ABSTRACT
Hydatid cyst is a major health problem in developing countries. The kidney is in third position of organs affected by hydatid cyst. One of the complications of renal hydatid cyst is a urinary fistula. The purpose of this study is to identify preoperative predictive factors of urinary fistula in renal hydatid cyst and to develop a scoring system for this disorder. We retrospectively analyzed all patients operated for renal hydatid cysts between January 2000 and December 2020. We divided our patients into two groups according to whether or not the renal hydatid cysts opened in the urinary tract. Predictive factors of the presence of a urinary fistula have been studied to obtain a simple score to predict the presence of a urinary fistula. Differences were considered significant if p < 0.05. Urinary fistula was detected in 33 of 96 patients. Univariate analyses showed significant differences in patient age, cyst size, location, hydaturia, eosinophil count, and platelet count between patients with and without urinary fistula. In multivariate analyses, hydaturia (p < 0.005), eosinophil count >500/mm3, (p = 0.01), cyst diameter >5 cm (p = 0.02), and upper or lower renal pole location (p = 0.003) were significant and independent predictors of urinary fistula. A score was developed to predict the opening of the cyst in the urinary tract. The total score varies between 0 and 15. The resulting area under the receiver operator characteristic curve was 0.798 (95% CI, 0.726–0.866; p = 0.023). At a cutoff point ≥8, the specificity achieved was 100%. Preoperative detection and management of urinary fistula are important issues in the treatment of renal hydatid cyst. Developing a scoring system based on routinely measured laboratory and radiologic factors will help the clinician to manage patients with renal hydatid cysts. External studies are needed to validate this new scoring system in routine clinical practice.
1. Background
Echinococcosis is a zoonotic disease caused by the larva of Echinococcus granulosus parasite [Citation1]. This parasitosis is endemic in regions where cattle and sheep farming is widespread. Hydatidosis is therefore a real public health problem in these regions. Renal localization is rare and ranks third (2–4%) after hepatic and pulmonary involvement [Citation1–3]. The renal hydatid cyst (RHC) can fistulize into the urinary tract, giving additional challenges for the diagnosis and treatment of this particular entity. The purpose of this study is to identify preoperative predictors of urinary fistula in renal hydatid cyst and to develop a scoring system for this disorder.
2. Methods
This is a descriptive, longitudinal, retrospective study carried out in our institution collected over a period of 20 years from January 2000 to December 2020. We included in this study all patients operated on in the department and whose anatomopathological proof of a hydatid cyst was brought. We excluded patients with fistulized cysts in anatomical structures other than the urinary tract or in whom the anatomopathological proof of a hydatid cyst was not provided or was not formal and patients with unusable or lost records. An analysis of all these data was carried out using IBM SPSS Statistics 25 software. The results of quantitative variables were presented as mean ± SD or median and interquartile range (IQR), and those of qualitative variables as number and percentage. For normally distributed variables, the t-test was used to compare two means, and analysis of variance was used to compare several means. For categorical variables, the chi-square test and Fisher's exact test were used in independent samples. Statistical analysis of the categorical data was performed using univariate binary logistic regression. Variables associated with urinary fistula in renal hydatid cyst in the univariate analysis (p < 0.05) were included in a multivariate model using binary logistic regression to determine the independent factors of this disorder. Odds ratios (OR) and 95% confidence intervals (CI) were calculated to evaluate the strength of any association that emerged. The regression coefficients were converted to weighted scores assigned to each variable by dividing each regression coefficient by half of the smallest regression coefficient and rounding to the nearest integer. Then, for each patient, the individual weighted scores corresponding to the predictors were summed to produce an overall weighted score. We used the ROC curve (Receiver Operating Characteristics) to qualify the performance of the score obtained by the sensitivity/specificity graphic representation. The discriminatory power of the prediction value was determined by the area under the receiver operating characteristic curve (AUROC). The sensitivity, the specificity, and the positive and negative predictive values (PPV, NPV) were obtained with standard methods and calculated at different cutoff values. P value of <0.05 was considered statistically significant.
3. Results
Ninety-six patients were included. The mean age of these patients was 46.08 ± 17.10 years. The sex ratio (M/F) was 0.81. Thirty-eight patients (39.6%) had reported hydatid contamination in their immediate surroundings. Lumbar pain was reported by 91.7% of our patients. Hydaturia was reported by 21 patients (21.9%). Lower urinary tract symptoms were observed in 45.8% of cases. Hematuria was found in 17.7% of cases. The hydatid cyst was located in the right kidney in 54 cases (56.3%) and in the left kidney in 42 cases (43.8%). Cystic formation was lower polar in 44.8% of cases, upper polar in 37.5% of cases, and mid-renal in 17.7% of cases. The average size of the cyst was 7.01 ± 4.1 cm. The mean eosinophil count was 461.1 ± 574.1/mm3. Hydatid serology (ELISA test) was positive in 40.6% of cases. RHC was classified according to the Gharbi ultrasound classification [Citation4]. The cyst was multivesicular type 3 in 52.1% of patients. The fistula was observed on computed tomography (CT) scan in three cases (9.09%). CT showed dilation of the excretory cavities in 42.6% of the cases and a fistula between the hydatid cyst and the urinary tract was visualized in three cases (9.09%). Thirty-three patients (34.37%) presented a fistulized renal hydatid cyst into the urinary tract. The treatment of open RHC in the urinary tract consisted of the resection of the prominent dome (partial pericystectomy) or total pericystectomy, respectively, in 75% and 25% of cases. The fistula was closed using separate stitches. Antegrade drainage using a ureteral double-J stent through the fistula or through a pyelotomy was performed in 43.8% of cases. The demographic and clinical characteristics of the patients with and without urinary fistula are compared in . Univariate analysis showed that patient age, cyst size, location, hydaturia, eosinophil count, and platelet count were associated with a significant risk of fistulized renal hydatid cyst in the urinary tract. Multivariate analysis concluded that a cyst size larger than 5 cm (p = 0.02), the polar location of the cyst (p = 0.003), hydaturia (p < 0.005), and an eosinophil count >500/mm3 (p = 0.01) were independent factors of fistulized renal hydatid cyst in the urinary tract. A score was developed to predict the urinary fistula (). The total score varies between 0 and 15. The area under the ROC curve for this score was 0.798 (95% CI, 0.726–0.866; p = 0.023) (). summarizes the sensitivity, specificity, PPV, and NPV of each cutoff value. At a cutoff point ≥1, the scoring system had a sensitivity of 91.9% and a specificity of 54.9%. This cutoff level was associated with a PPV and NPV of 52.5% and 86.8%, respectively. At a cutoff point ≥8, the sensitivity was 46.4% and the specificity was 100% with a PPV of 100% and an NPV of 46.4%.
Figure 1. The ROC curve for the predictive score of fistulized renal hydatid cyst into the urinary tract.
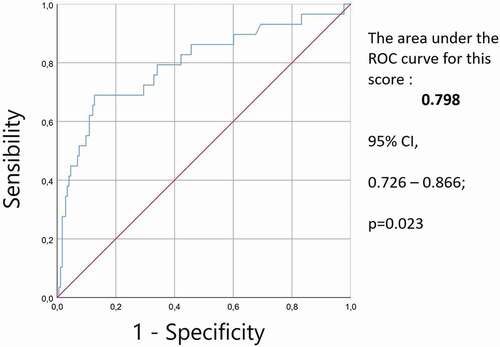
Table 1. Demographic and clinical characteristics of patients with or without a urinary fistula
Table 2. Weighted scores corresponding to predictive factors of the urinary fistula in patients with renal hydatid cysts
Table 3. The sensitivity, specificity, and predictive values of the weighted score predictive of urinary fistula at various cutoff points
4. Discussion
The hydatid cyst is an endemic disease in countries around the Mediterranean sea, and constitutes a public health problem [Citation5–7]. According to a Tunisian study conducted between 2001 and 2005 in 54 surgical departments of 35 hospitals in the country, the annual incidence rate of surgical hydatid cyst is 12.6 per 100.000 over this period, proving that the Hydatidosis remains a public health problem [Citation8]. This annual incidence rate has been falling slightly since the 1980s, when the incidence was 15.1 per 100.000 [Citation9]. Renal damage is most often initial, two hypotheses are found in the literature. The first justifies this isolated damage by the importance of the vascularization at the level of this organ, the second puts forward the hypothesis of a passage towards the retroperitoneal space through the lymphatic pathways [Citation10]. RHC can develop at any age, although it remains rare before the age of 12 years [Citation11,Citation12]. Slowly growing, RHC can remain asymptomatic for a long time and only manifest itself following a complication such as fistulization in the urinary tract or its compression [Citation13]. Lumbar pain, present in 91.7% of cases in our series, is the main symptom [Citation13]. Hematuria is secondary to friction caused by the passage of hydatid material through the urinary tract according to a first theory [Citation14], or secondary to caliceal fissure in a second theory [Citation15]. Hydaturia which is characterized by the presence in the urine of gelatinous material and membranes reminding grape skins in texture, is pathognomonic of a renal hydatid cyst ruptured into the collecting system [Citation16–18]. In the literature, hydaturia in renal echinococcosis is described as a rare event occurring only in 10–20% of cases and generally going unnoticed because microscopic [Citation19,Citation20]. Mellas et al, concerning 14 cases of open RHC in the urinary tract, 57% of the patients presented with hydaturia [Citation21]. In our series, hydaturia was present in 21.9% of cases. This difference in the frequency of hydaturia between the series treating only open RHC into the urinary tract and those treating RHC in general, demonstrates once again the importance of the search for this symptom. The second element that orients toward the rupture of a hydatid cyst into the urinary tract relies on blood biology. Hypereosinophilia is noted in 20–50% of the cases and is particularly increased in opened cyst [Citation18]. In our series, hypereosinophilia was noted in 37.7% of the cases. In case of rupture, RHC often causes severe lumbar pain. The release of daughter vesicles in the urinary tract can result in a true nephritic colic [Citation21]. The main serological methods used in the diagnosis and monitoring of human echinococcosis are based on the detection of anti-Ag IgG in hydatid fluid. Among these serological tests, we can mention Enzyme-Linked Immunosorbent Assay (ELISA), Indirect Hemagglutination test (HAI) and Western Blot (WB) [Citation22]. Some radiological signs, represented mainly by dilatation of the excretory cavities, also call for the diagnosis of an opened cyst into the urinary tract. Indeed, ultrasonography can already suspect rupture into the urinary tract when showing ureterohydronephrosis [Citation4]. CT scan can show a communication between the cyst and the urinary tract, especially during the excretory phase [Citation21]. The major risk during the surgical treatment of a hydatid cyst is it’s rupture. Treatment of an open renal hydatid cyst into the urinary tract is surgical and should be conservative whenever possible to preserve renal function. The choice of scolicide used is still a matter of debate. Some authors forbid the use of hydrogen peroxide in case of fistulized cysts because of a theoretical risk of erosion and sclerosis of the urinary tract [Citation3,Citation23]. Treatment of a urinary fistula between the cyst and the collecting system varies according to the size of the fistula and the aspect of the pericyst. In case of a minor fistula, closure using separate stitches without drainage of the urinary tract is sufficient [Citation24]. A large fistula should be closed after washing of the urinary tract and extraction of the hydatid material from the collecting system [Citation12]. In such cases, an internal drainage using a double J stent is necessary [Citation12]. Some authors recommend placing a ureteral catheter preoperatively when the diagnosis of a urinary fistula is suspected. It has a double interest: detecting the fistula by injection of methylene blue and therapeutic by protecting the cure of the fistula [Citation11]. To reduce the risk of suppuration, capsulorrhaphy or fat padding can be performed [Citation12]. Postoperative complications are dominated by a urinary fistula and suppuration of the residual cavity [Citation12]. Urinary fistula occurs in 2–7% of cases [Citation24]. It is mainly due to a fistula not identified during surgery or the presence of residual hydatid material in the urinary tract [Citation24]. Spontaneous drying can be achieved in about half of the cases. Otherwise, an internal drainage of the ureter is necessary [Citation24,Citation25]. The rate of postoperative suppuration was 8–10% [Citation24,Citation25]. It is most often treated by maintaining the drain for a few weeks. If this fails, surgical drainage is necessary [Citation24,Citation25]. The strong point of this study is the new system of notation of the independent factors of the RHC fistulized into the urinary tract. This score could reliably help to identify patients at risk. This score is easy to generate, does not include intraoperative variables, and, therefore, can be computed before surgery to avoid serious postoperative complications, in particular, urinary fistula and suppuration of the residual cavity. There are limitations to the current study. First, the study was retrospective in nature, with inherent selection bias and a small number of patients. In addition, a single-center study with internal validation only is performed. Despite these limitations, this individualized score can function as an effective tool to predict urinary fistula in patients with renal hydatid cysts.
5. Conclusion
Communication of a hydatid cyst with the collecting system is a frequent complication of this disease. The search for a fistula must be systematic during the intervention. We have shown that a large cyst size, a polar location, and the presence of hydaturia and hypereosinophilia were independent factors of fistulized renal hydatid cyst in the urinary tract. We have developed a new scoring system that can reliably identify patients at risk in order to guide surgical procedures and avoid complications.
Abbreviations
RHC: renal hydatid cyst; IQR: interquartile range; OR: odds ratios; CI: confidence intervals; AUROC: the area under the receiver operating characteristic curve; PPV: positive predictive value; NPV: negative predictive value; ELISA: linked immunosorbent assay; HAI: indirect hemagglutination test; WB: western blot; CT: computed tomography
Authors’ contributions
K.C. wrote and drafted the manuscript.
Y.N: Project development and manuscript correction.
Y.G. contributed to data collection.
Y.O. contributed to data collection, analysis, and interpretation.
All authors (K.C., Y.N., Y.G., and Y.O.) critically revised the manuscript, read, and approved the final version of the manuscript.
Ethics approval and consent to participate
The study was approved by the ethics committee of the Rabta University Hopital, Tunis.
Approval was granted by the Rabta University Hopital Local Ethics Committee (ID: 187165) (Approval date: 19.01.2020).
All methods were performed in accordance with the relevant guidelines and regulations set out by the Declaration of Helsinki.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets generated and analyzed during the current study are not publicly available due to patient privacy but are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Darbi A, Bassou D, Akjouj S, et al. Imagerie de l’hydatidose rénale. Feuill Radiol. 2008;48. 283–6.
- Ameur A, Lezrek M, Boumdin H, et al. Hydatid cyst of the kidney based on a series of 34 cases. Prog Urol. 2002;12:409–414.
- Benchekroun A, Lachkar A, Soumana A, et al. Hydatid cyst of the kidney. Report of 45 cases. Ann Urol. 1999;33. 19–24.
- Gharbi HA, Hassine W, Brauner MW, et al. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459–463.
- Dziri C. Hydatid disease-continuing serious public health problem: introduction. World J Surg. 2001;25:1–3.
- Develoux M, Gali A, Wartern A. Particularities of hepatic hydatidosis in black Africa. 32 hydatidosis cases observed in Niger Republic. Dakar Med. 1996;24:4–5.
- Nozais JP. L’hydatidose dans le bassin mediterraneen. Historique, repartition actuelle. Med Mal Infect. 1989;19:439–443.
- Chahed MK, Bellali H, Touinsi H, et al. Distribution of surgical hydatidosis in Tunisia, results of 2001-2005 study and trends between 1977 and 2005. Arch Inst Pasteur Tunis. 2010;87. 43–52.
- Bellil S, Limaiem F, Bellil K, et al. Épidémiologie des kystes hydatiques extrapulmonaires: 265 cas en Tunisie. Med Mal Infect. 2009;39:341–343.
- Okuş A, Sevinç B, Ay S, et al. Relation between serology and grow-up time in atypically localized hydatic cysts. Turkiye Parazitol Derg. 2013;37:257–261.
- Zmerli S, Ayed M, Horchani A, et al. Hydatid cyst of the kidney: diagnosis and treatment. World J Surg. 2001;25:68–74.
- Horchani A, Nouira Y, Kbaier I, et al. Hydatid cyst of the kidney. A report of 147 controlled cases. Eur Urol. 2000;38:461–467.
- Amrani A, Zerhouni H, Benabdallah FF, et al., Le kyste hydatique du rein chez l’enfant: à propos de 6 cas. 2003;Ann Urol. 37:8–12.
- Gharde P, Wagh D, Patil A. Left renal hydatid cyst presenting as hematuria and macroscopic hydatiduria since last ten years. Trop Parasitol. 2012;2:58–60.
- Fekak H, Bennani S, Rabii R, et al. Hydatic kidney cyst: 90 case reports. Ann Urol. 2003;37. 85–89.
- Ozturk A, Onur K, Ozturk E, et al. An unusual complication of renal hydatid disease: macroscopic hydatiduria. Eur J Radiol. 2005;54:35–37.
- Hamidi A, Enshaei A, Pourreza F, et al. Macroscopic hydatiduria: an uncommon pathognomonic presentation of renal hydatid disease. Iran J Public Health. 2015;44:1283–1287.
- Bhat GS, Burude VA, Hegde SD, et al. Isolated renal hydatid cyst masquerading as cystic renal cell carcinoma: a case report. J Clin Diagn Res. 2015;9:7–8.
- Amin MU, Siddique K, Aftab PA. Imaging features of renal hydatid cyst presenting with hydatiduria. J Radiol Case Rep. 2009;3:6–11.
- Parashari UC, Upadhyay D, Khanduri S, et al. Primary renal hydatidosis with associated macroscopic hydatiduria: a computed tomography urography diagnosis with pathological confirmation. Trop Doct. 2011;41:187–189.
- Mellas S, Mustapha A, Youness A, et al. Le kyste hydatique du rein fistulisé dans les voies urinaires, prise en charge diagnostique et thérapeutique A propos de 14 cas. Afr J Urol. 2010;16:27–32.
- Manzano-Roman R, Sanchez-Ovejero C, Hernandez-Gonzalez A, et al. Serological diagnosis and follow-up of human cystic echinococcosis: a new hope for the future? Biomed Res Int. 2015;2015:428205.
- Ben Khelil M, Allouche M, Banasr A, et al. Sudden death due to hydatid disease: a six-year study in the northern part of Tunisia. J Forensic Sci. 2013;58:1163–1170.
- Ketata H, Peyromaure M. Hydatid cyst of the kidney. Ann Urol. 2004;38:259–265.
- Kabbali N, Sqalli T. Fistulized renal hydatic cyst in a patient on chronic hemodialysis. Pan Afr Med J. 2017;28:219.
