Abstract
Our aim in this study was to examine which factors are associated with post-operative complications after surgery for pressure ulcers in individuals with spinal cord injury. We performed a retrospective cohort study including all spinal cord injured patients undergoing pressure ulcer surgery in our department between 2002 and 2019. Patient demographics and comorbidity were collected from medical records, as were treatment data and information on post-operative complications within 30 days. Assessment of outcomes was performed through t-tests, χ2-tests and ANOVA. Out of 118 operations, 51 (43%) had a post-operative complication of any kind. The vast majority (44 cases, 86% of all complications) had minor complications (Clavien–Dindo grade I or II). Seven patients (6%) had a complication of Clavien–Dindo grade III or higher, requiring return to theatre or ICU care. We found that a higher age, a low serum albumin (<3.5 g/dl), and over or underweight, were associated with an increased risk of complications (p < 0.05). Out of 143 treated ulcers, 132 were evaluated at a follow-up visit one to two months after surgery, and 99 of these (75%) were healed. Surgery of pressure ulcers in patients with spinal cord injury is not a low-risk venture, however, few patients will suffer serious post-operative complications. A majority of treated ulcers will heal shortly post-operatively. A number of risk factors are associated with post-operative complications, which can be of help to guide patient selection in the future.
Introduction
As many as 86% of spinal cord injured individuals will develop a pressure wound during their lifetime [Citation1–4]. Risk factors for pressure ulcers in this patient group include male gender, high age, complete spinal cord injury, metabolic syndrome, smoking, and overconsumption of alcohol [Citation5–7].
Pressure ulcers influence patient quality of life as well as self-esteem negatively [Citation8–10]. The risk of infections is elevated [Citation11,Citation12]. Furthermore, pressure ulcers are associated with high costs for the health care system [Citation13,Citation14]. A successful treatment strategy is of the essence for both patient and society. Superficial ulcers can heal on conservative treatment, while deeper ulcers may require surgical treatment. Successful surgery has been shown to improve both patient health and quality of life [Citation15].
Surgery and anesthesia on spinal cord injured patients involve specific challenges, due to the increased risk of spinal cord dysregulation such as autonomic dysreflexia and hypotension [Citation16,Citation17]. On the other hand, the risk of for example deep venous thrombosis is probably lower than among other patients [Citation18,Citation19].
As many as half of all patients develop post-operative complications such as wound dehiscence, local necrosis, or infection, however, no previous study has investigated other complications than flap-related, and only one looked at risk factors for complications [Citation15,Citation20–27]. Among 135 patients, Keys et al. found a high HbA1c and previous pressure ulcer surgery to be associated with increased risk of wound dehiscence, and younger age as well as low serum albumin (<3.5 g/dl) to be associated with flap necrosis [Citation26]. Two additional studies, not limited to spinal cord injured patients, found an increased risk of post-operative complications in individuals with female gender, renal failure, low serum albumin (<3.0 g/dl), or obesity [Citation27,Citation28]. Various surgical approaches for wound excision followed by coverage by musculocutaneous or fasciocutaneous flaps of different designs have been described [Citation25,Citation27,Citation29–33]. Whether one flap is preferable over others is unclear [Citation34].
The importance of a close, multidisciplinary collaboration between the surgical clinic and the rehabilitation clinic has been described previously [Citation20,Citation35]. Since 2002, we offer patients with spinal cord injury and pressure ulcers a comprehensive treatment program consisting of standardized perioperative care, surgery with flap coverage, and a four week post-operative rehabilitation regime, in a collaboration between Karolinska University Hospital and Rehab Station Stockholm. A first evaluation of patients treated 2002–2007 showed very promising results [Citation36].
The aim of this study was to examine the risk of immediate (within 30 days) post-operative complications after pressure ulcer surgery in spinal cord injured patients, and to identify potential patient-related or surgery-related risk factors for complications.
Material and methods
Treatment programme
Patients were offered surgery if they had a pressure ulcer category 4 which had not healed after 6–9 months of conservative treatment, and if they were motivated to participate in the post-operative rehabilitation programme. Patients had to be in a non-infectious state to be admitted to the treatment programme. A pre-operative CT scan was occasionally performed in severe cases to confirm suspected osteomyelitis, but the absence of an ongoing clinically significant infection was normally assessed through ulcer status and through inflammatory parameters. Regardless of radiologic findings, the extent of resection was determined by intra-operative wound status.
Included patients were admitted firstly via a visit at the rehabilitation clinic, and then admitted to the hospital ward 1–2 days prior to surgery. Blood samples were drawn and microbial swabs from the wound were taken. The patients underwent enema pre-operatively if they did not have an ostomy. A first meeting with nutritionist and physiotherapist took place upon admittance or immediately post-operatively. The operation was performed under general anaesthesia, where the wound was thoroughly excised and fistulas removed. Immediately underlying bone was removed and the remaining bony surface smoothed. The defect was covered with a musculocutaneous or a fasciocutaneous flap. No wound dressing was used. Wound drainages were kept for 4–7 days and removed when producing less than 40 ml per 24 h. All patients were treated with intravenous antibiotics (Cloxacillin and Metronidazole) followed by oral antibiotics for one week in total, starting the day of surgery.
Post-operatively, the patients lay in supine position in an air fluidized therapy bed (Clinitrone®, Hill-Rom), until transferred to the rehabilitation centre after 7–11 days. At the rehabilitation centre, the patients were given thorough information and instructions regarding transfers, positioning, toilet routines, self-care with skin check, and behavior to facilitate healing and to reduce risk of recurrent ulcers. Careful mobilization took place and after two weeks the patients were gradually allowed to sit. Patients were discharged after 4–5 weeks, with follow-up visits at the outpatient clinic within 60 days of surgery.
Patients
All spinal cord injured patients participating in our treatment programme for pressure ulcers between 1 January 2002 and 31 January 2019 were included in this retrospective cohort study. Patients were identified through a patient register kept by the responsible caregivers, as well as through a search of the pressure ulcer diagnosis code L89.X (ICD-10) in the electronic medical records system. Patients treated for chronic ulcers that were not pressure-induced, and non-compliance with the treatment programme, such as premature discharge from the rehabilitation clinic, or discharge from the hospital not to the designated rehabilitation clinic but elsewhere, were excluded. Individuals could participate more than once in the treatment programme, and each care episode was entered as one case of surgery and included in the analysis.
Data was collected retrospectively through the electronic medical records system, and assembled in an Excel® protocol. Data comprised of patient characteristics, including age, gender, smoking status, type and genesis of spinal cord injury, comorbidity, and prior medical history; wound characteristics, including location and previous surgery; and treatment, including type of surgery and adherence to standardized peri-operative antibiotics and antithrombotic treatment plan.
Information on all post-operative complications, occurring within 30 days from surgery, was collected, as was information on healing status at the first post-operative visit to surgeon or specialized wound care nurse, usually 30–60 days post-operatively. Complications were graded according to Clavien–Dindo [Citation37,Citation38]. The criterion for local infection was administration of antibiotics for clinical symptoms of infection, such as redness, swelling or tenderness, at the surgical site. The criterion for systemic infection was administration of intravenous antibiotics, or a switch in antibiotic regime, due to fever, elevated infectious parameters, or investigations revealing distant infections such as pneumonia or urinary tract infection. Complications were regarded as flap-related if they occurred at the site of surgery, and included wound dehiscence, flap necrosis, bleeding/hematoma, and surgical site infections. These could occur concurrently in the same patient and all complications were counted.
Statistical analysis
Assessment of outcomes was performed through t-tests, χ2-tests and ANOVA. Age was tested as a continuous variable as well as a categorical variable (0–18, 19–39, 40–59, 60–79, and ≥80), smoking was tested as a categorical variable (previous smoker, current smoker, and never smoker) and as a binary variable (ever smoker and never smoker), and BMI was tested as a continuous variable as well as a categorical variable (<19.0, 19.0–24.99, and ≥24.99). A p-value of 0.05 or smaller was considered statistically significant. Data was assessed per care episode, referred to as case, not per individual, since several individuals in the cohort participated more than once in the care programme. Statistical analysis was carried out using STATA version 13 (StataCorp, Texas, USA). The Regional Ethical Review Board in Stockholm, Sweden, approved the study (reference number 2018/694-31).
Results
We identified 138 cases of surgery in our records search (). Out of these, 5 cases were excluded due to surgery being for non-pressure-induced ulcers, 10 cases were excluded for not having any spinal cord injury, and 5 were excluded because they had surgery without being included in the treatment programme or because they opted out of all follow-up. A total of 118 cases of surgery, hereafter referred to as cases, operations, or care episodes, on 97 individual patients, hereafter referred to as patients, fulfilled the inclusion criteria, see . The majority of cases were male (82, 69.5%) and paraplegic (87, 73.7%), mean age at surgery was 49.7 years (standard deviation, SD, 17), and the most common cause of the spinal cord injury was trauma. At time of admittance for surgery, most cases had no known history of smoking (72, 62.6%) or of diabetes (102, 86.5%), and the mean BMI was 22.8 (SD 4). A colostomy, ileostomy, or sigmoidostomy was present in 29 (24.6%) of cases.
Figure 1. Flow chart. Cases identified through records search (138), exclusion criteria, and included patients (118).
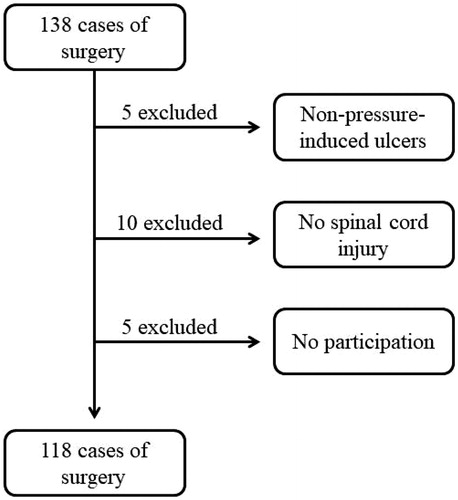
Table 1. Characteristics of the study population.
A majority of care episodes concerned only one pressure ulcer (97 episodes, 82.2%), whereas in 17 cases (14.4%) two ulcers on the patient were treated as the same time, and 3 wounds were surgically treated in the same session in 4 (3.4%) care episodes. Thus, in 118 cases of surgery, 143 pressure ulcers were treated in total.
Out of 143 treated pressure ulcers, 43 (30.1%) were known to be recurrent ulcers from previous surgery. The most common location of the pressure ulcer was the tuber ischii (109 wounds, 76.2%), followed by the trochanter major (19 wounds, 13.3%) and the sacrum or coccyx area (15 wounds, 10.5%). Flaps raised were musculocutaneous gluteal (81 ulcers, 56.6%), biceps femoris (29, 20.3%), fascia lata (12, 8.4%), and gracilis (1, 0.7%). In the remaining 20 cases (14.0%), one or more local fasciocutaneous flaps were used.
Out of 118 operations, 51 (43.2%) were followed by a post-operative complication of any kind (). The majority of complications (44 complications, 86.3% of all complications) occurring after these operations were minor complications of Clavien–Dindo grade I or II. Seven cases, corresponding to 5.9% of all cases, had a complication of Clavien–Dindo grade III or higher. Five of these required return to theatre because of bleeding, major wound rupture or substantial flap necrosis, and two required intensive care unit (ICU) management due to hyponatremia with seizures, and cardiac failure, respectively. There were no deaths (Clavien–Dindo grade V) in our study. An additional 13 cases (11.0% of all cases) had minimal wound dehiscence or local wound hematoma, treated conservatively, which were graded as Clavien–Dindo 0.
Table 2. Post-operative complications by Clavien–Dindo, with examples.
Compared to cases without post-operative complications, individuals with post-operative complications were older (mean age 54.9 versus mean age 45.8), more likely to have a low serum albumin pre-operatively (<3.5 g/dl) (68.3% versus 43.6%), and more likely to be under- or overweight (57.6% versus 42.4%) (p ≤ 0.05). Cases with post-operative complications were also to a larger extent women (47.2% versus 41.5%), underwent surgery for three concurrent wounds (75.0% versus 25.0%), had diabetes mellitus (56.3% versus 41.2%), or had an ostomy of any kind (55.2% versus 39.3%), although these differences were not statistically significant (p > 0.05 for all). Smoking, genesis to or type of spinal cord injury, location of ulcer, recurrent ulcer, or previous pressure ulcer surgery, did not appear to be associated with higher risk of post-operative complications.
One or more flap-related complications occurred in 30 cases (25.4% of all cases) (). Out of 28 cases of wound dehiscence, two needed surgical treatment. Two of the eight cases of hematomas or local bleeding required return to theatre, five were managed bedside through local evacuation and/or compression, and one only through blood transfusion. Out of five cases of flap necrosis four cases were partial and could be managed conservatively, whereas one was substantial and required surgical treatment. The frequency of complications did not vary between different flaps (p = 0.259).
Table 3. Flap-related complications.
Out of 143 treated ulcers, 132 were evaluated at a post-operative follow-up visit 30–60 days after surgery, out of which 99 ulcers (75.0%) were healed. Cases with post-operative complications (p < 0.01), cases of age 60 years or older (p < 0.01), and cases with low serum albumin (p < 0.05) were less likely to be completely healed at the first post-operative follow-up visit. Smoking, genesis to or type of spinal cord injury, location of ulcer, recurrent ulcer, or previous pressure ulcer surgery were not associated with lower healing rates.
Discussion
In this retrospective cohort study we reviewed 118 cases of surgery and standardized post-operative rehabilitative care for pressure ulcers in individuals with spinal cord injury. We found that although post-operative complications were common (43.2%), most consisted of minor complications, and serious complications of Clavien–Dindo grade III or IV were rare.
Our finding of 25% flap-related complications is similar to the findings of Biglari et al., who found an overall rate of 21% flap-related complications in 352 spinal cord injured patients undergoing pressure ulcer surgery, and considerably lower than two other studies, in which suture line dehiscence occurred among 49% and 31% of patients, and 16% and 13% required return to theatre, respectively [Citation22,Citation26]. In line with previous findings, wound dehiscence was the most common complication in our cohort, followed by infection and hematoma, however, only two individuals in our cohort required return to theatre because of wound dehiscence. We could not replicate the findings of Biglari et al. of difference in complication rates or types between different flaps.
The Clavien–Dindo classification of post-operative complications has gained widespread use, but this is to our knowledge the first study to use this classification for pressure ulcer surgery in this patient group [Citation37,Citation38]. Among 118 cases only seven patients (6%) had a complication of Clavien–Dindo grade III or IV. Schryvers et al. report a high re-admission rate in this patient group [Citation25]. We did not look at re-admissions to hospital, as the collaboration between the rehabilitation centre and the hospital usually allows for direct consultation in case of post-operative complications after discharge from the hospital.
We found higher age, low serum albumin, and over- or underweight to be associated with a higher risk of all post-operative complications. This is somewhat different from the findings of Keys et al., who similar to us found a low serum albumin to be a risk factor, but who, contrary to our findings, also identified young age and previous pressure ulcer surgery as risk factors [Citation26]. We found no such associations in our material.
Cases with post-operative complications were to a larger extent under treatment for diabetes mellitus, a finding which was not statistically significant, possibly due to low power. This could be in line with the findings of Keys et al. of a high HbA1c, as in dysregulated diabetes mellitus, to be associated with increased risk of complications [Citation26]. No other previous study has assessed risk factors for post-operative complications after pressure ulcer surgery in spinal cord injured patients, however, studies on other patient groups have identified female gender, obesity, and low serum albumin as risk factors, findings that are mostly in line with our results. Furthermore, we found that higher age and low serum albumin were associated with prolonged wound healing. Non-surprisingly, post-operative complications were related to prolonged wound healing.
Pressure ulcers are debilitating for the patient, but surgery is not first-line treatment. The decision to proceed with surgical excision and wound coverage should be made by the treating surgeon, wound care nurse, and the patient together. Our findings that high age, low serum albumin, and malnutrition - be it underweight or overweight - are associated with increased risk of post-operative complications and prolonged wound healing, are important factors to include in the decision of surgery.
The strengths of our study include the relatively large amount of cases in this specific patient group, the well-defined treatment programme, and the complete follow-up data. Limitations are the risk of misinformation or recall bias relative to the information of smoking, which was patient-reported, and a high amount of missing values in BMI. Furthermore, minor (Clavien–Dindo grade I) complications might not always be recorded in the medical journal, and some minor complications might have been missed due to incomplete recording.
In conclusion, we present our results from this review of 118 cases of surgery and standardized post-operative rehabilitative care according to a well-defined treatment programme for pressure ulcers in individuals with spinal cord injury. We present for the first time in this patient group post-operative complications according to the Clavien–Dindo classification, and we show that although post-operative complications are relatively common, serious complications are rare, and most wounds are healed at the initial follow-up visit. Our rate of flap-related complications in this treatment programme is similar to or lower than previously reported rates from similar cohorts. Furthermore, we identify high age, low serum albumin, and under- or overweight as risk factors for post-operative complications, and suggest these variables are taken into account in the clinical decision-making concerning these patients.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Sumiya T, Kawamura K, Tokuhiro A, et al. A survey of wheelchair use by paraplegic individuals in Japan. Part 2: prevalence of pressure sores. Spinal Cord. 1997;35(9):595–598.
- Garber SL, Rintala DH, Hart KA, et al. Pressure ulcer risk in spinal cord injury: predictors of ulcer status over 3 years. Arch Phys Med Rehabil. 2000;81(4):465–471.
- Joseph C, Nilsson Wikmar L. Prevalence of secondary medical complications and risk factors for pressure ulcers after traumatic spinal cord injury during acute care in South Africa. Spinal Cord. 2016;54(7):535–539.
- Scheel-Sailer A, Wyss A, Boldt C, et al. Prevalence, location, grade of pressure ulcers and association with specific patient characteristics in adult spinal cord injury patients during the hospital stay: a prospective cohort study. Spinal Cord. 2013;51(11):828–833.
- Chen Y, Devivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86(6):1208–1213.
- Li C, DiPiro ND, Cao Y, et al. The association between metabolic syndrome and pressure ulcers among individuals living with spinal cord injury. Spinal Cord. 2016;54(11):967–972.
- Li C, DiPiro ND, Krause J. A latent structural equation model of protective behaviors and pressure ulcer outcomes among people living with spinal cord injury. Spinal Cord. 2017;55(2):135–140.
- Langemo DK, Melland H, Hanson D, et al. The lived experience of having a pressure ulcer: a qualitative analysis. Adv Skin Wound Care. 2000;13(5):225–235.
- Lourenco L, Blanes L, Salome GM, et al. Quality of life and self-esteem in patients with paraplegia and pressure ulcers: a controlled cross-sectional study. J Wound Care. 2014;23(6):331–334, 6-7.
- Fuhrer MJ, Garber SL, Rintala DH, et al. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. 1993;74(11):1172–1177.
- Brunel AS, Lamy B, Cyteval C, et al. Diagnosing pelvic osteomyelitis beneath pressure ulcers in spinal cord injured patients: a prospective study. Clin Microbiol Infect. 2016;22:267 e1–8.
- Backhaus M, Citak M, Tilkorn DJ, et al. Pressure sores significantly increase the risk of developing a Fournier’s gangrene in patients with spinal cord injury. Spinal Cord. 2011;49(11):1143–1146.
- Kruger EA, Pires M, Ngann Y, et al. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013;36(6):572–585.
- Chan BC, Nanwa N, Mittmann N, et al. The average cost of pressure ulcer management in a community dwelling spinal cord injury population. Int Wound J. 2013;10(4):431–440.
- Singh R, Rohilla RK, Siwach R, et al. Surgery for pressure ulcers improves general health and quality of life in patients with spinal cord injury. J Spinal Cord Med. 2010;33(4):396–400.
- Israel JS, Carlson AR, Bonneau LA, et al. Reconstructive surgery and patients with spinal cord injury: perioperative considerations for the plastic surgeon. J Plast Surg Hand Surg. 2016;50(1):44–49.
- Moghimi MH, Reitman CA. Perioperative complications associated with spine surgery in patients with established spinal cord injury. Spine J. 2016;16(4):552–557.
- Moore RM, Rimler J, Smith BR, et al. Venous thromboembolism: a comparison of chronic spinal cord injury and general surgery patients in a metropolitan veterans affairs hospital. Plast Reconstr Surg. 2016;138(5):908e–914e.
- Rimler JC, Scholz T, Shbeeb A, et al. The incidence of venous thromboembolism in postoperative plastic and reconstructive surgery patients with chronic spinal cord injury. Plast Reconstr Surg. 2011;128(6):1230–1235.
- Josvay J, Klauber A, Both B, et al. The operative treatment of pressure sores in the pelvic region: a 10-year period overview. J Spinal Cord Med. 2015;38:432–438.
- Srivastava A, Gupta A, Taly AB, et al. Surgical management of pressure ulcers during inpatient neurologic rehabilitation: outcomes for patients with spinal cord disease. J Spinal Cord Med. 2009;32(2):125–131.
- Biglari B, Buchler A, Reitzel T, et al. A retrospective study on flap complications after pressure ulcer surgery in spinal cord-injured patients. Spinal Cord. 2014;52(1):80–83.
- Haiun M, Feuvrier D, Bayti T, et al. Surgical management of a series of pressure ulcers: report of 61 cases. Ann Chir Plast Esthet. 2016;61(6):836–844.
- Foster RD, Anthony JP, Mathes SJ, et al. Flap selection as a determinant of success in pressure sore coverage. Arch Surg. 1997;132(8):868–873.
- Schryvers OI, Stranc MF, Nance PW. Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil. 2000;81(12):1556–1562.
- Keys KA, Daniali LN, Warner KJ, et al. Multivariate predictors of failure after flap coverage of pressure ulcers. Plast Reconstr Surg. 2010;125(6):1725–1734.
- Tashiro J, Gerth DJ, Thaller SR. Pedicled flap reconstruction for patients with pressure ulcers: complications and resource utilization by ulcer site. JAMA Surg. 2016;151(1):93–94.
- Chiu YJ, Liao WC, Wang TH, et al. A retrospective study: multivariate logistic regression analysis of the outcomes after pressure sores reconstruction with fasciocutaneous, myocutaneous, and perforator flaps. J Plast Reconstr Aesthet Surg. 2017;70(8):1038–1043.
- Iida N, Watanabe A. Usefulness of simple-designed bilobed flap for reconstruction of ischial decubitus ulcer. Plast Reconstr Surg Glob Open. 2015;3(9):e525.
- Jordan SW, De la Garza M, Lewis VL. Jr. Two-stage treatment of ischial pressure ulcers in spinal cord injury patients: Technique and outcomes over 8 years. J Plast Reconstr Aesthet Surg. 2017;70(7):959–966.
- Sorensen JL, Jorgensen B, Gottrup F. Surgical treatment of pressure ulcers. Am J Surg. 2004;188:42–51.
- Lin CT, Ou KW, Chiao HY, et al. Inferior gluteal artery perforator flap for sacral pressure ulcer reconstruction: a retrospective case study of 11 patients. Ostomy Wound Manage. 2016;62(1):34–39.
- Mehta A, Baker TA, Shoup M, et al. Biplanar flap reconstruction for pressure ulcers: experience in patients with immobility from chronic spinal cord injuries. Am J Surg. 2012;203(3):303–306. discussion 6–7.
- Sameem M, Au M, Wood T, et al. A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg. 2012;130(1):67e–77e.
- Kierney PC, Engrav LH, Isik FF, et al. Results of 268 pressure sores in 158 patients managed jointly by plastic surgery and rehabilitation medicine. Plast Reconstr Surg. 1998;102(3):765–772.
- Ljung AC, Stenius MC, Bjelak S, et al. Surgery for pressure ulcers in spinal cord-injured patients following a structured treatment programme: a 10-year follow-up. Int Wound J. 2017;14(2):355–359.
- Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111(5):518–526.
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213.
