ABSTRACT
Creutzfeldt-Jakob disease (CJD) is a low-prevalence, fatal neurodegenerative disease. Parkinsonism as first symptom of CJD is rare. We present a case manifesting difficulty falling asleep as unspecific prodromal symptom and parkinsonism as initial symptom. The patient received positron emission tomography/computed tomography (PET/CT) of dopamine transporter (DAT) using 18 F-FP-CIT. The DAT-scan demonstrated presynaptic dopaminergic deficit in bilateral posterior putamen, which supports the hypothesis of nigrostriatal pathway dysfunction in CJD.
Background
Creutzfeldt-Jakob disease (CJD) is a low-prevalence, fatal neurodegenerative disease consisting of sporadic CJD (sCJD), familial CJD (fCJD), iatrogenic CJD (iCJD) and variant CJD (vCJD) [Citation1]. The global incidence of CJD approximately is 1–2 cases per million per year [Citation2]. The most common CJD is sCJD whose typical clinical features are rapidly progressive dementia, ataxia and myoclonus [Citation3]. Other clinical features including dizziness, agitation, depression, language disturbances and visual impairment have been also reported [Citation3–5]. However, parkinsonism as the initial symptom of sCJD is seldomly reported. Here, we present a case manifesting difficulty falling asleep as unspecific prodromal symptom and parkinsonism as initial symptom.
Case report
A 67-year-old woman visited the hospital due to a 5-month history of difficulty falling asleep in January 2022, without remarkable familial and past clinical history. As her electroencephalogram (EEG) and electrocardiogram (ECG) were negative, she was diagnosed with insomnia and treated with mirtazapine and eszopiclone. However, her symptom of difficulty falling asleep deteriorated and she presented progressive symptoms of emotion, cognization and motion during the following month. Then she was admitted to our hospital in February 2022. After admission, the patient appeared with symptoms of apathy, aprosexia, hypomnesia, bradykinesia, gait instability, bradylalia and occasional hand tremors. In the meantime, she received neurological examination which suggested hypermyotonia of extremities and tendon hyperreflexia.
Laboratory tests were normal, containing routine blood, urine tests, liver and kidney function, blood glucose, lipid, folic acid and vitamin B12 levels, tumour markers, autoimmune antibody levels. Also, screening tests for human immunodeficiency virus and syphilis were negative. Thyroid function suggested that thyroglobulin and antithyroid peroxidase antibodies were elevated to 151.00 μg/L, 16.39 IU/mL, respectively (normal range: 3.50–77.00 μg/L, <5.61 IU/mL, respectively).
EEG recordings suggested diffuse delta slow activities and no typical periodic triphasic sharp-wave complexes (PSWCs).
Cerebrospinal fluid (CSF) examination revealed that detection of 14-3-3 protein was positive and glucose mildly elevated to 4.06 mmol/L (normal range 2.2–3.9 mmol/L) and autoimmune-encephalitis-associated antibodies were negative.
In the brain MRI, diffusion weighted imaging (DWI) showed restricted diffusion within the cortical ribbon of bilateral frontal, parietal, temporal, occipital lobes and left insular lobes while fluid attenuated inversion recovery (FLAIR) sequence showed no significant abnormalities ().
Figure 1. (a-e) Diffusion-weighted imaging. (DWI); (f-j) 18 F-FDG PET/CT imaging DWI showed restricted diffusion within the cortical ribbon of bilateral frontal, parietal, temporal, occipital lobes and left insular lobes where 18 F-FDG PET/CT demonstrated hypometabolism.
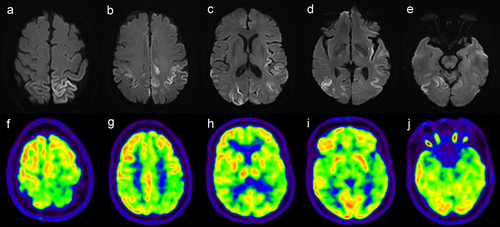
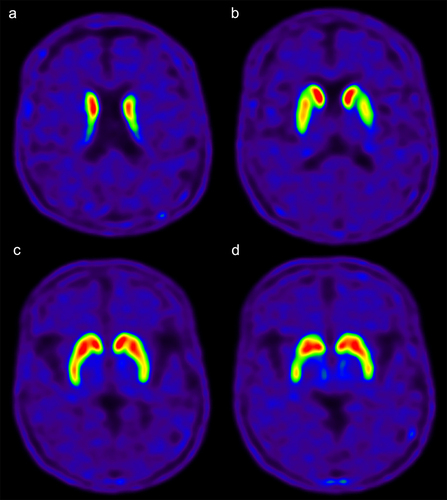
Given the extrapyramidal symptoms, the patient was assessed by PET/CT of dopamine transporter (DAT) and glucose metabolism using 18 F-FP-CIT and 18 F-FDG, respectively. 18 F-FP-CIT demonstrated decreased uptake in bilateral posterior putamen, especially on the left side (). 18 F-FDG PET/CT demonstrated hypometabolism in bilateral frontal, parietal, temporal, occipital lobes and left insular lobes, which was consistent with DWI ().
Figure 2. (a-d) 18 F-FP-CIT PET/CT imaging. 18 F-FP-CIT demonstrated decreased uptake in bilateral posterior putamen, especially on the left side.
Considering the possibility of Hashimoto’s encephalitis, the patient was treated with methylprednisolone and immunoglobulin for 5 days. Considering that the patient’s symptoms progressed gradually, the diagnosis of Hashimoto’s encephalitis was ruled out.
Discussion
According to progressive cognitive impairment, extrapyramidal and cerebellar signs, typical MRI brain scan and positive CSF 14-3-3, the patient was diagnosed with probable sCJD.
In previous research, hypothesis of nigrostriatal pathway dysfunction in CJD was proposed [Citation6]. Our case supports this hypothesis. In patients with suspected Parkinson’s disease, DAT-scan is a frequent examination. Considering this patient’s extrapyramidal symptoms including bradykinesia, occasional hand tremors and sign including hypermyotonia of extremities, she received DAT PET/CT examination which proved presynaptic dopaminergic deficit in bilateral posterior putamen. In the meanwhile, DWI showed no significant hyperintensity in bilateral basal ganglia. DAT PET/CT is a more preponderant detection of dopaminergic deficit than DWI. Besides, 18 F-FDG PET/CT showed hypometabolism in bilateral frontal, parietal, temporal, occipital lobes and left insular lobes, which was consistent with DWI. This finding accorded with conclusion that abnormalities in 18 F-FDG PET/CT were consistent with or more sensitive than DWI in CJD patients in previous reports [Citation7,Citation8]. PET/CT combined with MRI is able to detect earlier CJD.
To the best of our knowledge, cases about DAT PET/CT in CJD are rarely reported. The finding in our case, presynaptic dopaminergic deficit in CJD patients presenting parkinsonism at onset, is consistent with previous reports using 123I-FP-CIT single photon emission computed tomography (SPECT) [Citation9–11]. Some previous studies have shown that no definite presynaptic dopaminergic deficit was observed in their DAT-scan despite the existence of rapidly progressive parkinsonism [Citation12,Citation13]. Park et al. [Citation12] and Kim et al. [Citation13] assumed that postsynaptic dopaminergic dysfunction occurs before presynaptic dopaminergic deficit. The mechanism of nigrostriatal pathway dysfunction in CJD needs further researches.
In conclusion, nigrostriatal pathway dysfunction could explain parkinsonism in CJD. DAT PET/CT combined with MRI as non-invasive examinations can manifest specific abnormalities in brain and may serve as important approaches for studying pathogenesis and making early diagnosis of CJD presenting extrapyramidal symptoms and signs.
Consent to participate
Informed consent was obtained from individual participant included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Venneti S. Prion diseases. Clin Lab Med. 2010 Mar;30(1):293–309.
- Uttley L, Carroll C, Wong R, et al. Creutzfeldt-Jakob disease: a systematic review of global incidence, prevalence, infectivity, and incubation. Lancet Infect Dis. 2020 Jan;20(1):e2–e10.
- Baldwin KJ, Correll CM. Prion disease. Semin Neurol. 2019 Aug;39(4):428–439.
- Rabinovici GD, Wang PN, Levin J, et al. First symptom in sporadic Creutzfeldt-Jakob disease. Neurology. 2006 Jan 24;66(2):286–287.
- Krasnianski A, Kaune J, Jung K, et al. First symptom and initial diagnosis in sporadic CJD patients in Germany. J Neurol. 2014 Sep;261(9):1811–1817.
- Vital A, Fernagut PO, Canron MH, et al. The nigrostriatal pathway in Creutzfeldt-Jakob disease. J Neuropathol Exp Neurol. 2009 Jul;68(7):809–815.
- Xing XW, Zhang JT, Zhu F, et al. Comparison of diffusion-weighted MRI with 18F-fluorodeoxyglucose-positron emission tomography/CT and electroencephalography in sporadic Creutzfeldt-Jakob disease. J Clin Neurosci. 2012 Oct;19(10):1354–1357.
- Kiliç AK, Kaymakamzade B, Saka E, et al. The sole initial imaging finding in Creutzfeldt-Jacob disease: focal FDG-PET hypometabolism. Noro Psikiyatr Ars. 2018 Jul 4;56(3):226–228.
- Carrasco García de León S, Cabello JP, Ortiz R, et al. Parkinsonism associated with pathological 123I-FP-CIT SPECT (DaTSCAN) results as the initial manifestation of sporadic Creutzfeldt-Jakob disease. Case Rep Neurol Med. 2018 May 31;2018:5157275.
- Ragno M, Scarcella MG, Cacchiò G, et al. Striatal [123I] FP-CIT SPECT demonstrates dopaminergic deficit in a sporadic case of Creutzfeldt-Jakob disease. Acta Neurol Scand. 2009 Feb;119(2):131–134.
- Magnin E, Chopard G, Galmiche J, et al. Unusual dopaminergic depletion in variant Creutzfeldt-Jakob disease with early and rapid cognitive decline. Eur Neurol. 2011;65(6):368.
- Kim YE, Kim JM, Jeong HY, et al. Parkinsonism in early Creutzfeldt-Jacob disease: possible pre- and post-synaptic mechanism. J Neurol Sci. 2014 Aug 15;343(1–2):228–229.
- Park Y, Lee CN. A case of Creutzfeldt-Jakob disease presented as rapid progressive parkinsonism. Dement Neurocogn Disord. 2019 Dec;18(4):152–156.
