. Structural elements include waiting times, appropriateness, and availability of services, as well as access to healthcare information (Donabedian, Citation1988). Participants called for a centralised hub of reliable information about PPA and clearer signposting of post-diagnostic support options at different points of the care continuum. Care models and consensus best practice principles are now available to guide treatment decisions in response to individual needs (Volkmer et al., Citation2023) and could be used to inform the development of a centralised web portal, such as the Australian Aphasia Rehabilitation Pathway, to support service access and informed decision making across the continuum of care.
Process factors include what is done in giving and receiving care, encompassing the interpersonal skills of health professionals and the quality, continuity, and coordination of care (Donabedian, Citation1988). Models of care must be underpinned by relational strategies to ensure positive healthcare experiences, for example, establishing a relationship before commencing clinical procedures such as diagnostic assessments (Molony et al., Citation2018). Empathic, person-centred, and responsive ways of working with people with PPA and their families are required that promote empowerment (Van Corven et al., Citation2021), and which take into consideration individual expectations and attitudes towards help seeking.
Future directions and limitations
Future studies are encouraged to build on the preliminary findings of this study and address the limitations identified here. Future studies may benefit, for example, from recruiting people closer to the time of diagnostic and/or speech-language pathology assessment to extend the current findings. In this study, recruiting participants at different stages of their PPA journey enabled insight into their experiences across the continuum of care, however, four of the five participants were four or more years post-diagnosis. As such, they had to recall further back in time their first contacts with the health system and expressed difficulty differentiating services received in the public versus the private system. Further, while IPA studies typically use small sample sizes (Smith et al., Citation2009), future research could recruit a larger sample to help confirm and expand on the current findings. Comparison of the assessment experiences of people with PPA across service types, as well as with other types of dementia or post-stroke aphasia, could also be considered to identify shared and unique healthcare concerns across practice contexts and different populations. Future studies could seek to explore any influence of the nature and severity of language characteristics on the views reported. It is also acknowledged that interviewing people with PPA in dyads may have influenced the results. Despite attempts to facilitate a contribution to the interviews, many of the participants with PPA deferred to their family members. Future studies should explore strategies to interview participants separately or to encourage individual follow-up following the shared interview. Ultimately, future studies should extend the evaluation of screening, assessment, diagnostic, and management processes by health professionals to establish a more streamlined and coordinated care pathway for people with PPA.
Conclusion
This study sought to explore the lived experiences of people with PPA, with findings providing rich insights into their healthcare and assessment experiences, what it means to provide valued services, and factors influencing satisfaction and dissatisfaction with structural and process elements of healthcare. This has particular relevance given PPA is a progressive condition and ongoing, long-term support is required. With the wide ranging impacts of PPA on individuals and families, there is a need to respond to the voices of people living with the condition and their significant others to improve the quality of care.
Ethical approval
Ethics approval was obtained from Curtin Human Research Ethics Committee (HR218/2015).
Supplemental Material
Download PDF (94.8 KB)Supplemental Material
Download PDF (11.6 KB)Supplemental Material
Download Zip (90 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Beales, A., Bates, K., Cartwright, J., & Whitworth, A. (2019). Lost for words: Perspectives and experiences of people with primary progressive aphasia and Alzheimer’s disease and their families of participation in a lexical retrieval intervention. International Journal of Speech-Language Pathology, 21(5), 483–492. https://doi.org/10.1080/17549507.2019.1625439
- Cheng, B., Worrall, L., Copland, D., & Wallace, S. (2020). Prognostication in post-stroke aphasia: How do speech pathologists formulate and deliver information about recovery? International Journal of Language & Communication Disorders, 55(4), 520–536. https://doi.org/10.1111/1460-6984.12534
- Coyle-Gilchrist, I. T. S., Dick, K. M., Patterson, K., Vázquez Rodríquez, P., Wehmann, E., Wilcox, A., Lansdall, C. J., Dawson, K. E., Wiggins, J., Mead, S., Brayne, C., & Rowe, J. B. (2016). Prevalence, characteristics, and survival of frontotemporal lobar degeneration syndromes. Neurology, 86(18), 1736–1743. https://doi.org/10.1212/WNL.0000000000002638
- Davies, K., & Howe, T. (2020). Experience of living with PPA: A scoping review of qualitative studies. American Journal of Alzheimer’s Disease & Other Dementias, 35. https://doi.org/10.1177/1533317519886218
- Donabedian, A. (1988). The quality of care: How can it be assessed? JAMA, 260(12), 1743–1748. https://doi.org/10.1001/jama.260.12.1743
- Foxe, D., Irish, M., Hu, A., Carrick, J., Hodges, J. R., Ahmed, R. M., Burrell, J. R., & Piguet, O. (2021). Longitudinal cognitive and functional changes in primary progressive aphasia. Journal of Neurology, 268(5), 1951–1961. https://doi.org/10.1007/s00415-020-10382-9
- Frazer, S. M., Oyebode, J. R., & Cleary, A. (2012). How older women who live alone with dementia make sense of their experiences: An interpretative phenomenological analysis. Dementia, 11(5), 677–693. https://doi.org/10.1177/1471301211419018
- Gorno-Tempini, M. L., Hillis, A. E., Weintraub, S., Kertesz, A., Mendez, M., Cappa, S. F., Ogar, J. M., Rohrer, J. D., Black, S., Boeve, B. F., Manes, F., Dronkers, N. F., Vandenberghe, R., Rascovsky, K., Patterson, K., Miller, B. L., Knopman, D. S., Hodges, J. R., Mesulam, M. M., & Grossman, M. (2011). Classification of primary progressive aphasia and its variants. Neurology, 76(11), 1006–1014. https://doi.org/10.1212/WNL.0b013e31821103e6
- Henry, M. L., & Grasso, S. M. (2018). Assessment of individuals with primary progressive aphasia. Seminars in Speech & Language, 39(3), 231–241. https://doi.org/10.1055/s-0038-1660782
- Hersh, D., Worrall, L., O'Halloran, R., Brown, K., Grohn, B., & Rodriguez, A. D. (2013). Assess for success: Evidence for therapeutic assessment. In N. Simmons-Mackie, J. M. King & D. R. Beukelman (Eds.), Supporting communication for adults with acute and chronic aphasia (pp. 145–164). Paul H Brookes Publishing Co.
- Kaiser, S., & Panegyres, P. (2007). The psychosocial impact of young onset dementia on spouses. American Journal of Alzheimer’s Disease & Other Dementias, 21(6), 398–402. https://doi.org/10.1177/1533317506293259
- Keady, J., & Gilliard, J. (2002). Testing Times: The experience of neuropsychological assessment for people with suspected Alzheimer's disease. In P. B. Harris (Ed.), The person with Alzheimer's disease: Pathways to understanding the experience (pp. 4–28). The John Hopkins University Press.
- Khayum, B., Wieneke, C., Rogalski, E., Robinson, J., & O'Hara, M. (2012). Thinking outside the stroke: Treating primary progressive aphasia. Perspectives on Gerontology, 17(2), 37–49. https://doi.org/10.1044/gero17.2.37
- Lee, S., O'Neill, D., & Moss, H. (2022). Promoting well-being among people with early-stage dementia and their family carers through community-based group singing: A phenomenological study. Arts & Health, 14(1), 85–101. https://doi.org/10.1080/17533015.2020.1839776
- Low, L. F., Swaffer, K., McGrath, M., & Brodaty, H. (2018). Do people with early stage dementia experience prescribed disengagement®? A systematic review of qualitative studies. International Psychogeriatrics, 30(6), 807–831. https://doi.org/10.1017/S1041610217001545
- Luck, A., & Rose, M. (2007). Interviewing people with aphasia: Insights into method adjustments from a pilot study. Aphasiology, 21(2), 208–224. https://doi.org/10.1080/02687030601065470
- Mesulam, M. (2013). Primary progressive aphasia: A dementia of the language network. Dementia & Neuropsychologia, 7(1), 2–9. https://doi.org/10.1590/s1980-57642013dn70100002
- Molony, S. L., Kolanowski, A., Van Haitsma, K., & Rooney, K. (2018). Person-centered assessment and care planning. The Gerontologist, 58(suppl_1), S32–S47. https://doi.org/10.1093/geront/gnx173
- Nickels, L., & Croot, K. (2014). Understanding and living with primary progressive aphasia: Current progress and challenges for the future. Aphasiology, 28(8-9), 885–899. https://doi.org/10.1080/02687038.2014.933521
- Prorok, J. C., Horgan, S., & Seitz, D. P. (2013). Health care experiences of people with dementia and their caregivers: A meta-ethnographic analysis of qualitative studies. Canadian Medical Association Journal, 185(14), E669–E680. https://doi.org/10.1503/cmaj.121795
- QSR International Pty Ltd. (2020). NVivo (released in March 2020). https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Quinn, C., Clare, L., Pearce, A., & van Dijkhuizen, M. (2008). The experience of providing care in the early stages of dementia: An interpretative phenomenological analysis. Aging & Mental Health, 12(6), 769–778. https://doi.org/10.1080/13607860802380623
- Rogalski, E. J., & Khayum, B. (2018). A life participation approach to primary progressive aphasia intervention. Seminars in Speech & Language, 39(3), 284–296. https://doi.org/10.1055/s-0038-1660786
- Ruggero, L., Nickels, L., & Croot, K. (2019). Quality of life in primary progressive aphasia: What do we know and what can we do next? Aphasiology, 33(5), 498–519. https://doi.org/10.1080/02687038.2019.1568135
- Samsi, K., Abley, C., Campbell, S., Keady, J., Manthorpe, J., Robinson, L., Watts, S., & Bond, J. (2014). Negotiating a labyrinth: Experiences of assessment and diagnostic journey in cognitive impairment and dementia. International Journal of Geriatric Psychiatry, 29(1), 58–67. https://doi.org/10.1002/gps.3969
- Samsi, K., & Manthorpe, J. (2014). Care pathways for dementia: Current perspectives. Clinical Interventions in Aging, 9, 2055–2063. https://doi.org/10.2147/CIA.S70628
- Sapolsky, D., Domoto-Reilly, K., Negreira, A., Brickhouse, M., McGinnis, S., & Dickerson, B. C. (2011). Monitoring progression of primary progressive aphasia: Current approaches and future directions. Neurodegenerative Disease Management, 1(1), 43–55. https://doi.org/10.2217/nmt.11.2
- Scantlebury, K., Bixley, M., & Williamson, I. (2018). Exploring accounts of collaborative working between speech and language therapists and stroke association communication support coordinators following stroke. Journal of Interprofessional Care, 32(4), 490–500. https://doi.org/10.1080/13561820.2018.1446921
- Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative Phenomenological Analysis. SAGE Publications.
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
- Van Corven, C., Bielderman, A., Wijnen, M., Leontjevas, R., Lucassen, P., Graff, M., & Gerritsen, D. (2021). Empowerment for people living with dementia: An integrative literature review. International Journal of Nursing Studies, 124, 104098. https://doi.org/10.1016/j.ijnurstu.2021.104098
- Volkmer, A., Rogalski, E., Henry, M., Taylor-Rubin, C., Ruggero, L., Khayum, R., Kindell, J., Gorno-Tempini, M., Warren, J. D., & Rohrer, J. D. (2020). Speech and language therapy approaches to managing primary progressive aphasia. Practical Neurology, 20(2), 154–161. https://doi.org/10.1136/practneurol-2018-001921
- Volkmer, A., Cartwright, J., Ruggero, L., Beales, A., Gallée, J., Grasso, S., Henry, M., Jokel, R., Kindell, J., Khayum, R., Pozzebon, M., Rochon, E., Taylor-Rubin, C., Townsend, R., Walker, F., Beeke, S., & Hersh, D. (2023). Principles and philosophies for speech and language therapists working with people with primary progressive aphasia: an international expert consensus. Disability & Rehabilitation, 45(6), 1063–1078. https://doi.org/10.1080/09638288.2022.2051080
- Weiss, T., & Swede, M. J. (2019). Transforming preprofessional health education through relationship-centered care and narrative medicine. Teaching & Learning in Medicine, 31(2), 222–233. https://doi.org/10.1080/10401334.2016.1159566
- World Health Organisation. (2001). International Classification of Functioning, Disability and Health. https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health