1. Introduction
The respiratory functional defects can be evaluated by some tests exploring the ventilatory mechanics, such as spirometry and plethysmography, which determine airflows, dynamic lung volumes, and static lung volumes (SLVs) [Citation1–4] (). Indeed, the decrease in some spirometric [e.g.; ratio between the forced expiratory volume in the first second and the forced vital capacity (FEV1/FVC)] or SLV [e.g.; total lung capacity (TLC)] parameters allow to diagnose, respectively, obstructive ventilatory (OVD) and restrictive ventilatory (RVD) defects, and to assess their severities [Citation1–4]. Inversely, the increase of other parameters [e.g.; residual volume (RV), functional residual capacity (FRC)] retains the diagnosis of lung-hyperinflation [Citation1–3]. According to some scholarly societies [Citation1–5], the interpretation of the spirometric/SLV parameters requires a series of four steps [Citation6]. The first is a comparison of the parameters measured/calculated with these of reference predicted using norms (i.e.; reference equations) [Citation1,Citation2]. These norms are derived from tests carried out within a representative sample of the general population (i.e.; “healthy/normal’ subjects), having similar anthropometric, ethnic, socio-economic and environmental characteristics as the patient tested [Citation1–3]. According to the American thoracic society (ATS), a ‘healthy’ person is defined as one in whom there is: i) no presence of acute and no past chronic condition of the pulmonary system; ii) no major pulmonary condition in past medical history; iii) no systemic condition which may impact the pulmonary system and general state of well-being; iv) no history of upper respiratory tract infection during three weeks prior to exploration, and v) normal body composition taking into account ethnic group, vi) no more than incidental smoking experience (in children), vii) gestational age at least 37 weeks, and birthweight at least 2.5 kg (in infants), viii) no history of other than transient respiratory problems during the neonatal period (in infants), and ix) lifelong nonsmokers, or no more than incidental smoking experience (in adults) [Citation7]. Some authors have suggested more stringent criteria for defining ‘health’ [Citation8]. In the absence of specific intra-individual norms, the interpretation of spirometric/SLV parameters often encounters difficulties [Citation6]. Indeed, trustworthy interpretation of spirometric/plethysmographic results relies on the availability of appropriate norms to help differentiate between ‘health’ and ‘disease’ and to evaluate the severity and nature of any ventilatory defect [Citation4,Citation5,Citation9]. Among the five countries of the GAM (namely Tunisia, Algeria, Libya, Morocco, and Mauritania), only Mauritania has not established any spirometric/SLVs norms. Tunisia, Libya, Algeria, and Morocco has some spirometric and/or SLVs norms [Citation10–21]. The second step is a comparison of the determined parameter’ value with the distinctive thresholds of the main ventilatory defects (VDs) noted during chronic diseases [e.g.; OVD, RVD, mixed VD, non-specific VD, lung-hyperinflation) [Citation1,Citation2,Citation4]. In this context, norms are useful for classifying a spirometric/SLV parameter as decreased, normal or increased based on fixed thresholds (e.g.; 0.70, 70% or 80%) [Citation22], or more better on the 95% confidence interval (e.g.; lower limit of normal (LLN), upper limit of normal (ULN)) [Citation1,Citation2]. It is worth noting that the method based on a fixed threshold has major limitations [Citation23–25]. First, it is documented that the FEV1/FVC ratio declines with increasing age and height, even in healthy lifelong non-smokers, in whom the LLN drops below a ratio of 0.70 from about 45 years of age [Citation24]. Second, using the fixed ratio of 0.70 may result in under-diagnosis of OVD in young people and over-diagnosis in the elderly due to an age-related decline in pulmonary volumes, especially in FEV1 [Citation25]. This might lead to unnecessary use of medications and increased risk of adverse effects [Citation24,Citation25]. Since 2012, several vital developments related to the spirometric/SLV parameters, have occurred including i) the development by the GLI task force of multi-ethnic norms for spirometry (GLI-2012) [Citation5], and SLVs’ norms in individuals of ‘European’ ancestry” (GLI-2021) [Citation9], and ii) the application of more appropriate and novel statistical techniques for determining the LLN and ULN [Citation5,Citation9]. The LMS [lambda (skewness), mu (median), sigma (coefficient of variation)] method was applied and the ‘generalized additive models of location shape and scale’ was used [Citation5,Citation9]. In order to reflect variations in spirometric/SLV parameters distributions as people grow and age, LMS change with height and/or age [Citation9]. Based on the LMS technique, an additional method based on the determined parameters’ z-scores, was proposed to interpret spirometric/SLV parameters [Citation5,Citation9]. The LMS method allows modelling the expected mean (μ), the coefficient of variation (σ), and skewness (λ), and the z-score of any LFT parameter (e.g.; Y) is calculated as follows: z-score of Y = ((Y/μ)λ – 1)/(λ x σ) [Citation26]. The z-score is an index independent of height, age, sex and ethnicity, which indicates by how many standard deviations a subject’ spirometric/SLV parameter is deviated from its predicted value, with only 5% of healthy subjects having a z-score ≤−1.645 [Citation5,Citation9]. Unlike percentage predicted, z-scores are free from bias due to age, height, sex and ethnic group, and are therefore particularly useful in defining the LLN and ULN; they also simplify uniform interpretation of spirometric/SLVs results [Citation5,Citation9]. Both the GLI- 2012 and 2021 norms [Citation5,Citation9] were endorsed by several scholarly societies [e.g.; European respiratory society (ERS), ATS, pan African thoracic society].
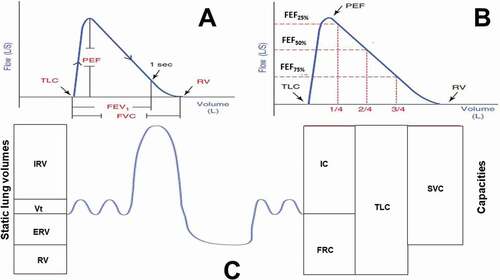
Figure 1. Lung function test parameters. A. Flow-volume curve. The following parameters can be extracted: TLC: represented by the left-most end of the curve (cannot be measured by spirometry); RV: represented by the right-most end of the curve (cannot be measured by spirometry); FVC: represented by the width of the curve; PEF: represented by the height of the curve; FEV1: the distance from TLC to the 1st second mark. B. Flow-volume curve demonstrating the effort-dependent (PEF and FEF75%) and the effort-independent (FEF50% and FEF25%) parameters. Instantaneous FEF% are directly determined from the curve by dividing the FVC into 4 quarters and getting the corresponding flow for the 1st, 2nd, and 3rd quarters representing FEF25%, FEF50%, and FEF75%, respectively. C. Different static lung volumes (on the left) and capacities (on the right).
Since the GLI- 2012 and 2021 norms [Citation5,Citation9] are now implemented by manufacturers of spirometric/plethysmographic devices and are commercialized in the GAM, it is capital to perform an update related to the possible application of the aforementioned norms in this region. This update will help clinicians/researchers from the GAM in interpreting spirometric/SLV parameters.
1.1. What are the data collected during the spirometric/plethysmographic tests?
Spirometry consists of performing vital capacity maneuvers [Citation1] (). The first maneuver is the FVC, which corresponds to the volume of air that can be forcefully and maximally exhaled after a maximal inspiration [Citation1]. During this maneuver, the spirometry measures dynamic lung volumes (l) [e.g.; FVC, FEV1], instantaneous forced expiratory flow (FEF at x% of FVC (FEFx%, l/s)), FEF between 25 and 75% of FVC (FEF25-75%), and peak expiratory flow (l/s) [Citation1] (). The second maneuver is the slow vital capacity (SVC, l) where the exhalation is intentionally slow. The SVC facilitates the determination of the inspiratory capacity (IC, l) [Citation1] (). During the plethysmography test, two SLVs (l) are measured (i.e.; expiratory reserve volume (ERV) and FRC) [Citation3] (). FRC is the volume of air that remains in the lungs at the end of a tidal exhalation, when the respiratory muscles are at rest [Citation3]. The calculated SLVs (l) are the RV (= FRC – ERV), and the TLC (= IC + FRC, or = SVC + RV] [Citation3] ().
1.2. What are the spirometric and SLVs norms available in the GAM?
exposes the spirometric/SLVs norms available in the GAM. Tunisia has some spirometric/SLVs norms for children [Citation13], adults [Citation12]; females aged ≥ 45 years [Citation11]; and elderly [Citation10]. Algeria has spirometric/SLVs norms for children [Citation19] and adults [Citation18]. Libya has spirometric norms for children [Citation17] and adult males [Citation16], and peak expiratory flow rate norms for schoolchildren [Citation15] and adolescents [Citation14]. Morocco has spirometric norms for children [Citation20] and adults [Citation21].
Table 1. Spirometric and static lung volumes (SLVs) norms available in the Great Arab Maghreb
Some remarks related to the aforementioned norms should be noted. First, there is no single norms across all ages. Second, some norms are old, such as Tunisian adults’ SLVs norms, which were published almost 27 years ago [Citation12], and some Libyan spirometric norms, which were established 33 years ago [Citation14,Citation16,Citation17]. Third, the Algerian SLVs’ norms generated from adults living in Constantine [Citation18] are not applicable in adult natives of Northern Algeria [Citation27]. Fourth, Libya and Morocco do not have SLVs’ norms.
1.3. Should the GLI-2012 spirometric norms be applied in the GAM?
In 2012, the GLI task force released the GLI-2012 spirometric norms from data collected from 72,031 healthy individuals (26 countries) aged 3–95 years [Citation5]. The GLI-2012 norms provided age-, height- sex-, and ethnic-specific norms and LLN/ULN for spirometry. Among the countries of the GAM, only Tunisia and Algeria have participated in the above-cited study. The spirometric values of 870 Tunisian aged ≥45 years and 273 Algerian aged 19 to 73 years were included in the Caucasian group (n = 55,428), and therefore the Tunisian and Algerian sample represents 2.06% of the Caucasian data.
In the GAM, the applicability of the GLI-2012 spirometric norms [Citation5] were evaluated only in Tunisia [Citation28] and Algeria [Citation29]. In Tunisia, the use of the GLI-2012 spirometric norms [Citation5] is controversial. On the one hand, a study including 1192 (104 females) adults aged 18 to 60 years, and where 489 adults (96 females) were healthy, advised against the use of the GLI-2012 spirometric norms (Caucasian group) in Tunisia [Citation28]. Indeed, using the Tunisian adults’ spirometric norms [Citation12], 71%, 19%, and 7% of the spirometric records were interpreted, respectively, as normal, as having a tendency through a RVD, and as having an OVD [Citation28]. Using the GLI-2012 spirometric norms [Citation5], these percentages became 86%, 8%, and 4%, respectively. In addition, the mean z-scores of healthy Tunisians were out of the normal range (i.e.; z-score between −0.5 and +0.5 [Citation5]) for FEV1 (−0.55 ± 0.87), and FVC (−0.62 ± 0.86), and only mean z-score FEV1/FVC (=0.10 ± 0.73) was well within physiologically range considered to be irrelevant [Citation28]. On the other hand, a multicenter African study recommended the use of the GLI-2012 spirometric norms (Caucasian group) in Tunisia [Citation30]. In this study, Tunisia was represented by 2362 healthy subjects [1266 females, age median (IQR): 38.3 (12.0–50.0) years] [Citation30]. FEV1, FVC, and FEV1/FVC z-scores were within the normal range, respectively, −0.12 ± 1.37, −0.26 ± 1.36, and 0.25 ± 1.11 [Citation30]. In Algeria, the use of the GLI-2012 spirometric norms is ‘recommended’ by the authors of a study including a convenience sample of 300 healthy non-smoker adults (150 females, age range: 18–85 years) recruited from the Algiers region general population [Citation29]. The total sample means ± SDs z-scores were 0.22 ± 0.87 for FVC, 0.04 ± 0.88 for FEV1, −0.34 ± 0.67 for FEV1/FVC, and 0.93 ± 0.79 for FEF25-75% [Citation29]. The authors supported the applicability of the GLI-2012 norms to interpret FEV1, FVC and FEV1/ FVC, but not the FEF25-75% [Citation29]. Moreover, the above-cited multicenter African study recommended the use of the GLI-2012 spirometric norms (Caucasian group) in Algeria [Citation30]. In this study, Algeria was represented by 409 healthy subjects [245 females, age median (IQR): 47.0 (32.7–60.4) years]. FEV1, FVC, and FEV1/FVC z-scores were within the normal range, respectively, −0.07 ± 0.90, −0.17 ± 0.88, and −0.41 ± 0.73 [Citation30].
External validation of the GLI-2012 spirometric norms, especially in Libya, Morocco and Mauritian, is recommended [Citation5]. The author of this update recommends the application of the GLI-2012 spirometric norms (Caucasian group) in the GAM. In this case, the old applied definitions retaining the diagnosis of some VDs [Citation2,Citation22,Citation28] should be updated by new ones [Citation4,Citation5,Citation9,Citation31] ().
Table 2. Old vs. new definitions/classifications of some ventilatory defects
1.4. Should the GLI-2021 norms for SLVs be applied in the GAM?
In 2021, the GLI task force released SLVs norms (GLI-2021) including 7190 observations from healthy individuals between the ages of 5 and 80 years [Citation9]. Observations were collected from 17 centers in 11 countries including Tunisia [Citation9]. Indeed, Tunisia was the only Arab and African country who participated in the aforementioned study [Citation9], and SLVs values of 615 Tunisians (341 females) aged 18 to 80 years (8.55% of total data) were included in the retained final sample from which the GLI-2021 norms were derived [Citation9]. Since Tunisian SLVs data were injected in the GLI-2021 SLVs norms [Citation9], the qualification of included individuals as having a ‘European ancestry’ is a source of ethnical and historical confusion [Citation32]. This point was largely discussed elsewhere [Citation32]. The GLI-2021 sex-specific norms [Citation9], which include height and age, were developed for TLC, FRC, RV, IC, SVC, ERV, and RV/TLC. Further evaluations of the applicability of the GLI-2021 SLVs’ norms in the GAM are required in order to verify their appropriateness in this region [Citation9]. The author of this update recommends the application of the GLI-2021 SLVs norms in the GAM. In this case, the old applied definitions to retain the diagnosis of some VDs [Citation2,Citation22,Citation28] should be updated by new ones [Citation5,Citation9,Citation31] ().
A 2021-ATS/ERS task force report [Citation4] has considered the 2005-ATS/ERS recommendations [Citation1–3], and has incorporated evidence from subsequent literature to establish new standard for LFT interpretation.
2. Where physicians/researchers can retrieve the GLI- 2012 and 2021 norms?
For the GLI-2012 norms [Citation5], a desktop individual calculator software for personal computers is available to generate predicted values, LLN and z-scores for each spirometric parameters in one’s own laboratory (https://www.ers-education.org/guidelines/global-lung-function-initiative/spirometry-tools/desktop-individual-calculator/).
For the GLI-2021 norms [Citation9], an online calculator was developed to calculate SLVs’ values (http://gli-calculator.ersnet.org/index.html). The calculator generates predicted values, z-scores, LLN, ULN, and percent predicted.
An online calculator has been developed to incorporate both GLI- 2012 and 2021 norms [Citation5,Citation9], in addition to the GLI-2017 norms for transfer factor for carbon monoxide [Citation33] (http://gli-calculator.ersnet.org/index.html).
For multiple records (e.g.; research studies), an Excel file processing functionality should be used. Physicians/scientists are asked to prepare an Excel file with the mandatory and optional input values for their calculator of interest and upload to the dedicated input field on the left of the calculator page (http://gli-calculator.ersnet.org/index.html). The mandatory variables to include in the Excel file are age, height, sex and ethnicity. The optional input values are the lung function tests (LFTs) parameters. For each LFT parameter, the software calculated several outcomes (i.e.; predicted value, LLN, ULN, and z-score). More details related to how obtain multiple records are available via this link: http://gli-calculator.ersnet.org/docs.html.
To conclude, the author of this update recommends to ascertain how well do the GLI- 2012 and 2021 norms [Citation5,Citation9] fit to contemporary spirometric/SLVs data in the GAM region, especially in Morocco, Libya and Mauritania. Waiting for such studies, the author of this update recommends the use of the aforementioned norms [Citation5,Citation9] in the GAM.
Acknowledgments
I dedicate this paper to the souls of my father Abdelhamid BEN SAAD and my two brothers Mehdi and Jamel BEN SAAD. I also dedicate this paper to my mother Khadija KHOUAJA who gave me her strength and her courage, who gave me wind in my wings. My mother supported my every step, encouraged all my dreams. My mother, no tribute could be equal to your excessive sacrifices, the love and tenderness you have never ceased to show. May God preserve you and grant you health, happiness and prosperity. To my wife Henda GHARBI, for your love, your patience and your constant support. To my three princesses Hana, Meriem and Molk: I apologize for not being able to find time to take care of you. I was so committed, that I did not notice that you grew up, quickly even very quickly.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–6.
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968.
- Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522.
- Stanojevic S, Kaminsky DA, Miller M, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2021;23:2101499.
- Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343.
- Ben Saad H. Interpretation of respiratory functional explorations of deficiency and incapacity in adult. Tunis Med. 2020;98(11):797–815.
- Stocks J, Quanjer PH. Reference values for residual volume, functional residual capacity and total lung capacity. ATS workshop on lung volume measurements. Official statement of the European respiratory society. Eur Respir J. 1995;8(3):492–506.
- Hopper JL, Hibbert ME, Macaskill GT, et al. Longitudinal analysis of lung function growth in healthy children and adolescents. J Appl Physiol (1985). 1991;70(2):770–777.
- Hall GL, Filipow N, Ruppel G, et al. Official ERS technical standard: global lung function initiative reference values for static lung volumes in individuals of European ancestry. Eur Respir J. 2021;57(3):2000289.
- Ben Saad H, Rouatbi S, Raoudha S, et al. Vital capacity and peak expiratory flow rates in a North-African population aged 60 years and over: influence of anthropometric data and parity. Rev Mal Respir. 2003;20(4):521–530.
- Ben Saad H, Tfifha M, Harrabi I, et al. Factors influencing pulmonary function in Tunisian women aged 45 years and more. Rev Mal Respir. 2006;23(4 Pt 1):324–338.
- Tabka Z, Hassayoune H, Guenard H, et al. Spirometric reference values in a Tunisian population. Tunis Med. 1995;73(2):125–131.
- Trabelsi Y, Ben Saad H, Tabka Z, et al. Spirometric reference values in Tunisian children. Respiration. 2004;71(5):511–518.
- Mukhtar MS, Rao GM, Morghom LO. Peak expiratory flow rates in Libyan adolescents. Indian J Physiol Pharmacol. 1989;33(4):223–227.
- Sagher FA, Roushdy MA, Hweta AM. Peak expiratory flow rate nomogram in Libyan schoolchildren. East Mediterr Health J. 1999;5(3):560–564.
- Shamssain MH. Forced expiratory indices in normal Libyan men. Thorax. 1988;43(11):923–925.
- Shamssain MH, Thompson J, Ogston SA. Forced expiratory indices in normal Libyan children aged 6-19 years. Thorax. 1988;43(6):467–470.
- Bougrida M, Ben Saad H, Kheireddinne Bourahli M, et al. Spirometric reference equations for Algerians aged 19 to 73 years. Rev Mal Respir. 2008;25(5):577–590.
- Bougrida M, Bourahli MK, Aissaoui A, et al. Spirometric reference values for children living in constantine (Eastern region of Algeria). Tunis Med. 2012;90(1):51–61.
- Bouti K, Benamor J, Bourkadi JE. Predictive regression equations of flowmetric and spirometric peak expiratory flow in healthy Moroccan children. J Clin Diagn Res. 2017;11(8):SC01–SC04.
- Bouti K, Maouni I, Benamor J, et al. Predictive regression equations of flowmetric and spirometric peak expiratory flow in healthy Moroccan adults. Int Sch Res Notices. 2017;2017:8985067.
- Celli BR, Halbert RJ, Isonaka S, et al. Population impact of different definitions of airway obstruction. Eur Respir J. 2003;22(2):268–273.
- Affes Z, Rekik S, Ben Saad H. Defining obstructive ventilatory defect in 2015. Libyan J Med. 2015;10:28946.
- Quanjer PH, Enright PL, Stocks J, et al. Open letter to the members of the GOLD committee. Rev Mal Respir. 2010;27:1003–1007.
- Sorino C, D’Amato M, Steinhilber G, et al. Spirometric criteria to diagnose airway obstruction in the elderly: fixed ratio vs lower limit of normal. Minerva Med. 2014;105(6 Suppl 3):15–21.
- Rigby RA, Stasinopoulos DM. Generalized additive models for location, scale and shape (with discussion). Appl Statist. 2005;54:507–554.
- Ketfi A, Gharnaout M, Ben Saad H. The plethysmographic reference equations established for adult natives of Eastern Algeria are not applicable to natives of Northern Algeria. Rev Mal Respir. 2019;36(7):870–879.
- Ben Saad H, El Attar MN, Hadj Mabrouk K, et al. The recent multi-ethnic global lung initiative 2012 (GLI2012) reference values don’t reflect contemporary adult’s North African spirometry. Respir Med. 2013;107(12):2000–2008.
- Ketfi A, Gharnaout M, Bougrida M, et al. The multi-ethnic global lung initiative 2012 (GLI-2012) norms reflect contemporary adult’s Algerian spirometry. PLoS One. 2018;13(9):e0203023.
- Masekela R, Hall GL, Stanojevic S, et al. An urgent need for African spirometry reference equations: the paediatric and adult African spirometry study. Int J Tuberc Lung Dis. 2019;23(8):952–958.
- Quanjer PH, Pretto JJ, Brazzale DJ, et al. Grading the severity of airways obstruction: new wine in new bottles. Eur Respir J. 2014;43(2):505–512.
- Ben Saad H. Do Tunisians have a European ancestry? Eur Respir J. 2021;58(1):2100761.
- Stanojevic S, Graham BL, Cooper BG, et al. Official ERS technical standards: global lung function initiative reference values for the carbon monoxide transfer factor for caucasians. Eur Respir J. 2017;50(3):1700010.
