Abstract
Magnetic resonance imaging (MRI) is a common diagnostic tool in hand surgery. However, there is limited knowledge on the kind of findings that are relevant in treatment planning. We analysed the findings and utility of arm, wrist, metacarpal, and finger MRIs taken in a tertiary hand surgery clinic of 318 consecutive images from 316 patients referred by a hand surgeon or hand surgeon resident. Ganglions (28%), findings on the extensor carpi ulnaris tendon (18%) and on the triangular fibrocartilage (18%) were the most common findings and increased with patient age; the clinical significance of these findings was minimal. The correlation between the clinical scaphoid shift test or the fovea sign test and MRI was also non-significant. Despite findings on MRI, the diagnosis remained unsolved in 76 (24%) cases. However, MRI had a role in reassuring the patient, and in 70% of the cases, further follow-up was unnecessary. This study demonstrates that the indications for wrist and hand MRI must be considered thoroughly and interpretation of the MRI report requires knowledge.
Keywords:
Introduction
Magnetic resonance imaging (MRI) is an important and standard diagnostic tool for evaluating pathologies of the wrist and hand. The advantage of MRI is a good visualization of soft tissue and bone without exposure to ionizing radiation [Citation1]. MRI has a high degree of accuracy for investigating cartilage lesions, ligaments, neoplasms, and bone marrow [Citation2,Citation3]. However, it is not clear how MRI correlates with the clinical picture. In many fields of musculoskeletal radiology, it is possible to detect numerous small findings on MRI of which the clinical relevance is unclear or subject to dispute [Citation4]. In addition, the learning curve for radiologists to become experts in wrist MRI is lengthy. More experienced observers make more sensitive, specific, and accurate radiological MRI interpretations than less experienced observers [Citation3,Citation5]. Other disadvantages of MRI include increased costs and delay in diagnostics due to possible limited availability [Citation6].
The appropriate use of MRI imaging for the evaluation of a painful wrist or hand is a topic of controversy. One study in children revealed that MRI has a major impact on management [Citation7], while another study concluded that MRI has only limited utility in generalized wrist pain [Citation8]. As the availability and the technique of MRI are improving, the role of MRI in hand surgery decision-making is increasing. Along with MRI, clinicians routinely use several documented provocative clinical tests, such as the distal radioulnar joint test, the triangular fibrocartilage complex stress test (TFCC test), and the scaphoid shift test (SS test) to arrive at the correct diagnosis. Unfortunately, there is little evidence for the accuracy of these tests [Citation9].
The correlation between clinical and MRI findings and the type of patient who would most benefit from advanced MRI remains unknown. Our aim was to describe an outcome analysis of the utility of MRI in a cohort of patients treated in our hand surgery clinic. This study addressed the following: indications for MRI, common findings in MRI, the correlation between clinical symptoms and MRI findings, and impact of MRI findings on treatment decisions.
Materials and methods
After obtaining institutional review board approval, we conducted a retrospective review of the electronic medical records in a tertiary hospital. All consecutive patients (n = 316) >15 years who underwent at least one arm, wrist or hand MRI investigation referred by a hand surgeon (n = 147) or a hand surgery resident (n = 171) between January and June 2016 were included in the study. If a patient had undergone multiple MRI examinations during the study period, only the first MRI was included in the study. Both MRIs were included if both arms were examined. The patient was imaged either with a GE Optima 430 1.5 T or Sigma HDxt 1.5 T MR scanner. Routine clinical MRI protocols, including coronal T1, PD with fat saturation, gradient-echo T2, sagittal T1, and axial PD and PD with fat saturation were used. The protocols varied based on the clinical question posed by the hand surgeon in the referral to the imaging department. The study included 38 (11.95%) images with intravenous contrast and 43 (13.5%) with arthrography. The locations for imaging were wrist (n = 193, 60.7%), metacarpals (n = 40, 12.6%), fingers (n = 81, 25.5%), thumb (n = 38, 10.7%), and antebrachium (n = 4, 1.3%). The primary MRI reports were analyzed by musculoskeletal radiologists in our university hospital. All MRI images were then re-evaluated by a musculoskeletal radiologist with 7 years of experience in musculoskeletal radiology.
Radiological diagnoses were obtained both from the primary MRI and the re-evaluated reports. All findings observed in bones, joints, ligaments, tendons, and soft tissues were recorded. Data from patient records prior to and after MRI on age, sex, medical history, the reason for visit (trauma, stress-related, tumour, unspecific pain, postoperative problem, tendinitis, arthritis, infection), clinical symptoms (location, pain, swelling, deformity, range of motion), waiting time for MRI and for the report, clinical visits, and procedures (operations or injections) were recorded.
The clinical scaphoid shift test (assessing possible damage to the SL ligament) and the fovea sign test (assessing possible foveal disruption of the distal radioulnar ligaments or ulnotriquetral ligament injuries) were compared with MRI findings. Patients were given one point on each finding in different anatomical structures (bones, tendons, ligaments, subcutis) and were divided according to age into three different groups (<30, 30–60, and >60 years). The correlation of summarized points and different age groups was calculated. In bivariate analysis, clinical tests and MRI findings were compared using Fisher’s exact test. Linear regression analysis was performed on the correlation of age and number of MRI findings.
A diagnosis was considered to have changed if the pre-MRI diagnosis was unspecific and had changed to a specific diagnosis after imaging, or if the clinical diagnosis was replaced by a diagnosis discovered on MRI that had not been considered clinically. The pre-MRI diagnosis remained the same if the clinical assumption and the MRI findings were the same or remained unknown if there was no explanation for symptoms on MRI. A change in medical management was considered as a difference between the pre- and post-MRI medical management, a recommendation for additional services, medications, referrals, or interventions (such as injection, arthroscopy, or surgery) based on MRI findings or lack of findings, or treatment cessation.
Results
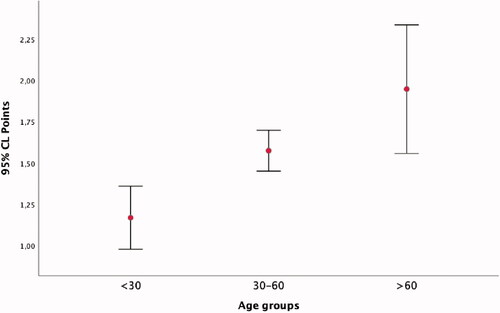
A total of 318 MRIs were included in the study as two patients had MRIs on both hands. Most patients were female (61.7%). The mean patient age was 40.5 years (range 15–79 years). The mean interval between the outpatient clinic and MRI imaging was 6.7 weeks (median time 6.1 weeks). A statistically significant increase of findings with respect to age could be demonstrated with linear regression analysis [F(1, 313) = 31.158, p < 0.001, R2 = 0.091) ().
Figure 1. A line diagram demonstrating the correlation between age and amount of MRI findings. Each patient received one point for each finding in a different anatomic structure (bones, ligaments, tendons, subcutis).
Indications for MRI, clinical correlation, lack of findings on MRI, unresolved cases, and change in management are shown in .
Table 1. Indication for MRI, mean age, clinical correlation on MRI, cases without findings, cases where the diagnosis was not resolved, and change in management after MRI.
Trauma was most often due to falls or sprains and appeared clinically as tenderness in the examined area. The clinical correlation between experienced pain and findings on MRI was 70%. No findings were observed in 18% of cases and the diagnosis remained unsolved in 30% of cases.
Stress-related discomfort was often work-related. Although MRI did not reveal any specific cause in 20% of cases, follow-up could be ended.
The most common masses observed on MRI (indication for MRI in n = 75) were ganglions (n = 90, 28.3%), followed by neurogenic tumours (n = 8, 2.5%), enchondromas (n = 7, 2.2%), giant cell tumours (n = 6, 1.9%), and arteriovenous malformations (n = 5, 1.6%). Although 44 of the ganglions were dorsally located, only 19 of the patients reported dorsal wrist pain. Other common findings on MRI were triangular fibrocartilage complex pathology (n = 58, 18%), extensor carpi ulnaris pathology (n = 56, 18%), bone cysts (n = 41), and arthrosis (n = 38). These typical findings rarely led to operative treatment ().
Table 2. Common findings from hand or wrist MRI, total amount of findings, and number of second-look findings and correlation to clinical examination (pain and movement restriction) and operative decision.
In the groups of patients with postoperative problems (8.2%) and patients with unspecific diffuse pain without any specific findings (4.7%), a clinical correlation on MRI was observed for half of the patients. Tendinitis (2.5%), arthritis (1.6%), and infection (1.3%) were found to a lesser extent.
The highest correlation between clinical examination and MRI findings was found for the mass group and the lowest for the group with unspecific pain. Although there were second-look findings in 88 (27.8%) cases (24–33% in every diagnostic group), most of these were of minimal or no clinical significance. The most common second-look findings were extensor carpi ulnaris (ECU) tendinopathy (n = 28, 31.8%) and ganglions (n = 25, 28.4%). In 10 cases (11.4%) with a primary diagnosis on MRI, after a second look, the MRI was considered to be normal. However, the second-look finding would have changed the course of treatment in 13 cases, as in six of these cases the second-look opinion was that there were no pathological findings on MRI. Two of these included the scapholunate ligament.
Overall, MRI led to a change in management in 221 cases (69.5%), which for 61 cases meant that follow-up could be ended. The diagnosis was changed in 134 cases (42%), the management and diagnosis in 120 cases (37.7%), and no change in management or diagnosis in 81 cases (25.5%). Change in management was observed the least often for the group including postoperative problems (). The diagnosis was not resolved in 45 (23.3%) of the wrist images, in 5 (12.5%) of the metacarpal images, and in 26 (32%) of the finger images.
In several cases, the patient was treated without MRI findings. One patient was operated on due to ECU pathology and two patients received a corticosteroid injection due to tendinitis in the first compartment without MRI findings. There were three TFC reinsertions even though the MRI reports stated a perforation diagnosis, and in 11 other cases, there was treatment, an injection, or an operation without an MRI finding. Postoperative procedures were planned for half of the patients suffering from postoperative problems, although there was no correlation between clinical and MRI findings in five of the cases. These included, for example, an ulna shortening osteotomy.
A cross-tabulation on MRI findings and clinical tests, including the scaphoid shift test performed on 118 patients and the fovea sign test performed on 92 patients, is shown in . A positive scaphoid shift test and a finding on MRI were reported in only 3/118 cases. Of all MRIs performed in the study, a finding on the SL in MRI was observed in 20 cases, including 13 dorsal lesions, five total ruptures, three partial ruptures, three post-injury states, and three distensions. A positive fovea sign test and a finding on MRI were reported in 5/92 cases. In 13 patients with a positive fovea test, eight were scheduled for an operation and six of these were operated, of which one patient had a TFC ligament reinsertion. Although statistical parameters (Fisher’s exact test) did reveal a slight correlation between the fovea sign test and the MRI result, the positive predictive values were weak.
Table 3. Crosstabulation of clinical tests (scaphoid test and fovea sign test) and MRI findings, results of Fisher’s exact test, and positive (PPV) and negative predictive values (NPV).
Various technical problems were reported in 28 (8.8%) of the MR images. The reasons included patient movement (15 cases), contrast medium in the wrong place (6 cases), significant pulsation artefacts (4 cases), and artefacts caused by foreign materials (3 cases). No specific risk factor, such as age, indication, or patient disease history, was associated with technical problems.
Discussion
Many studies have demonstrated the utility of wrist MRI imaging in the adult population [Citation10,Citation11]. However, it has been suggested that MRI will lead to inappropriate diagnoses and unnecessary treatment. MRI produces numerous findings; this was also true in our study. There were findings such as ganglions, bone cysts, and ECU pathology, which did not correlate with patient symptoms. This high rate of incidental findings presents challenges for clinicians. Thus, surgeons must be able to comprehend the significance of MRI findings to reassure patients with findings of uncertain clinical significance.
While the MRI findings did not always correlate with clinical diagnosis, the diagnosis also remained unsolved in several cases. MRI evaluation of the wrist and hand presents special challenges for the radiologist, as the clinically important structures are small, have complex anatomy, and have inadequate contrast to the surrounding structures. In our study, the diagnosis remained unsolved in 30% of finger MRIs.
In our study, there were also 88 (27.7%) second-look findings, even though the primary images were reviewed by musculoskeletal radiologists. This suggests that there can be inter-radiologist disagreement or the focus of the primary evaluation was influenced more by the clinical question.
Interestingly, three patients had an operation due to clinical examination on ECU pathology, which was not confirmed on MRI. This is consistent with a large multivariable analysis that revealed that ECU signal changes are common in the absence of clinical diagnosis and that nearly half of patients with a clinical diagnosis had no signal changes [Citation12]. This indicates that MRI is only of limited use in evaluating ECU pathology. A negative MRI does not always exclude injuries, particularly those of the TFCC or SL ligaments [Citation10,Citation13]. In our study, there were four re-attachment or triple tenodesis operations for SL injury, but only one had a total SL ligament injury in the primary MRI report. The decision to operate on the TFC complex was not based on MRI findings, as there was one re-insertion with MRI changes and three without.
We observed a limited correlation between the clinical tests and the MRI findings, as there was no convincing statistical correlation between the scaphoid shift test and the fovea sign test and the MRI findings. This is consistent with a previous study on several provocative tests, where most tests appeared to have little or no diagnostic value [Citation9].
The MRI report changed the course of management in almost 70% of cases, which can be considered a high rate. The diagnosis was changed in 42% of cases in this study, which is comparable to the 46% observed in children [Citation7]. In patients referred to MRI due to unspecific pain, MRI changed the management in 11 of 15 cases. However, none of these led to operative treatment but rather to an end of follow-up in most of these cases.
Wrist MRI is not an ideal screening tool in children and should only be used to exclude or confirm a specific diagnosis [Citation8]. In adults, MRI can be considered useful in cases where follow-up can be ended by reassuring the patient that the condition is benign. However, this suggests that a more convenient and less expensive examination method could be used. For example, ultrasound can detect some anatomical structures with similar sensitivity as MRI [Citation14]. Ultrasound has also yielded good results on diagnosing ganglions and TFCC injuries [Citation15] and soft tissue injuries [Citation16]. Ultrasound was used in only a few of the cases in our clinic.
There were some limitations to this study. This was a retrospective study and it was not clear how accurately the clinical findings were recorded in the electronic patient records. There were some patients who did not come to follow up after MRI and some did not have surgery even though it was scheduled. The reasons for this could not be determined from the electronic records.
Even more accurate imaging will be available in the future. There are already reports on 7T wrist MRI that provide improvement in visualization of the carpal complex [Citation17,Citation18]. It will be even more important to understand the indications to perform a wrist MRI and what findings could be expected. It is particularly important to define the pain area and the clinical question when ordering the MRI. The patient should also be informed about occult findings.
In conclusion, there were several non-significant findings in wrist and hand MRIs; such findings increased with age. MRI did not correlate well with single specific clinical tests, such as the scaphoid shift test or the fovea sign test. The diagnosis remained unsolved in several cases, but MRI could also be used in reassuring the patient about a benign condition. Second-look findings were of little clinical relevance.
Author contributions
Design of the study (MR, MS), Data collection (MR, MS), Data analysis (MR), Drafting the article (MR, MS, NL), Critical revision of article (MR, NL).
Disclosure statement
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Funding
References
- Boutin RD, Buonocore MH, Immerman I, et al. Real-time magnetic resonance imaging (MRI) during active wrist motion-initial observations. PLoS One. 2013;8(12):e84004.
- Ochman S, Wieskotter B, Langer M, et al. High-resolution MRI (3T-MRI) in diagnosis of wrist pain: is diagnostic arthroscopy still necessary? Arch Orthop Trauma Surg. 2017;137(10):1443–1450.
- Ringler MD. MRI of wrist ligaments. J Hand Surg Am. 2013;38(10):2034–2046.
- Hancock MJ, Kjaer P, Kent P, et al. Is the number of different MRI findings more strongly associated with low back pain than single MRI findings? Spine. 2017;42(17):1283–1288.
- Blazar PE, Chan PS, Kneeland JB, et al. The effect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J Hand Surg Am. 2001;26(4):742–748.
- Andersson JK, Hansson-Olofsson E, Karlsson J, et al. Cost description of clinical examination and MRI in wrist ligament injuries. J Plast Surg Hand Surg. 2018;52(1):30–36.
- Taylor KW, Moore MM, Brian J, et al. Wrist MR imaging in children: effect on clinical diagnosis and management. Clin Imaging. 2017;44:61–65.
- Gornitzky AL, Lin IC, Carrigan RB. The diagnostic utility and clinical implications of wrist MRI in the pediatric population. Hand. 2018;13(2):143–149.
- Prosser R, Harvey L, Lastayo P, et al. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. J Physiother. 2011;57(4):247–253.
- Hobby JL, Dixon AK, Bearcroft PW, et al. MR imaging of the wrist: effect on clinical diagnosis and patient care. Radiology. 2001;220(3):589–593.
- Karl JW, Swart E, Strauch RJ. Diagnosis of occult scaphoid fractures: a cost-effectiveness analysis. J Bone Joint Surg. 2015;97(22):1860–1868.
- Kuntz MT, Janssen SJ, Ring D. Incidental signal changes in the extensor carpi ulnaris on MRI. Hand. 2015;10(4):750–755.
- Andersson JK, Andernord D, Karlsson J, et al. Efficacy of magnetic resonance imaging and clinical tests in diagnostics of wrist ligament injuries: a systematic review. Arthroscopy. 2015;31(10):2014–2020.
- Chang CY, Kheterpal AB, Vicentini JRT, et al. Variations of anatomy on MRI of the first extensor compartment of the wrist and association with DeQuervain tenosynovitis. Skeletal Radiol. 2017;46(8):1047–1056.
- Lee SH, Yun SJ. Point-of-care wrist ultrasonography in trauma patients with ulnar-sided pain and instability. Am J Emerg Med. 2018;36(5):859–864.
- Oguz AB, Polat O, Eneyli MG, et al. The efficiency of bedside ultrasonography in patients with wrist injury and comparison with other radiological imaging methods: a prospective study. Am J Emerg Med. 2017;35(6):855–859.
- Nobauer-Huhmann IM, Pretterklieber M, Erhart J, et al. Anatomy and variants of the triangular fibrocartilage complex and its MR appearance at 3 and 7T. Semin Musculoskelet Radiol. 2012;16(2):93–103.
- Ladd ME, Bachert P, Meyerspeer M, et al. Pros and cons of ultra-high-field MRI/MRS for human application. Prog Nucl Magn Reson Spectrosc. 2018;109:1–50.
