ABSTRACT
Background
Little is known about the efficacy of eye movement desensitization and reprocessing (EMDR) therapy for post-traumatic stress disorder (PTSD) symptoms in people with mild intellectual disability or borderline intellectual functioning (MID-BIF).
Aims
To explore the safety, feasibility, and efficacy of EMDR therapy in adults with MID-BIF, PTSD, and comorbid mental health and psycho-social problems.
Methods and procedures
Data were collected from nine participants using a non-concurrent multiple baseline design. PTSD symptoms, level of daily life impairment, and possible adverse effect were measured weekly during baseline, treatment, post-treatment, and at three-month follow-up. Depressive symptoms, general psychopathology, and mental health problems were assessed once in every phase.
Outcomes and results
Participants displayed a significant reduction of PTSD symptoms, and the majority of participants no longer met criteria for DSM-5 PTSD diagnosis after therapy. EMDR therapy appeared to be safe, as no adverse events were reported during the study time frame. Further, participants showed a decrease in depressive symptoms as well as less severe general psychopathology and mental health problems following therapy.
Conclusion
EMDR therapy was found to be safe, feasible, and (potentially) efficacious in decreasing PTSD symptoms, loss of PTSD diagnoses, reduction of level of daily life impairment, and general psychopathology for adults with MID-BIF, suffering from both severe mental health and psycho-social problems.
What This Paper Adds
People with mild intellectual disability or borderline intellectual functioning (MID-BIF) have an increased risk of developing post-traumatic stress disorder (PTSD). Therefore, the treatment of PTSD in this population is receiving increased attention from clinicians and researchers. Although cognitive behavior therapy and eye movement desensitization and reprocessing (EMDR) therapy are both recommended in the treatment of PTSD in adults, EMDR seems more feasible for adults with MID-BIF because there is no need for homework or practice outside the sessions (Mevissen et al., Citation2016a). However, the evidence base for the treatment of PTSD with EMDR therapy in people with MID-BIF is meager. The small number of controlled studies, nonetheless, suggests that EMDR therapy is potentially effective in treating PTSD (symptoms) in this cohort (Karatzias et al., Citation2019; Mevissen et al., Citation2017; Penninx Quevedo et al., Citation2021). The current study extends this evidence base by using a multiple baseline design in a population with MID-BIF and PTSD, as well as comorbid mental health and psycho-social problems, and by suggesting that EMDR therapy is safe, feasible, and efficacious in the treatment of PTSD in this population. To this end, this study provides suggestions for the application of EMDR therapy in clinical practice in this complex population, with particular attention to EMDR treatment completion and the relationship with comorbid mental health problems.
Introduction
People with a mild intellectual disability or borderline intellectual functioning (MID-BIF) are more likely to be exposed to traumatic events, such as physical, emotional, and sexual abuse, than their nondisabled peers (Hulbert-Williams et al., Citation2014; Soylu et al., Citation2013). Moreover, due to impairments in their intellectual and adaptive skills and limited supportive networks, they are less able to process (potentially) traumatic events (McCarthy et al., Citation2017). As a result, people with MID-BIF are more susceptible to developing a wide range of mental health problems, such as mood, anxiety, and behavioral problems, including post-traumatic stress disorder (PTSD; Mevissen et al., Citation2016a; Wigham et al., Citation2014). PTSD is characterized by the presence of intrusions, avoidant behavior, and negative alterations in cognitions, mood, arousal, and reactivity. These symptoms result from exposure to actual or threatened death, serious injury, or sexual violence in one or more of the following ways: (1) directly experiencing the traumatic event, (2) witnessing the events as they occurred to others, (3) learning that the traumatic event occurred to a close family member or friend, and/or (4) experiencing repeated or extreme exposure to aversive details of the traumatic event in the work environment (DSM-5; American Psychiatric Association, Citation2013).
Within the general population, estimates of the prevalence of PTSD range between 1 and 12% (Shalev et al., Citation2017). Among individuals with one or more mental health problems, the prevalence rate of PTSD is higher, ranging between 20 and 47% (Mauritz et al., Citation2013). Prevalence rates of PTSD among individuals with MID-BIF and comorbid health problems are higher still. A study by Nieuwenhuis et al. (Citation2019) screened for trauma and PTSD in a sample of adult patients with one or more mental disorders who received care from an outpatient service. In the group of patients suspected of having MID-BIF, 48% had indications for PTSD. However, only 8% of these patients received a PTSD diagnosis during treatment. Mevissen et al. (Citation2020) also assessed the prevalence of PTSD in patients with MID-BIF and found a rate of 40%, while only 2% of patients were diagnosed with PTSD according to the patient records. These studies suggest that PTSD is underdiagnosed in people with MID-BIF. Nieuwenhuis et al. (Citation2019) point out that this might be due to clinicians not enquiring about having been exposed to (potentially) traumatic events out of fear of symptom exacerbation.
The increased likelihood of exposure to traumatic events, the underdiagnosing of PTSD, and its adverse consequences in people with MID-BIF and mental health problems emphasize the need for effective treatment of PTSD in this population. Trauma-focused cognitive behavior therapy and eye movement desensitization and reprocessing (EMDR) therapy are first-line evidence-based psychotherapies recommended for the treatment of PTSD in adults (World Health Organization, Citation2013). Compared to trauma-focused cognitive behavior therapy, EMDR therapy seems more feasible for people with ID and comorbid PTSD, as these patients are less capable as a consequence of their impairment to independently do the necessary homework or practice outside the sessions (Mevissen et al., Citation2016a).
Although efficacy studies on PTSD in people with MID-BIF are still rare and consist mostly of case descriptions, they show promising results (for an overview, see, Luteijn et al., Citation2020). A study by Mevissen et al. (Citation2017) was the first to examine the treatment effects of PTSD in people with MID-BIF using a multiple baseline design. In this study, a child (aged 10 years) and an adolescent (aged 18 years), both with MID-BIF, received EMDR therapy. The results showed that PTSD symptoms decreased significantly to the extent that both participants no longer met PTSD criteria after treatment. Karatzias et al. (Citation2019) used a mixed-methods randomized controlled design to examine the effectiveness of EMDR therapy and standard care (EMDR+SC) versus standard care alone (SC) for PTSD in 22 adults with intellectual disabilities. The results showed a significantly greater decrease in general anxiety symptoms in the EMDR+SC group compared to the SC group. Also, in the EMDR+SC group, 60% of participants no longer met PTSD criteria at post-treatment and 47% of the participants at three-month follow-up, in comparison to 27% of patients at post-treatment and follow-up in the SC group. Finally, Penninx Quevedo et al. (Citation2021) used a multiple baseline design to examine the effectiveness, feasibility, and safety of EMDR-therapy in six patients with MID-BIF, PTSD, and a psychotic disorder. A significant decrease in the number of PTSD symptoms was found, such that five out of the six participants no longer met DSM-5 PTSD criteria post-treatment. In addition, an increase in general functioning and decreases in psychotic symptoms and general psychopathology were found.
The current study aimed to explore the safety, feasibility, and efficacy of EMDR therapy on PTSD symptoms in people with MID-BIF and comorbid mental health and psycho-social problems in a tertiary mental health care setting specialized in the diagnosis and treatment of mental health problems in people with MID-BIF. We hypothesized that EMDR treatment would be safe and feasible for this cohort. Further, we expected that the number of PTSD symptoms would be significantly reduced from baseline to post-treatment and from baseline to follow-up. Finally, we hypothesized that EMDR therapy would be associated with an improvement in general functioning and a reduction in psychopathology between baseline and post-treatment.
Methods And Procedures
Setting and Participants
All participants were recruited from an EMDR therapy waiting list and were included if they had MID-BIF and PTSD. Whether participants met diagnostic criteria of PTSD (DSM-5) was assessed using the adapted Anxiety Disorders Interview Schedule for adults with MID-BIF, PTSD section (ADIS-C PTSD-adults; Mevissen et al., Citation2020). In accordance with the DSM-5 criteria, participants were diagnosed with MID-BIF based on intelligence test results (e.g., WAIS-III, WAIS-IV), a Dutch proxy questionnaire indexing adaptive functioning: sociale redzaamheidsschaal voor verstandelijke gehandicapten (SRZ-P; Kraijer & Kema, Citation2004) and the history of the intellectual and adaptive development during childhood and adolescence. In addition to MID-BIF, all participants were known to have comorbid mental health and social problems. A psychiatrist and a psychologist together conducted the assessments of the aforementioned diagnoses and problems. Patients were excluded from the study if they had insufficient competence in the Dutch language, severe substance abuse, major depression, and/or a suicide attempt in the last three months.
Participants were eight women and one man between 34 and 53 years of age who were patients within a specialized mental health facility for people with MID-BIF and psychiatric problems in the Netherlands (i.e., Center for Mild Intellectual Disabilities and Psychiatry at GGZ Oost Brabant). provides participant characteristics. The participants received inpatient or outpatient treatment. Inpatient treatment took place in a social and therapeutic (i.e., socio-therapeutic) environment created by a multidisciplinary team including a psychiatrist, psychologist(s), and psychiatric nurses. In the socio-therapeutic environment, adaptive skills are taught. The environment is structured by staff members and demands placed upon the patients are adapted to their level of intellectual, adaptive, and emotional functioning. Participants who received outpatient treatment have regular appointments with a psychiatrist for pharmacotherapy and/or a psychologist for psychotherapeutic interventions (i.e. cognitive behavior therapy). Eight out of nine participants received pharmacotherapy (e.g., benzodiazepines, antidepressants, antipsychotics).
Table 1. Participant characteristics.
Consent Procedure
The study was approved by the Committee of Ethics of the Faculty of Social Sciences, Radboud University, Nijmegen, the Netherlands (NL55553.091.15). The participants who were recruited from the waiting list for EMDR treatment were informed about the study by their therapist. Patients who met the criteria for inclusion and were interested in participating in the study met with the primary researcher (first author), who informed them about the purpose of the study, type of treatment, possible adverse side effects, measurements, and video recordings of the sessions. After a week, if the participants were still interested in participating, the primary researcher and participant signed an informed consent form. All participants had the legal capacity to decide to participate. Participants could withdraw or refuse participation at any point during the study.
Design
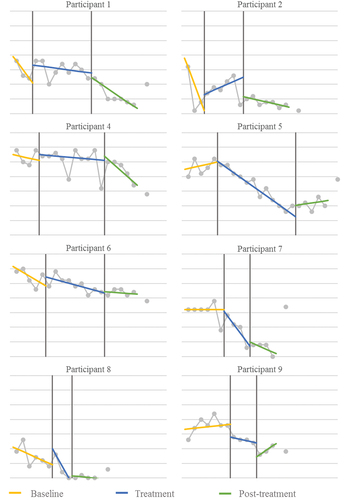
A non-concurrent multiple baseline design across subjects was used (see, Kazdin, Citation2020) to examine the effects of EMDR therapy on PTSD symptoms, depressive symptoms, mental health and social functioning, general psychopathology, and distress. The nine participants were randomly assigned to five different baseline lengths (i.e. a minimum of three to a maximum of seven baseline assessments and vice versa for the post-treatment assessments, see, ). Participants were assessed weekly for PTSD symptoms and clinically adverse events (primary outcome measures) during baseline (B), treatment (T), post-treatment (P), and follow-up (FU). Secondary outcome measures (depressive symptoms, mental health and social functioning, general psychopathology, and distress) were administered at three time points: after baseline (T1), after treatment (T2), and at follow-up (T3).
EMDR Therapy
EMDR treatment was provided weekly by three certified psychologists working at the center, who all attended accredited basic and advanced training from the Dutch EMDR Association and had at least three years of experience providing EMDR treatment to patients with MID-BIF and severe mental health and social problems. For supervision purposes, all sessions were videotaped. The psychologists received weekly supervision by an accredited supervisor and trainer from the Dutch EMDR Association. Treatment integrity was monitored by the supervisor and primary researcher (first author), to whom all deviations from the protocol were reported. The first author of this paper was not involved as a therapist. The treatment sessions were conducted individually. Each participant was assigned to one of the psychologists for the duration of the EMDR treatment. Participants received a maximum of twelve sessions. Early completion was allowed. If necessary, EMDR treatment was continued after the last measurement at follow-up.
The Dutch EMDR protocol for children and adolescents up to 18 years (De Roos et al., Citation2012) was used so that instructions as to how to activate the trauma memories and instructions on how to support the participants during therapy corresponded to the cognitive and emotional abilities of the participants. This protocol comprises of the same eight phases as the standard protocol developed by Shapiro (Citation2001), but differs in the way that the language used is suited for individuals with less language proficiency and that icons and/or pictures are used while explaining or inquiring. The protocol for children and adolescents was not altered for the current patient group. However, bilateral stimulation occurred only by using eye movements (i.e. fingers of the psychologist). The phases of the protocol, of which phase three through eight are repeated each session, are described briefly as follows:
Constructing a case conceptualization by taking a full history and assessing suitable targets for EMDR. In this study this was done by using the ADIS-C PTSD-adults (see Measures) and the Two Method Approach (De Jongh et al., Citation2010);
Establishing of a therapeutic relation, and enhancing personal resources and self-calming techniques;
Assessing of the components of the distressing memory, including the dysfunctional negative cognition of oneself and accompanying emotions and body disturbances;
Bilateral stimulation and assessing emotional, cognitive, somatic and imagistic experiences;
Preparing the patient for the period between sessions;
Reevaluation to determine the treatment gains, at the beginning of every EMDR session.
Measures
Primary Outcome Measures
Clinically Adverse Events/Patient Safety
Undesirable effects that were potentially related to the EMDR treatment were screened and reported by the EMDR therapist throughout the study. The participants were asked about (a) major events last week, (b) hospital admission, (c) suicidal thoughts and behavior, (d) changes in (non-prescribed) medication, (e) crisis interventions in the past week, and (f) changes in the use of alcohol and/or drugs. When adverse events occurred, they were reported to the Committee of Ethics of the Faculty of Social Sciences, Radboud University.
PTSD Symptoms, Interference Scores, and DSM-5 PTSD Classification
The adapted Anxiety Disorders Interview for adults with MID-BIF, PTSD-section (ADIS-C PTSD-ID-Adults; Mevissen et al., Citation2016b) consisted of two sections. The first section contained 29 items on type-A trauma events (e.g., sexual abuse and serious accident) and other life events (e.g., outplacement and serious illness). The second section consisted of 35 items on PTSD symptoms and four items on potentially atypical symptoms (i.e., eating problems, compulsions, poor self-care, and upset by sudden changes) to which respondents answered with “yes,” “no,” or “otherwise.” Finally, the participant was asked to rate his or her subjective level of daily life impairment related to the PTSD symptoms and traumatic events (i.e., interference score), corresponding with criteria G of the DSM-5 PTSD classification. To this end, a thermometer card was used with a scale ranging from 0 “not at all,” 2 “a little bit,” 4 “somewhat,” 6 “a lot,” to 8 “very much” negative impact on daily life. A score of 4 or higher is interpreted as clinically significant distress or impairment in social, occupational, or other important areas of functioning (Mevissen et al., Citation2016b).
Agreement between raters of the ADIS-C PTSD-ID was found to be good to excellent (Cohen’s kappa ranging from .50 to .90). In addition, the content validity and convergent validity were considered good (Mevissen et al., Citation2020).
The ADIS-C PTSD-ID-Adults was used during the selection process to assess the diagnostic criteria for PTSD and to develop a case conceptualization. The second section of the interview was used to measure weekly changes in PTSD symptoms. During the treatment phase of the study, the interview was administered at the start of each session by the assigned EMDR therapist and during the other phases of the study by a trained research assistant. The ADIS-C PTSD-ID-Adults was also used after treatment and at follow-up to inform classification of PTSD according to DSM-5. After the data collection of the current study, minor changes were applied to the ADIS-C PTSD-ID-Adults, and the measure is now known as the Diagnostic Interview Trauma and Stressors – Intellectual Disability (DITS-ID; Mevissen et al., Citation2018).
Secondary Outcome Measures
In the present study, secondary measures were administered at the start of baseline (T1), at the end of the treatment phase (T2), and at follow-up (T3) by a trained research assistant or by the EMDR therapist.
Depressive Symptoms
The Beck Depression Inventory – 2nd edition Dutch version (BDI-II-NL) is a 21-item instrument measuring behavioral, cognitive, and motivational symptoms of depression. Respondents rated the items on a four-point scale ranging from 0 (symptoms absent) to 3 (severe symptoms), resulting in a total score ranging from 0 to 63 (Van der Does, Citation2002). Higher scores indicated greater depressive symptom severity. The internal consistency was considered high in a sample of psychiatric outpatients (Cronbach’s alpha was .91; Beck et al., Citation1996). Studies on the psychometric properties of the BDI-II in people with MID-BIF also showed high internal consistency (Cronbach’s alpha ranging from .86 – .90), and factor analysis found results that were consistent with the results found in mainstream populations (Lindsay & Skene, Citation2007; Powell, Citation2003).
Mental Health and Social Functioning
The Health of the Nation Outcome Scales (HoNOS) in Dutch (Mulder et al., Citation2004) was used to assess overall mental health and social functioning. An informant of the patient scores 12 items on a five-point scale ranging from 0 (no problem) to 4 (severe to very severe problem), resulting in a total score ranging from 0 to 48, with higher scores indicating more severe problems. The content validity and internal consistency (Cronbach’s alphas ranging from .59 to .76) of the HoNOS were considered good, and the predictive validity was reasonably good (Pirkis et al., Citation2005). In addition, test–retest reliability, inter-rater reliability, sensitivity to change, and feasibility and utility were considered adequate (Pirkis et al., Citation2005).
General Psychopathology and Distress
The Brief Symptom Inventory (BSI) is a short version of the SCL-90-R and measures psychological symptoms (Derogatis & Melisaratos, Citation1983). Fifty-three items were scored using a five-point scale of distress ranging from 0 (not at all) to 4 (extremely), resulting in a total averaged score between 0 and 4. Higher scores indicated greater general psychopathology and distress. In the present study, the Dutch translation of the BSI (De Beurs & Zitman, Citation2006) was used. The Dutch version of the BSI showed good reliability (Cronbach’s alphas ranging from .71 to .87) and the same nine-factor structure as the original version. Also, the convergent validity and divergent validity were considered adequate (De Beurs & Zitman, Citation2006). The psychometric properties in psychiatric outpatients with intellectual disabilities showed similar reliability (Cronbach’s alphas ranging from .70 to .96) and adequate to good internal consistency and discriminant validity. The nine-factor structure of the BSI was replicated (Wieland et al., Citation2012).
Data Analyses
Primary Outcome Measures
Data analyses of the effectiveness of EMDR on PTSD symptoms and interference scores consisted of visual and statistical analyses on individual and group levels. Visual analyses included evaluation of level and trend (stability of effect) within phases and between baseline, treatment, and post-treatment phases, following the guidelines provided by Lane and Gast (Citation2014). For each phase, a trend line was calculated using the split level/middle method of trend estimation. Levels were analyzed between phases (i.e., baseline, treatment, post-treatment) by comparing median values.
A quantitative approach for analyzing single-case design data was used for the calculation of non-overlapping data between the three phases (i.e., baseline, treatment, and post-treatment). The web-based program Single Case Research (SCR; Vannest et al., Citation2016) was used to calculate Taunovlap, Tau-U, and p-values for the contrast between baseline and treatment phases (B–T) and between baseline and post-treatment phases (B–P). Taunovlap and Tau-U are effect sizes that examine the proportion of non-overlapping data between two phases. The difference between Taunovlap and Tau-U is that the latter controls for an undesirable positive baseline trend (Parker et al., Citation2011). If visual analysis indicated a positive baseline trend, Tau-U was calculated; in all other cases, the Taunovlap was used. Guidelines for the interpretation of Taunovlap and Tau-U indicate that scores below .20 are small effects, scores from .20 to .60 are moderate effects, scores from .60 to .80 are large effects, and scores above .80 are large to very large effects (Vannest & Ninci, Citation2015). Tau analyses between baseline and follow-up phases were not possible due to an insufficient number of data points in the follow-up phase: one instead of a minimum of three (Kratochwill et al., Citation2010).
Secondary Outcome Measures
Analyses of the secondary outcome measures for general functioning and psychopathology (i.e., BDI-II-NL, HoNOS, and BSI) included General Linear Model (GLM) repeated measures analyses and subsequent post-hoc Bonferroni tests for the three time points T1, T2, and T3 . Scores of partial eta squared (partial η2) below .10 are considered small effects, .30 represents a medium effect, and .50 reflects a large effect (Field, Citation2013).
Table 2. Means and standard deviations of PTSD symptoms.
Results
Treatment Completion
Six out of nine participants received EMDR treatment until all treatment targets were adequately treated. Participants 3 and 9 discontinued their treatment after 3 and 4 treatment sessions, respectively. Participant 3 reasoned that psychosocial problems (e.g., familial problems, financial problems, inadequate housing) hindered the EMDR treatment and chose to withdraw from the treatment. The measurements from participant 3 were insufficient and were therefore excluded. Participant 9 stopped the treatment earlier than desired after four sessions because the participant considered the complaints sufficiently reduced. The participant could not be motivated for further treatment, therefore the treatment terminated and the post-treatment phase started. The measurements from participant 9 were included in the analyses. Due to many psychosocial problems (i.e. inadequate housing, financial problems, and relationship problems) participant 6 ruminated and slept badly, leading to a reduction of cognitive capacity despite good motivation. Therefore, the psychologist and supervisor assumed that the effects after the maximum twelve sessions were not sufficient. EMDR treatment resumed after the follow-up assessment. The measurements from participant 6 were included in the analyses.
The mean number of EMDR sessions of the remaining eight participants included in the analyses (excluding participant 3) was 7.13 (SD = 3.10), ranging between 3 and 12 sessions. The mean session duration of these eight participants was 68.2 minutes (SD = 19.4), ranging between 26 and 111 minutes per session.
Primary Outcome Measures
Adverse Events and Patient Safety
Although minor events did occur, as indicated in section 3.1, no major adverse events were reported by the therapists during the study time frame. There were no deviations from the protocol.
PTSD Symptoms
shows the course of PTSD symptoms during the study time frame for all eight participants included in the analyses. Three out of eight participants (1, 2, 8) showed a downward trend during baseline to such an extent that their stability envelope was not stable enough according to the guidelines of Lane and Gast (Citation2014), and the method of analysis was adapted accordingly (see section 2.6.1). During the treatment phase, seven out of eight participants showed a downward trend in PTSD symptoms. Post-treatment, PTSD symptoms decreased further or remained stable in seven out of eight participants.
depicts means and standard deviations of the number of PTSD symptoms during baseline, treatment, and post-treatment at individual and group levels. PTSD symptoms decreased in all eight participants between baseline and post-treatment and in seven out of eight participants between baseline and follow-up.
presents the results of the Tau analyses on the differences in PTSD symptoms between different phases on individual and group levels. Five out of eight participants showed significant decreases in PTSD symptoms between baseline and post-treatment with large to very large effects. At the group level, shows a significant and large treatment effect between baseline and post-treatment. No significant effect was found between baseline and follow-up.
Table 3. Effect sizes and p-values of PTSD symptoms.
Interference Scores
presents the means and standard deviations of the interference scores on individual and group levels. The interference scores decreased in all eight participants between baseline and post-treatment and between baseline and follow-up.
Table 4. Means and standard deviations of interference scores.
shows the results of the Tau analyses on the differences in interference scores between different phases on individual and group levels. Five out of eight participants showed significant decreases in interference scores between baseline and post-treatment with very large effects. At the group level, there was a significant and moderate to very large treatment effect for all three comparisons between the study phases.
Table 5. Effect sizes and p-values of interference scores.
Criteria DSM-5 PTSD Diagnosis
At post-treatment, six out of the eight participants no longer met the DSM-5 criteria for a PTSD classification. At follow-up, the number increased to seven out of the eight participants.
Secondary Outcome Measures
shows the total scores of the BDI-II-NL, the HoNOS, and the BSI for each participant and the means and standard deviations of the group for the three measurement points (i.e., T1, T2, and T3). BDI-II-NL scores decreased in all eight participants between T1 and T2 and in six out of eight participants between T1 and T3. HoNOS scores decreased in six out of eight participants between T1 and T2 and between T1 and T3. BSI scores decreased in six out of eight participants between T1 and T2 and in seven out of eight participants between T1 and T3. On a group level, BDI-II-NL, HoNOS, and BSI scores decreased between T1 and both other measurements.
Table 6. Total scores, means, and standard deviations of BDI-II-NL, HoNOS, and BSI.
shows the results of the GLM repeated measures analysis on the differences in the measures of general functioning and psychopathology between phases at the group level. There was a significant decrease in BDI-II-NL and HoNOS scores with medium effects between T1 and T2. Subsequent Bonferroni pairwise comparisons showed that BDI-II-NL and HoNOS scores at T2 were significantly lower than at T1. There were no significant differences in BSI scores between T1 and T2. In addition, no significant differences between T1 and T3 were found for all measurements.
Table 7. Effect sizes and p-values of BDI-II-NL, HoNOS, and BSI.
Discussion
The present study explored the safety, feasibility, and efficacy of EMDR therapy in a sample of nine people with PTSD, MID-BIF, and severe mental health and psycho-social problems who were patients of a specialist mental health facility. The results showed that all eight participants who completed the EMDR therapy experienced a reduction in PTSD symptoms and lower levels of daily life impairment. In addition, six out of eight participants no longer met criteria for DSM-5 PTSD diagnosis after treatment; at follow-up the number decreased even further, when seven out of eight participants no longer met criteria. EMDR therapy was also safe, as no adverse events were reported during the study time frame. Further, a large majority of participants showed a decrease in depressive symptoms, general psychopathology, and distress, and problems in mental health and social functioning were less severe following EMDR therapy. In sum, these results support the notion that EMDR therapy is an efficacious treatment option for people with comorbid MID-BIF. More specifically, the results provide support for our hypotheses that EMDR therapy would (1) be safe and feasible for people with MID-BIF and comorbid mental health and psycho-social problems, (2) be associated with a decrease in the number of PTSD symptoms, and (3) improve general functioning and reduce psychopathology.
The main findings, in which all participants showed a decrease in PTSD symptoms and seven out of eight participants no longer met DMS-5 PTSD criteria at follow-up, are in line with results of studies that investigated the effectiveness of EMDR therapy in people without MID-BIF (for an overview, see, De Jongh et al., Citation2019) and with a number of studies examining the efficacy of EMDR therapy in people with MID-BIF (Karatzias et al., Citation2019; Mevissen et al., Citation2017; Penninx Quevedo et al., Citation2021). The decrease in depressive symptoms, general psychopathology, and distress and the increase in general functioning are in line with results of other studies with samples of participants without MID-BIF (for an overview, see, Van Minnen et al., Citation2015). Current results suggest that EMDR therapy is also a safe, feasible, and efficacious treatment option for people with MID-BIF, PTSD, severe psychiatric symptoms, and psychosocial problems, and it might also decrease symptoms of other comorbid mental health symptoms.
Several notes should be made regarding the course of PTSD symptoms during the study time frame. During baseline, three out of eight participants showed a reduction in PTSD symptoms. This effect has also been observed in a previous study in people with MID-BIF and was explained by an increased sense of control due to the hope for an effective result, which caused symptoms to decrease (Penninx Quevedo et al., Citation2021). It should also be mentioned that PTSD symptoms increased at the start of treatment in four out of eight participants. However, no adverse events, such as crisis interventions, suicidal thoughts and behavior, or changes in alcohol and/or drug use, were observed or reported for any of the participants. In addition, all participants experienced positive effects of the intervention and no longer met the DSM-5 criteria for PTSD at follow-up. Altogether, this outcome is in line with studies demonstrating that trauma-focused treatments can be endured without lasting symptom exacerbation (e.g., Larsen et al., Citation2016). Also, at follow-up, four out of eight participants reported an increase in the number of PTSD symptoms, after first experiencing a decrease in symptoms directly following EMDR therapy, an effect which has also been observed in previous studies in people without MID-BIF (e.g., Van Woudenberg et al., Citation2018), as well as in studies in people with MID-BIF (e.g., Karatzias et al., Citation2019; Penninx Quevedo et al., Citation2021). A possible explanation for the increase of PTSD symptoms at follow-up, after EMDR treatment was completed, is that exposure to new or previously experienced traumatic events (re)occurred that again triggered an increase in PTSD symptoms (Wilker et al., Citation2015).
The current study has strengths and limitations. One strength is the procedural integrity of the therapists, as they were extensively trained, had at least three years of experience providing EMDR therapy in this cohort, and received weekly supervision from an accredited supervisor and trainer from the Dutch EMDR Association. Furthermore, the current study represents a highly complex patient group with intellectual disabilities and a large variety in mental health and psychosocial problems, which adds to the credibility of obtained results on the positive effects of EMDR treatment for this cohort. However, it may be considered a limitation that we did not assess whether the level of intellectual disability or type of comorbid mental health problems influenced the implementation or outcome of the EMDR treatment. Another limitation pertains to the cut off set to determine when EMDR treatment was completed. It was assumed that if all trauma memories in the case conceptualization had reached a subjective unit of discomfort score (SUD score) of zero and a validity of cognition score (VOC score) of seven, as is stated in the treatment protocol, the PTSD symptoms would in consequence reduce, and treatment could stop. However, five out of eight participants still reported ten or more PTSD symptoms at the end of the EMDR therapy trajectory. Interference scores, however, were low, so that DSM-5 PTSD criteria were no longer met.
As mentioned earlier, these results provide evidence for an association between PTSD and depressive symptoms, general psychopathology, and mental health. First, the relationship may be due to common underlying etiologies or vulnerabilities, such as the shared underlying factor of negative affect in depression and PTSD (Zoellner et al., Citation2014). The second explanation for the high level of PTSD symptoms at the end of treatment is more conceptual and relates to symptom overlap. PTSD and major depression have a number of symptoms in common, such as anhedonia, insomnia, and difficulty concentrating (Gros et al., Citation2012). Therefore, it is possible that a number of participants still scored high at the end of treatment due to some common underlying etiology or symptom overlap of a comorbid mental health disorder, such as depression, not specifically related to the PTSD they were treated for. To overcome this limitation, future studies and clinical practice should not solely use a SUD of zero as the only criterion to determine when treatment is completed but should also assess residual symptoms. Especially in patients with comorbid mental health and social problems, clinicians need to also assess whether symptoms are due to exposure to a traumatic event or whether they should be interpreted as symptoms of comorbid mental health or social problems. In addition, the treatment aims of the patient and general recovery, as rated by the patient, should be guiding factors for treatment completion.
A remark should be made about the assessment load, difficulty and quantity during the study timeframe. All instruments used, except the HoNOS as an informant report, showed good psychometric properties in samples of adults with mild intellectual disabilities (Lindsay & Skene, Citation2007; Mevissen et al., Citation2020; Powell, Citation2003; Wieland et al., Citation2012). The average assessment time of the instruments was fifteen minutes. This meant that weekly assessments took approximately fifteen minutes and the assessments at T1, T2 and T3 took approximately thirty minutes. In addition, a clinician or research assistant supported participants to complete the instruments, so that if difficult questions arose an explanation was given.
In addition, the variation in session number and length between participants are notable. The number of sessions depended on the number and complexity of targets, the amount of time needed to complete one target (i.e. until the SUD score reached zero and the VOC-score reached seven), and the level of cognitive capacity of the participant. This also influenced the session length. Also, after one target was treated and there was ample time in the session left, participants were given the choice to continue the session with the next target or to stop the current session and start the next target in the next session. This choice in combination with the other factors mentioned could lead to either a brief session or extended session.
In conclusion, the present study supports other research findings (Karatzias et al., Citation2019; Mevissen et al., Citation2017; Penninx Quevedo et al., Citation2021) that EMDR therapy is a safe, feasible, and (potentially) efficacious treatment option for people with MID-BIF, PTSD symptoms, and severe mental health and social problems. EMDR therapy may decrease PTSD symptoms to below DSM-5 criteria; reduce the level of daily life impairment, depressive symptoms, problems in mental health, general psychopathology, and distress; and improve social functioning in this cohort. Future research on the efficacy of EMDR treatment in people with MID-BIF and mental health problems should continue using multiple baseline designs in small samples because of their usefulness in clinical practice (Nock et al., Citation2007), albeit replication in larger samples using randomized controlled designs would certainly be desirable. Outcome measures should not only focus on symptom reduction but also include measures of personal and societal recovery.
Highlights
People with MID-BIF have a higher risk of being exposed to a traumatic event.
PTSD is underdiagnosed in people with MID-BIF.
EMDR therapy seems relatively easy to apply.
EMDR proved safe and capable of reducing PTSD symptoms and comorbid symptoms.
Discolsure Statement
Ad de Jongh receives income from published books on EMDR therapy and for the training of postdoctoral professionals in this method.
Credit Authorship Contribution Statement
Inge Verhagen: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, validation, visualization, writing. Renate van der Heijden: data curation, visualization, writing. Ad de Jongh: conceptualization, methodology, validation, resources, writing – review & editing, supervision. Hubert Korzilius: methodology, formal analysis, data curation, writing – review & editing, visualization. Liesbeth Mevissen: conceptualization, methodology, validation, writing – review & editing. Robert Didden: conceptualization, methodology, validation, resources, writing – review & editing, supervision.
Acknowledgments
We would like to thank the Dutch EMDR Association (Vereniging EMDR Nederland) and GGZ Oost Brabant for providing a grant to the first author. In addition, we would like to express thanks to research assistant M. van Galen and supervisor I. Spierts.
Data Availability Statement
The data that support the findings of this study are available from GGZ Oost Brabant. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the corresponding author, IV, with the permission of GGZ Oost Brabant.
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th) ed.).
- Beck, A. T., Steer, R. A., Ball, R., & Ranieri, W. F. (1996). Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. Journal of Personality Assessment, 67(3), 588. https://doi.org/10.1207/s15327752jpa6703_13
- De Beurs, E., & Zitman, F. (2006). The Brief Symptom Inventory (BSI): Reliability and validity of a practical alternative to SCL-90. Maandblad Geestelijke Volksgezondheid, 61, 120–141. https://www.researchgate.net/publication/284679116_The_Brief_Symptom_Inventory_BSI_Reliability_and_validity_of_a_practical_alternative_to_SCL-90.
- De Jongh, A., Amann, B. L., Hofmann, A., Farrell, D., & Lee, C. W. (2019). The status of EMDR therapy in the treatment of posttraumatic stress disorder 30 years after its introduction. Journal of EMDR Practice and Research, 13(4), 261–269. https://doi.org/10.1891/1933-3196.13.4.261
- De Jongh, A., Broeke, E., & Meijer, S. (2010). Two Method approach: A case conceptualization model in the context of EMDR. Journal of EMDR Practice and Research, 4(1), 12–21. https://doi.org/10.1891/1933-3196.4.1.12
- Derogatis, L. R., & Melisaratos, N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13(3), 595–605. https://doi.org/10.1017/S0033291700048017
- De Roos, R., Beer, R., De Jongh, A., & ten Broeke, E. (2012). EMDR Protocol voor kinderen en jongeren tot 18 jaar. [EMDR Protocol for children and adolescents up to 18 years]. Pearson.
- Field, A. (2013). Discovering statistics using IBM SPSS statistics: And sex and drugs and rock ‘n’roll (4th) ed.). Sage.
- Gros, D. F., Price, M., Magruder, K. M., & Frueh, B. C. (2012). Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Research, 196(2), 267–270. https://doi.org/10.1016/j.psychres.2011.10.022
- Hulbert-Williams, L., Hastings, R., Owen, D. M., Burns, L., Day, J., Mulligan, J., & Noone, S. J. (2014). Exposure to life events as a risk factor for psychological problems in adults with intellectual disabilities: A longitudinal design. Journal of Intellectual Disability Research, 58(1), 48–60. https://doi.org/10.1111/jir.12050
- Karatzias, T., Brown, M., Taggart, L., Truesdale, M., Sirisena, C., Walley, R., Mason-Roberts, S., Bradley, A., & Paterson, D. (2019). A mixed-methods, randomized controlled feasibility trial of Eye Movement Desensitization and Reprocessing (EMDR) plus Standard Care (SC) versus SC alone for DSM-5 Posttraumatic Stress Disorder (PTSD) in adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 32(4), 806–818. https://doi.org/10.1111/jar.12570
- Kazdin, A. E. (2020). Single-case research designs: Methods for clinical and applied settings (3rd) ed.). Oxford University Press.
- Kraijer, D. W., & Kema, G. N. (2004). SRZ-P, sociale redzaamheidsschaal voor verstandelijk gehandicapten van een hoger niveau. [ SRZ-P, social self-reliance scale for the mentally disabled with higher functioning]. Pearson Clinical.
- Kratochwill, T. R., Hitchcock, J., Horner, R. H., Levin, J. R., Odom, S. L., Rindskopf, D. M., & Shadish, W. R. (2010). Single-case designs technical documentation. https://ies.ed.gov/ncee/wwc/Docs/ReferenceResources/wwc_scd.pdf
- Lane, J. D., & Gast, D. L. (2014). Visual analysis in single case experimental design studies: Brief review and guidelines. Neuropsychological Rehabilitation, 24(3–4), 445–463. https://doi.org/10.1080/09602011.2013.815636
- Larsen, S. E., Wiltsey Stirman, S., Smith, B. N., & Resick, P. A. (2016). Symptom exacerbations in trauma-focused treatments: Associations with treatment outcome and non-completion. Behaviour Research and Therapy, 77, 68–77. https://doi.org/10.1016/j.brat.2015.12.009
- Lindsay, W. R., & Skene, D. D. (2007). The Beck Depression Inventory II and the Beck Anxiety Inventory in people with intellectual disabilities: Factor analyses and group data. Journal of Applied Research in Intellectual Disabilities, 20(5), 401–408. https://doi.org/10.1111/j.1468-3148.2007.00380.x
- Luteijn, I., Van der Nagel, J. E. L., Van Duijvenbode, N., De Haan, H. A., Poelen, E. A. P., & Didden, R. (2020). Post-traumatic stress disorder and substance use disorder in individuals with mild intellectual disability or borderline intellectual functioning: A review of treatment studies. Research in Developmental Disabilities, 105, 103753. https://doi.org/10.1016/j.ridd.2020.103753
- Mauritz, M. W., Goossens, P. J. J., Draijer, N., & Van Achterberg, T. (2013). Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illness. European Journal of Psychotraumatology, 4(1), 19985. https://doi.org/10.3402/ejpt.v4i0.19985
- McCarthy, J., Blanco, R. A., Gaus, V. L., Razza, N. J., & Tomasulo, D. J. (2017). Trauma- and stressor-related disorders. In R. J. Fletcher, J. Barnhill, & S. Cooper (Eds.), Diagnostic Manual - Intellectual Disability (DM-ID-2): A textbook of diagnosis of mental disorders in persons with intellectual disability (pp. 365–378). National Association for the Dually Diagnosed.
- Mevissen, L., Didden, R., & De Jongh, A. (2016a). Assessment and treatment of PTSD in people with intellectual disabilities. In C. R. Martin, V. R. Preedy, & V. B. Patel (Eds.), Comprehensive guide to post-traumatic stress disorders (pp. 281–299). Springer International Publishing Switzerland.
- Mevissen, L., Didden, R., & De Jongh, A. (2018). Handleiding diagnostisch interview trauma en stressoren - licht verstandelijke beperking. [ Manual diagnostic interview trauma and stressors - mild intellectual disabilites]. Accare.
- Mevissen, L., Didden, R., De Jongh, A., & Korzilius, H. (2020). Assessing posttraumatic stress disorder in adults with mild intellectual disabilities or borderline intellectual functioning. Journal of Mental Health Research in Intellectual Disabilities, 13(2), 1–17. https://doi.org/10.1080/19315864.2020.1753267
- Mevissen, L., Didden, R., Korzilius, H., & De Jongh, A. (2016b). Assessing posttraumatic stress disorder in children with mild to borderline intellectual disabilities. European Journal of Psychotraumatology, 7(1), 29786. https://doi.org/10.3402/ejpt.v7.29786
- Mevissen, L., Didden, R., Korzilius, H., & De Jongh, A. (2017). Eye movement desensitisation and reprocessing therapy for posttraumatic stress disorder in a child and an adolescent with mild to borderline intellectual disability: A multiple baseline across subjects study. Journal of Applied Research in Intellectual Disabilities, 30(S1), 34–41. https://doi.org/10.1111/jar.12335
- Mulder, C. L., Staring, A. B. P., Loos, J., Buwalda, V. J. A., Kuijpers, D., Sytema, S., & Wierdsma, A. I. (2004). De Health of the Nation Outcome Scales (HoNOS) als instrument voor ‘routine outcome assessment. [ The Health of the Nation Outcome Scales (HoNOS) as an instrument for routine outcome assessment]. Tijdschrift voor Psychiatrie, 46(5), 273–284. https://www.tijdschriftvoorpsychiatrie.nl/nl/artikelen/article/50-1238_De-Health-of-the-Nation-Outcome-Scales-HoNOS-als-instrument-voor-routine-outcome-assessment
- Nieuwenhuis, J. G., Smits, H. J. H., Noorthoorn, E. O., Mulder, C. L., Penterman, E. J. M., & Nijman, H. L. I. (2019). Not recognized enough: The effects and associations of trauma and intellectual disability in severely mentally ill outpatients. European Psychiatry, 58, 63–69. https://doi.org/10.1016/j.eurpsy.2019.02.002
- Nock, M. K., Michel, M. D., & Photos, V. (2007). Single-case research designs. In D. McKay (Ed.), Handbook of research methods in abnormal and clinical psychology (pp. 337–350). Sage Publications.
- Parker, R., Vannest, K., & Davis, J. (2011). Effect size in single-case research: A review of nine nonoverlap techniques. Behavior Modification, 35(4), 303–322. https://doi.org/10.1177/0145445511399147
- Penninx Quevedo, R., De Jongh, A., Bouwmeester, S., & Didden, R. (2021). EMDR therapy for PTSD symptoms in patients with mild intellectual disability or borderline intellectual functioning and comorbid psychotic disorder: A case series. Research in Developmental Disabilities, 117, 104044. https://doi.org/10.1016/j.ridd.2021.104044
- Pirkis, J. E., Burgess, P. M., Kirk, P. K., Dodson, S., Coombs, T. J., & Williamson, M. K. (2005). A review of the psychometric properties of the Health of the Nation Outcome Scales (HoNOS) family of measures. Health and Quality of Life Outcomes, 3(76), 1–12. https://doi.org/10.1186/1477-7525-3-76
- Powell, R. (2003). Psychometric properties of the Beck Depression Inventory and the Zung Self Rating Depression Scale in adults with mental retardation. Mental Retardation, 41(2), 88–95. https://doi.org/10.1352/0047-6765(2003)041
- Shalev, A., Liberzon, I., & Marmar, C. (2017). Post-traumatic stress disorder. New England Journal of Medicine, 376(25), 2459–2469. https://doi.org/10.1056/NEJMra1612499
- Shapiro, F. (2001). Eye‐movement desensitization and reprocessing: Basic principles, protocols and procedures (2nd) ed.). Guilford.
- Soylu, N., Alpaslan, A. H., Ayaz, M., Esenyel, S., & Oruç, M. (2013). Psychiatric disorders and characteristics of abuse in sexually abused children and adolescents with and without intellectual disabilities. Research in Developmental Disabilities, 34(12), 4334–4342. https://doi.org/10.1016/j.ridd.2013.09.010
- Van der Does, A. J. W. (2002). BDI-II-NL handleiding: De Nederlandse versie van de Beck Depression Inventory-2nd edition. BDI-II-NL Manual: The Dutch version of the Beck Depression Inventory - 2nd edition. Harcourt Test Publishers.
- Van Minnen, A., Zoellner, L. A., Harned, M. S., & Mills, K. (2015). Changes in comorbid conditions after prolonged exposure for PTSD: A literature review. Current Psychiatry Reports, 17(3), 17. https://doi.org/10.1007/s11920-015-0549-1
- Vannest, K. J., & Ninci, J. (2015). Evaluating intervention effects in single-case research designs. Journal of Counseling & Development, 93(4), 403–411. https://doi.org/10.1002/jcad.12038
- Vannest, K. J., Parker, R. I., Gonen, O., & Adiguzel, T. (2016). Single case research: Web based calculators for SCR analysis (version 2.0). singlecaseresearch.org
- Van Woudenberg, C., Voorendonk, E. M., Bongaerts, H., Zoet, H. A., Verhagen, M., Lee, C. W., Van Minnen, A., & De Jongh, A. (2018). Effectiveness of an intensive treatment programme combining prolonged exposure and eye movement desensitization and reprocessing for severe post-traumatic stress disorder. European Journal of Psychotraumatology, 9(1), 1487225. https://doi.org/10.1080/20008198.2018.1487225
- Wieland, J., Wardenaar, K. J., Fontein, E., & Zitman, F. G. (2012). Utility of the Brief Symptom Inventory (BSI) in psychiatric outpatients with intellectual disabilities. Journal of Intellectual Disability Research, 56(9), 843–853. https://doi.org/10.1111/j.1365-2788.2011.01440.x
- Wigham, S., Taylor, J. L., & Hatton, C. (2014). A prospective study of the relationship between adverse life events and trauma in adults with mild to moderate intellectual disabilities. Journal of Intellectual Disability Research, 58(12), 1131–1140. https://doi.org/10.1111/jir.12107
- Wilker, S., Pfeiffer, A., Kolassa, S., Koslowski, D., Elbert, T., & Kolassa, I. T. (2015). How to quantify exposure to traumatic stress? Reliability and predictive validity of measures for cumulative trauma exposure in a post-conflict population. European Journal of Psychotraumatology, 6(1), 28306. https://doi.org/10.3402/ejpt.v6.28306
- World Health Organization. (2013). Guidelines for the management of conditions specifically related to stress.
- Zoellner, L. A., Pruitt, L. D., Farach, F. J., & Jun, J. J. (2014). Understanding heterogeneity in PTSD: Fear, dysphoria, and distress. Depress Anxiety, 31(2), 97–106. https://doi.org/10.1002/da.22133