Abstract
Proximal migration of the thumb metacarpal has been suggested as a possible cause of remaining pain after trapeziectomy for trapeziometacarpal joint osteoarthritis. The aim of this study was to investigate if proximal migration after trapeziectomy is associated with a poorer long-term outcome in terms of pain and objective physical variables. We retrospectively examined 91 thumbs in 65 patients after a mean of 10 years following trapeziectomy with or without ligament reconstruction and tendon interposition. Proximal migration of the thumb metacarpal was measured on plain lateral radiographs of the thumb and correlated to visual analogue pain scale (VAS), thumb range of motion and strength. Most thumbs had a severe proximal migration of the first metacarpal, the mean scaphoid metacarpal distance was 2.7 mm. Most patients reported no or little pain, median VAS was 0 at rest and 1 after load. There were no differences in reported VAS pain at rest or after load between patients with severe (<2 mm scaphoid metacarpal joint space) or less severe (≥2 mm metacarpal joint space) proximal migration. Patients that reported more pain (VAS >2) did not exhibit more migration than patients reporting less or no pain. Thumbs with severe migration had weaker key pinch (3.4 vs. 4.6 kg, p = 0.008) and grip strength (15 vs. 21 kg p = 0.002). We conclude that proximal migration most likely does not cause residual or recurrent pain after trapeziectomy.
Background
Painful trapeziometacarpal joint osteoarthritis is very common, especially among elderly women [Citation1]. Four % of women over the age of 50 have a diagnosed trapeziometacarpal joint osteoarthritis [Citation2]. Trapeziectomy with or without ligament reconstruction and tendon interposition (LRTI) result in major pain reduction in majority of the patients. Still, some patients have remaining pain after trapeziectomy or experience recurrent pain some years after surgery [Citation3,Citation4].
Radiologically, the thumb metacarpal migrates proximally towards the scaphoid to a varying degree after trapeziectomy. It has been proposed that maintenance of the scaphoid metacarpal distance and prevention of proximal migration of the thumb metacarpal is important for the functional outcome [Citation5,Citation6]. Different tendons (flexor carpi radialis (FCR), abductor pollicis longus (APL), extensor carpi radialis longus (ECRL)) are used as interposition to achieve stability of the thumb metacarpal and prevent migration. However, LRTI has not shown to prevent proximal migration better than simple trapeziectomy [Citation7]. Although sparse, the available evidence suggest that subsidence of the thumb metacarpal does not affect clinical or subjective outcomes [Citation8,Citation9]. Accordingly, in our clinical experience, many patients with severe proximal migration report pain free, highly functional thumbs.
The aim of this study was to investigate if proximal migration of the thumb metacarpal after trapeziectomy with or without LRTI is associated with a poor long-term outcome in terms of pain and objective physical variables.
Method
The inclusion criteria were trapeziectomy with or without LRTI due to painful trapeziometacarpal joint osteoarthritis at least 8 years earlier. Exclusion criteria were dementia or other disorders that complicated communication.
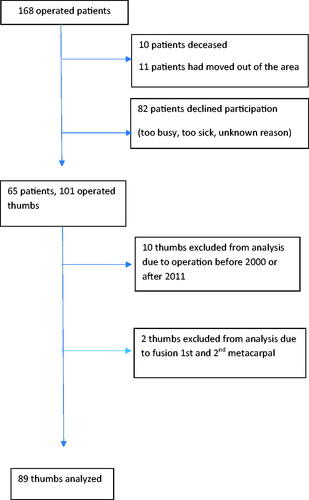
The patients were retrospectively identified in the local register for surgery performed at a specialized hand surgery unit. In total, 168 patients had been operated during the years 2007–2009 and were asked to participate in the study by letter and a following phone call. A flow chart of the patients is presented in . If a patient had been operated on the other thumb previously to 2007 or later than 2009, that thumb was included if operated between 2001 and 2011.
Plain radiographs of the thumb were taken (frontal, lateral and hyperpronated thumb view). Proximal migration was measured on the lateral radiograph [Citation7] as the minimum distance between the metacarpal and the scaphoid (). Two authors (UM and KE) assessed the radiographs and the inter-rater correlation of the measured scaphoid metacarpal distance was tested. A possible conflict between the first metacarpal and the trapezoid and osteoarthritis in the scaphoid-trapezoid joint was recorded. In cases where preoperative radiographs were available (n = 86), osteoarthritis was classified according to Eaton et al. [Citation10].
Pain was assessed with pain visual analog scale (VAS) at rest and immediately after load during the physical examination. Thumb palmar and radial abduction was assessed with a goniometer. Three-finger pinch, key pinch (intrinsic meter) and grip strength (JAMAR) were measured. The objective physical examinations were performed by an independent physiotherapist.
Statistics
The tested null hypothesis was that there is no difference in reported pain between thumbs with severe migration and thumbs with less migration. The patients were dichotomized in two groups according to the extent of migration. To detect a difference of 1.2 points in VAS pain [Citation11] and an estimated standard deviation (SD) of 1.5 [Citation9], 26 patients per group is required. Severe proximal migration was originally defined as a scaphoid metacarpal distance less than 5 mm which represents a migration of more than half the scaphoid metacarpal distance in most thumbs. Differences in pain VAS were analyzed with Wilcoxon rank–sum test and differences in objective physical parameters with t-test. Linear correlations between scaphoid metacarpal distance versus pain and objective physical parameters were tested with Spearman’s correlation test. All analyses were adjusted for age, gender and if the thumb has had secondary surgery. For pain VAS, the residuals of a linear model of the ranks was used with respect to age and gender. Pain VAS values are presented as median (IQR). Objective physical parameters and radiographic measurements are presented as mean (SD). p-Values < 0.05 were considered significant. The inter-rater and intra-rater reliability of the radiographic measurements of the scaphoid metacarpal distance was evaluated with the Intraclass correlation coefficient.
Results
presents descriptive data of the patients. 91 thumbs in 65 patients were examined after a mean of 10 (range, 8–15) years after the operation. Median VAS at rest was 0.0 (IQR 0.0–2.0) and median VAS after load was 1.0 (IQR 0.0–3.0). Fourteen thumbs had secondary surgery as listed in . Of these, four thumbs had two re-operations. Two thumbs had had a fusion between the first and second metacarpal. These two thumbs were excluded from further analyses since proximal migration could not be assessed. K-wire extraction (after first metacarpophalangeal joint (MCP1) fusion) or operations not directly related to the trapeziometacarpal joint such as De Quervain and ganglion cysts were not accounted for.
Table 1. Descriptive data of the patients.
Table 2. Secondary operations.
All in all, 89 thumbs were analyzed. There were no gender differences in pain at rest but men (n = 14) rated less pain after load than women (median 0.5 (IQR 0–0.5) vs. 1.5 (IQR 0–3.5) p = 0.008). Preoperative Eaton stage did not correlate with pain or objective physical variables.
In majority of the patients, there was a severe proximal migration of the first metacarpal. The mean scaphoid metacarpal distance was 2.7 mm (SD 1.7), median 2.4 (IQR 1.8–3.3). There was no correlation between time (years) since operation and scaphoid metacarpal distance (R2 < 0.001, p = 0.87). There was no difference in the scaphoid metacarpal distance between men and women. There was no difference in scaphoid metacarpal distance between patients operated with simple trapeziectomy or LRTI (mean scaphoid metacarpal distance 3.2 and 2.6 mm, respectively, p = 0.13). Likewise, there were no differences in pain or objective physical variables between simple trapeziectomy and LRTI. There was no difference in scaphoid metacarpal distance between thumbs that had a second operation and thumbs only operated on once. However, thumbs operated on more than once had more pain at rest (VAS 0.0 (0.0–1.0) vs 2.0 (0.0–5.5), p = 0.04).
The original plan was to compare patients with a scaphoid metacarpal distance less than 5 mm (severe migration), with patients with a scaphoid metacarpal distance of 5 mm or more (less migration). However, since the majority had migrated to much less than a scaphoid metacarpal distance of 5 mm, this was not applicable and to enable dichotomization we needed to redefine severe migration and choose a cut-off value of less than 2 mm which corresponds to the rounded median scaphoid metacarpal distance (2.4 mm) and the first quartile (1.8 mm) (n = 27). presents pain scores and objective physical variables according to migration group. There were no differences in VAS at rest or after load. The severe proximal migration group (n = 27) had significant less palmar abduction and weaker key pinch and grip strength.
Table 3. Pain and objective physical variables according to degree of migration.
presents linear correlations between the scaphoid metacarpal distance versus pain scores and objective physical variables. Key pinch was the only variable that significantly increased with increasing scaphoid metacarpal distance.
Table 4. Linear correlation between scaphoid the metacarpal distance versus pain scores and objective physical variables.
The 25% percentile of the patients that reported most pain at rest, i.e. VAS higher than 2 (n = 17) did not have significantly more migration than patients that scored 2 or less (mean scaphoid metacarpal distance 2.7 and 2.7 mm, respectively, p = 0.81).
In 79 thumbs (89%) there was a potential radiological conflict between the first metacarpal and the trapezoid. Patients did not report more pain at rest for thumbs with a potential metacarpal-trapezoid conflict. Radiographic osteoarthritis in the remaining scaphoid-trapezoid (ST) joint (n = 53) did not correlate with more pain or poorer objective physical function.
The inter-rater and intra-rater reliability of the radiographic measurements of the scaphoid metacarpal distance was very good; Intraclass correlation coefficient 0.90 (95%CI 0.85–9.94) and 0.96 (95%CI 9.94–0.98), respectively.
Discussion
This retrospective study shows that in the long-term, majority of the patients reported very low pain levels after trapeziectomy with or without LRTI and majority of the thumbs had a severe radiological proximal migration of the first metacarpal. We found no significant differences between patients with severe or less pronounced migration regarding pain and there was no linear correlation between the scaphoid metacarpal distance and reported pain. Hence the null hypothesis could not be rejected and based on the result of this study, it is not reasonable to attribute residual or recurrent pain to proximal migration. In further support of this, the few patients that reported higher levels of pain did not exhibit more migration than patients with no or little pain.
The group with severe migration had significantly weaker key pinch and grip strength. Biomechanically, a shorter thumb ray may reduce strength by decreased lever force. In contrast to our findings, Downing and Davis [Citation12] could not find any correlation between proximal migration and key pinch or tip pinch strength in 73 thumbs one year after trapeziectomy with or without LRTI. Similarly, Reissner et al. [Citation8] analysed 95 patients after trapeziectomy and LRTI and found that dorsal subluxation and proximal migration of the thumb metacarpal did not affect key pinch one year postoperatively. A possible explanation to the divergent findings could be that only very short scaphoid metacarpal distance affects strength, and one year postoperatively such grave proximal migration has not yet developed. A shorter scaphoid metacarpal distance also correlated with less palmar abduction. However, the difference was small and unlikely to be clinically relevant, and probably within the measurement error.
In accordance with our results, Reissner et al. [Citation8] did not find a correlation between proximal migration or subluxation and worse subjective outcome measured by the Michigan Hand Outcomes Questionnaire). Kriegs-Au et al. [Citation13] reported no correlation between proximal migration and tip-pinch strength or pain in 32 patients examined at least 32 months postoperatively.
We interpret the results as that proximal migration has no impact on remaining pain but could affect strength negatively. Pomares et al. [Citation9] also reported a short scaphoid metacarpal distance in 67 thumbs after a mean follow-up time of 10 years and in accordance with our findings, their sample reported a good outcome. Thus, it seems like proximal migration with time is inevitable but of no evident importance regarding pain.
A potential radiological conflict between the thumb metacarpal and the trapezoid was not associated with more pain. Radiological scaphoid trapezoid osteoarthritis did not correlate with thumb pain and is probably of little importance unless the patient has pain during wrist motion. Radiologically verified scaphoid-trapezium-trapezoid osteoarthritis often seems to be asymptomatic [Citation14] and this is likely to be the case after trapeziectomy as well.
There are several limitations of this study. It is retrospective and hence there is no baseline assessment. No patient reported outcome questionnaire regarding functional outcome was used with the rationale that elderly patients often have comorbidities that affect such scores, not least bilateral trapeziometacarpal osteoarthritis would make it difficult to interpret the results. Another weakness is that we could not present measurements of objective physical variables in relation to a healthy thumb since trapeziometacarpal osteoarthritis commonly is bilateral. Due to this, gender differences affected the strength measurements. This could be statistically corrected for. However, the within-gender inter-personal variance of strength could not be adjusted for and this bias might affect the correlation between migration and strength. There is a possible selection bias in this study. Some patients declined participation since they had no problems with their thumbs and were busy with other activities. Consequently, the examined sample was likely to have a worse outcome compared to decliners. We have included re-operated thumbs in the material thereby introducing a possible bias since thumbs that have undergone secondary surgery had more pain. We have adjusted for this statistically in the analyses. If this group, with the worse expected result, would have been excluded, another bias that cannot be corrected for, had been introduced.
The fact that the majority of the thumbs exhibited a severe subsidence is a problem and weakness of the analysis. We choose to dichotomize the material at 2 mm which was close to the median value and the first quartile of the scaphoid metacarpal distance. One must acknowledge that some patients in the ‘less severe’ group had a much more pronounced migration than the 5 mm we initially set as a limit.
This is a pragmatic study that reflects the clinician’s everyday situation. Hence, we did not use stress radiographs. Bhat et al. [Citation7] did not find notably different trapezial space height between 50 pairs of standard and stress radiographs obtained one year after trapeziectomy and conclude that the use of standard radiographs is valid to assess trapezial space height. We chose to measure the minimal scaphoid metacarpal distance on the lateral radiograph since it is easy, and the inter-rater validity was good.
In conclusion, it is not likely that proximal migration causes residual or recurrent pain after trapeziectomy. We advise against secondary surgery with the aim to correct migration with for example suture-button suspensionplasty or repeated LRTI in patients with pain after trapeziectomy. It is not reasonable to expose patients to the risk and potential harm of a re-operation when there is no convincing correlation between proximal migration and an inferior result in terms of pain.
Disclosure statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Sodha S, Ring D, Zurakowski D, et al. Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am. 2005;87:2614–2618.
- Moriatis Wolf J, Turkiewicz A, Atroshi I, et al. Prevalence of doctor-diagnosed thumb carpometacarpal joint osteoarthritis: an analysis of Swedish health care. Arthritis Care Res. 2014;66(6):961–965.
- Gangopadhyay S, McKenna H, Burke FD, et al. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37(3):411–417.
- Wilcke M, Roginski M, Åström M, et al. A registry-based analyzis of the patient reported outcome after surgery for trapeziometacarpal joint osteoarthritis. BMC Musculoskel Dis. 2020;21:63.
- Tomaino MM, Pellegrini VD, Jr, Burton RI. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg Am. 1995;77:346–355.
- Tomaino MM. Ligament reconstruction tendon interposition arthroplasty for basal joint arthritis. Rationale, current technique, and clinical outcome. Hand Clin. 2001;17(2):207–221.
- Bhat M, Davis T, Bannerjee A. Trapezial space height measurement after trapeziectomy: a comparison of the use of standard and stress radiographs. J Hand Surg Am. 2003;28(3):390–396.
- Reissner L, Marks M, Schindele S, et al. Comparison of clinical outcome with radiological findings after trapeziectomy with ligament reconstruction and tendon interposition. J Hand Surg Eur Vol. 2016;41(3):335–339.
- Pomares G, Delgrande D, Dap F, et al. Minimum 10-year clinical and radiological follow-up of trapeziectomy with interposition or suspensionplasty for basal thumb arthritis. Orthop Traumatol Surg Res. 2016;102(8):995–1000.
- Eaton RG, Lane LB, Littler JW, et al. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9(5):692–699.
- Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18(3):205–207.
- Downing ND, Davis TR. Trapezial space height after trapeziectomy: mechanism of formation and benefits. J Hand Surg Am. 2001;26(5):862–868.
- Kriegs-Au G, Petje G, Fojtl E, et al. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis: a prospective randomized study. J Bone Joint Surg Am. 2004;86(2):209–218.
- Wollstein R, Clavijo J, Gilula LA. Osteoarthritis of the wrist STT joint and radiocarpal joint. Arthritis. 2012;2012:242159.