ABSTRACT
The meniscus is a relatively avascular fibrocartilaginous structure that provides a key role in shock absorption and load transmission. However, accurate diagnosis of meniscal retear can present a clinical challenge. The purpose of this study was to conduct a systematic review on the available literature, which compare the sensitivities, specificities, and accuracies of different diagnostic modalities of diagnosing knee meniscal retears in patients who have undergone surgical meniscal repair, such as Magnetic Resonance Imaging (MRI), Magnetic Resonance Arthrography with intraarticular contrast (direct MRA), and a combination of MRI and direct MRA. Two authors independently searched two databases (PubMed and Scopus) for literature related to knee meniscus retear according to the PRISMA guidelines. Four studies were found, which resulted in 291 patients with 293 menisci. All studies were published in 2008 and 2014. In our analysis, we calculated sensitivity to be 78.79% (95% CI, 64.07–93.51), specificity to be 56.58% (95% CI, 20.21–92.94), and overall accuracy to be 66.25% (95% CI, 54.29–78.22) for MRI and sensitivity to be 87.84% (95% CI, 83.93–91.74), specificity to be 88.68% (95% CI, 81.93–95.43), and overall accuracy to be 87.22% (95% CI, 82.22–91.62) for direct MRA. We recommend the use of direct MRA for the diagnosis of meniscal retears due to its higher sensitivity, specificity, and accuracy as compared to MRI and its reduced cost and invasive nature as compared to second-look arthroscopy. However, our review is limited by the number of studies available on this topic. More studies using study designs such as randomized controlled trials, involving MRI, direct MRA, and combinations of such techniques, should be performed to accurately assess the different techniques and aid in designing guidelines to guide the diagnosis of meniscal retears following meniscal repair.
1. Introduction
The meniscus is a relatively avascular fibrocartilaginous structure that provides a key role in shock absorption and load transmission. However, accurate diagnosis of meniscal retear can present a clinical challenge [Citation1]. Although knee arthroscopy is the gold standard for diagnosing meniscal tears, before subjecting the patient to surgical risks of arthroscopy the preferred modality to diagnose and characterize meniscal tears is Magnetic Resonance Imaging (MRI) [Citation2–5]. Proper identification of a retear is the key for treating the knee, which might prove challenging by the conventional MRI, due to the distorted anatomy of the meniscus postoperatively [Citation6–9]. Therefore, the purpose of this study was to conduct a systematic review on the available literature, which compare the sensitivities, specificities, and accuracies of different diagnostic modalities of diagnosing knee meniscal retears in patients who have undergone previous meniscal repair, such as MRI, Magnetic Resonance Arthrography with intraarticular contrast (direct MRA), and a combination of MRI and direct MRA.
2. Materials and methods
2.1. Literature search
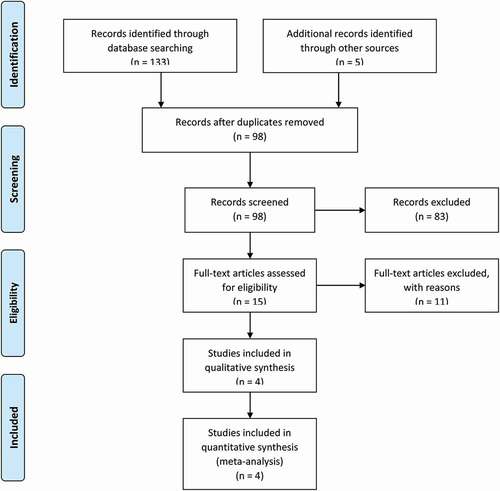
This study was designed as a systematic review based on the available literature and a comprehensive search of the literature following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines that was conducted on 30 November 2020 () [Citation10].
Two databases were searched in this systematic review: PubMed and Scopus by two independent reviewers (SS and MNZ). The search strategy employed keywords with appropriate BOOLEAN operators such as:
PubMed Search: Search: KNEE MENISCUS RETEAR Sort by: Most Recent
(‘knee’[MeSH Terms] OR ‘knee’[All Fields] OR ‘knee joint’[MeSH Terms] OR (‘knee’[All Fields] AND ‘joint’[All Fields]) OR ‘knee joint’[All Fields]) AND (‘meniscus’[MeSH Terms] OR ‘meniscus’[All Fields] OR ‘menisci’[All Fields]) AND (‘retear’[All Fields] OR ‘retearing’[All Fields] OR ‘retears’[All Fields])
2.2. Translations
KNEE: ‘knee’[MeSH Terms] OR ‘knee’[All Fields] OR ‘knee joint’[MeSH Terms] OR (‘knee’[All Fields] AND ‘joint’[All Fields]) OR ‘knee joint’[All Fields]
MENISCUS: ‘meniscus’[MeSH Terms] OR ‘meniscus’[All Fields] OR ‘menisci’[All Fields]
RETEAR: ‘retear’[All Fields] OR ‘retearing’[All Fields] OR ‘retears’[All Fields]
Scopus search: TITLE-ABS-KEY (knee AND meniscus AND retear)
Two authors (SS & MNZ) independently reviewed the abstracts of the studies and only studies eliminated in consensus were removed from the list. Two authors (SS and MNZ) independently reviewed the full texts of the studies. Following the systematic search, a snowballing method was used to identify additional relevant studies.
2.2.1. Inclusion criteria
Original research articles (prospective or retrospective cohort or case-controlled studies or randomized controlled trials) within the last 15 years, written in English language
Studies investigating diagnostic modalities such as MRI, direct MRA or a combination of MRI and direct MRA of knee meniscus retear after a meniscal repair surgery in comparison to second-look arthroscopy
Outcomes focused on were sensitivity, specificity and overall accuracy of the imaging modality.
2.2.2. Exclusion criteria
Studies investigating diagnostic modalities of knee meniscal tears in patients who have not undergone meniscal repair surgery
Case reports
Studies written more than 15 years ago
Review articles and meta-analyses
Book chapters
Conference abstracts
Expert opinions
Cadaveric or animal studies
Articles not written in English
We obtained 76 hits on PubMed and 57 hits on Scopus. Upon the elimination of duplicate articles, 98 articles remained. Eighty-three articles were excluded due to irrelevant focus to our study or meeting the types of published work satisfying the exclusion criteria. On full text screening, nine articles were excluded due to irrelevant focus, one article was excluded to being more like a review, and one article was excluded as being outdated by 25 years. The systematic search resulted in three studies. The snowballing search strategy resulted in another one study. In total, four studies were identified and analyzed after applying these criteria (). Articles in question were deliberated upon by the authors until consensus decision was reached.
Table 1. Summary of included studies
2.3. Data extraction and statistical analysis
Two authors (SS and MNZ) reviewed and extracted data from studies that satisfied the inclusion criteria. The following variables were extracted from each study: study design, year of publication, number of participants, number of menisci imaged, percentage of females (calculated), age (range and mean), diagnostic modalities compared, mean time gap between meniscal repair surgery and imaging protocol (in months), mean time gap between imaging protocol and second-look arthroscopy (in weeks), number of retears observed (calculated), number of retears proven arthroscopically, level of agreement between radiologists (Kappa test), radiological sign seen on MRI, type of magnet used in the study, sensitivity (%), specificity (%), PPV (%), NPV (%), accuracy (%), odds ratio, and confidence interval (95% CI).
Meta-analyses were done for sensitivity, specificity, and accuracy using STATA 16.0 software. Random effect model was fit and estimates were presented with 95% CI to find the pooled estimates. I2 statistic was used to assess the heterogeneity across the study. I2 over 50% was considered as heterogeneous.
3. Results
3.1. Risk of bias assessment
Bias assessment was performed using the MINORS criteria for non-randomized studies [Citation11]. Bias assessment included a clearly stated aim, inclusion of prospective patients, prospective collection of data, whether endpoints were appropriate to the aim of the study, unbiased assessment of study endpoint, whether follow-up period was appropriate to the aim of the study, loss to follow-up less than 5%, prospective calculation of the study size, and other biases not included in the criteria, such as blinding ad disagreement amongst radiologists. Our assessment of bias suggested high level of bias in one study (Kececi et al.), moderate level of bias in two studies (Cardello et al. and Magee T.), and low level of bias in one study (Cılız et al.). The study biases were summarized in .
Table 2. Assessment of bias using MINORS criteria
3.2. Patient and study characteristics
Four studies were found that resulted in 291 patients with 293 menisci. Two studies were published in 2008, and the other two were published in 2014. Four studies presented data on MRI findings, three studies presented data on direct MRA, and one study presented data on a combination of MRI + direct MRA. All the different modalities were compared to second-look arthroscopy as the gold standard. There was a variability in the types of magnets used for the MRI, which is shown in and 5. Summarized below is a synopsis of each diagnostic modality.
Table 3. Comparison between meniscal signs on MRI
Table 4. Comparison between meniscal signs on Direct MR arthrography
3.3. MRI
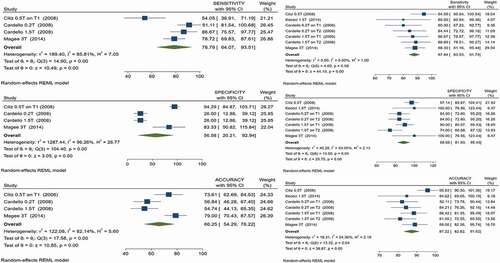
Three studies (Cardello et al., Magee T, and Cılız et al.) presented data regarding sensitivity, specificity, and accuracy [Citation1,Citation12,Citation13]. For some studies, positive predictive value and negative predictive value were manually calculated (). All studies compared meniscal shape changes indicating meniscal retears. The highest sensitivity was found in the paper by Cardello et al. to be 91.11 (95% CI, 78.78–97.52) with the 0.2 T magnet, the highest specificity was found in the paper by Cılız et al. to be 94.29 (95% CI, 80.84–99.30), and the highest accuracy was found in the paper by Magee T to be 79 (95% CI, 69.71–86.51).
In our analysis, we calculated sensitivity to be 78.79% (95% CI, 64.07–93.51, p-value: 0.00, heterogeneity, I2: 85.51%), specificity to be 56.58% (95% CI, 20.21–92.94, p-value: 0.00, heterogeneity, I2: 96.26%), and overall accuracy to be 66.25% (95% CI, 54.29–78.22, p-value: 0.00, heterogeneity, I2: 82.14%) ().
3.4. Direct MRA
All four studies (Cardello et al., Magee T, Cılız et al., Kececi et al.) presented presented data on direct MRA [Citation1,Citation12–14] (). The same types of magnets were used for each study as they did for MRI. All studies classified injecting gadolinium contrast material into the joint space as direct MRA. All studies compared contrast tracking into the tear in T1-weighted sequences as an indicator of meniscal retear. Cardello et al. presented data on T2-weighted images in addition to T1-weighted images and separated the data based on the type of magnet used (0.2 and 1.5 T). The highest sensitivity was found in the paper by Cılız et al. to be 94.59 (95% CI, 81.81–99.34), the highest specificity was found in the papers by Magee T and Kececi et al. to be 100 (95% CI, 54.07–100), and the highest accuracy was found in the paper by Cılız et al. to be 95.83 (95% CI, 88.3–99.13).
In our analysis, we calculated sensitivity to be 87.84% (95% CI, 83.93–91.74, p-value: 0.00, heterogeneity, I2: 0.00%), specificity to be 88.68% (95% CI, 81.93–95.43, p-value: 0.00, heterogeneity, I2: 53.05%), and overall accuracy to be 87.22% (95% CI, 82.22–91.62, p-value: 0.00, heterogeneity, I2: 54.36%) ().
3.5. Combination of MRI and direct MRA
One study (Magee T.) [Citation13] presented data on combination of MRI and direct MRA. Contrast tracking in the tear in T1-weighted sequences on 3 T magnet was considered as an indicator of meniscal retear. Sensitivity, specificity, PPV, NPV, and overall accuracy were either presented or calculated from the data presented in the paper to be 98.94% (95% CI, 94.21–99.97), 83.33% (95% CI, 35.88–99.58), 98.94% (95% CI, 93.95–99.82), 83.33% (95% CI, 40.79–97.32), and 98% (95% CI, 92.96–99.76) respectively.
4. Discussion
In our analysis we found significant heterogeneity between the data presented in the four studies. We found a higher sensitivity, specificity, and over accuracy with direct MRA as compared to MRI (87.84% vs 78.79%, 88.68% vs 56.58%, 87.22% vs 66.25%). Although a combination of MRI and direct MRA suggest a higher sensitivity, specificity, and overall accuracy, only one study presented such data and it is more cost ineffective and time-consuming than direct MRA only.
One study in our analysis had discrepancies in data representation. Cardello et el. switched their represented values in the article text and data tables when representing meniscal shape changes on MRI with 0.2 T and 1.5 T magnets. For this reason, we independently calculated values from the raw data presented in the articles.
One study by Applegate et al. described the presence of ‘meniscal ghosts’ which were poorly defined meniscal remnants seen on MRI which can cause difficulty in differentiating between the ends of the resected meniscus and granulation tissue [Citation15]. Another study by Vives et al. suggested that arthritic changes can affect the appearance of the knee of MRI [Citation16]. A study by Sciulli et al. found two potential causes for false-positive results on MRI, the first being that grade 1 and grade 2 lesions may be converted to grade 3 signal intensity and simulate a tear, as well as grade 3 signal intensity can be seen in repaired menisci long after they have healed [Citation17]. These could be some of the reasons that MRI was found to have a lower sensitivity, specificity, and overall accuracy than direct MRA.
We also found that recent studies did not assess the diagnostic efficacy of indirect MRA, which involves injecting intravenous contrast into the patient as compared to studies older than 15 years since publication. This could be because indirect MRA does not allow for joint space distension as compared to direct MRA, which can aid in the diagnosis of meniscal retears as suggested in the papers by Applegate et al. and Sciulli et al. [Citation15,Citation17]. Sciulli et al. found that the advantages to using MRA could be attributed to the properties of gadolinium-based contrast since it is less viscous than the synovial fluid making it more likely to be imbibed into a small cleft and aiding in the diagnosis of a meniscal tear, as well as that the use of gadolinium-based contrast allowed utilization of T1-wieghted pulse sequences with their inherently favorable signal-to-noise ratio. Cılız et al. recommended the use of direct MRA if Grade 3 signal intensity is the only finding on MRI in patients with more than 25% meniscal resection and who do not have sufficient joint effusion. The disadvantages of MRA are that it is an invasive, expensive, and time-consuming procedure [Citation1,Citation14]. Some reasons for false-negative results when performing direct MRA could be due to the formation of granulation tissue that obstructs the flow of the contrast material into the tear or if the contrast material is too viscous and doesn’t track into the meniscal tear [Citation17]. However, it is less invasive than second-look arthroscopy and may prevent unnecessary procedures [Citation14]. We intentionally decided to include studies only published within the last 15 years as the introduction of the PACS system and the use of newer magnets make some of the older studies’ results rendered obsolete [Citation13]. As such, the oldest and latest studies in our systematic review are separated by a gap of 7 years.
4.1. Limitations
There are a number of limitations to this systematic review. We only searched two databases and included only articles written in English. Different studies used different types of magnets, which may affect the image quality and diagnosis. This could be a reason that our meta-analysis contains significant heterogeneity between the studies. Since many studies are quite old, with our most recent study being published in 2014, most of them did not report a p-value for statistical significance. This review assesses whether a diagnostic modality is able to objectively aid in the detection of a meniscal retear and does not present data on the degree of prior partial resection or meniscal repair. A lot of the studies included were retrospective studies, with all studies presenting a selection bias in the sample chosen. In addition, most studies were evaluated by two radiologists and there may be some disagreement amongst the radiologists in the labelling of an image as a meniscal retear. Many studies also have a bias due to the lack of blinding due to ethical reasons. Due to similar ethical reasons, second-look arthroscopy was not performed in cases where MRI techniques failed to show a meniscal tear or in asymptomatic patients, which may affect the number of false negatives. Such patients may have clinically occult residual tears as described by a study by White et al. [Citation18]. All studies also use second-look arthroscopy as a gold standard to confirm meniscal retears after the imaging protocol, which presents its own limitations due to subjective expertise of the user performing the arthroscopy.
5. Conclusion
We performed a systematic review to identify the best imaging modalities in diagnosing meniscal retears following meniscal repair. We found that the highest sensitivity and overall accuracy of 100% to be with a combination of MRI and direct MRA. We found the sensitivity, specificity, and overall accuracy of direct MRA to be higher than that of MRI. Based upon the findings of our systematic review, we recommend the use of direct MRA for the diagnosis of meniscal retears due to its cost-effective nature and less invasive nature compared to a second look arthroscopy. However, our findings are limited due to the fact that a limited number of studies are published on this topic. More studies using study designs such as randomized controlled trials involving MRI, direct MRA, and combinations of such techniques should be performed in order to accurately assess the different techniques and aid in designing guidelines to guide the diagnosis of meniscal retears following meniscal repair.
Author contributions
SS drafted the study. SS and MNZ performed the systematic review and drafted the manuscript. JL performed the meta-analysis. RK suggested the topic, supervised the study and reviewed the manuscript. All authors read and approved the final manuscript.
Ethical approval
For this type of study formal consent is not required.
Registration and protocol
The systematic review was not registered on any register. The review protocol can be made available by contacting the correspondence author.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Cılız D, Cılız A, Elverici E, et al. Evaluation of postoperative menisci with MR arthrography and routine conventional MRI. Clin Imaging. 2008;32(3):212–8.
- Huysse W, Verstraete K, Verdonk P, et al. Meniscus Imaging. Semin Musculoskeletal Radiol. 2008;12(4):318–333
- Lefevre N, Naouri J, Herman S, et al. A Current Review of the Meniscus Imaging: proposition of a Useful Tool for Its Radiologic Analysis. Radiol Res Pract. 2016;2016:1–25.
- Maffulli N. Meniscal tears. Open Access Journal of Sports Medicine. 2010;45. 10.2147/OAJSM.S7753
- Raj MA, Bubnis MA. Knee Meniscal Tears. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. PUBMED ID: 28613721. July 19.
- DeHaven K. Meniscus Repair. Am J Sports Med. 1999;27(2):242–250.
- Farley T, Howell S, Love K, et al. Meniscal tears: MR and arthrographic findings after arthroscopic repair. Radiology. 1991;180(2):517–522.
- Magee T, Shapiro M, Williams D. Prevalence of Meniscal Radial Tears of the Knee Revealed by MRI After Surgery. AJR Am J Roentgenol. 2004;182(4):931–936.
- McCauley T. MR Imaging Evaluation of the Postoperative Knee. Radiology. 2005;234(1):53–61.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097.
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716.
- Cardello P, Gigli C, Ricci A, et al. Retears of postoperative knee meniscus: findings on magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) by using low and high field magnets. Skeletal Radiol. 2008;38(2):149–156.
- Magee T. Accuracy of 3-Tesla MR and MR arthrography in diagnosis of meniscal retear in the post-operative knee. Skeletal Radiol. 2014;43(8):1057–1064.
- Kececi B, Kaya Bicer E, Arkun R, et al. The value of magnetic resonance arthrography in the evaluation of repaired menisci. Eur J Orthop Surg Traumatol. 2014;25(1):173–179.
- Applegate G, Flannigan B, Tolin B, et al. MR diagnosis of recurrent tears in the knee: value of intraarticular contrast material. AJR Am J Roentgenol. 1993;161(4):821–825.
- Vives M, Homesley D, Ciccotti M, et al. Evaluation of Recurring Meniscal Tears with Gadolinium-Enhanced Magnetic Resonance Imaging. Am J Sports Med. 2003;31(6):868–873.
- Sciulli R, Boutin R, Brown R, et al. Evaluation of the postoperative meniscus of the knee: a study comparing conventional arthrography, conventional MR imaging, MR arthrography with iodinated contrast material, and MR arthrography with gadolinium-based contrast material. Skeletal Radiol. 1999;28(9):508–514.
- White L, Schweitzer M, Weishaupt D, et al. Diagnosis of Recurrent Meniscal Tears: prospective Evaluation of Conventional MR Imaging, Indirect MR Arthrography, and Direct MR Arthrography. Radiology. 2002;222(2):421–429.