ABSTRACT
Background: Posttraumatic stress disorder (PTSD) is a long-lasting and debilitating psychological disorder that affects a large portion of the population. Treatments such as Cognitive therapy for PTSD (CT-PTSD) and Eye movement desensitization and reprocessing (EMDR) have been shown to be effective and cost-efficient in clinical trials, but uptake and evidence of positive outcomes in real-world clinical services are limited. Implementation efforts have been hampered by providers’ concerns about the feasibility of trauma-focused treatments in more complex presentations (i.e. Complex PTSD).
Objective: To evaluate the effectiveness of CT-PTSD and EMDR in a real-world setting, as implemented in Norwegian outpatient mental health clinics for adults, and investigate the impact of probable Complex PTSD status on treatment outcomes.
Methods: Clinicians from 15 different outpatient clinics received training and supervision in EMDR or CT-PTSD as part of a national implementation project. 104 clinicians recruited and treated 196 participants with PTSD. Symptoms of PTSD, depression and anxiety were assessed session-by-session and used to estimate pre-post effect sizes. Mixed-models were employed to investigate the impact of complex PTSD.
Results: Both EMDR and CT-PTSD were associated with significant reductions in PTSD symptoms, with large effect sizes. Probable Complex PTSD was associated with higher levels of symptoms before and after treatment but did not significantly impact the effectiveness of treatment.
Conclusion: The use of evidence-based treatments for PTSD in routine clinical service is associated with good treatment outcomes, also for patients with Complex PTSD.
HIGHLIGHTS
Evidence-based treatments for PTSD, such as CT-PTSD and EMDR, are under-utilized in routine clinical services.
The use of CT-PTSD and EMDR in routine clinical service is associated with large reductions in symptoms for patients with PTSD.
Patients with probable Complex PTSD have equal reductions in symptoms.
Antecedentes: El trastorno de estrés postraumático (TEPT) es un trastorno psicológico duradero y debilitante que afecta a una gran parte de la población. Se ha mostrado que los tratamientos como la Terapia cognitiva para el TEPT (CT-PTSD en su sigla en inglés) y la Desensibilización y Reprocesamiento por Movimiento ocular (EMDR en su sigla en inglés) son efectivos y rentables en ensayos clínicos, pero la uso y la evidencia de resultados positivos en los servicios clínicos del mundo real son limitadas. Los esfuerzos de implementación se han visto obstaculizados por las preocupaciones de los proveedores sobre la viabilidad de los tratamientos centrados en el trauma en presentaciones más complejas (es decir, TEPT complejo).
Objetivo: Evaluar la efectividad de CT-PTSD y EMDR en un entorno del mundo real, tal como se implementa en las clínicas noruegas de salud mental ambulatorias para adultos, e investigar el impacto del probable TEPT complejo en los resultados del tratamiento.
Métodos: Los clínicos de 15 clínicas ambulatorias diferentes recibieron capacitación y supervisión en EMDR o CT-PTSD como parte de un proyecto de implementación nacional. 104 clínicos reclutaron y trataron a 196 participantes con TEPT. Los síntomas de TEPT, depresión y ansiedad se evaluaron sesión a sesión y se usaron para estimar los tamaños del efecto antes y después. Se emplearon modelos mixtos para investigar el impacto del TEPT complejo.
Resultados: Tanto EMDR como CT-PTSD se asociaron con reducciones significativas en los síntomas de TEPT, con tamaño de los efectos de gran magnitud. El TEPT complejo probable se asoció con niveles más altos de síntomas antes y después del tratamiento, pero no tuvo un impacto significativo en la efectividad del tratamiento.
Conclusión: El uso de tratamientos basados en la evidencia para el TEPT en el servicio clínico de rutina se asocia con buenos resultados del tratamiento, también para pacientes con TEPT complejo.
背景:创伤后应激障碍 (PTSD) 是一种长期存在且使人衰弱的心理障碍,影响了很大一部分人群。 PTSD 认知疗法 (CT-PTSD) 和眼动脱敏和再加工 (EMDR) 等治疗已被证明在临床试验中是有效且具有成本效益的,但在现实临床服务中正性结果的采用和证据有限。由于提供者担心聚焦创伤治疗在更复杂表现(即复杂性 PTSD )中的可行性,实施工作受到了阻碍。
目的:评估 CT-PTSD 和 EMDR 在现实环境中的有效性,如在挪威成人门诊心理健康诊所实施,并考查可能的复杂性 PTSD 状态对治疗结果的影响。
方法:作为国家实施项目的一部分,来自 15 个不同门诊诊所的临床医生接受了 EMDR 或 CT-PTSD 培训和监督。 104 名临床医生招募并治疗了 196 名 PTSD 参与者。对 PTSD 、抑郁和焦虑的症状进行逐次评估,并用于估计前后效应量。使用混合模型来研究复杂性 PTSD 的影响。
结果:EMDR 和 CT-PTSD 均与 PTSD 症状显著且具有大效应量的减轻相关。可能的复杂性 PTSD 与治疗前后更高的症状水平相关,但对治疗的有效性没有显著影响。
结论:在常规临床服务中使用 PTSD 循证治疗与良好的治疗结果相关,对于复杂性 PTSD 患者也是如此。
Posttraumatic stress disorder (PTSD) is estimated to affect 3.9% of the population. (Koenen et al., Citation2017). Untreated, the clinical course of the disorder is long and PTSD symptoms can persist decades after the traumatic experience (Kessler et al., Citation2005; Lassemo et al., Citation2017). PTSD is associated with functional impairment, reduced quality of life, and increased healthcare costs (Mavranezouli et al., Citation2020). Distress for patients is increased by high comorbidity rates, as people with PTSD typically also suffer from other symptoms such as depression, substance abuse, anxiety, or psychosis (Kessler et al., Citation2005). Complex symptom representations, especially when caused by repeated and prolonged interpersonal trauma, have been proposed as a separate diagnostic category termed Complex PTSD (Herman, Citation1992). The 11th edition of the International Classification of Diseases recognized Complex PTSD (CPTSD) as a diagnosis, defined by difficulties in emotional regulation, interpersonal relationships, and negative sense of self, in addition to PTSD symptoms of re-experiencing, avoidance, and persistent sense of threat (World Health Organization, Citation2019).
Clinical research has shown that PTSD can be effectively treated with psychotherapeutic interventions (Cusack et al., Citation2016; Mavranezouli et al., Citation2020). Based on comparative effectiveness and confidence in the evidence, treatment guidelines especially recommend individual trauma-focused interventions as first-line treatment for PTSD in adults (Bisson et al., Citation2019; National Institute for Health and Care Excellence, Citation2018). However, effective evidence-based treatments (EBTs) are infrequently available to patients in routine clinical services (Riggs et al., Citation2020), and a substantial gap exist between research and clinical practice (McHugh & Barlow, Citation2010). In order to close this gap, several large scale dissemination and implementation efforts have been initiated, such as the implementation of EBTs for PTSD by the Veteran Health Administration in the United States (Rosen et al., Citation2016) and the Improving Access to Psychological Therapies (IAPT) programme in the United Kingdom (Clark, Citation2018). These implementation programmes have shown that large-scale dissemination of EBTs is feasible in training clinicians to use these methods (Riggs et al., Citation2020). In Norway, the implementation of trauma-focused cognitive behavioural therapy for PTSD in children has been ongoing since 2012, while a project to implement EBTs for PTSD in adults was initiated in 2018 (Egeland et al., Citation2019).
However, many patients with PTSD are still not offered EBTs (Maguen et al., Citation2018; Murray, Citation2017). Reported barriers to implementation are described on many organizational levels, but one of the most important clinician-level barriers reported is attitudes about the effectiveness of EBTs (Rosen et al., Citation2016). Many clinicians remain concerned that the positive outcomes of EBTs for PTSD observed in clinical studies are not generalizable to ordinary clinical practice (Riggs et al., Citation2020), despite effectiveness research showing promising results (Eftekhari et al., Citation2013; Ehlers et al., Citation2013). This concern is especially related to patients with more complex presentations and CPTSD since the safety and effectiveness of trauma-focused treatments for CPTSD has been questioned (Bækkelund et al., Citation2021; Cloitre et al., Citation2010). It is argued that the problems with emotion regulation can interfere with the patients’ ability to tolerate trauma processing and that the heterogeneity of symptoms is not sufficiently addressed by standard EBTs (Karatzias & Cloitre, Citation2019).
It is therefore important to investigate the clinical outcomes of treatment delivered by routine clinical services, especially in patients with CPTSD. The main aim of the current study was therefore to investigate the clinical outcomes of EBTs for PTSD in ordinary clinical practice, delivered as part of a large-scale implementation effort in Norwegian clinical services for adults. We also examined if fulfilment of criteria for ICD-11 complex PTSD is associated with differences in outcomes.
1. Methods
1.1. Setting
The present study is based on data from an ongoing implementation of evidence-based practices for PTSD in Norwegian mental health services for adults. The implementation programme is initiated and financed by the Norwegian Ministry of Health and Care Services and led by the Norwegian Centre for Violence and Traumatic Stress Studies (NKVTS). The Norwegian health care system is semi-decentralized and consists of specialist and community care. Specialist mental health care is conducted by regional health trusts, and all treatments are without cost for the patients. There are 43 health trusts in Norway each responsible for one or more hospitals that include both inpatient and outpatient specialized mental health care services. Evidence-based treatments and practices for PTSD are implemented in these outpatient clinics for adults. The data for the present study were collected between August 2018 and December 2020, during the first round of implementation in 15 different clinics all over Norway. Details about the implementation project are further described by Egeland and colleagues (Citation2019).
1.2. Treatment
At the initiation of the implementation project it was decided to provide training in two different evidence-based treatments for PTSD: Cognitive therapy for PTSD (CT-PTSD; Ehlers & Clark, Citation2000; Ehlers & Wild, Citation2015) and Eye movement desensitization and reprocessing (EMDR; Shapiro, Citation2001; Shapiro & Laliotis, Citation2015). This was thought to increase flexibility and choice for providers. These two EBTs were chosen based on evidence of efficacy (Lewis et al., Citation2020; NICE, Citation2018) and existing training resources in Norway. Each therapist received training in either EMDR or CT- PTSD, based on therapist’s preference and needs of the clinic. Clinics were encouraged to train therapists in both EBTs. Training in both EBTs consisted of a three-day didactic workshop and ten hours of supervision. Workshops and supervision were provided by approved trainers and done in accordance with model standards. During supervision, therapists got feedback on a minimum of one taped recording of their sessions from their supervisors. Treatment length and frequency of sessions were not protocolled, but delivered as seen fit by the therapists and clinics.
1.2.1. Eye movement desensitization and reprocessing (EMDR)
EMDR is based on the Adaptive Information Processing model, conceptualizing psychopathology as a consequence of inadequately processed memories of adverse events (Shapiro, Citation2001; Shapiro et al., Citation2020). The treatment consists of eight phases designed to facilitate the reprocessing of traumatic memories. EMDR is most distinctly characterized by the therapeutic use of bilateral signals to guide the client's eye movements, thought to affect memory reconciliation through neurobiological mechanisms. EMDR received a strong recommendation for the treatment of adults with PTSD in the guidelines developed by the International Society for Traumatic Stress Studies (ISTSS; Bisson et al., Citation2019; Shapiro et al., Citation2020)
1.2.2. Cognitive therapy for PTSD (CT-PTSD)
CT-PTSD is based on the cognitive model of PTSD (Ehlers & Clark, Citation2000) and targets maintaining factors of the disorder through the elaboration of trauma memories, modification of trauma-related appraisals, and reduction of dysfunctional behaviours and strategies that maintain a sense of current threat (Ehlers, Citation2020). Based on available evidence, CT-PTSD received a strong recommendation for the treatment of adults with PTSD in the ISTSS guidelines (Bisson et al., Citation2019; Ehlers, Citation2020).
1.2.3. Treatment integrity
Up to five random recordings of sessions for each therapist were scored for fidelity by trained raters. For EMDR raters used Treatment Integrity Checklist EMDR, previously used in a Dutch clinical trial (de Bont et al., Citation2013), scoring the presence of 16 core components of the treatment. Cognitive Therapy for Post-Traumatic Stress Disorder: A Checklist of Therapist Competency, an adapted version of The Revised Cognitive Therapist Scale (Blackburn et al., Citation2001), was used to evaluate CT-PTSD.
1.3. Participants and procedures
Patients were recruited by therapists as training-cases, based on their clinical judgment and the patients’ preference. The only inclusion criterion was that the patient had received a clinical diagnosis of PTSD, according to ICD-10 criteria that are used in Norwegian health services. No other inclusion or exclusion criteria were specified. It was not required to conduct a structured diagnostic interview, but therapists were provided with screening tools for trauma history and PTSD symptoms (see Measures). Also, all therapists participated in a three-hour long workshop on trauma and how to diagnose PTSD. They were instructed on the scoring of the screening measures to diagnose PTSD, including evaluation of trauma and symptom criteria.
All therapists received a project iPad to be used for data collection, supervision, and recording of sessions. All data were encrypted and stored on secure servers for sensitive data at the University of Oslo. Patients registered informed consent and filled in self-report measures using the iPad. All procedures were approved by the Norwegian Regional Committees for Medical and Health Research Ethics (124871) and Data Protection Officials at each hospital.
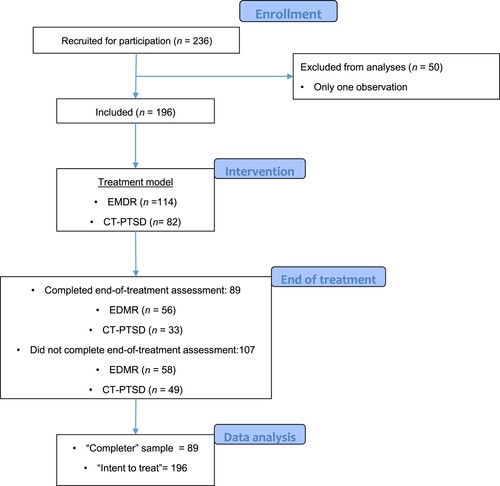
A total of 236 patients were recruited, but 50 participants had only one observation and were therefore excluded from the data analyses for the current paper (see ). The excluded patients were significantly younger (35.5 vs 37.3, t = −2.46, p = .015) and less likely to be incapacitated from work (64% vs 79%, Χ2 = 4.86, p = .040), compared to the included sample. Feedback reports on symptom trajectories and therapeutic alliance scores were available for the therapists through the project iPad. However, the use of self-report measures and feedback was not mandatory. Due to restraints from the ethical board, detailed information on the number of sessions and termination of treatment could not be collected.
1.4. Measures
1.4.1. Background information
A generic form developed for the project was used to record demographic information, cultural and ethnic background, education and socioeconomic status, work status, and previous treatment history. The form was filled out at the first session.
1.4.2. Stressful life events screening questionnaire (SLESQ; Goodman et al., Citation1998)
Trauma history was assessed at the first session with a revised version of the Stressful Life Events Screening Questionnaire asking for the patient’s exposure (yes or no) to 14 different trauma events, including natural disasters, life-threatening illnesses, sexual abuse, interpersonal violence, and psychological abuse. A 15th item allows the respondent to specify other frightening or horrific experiences that are not included in the other items.
1.4.3. PTSD checklist for DSM-5 (PCL-5; Weathers et al., Citation2013)
PCL-5 was used to assess PTSD symptoms at each session. It consists of 20 items measuring PTSD symptoms, scored on a scale from 0 (‘not at all’) to 4 (‘extremely’), indicating how much the respondent has been bothered by this symptom the last month. The Norwegian translation of PCL has previously shown good psychometric properties (Hem et al., Citation2012). Cronbach’s alpha in the present study was .922.
1.4.4. The international trauma questionaire (ITQ; Cloitre et al., Citation2018)
ITQ consists of 6 items measuring PTSD and 6 items measuring disturbances in self-organization (DSO). The latter subscale was used in this study to assess if patients fulfilled the criteria for ICD-11 Complex PTSD (World Health Organization, Citation2019) at the first session. The six items of the DSO scale are scored from 0 (‘not at all’) to 4 (‘extremely’) to indicate to what degree respondents typically suffer from problems of emotional dysregulation, relational difficulties, and negative self-worth. Diagnostic scoring criteria specified by the ITQ were used. Previous validation of the Norwegian translation of ITQ showed good psychometric properties (Sele et al., Citation2020). Cronbach’s alpha in the present study was .863.
1.4.5. Patient health questionnaire 9 (PHQ-9; Kroenke et al., Citation2001)
PHQ-9 was used to measure depression at each session. This brief self-report instrument consists of 9 items scored from 1 (‘not at all’) to 4 (‘nearly every day’) indicating the frequency of depressive symptoms. Cronbach’s alpha for PHQ-9 in the present study was .857.
1.4.6. General anxiety disorder 7 (GAD-7; Spitzer et al., Citation2006)
GAD-7 was used to assess symptoms of anxiety at each session. This widely used short-scale use 7 items, scored from 1 (‘not at all’) to 4 (‘nearly every day’), to measure the frequency of anxiety symptoms. Cronbach’s alpha was .872.
1.5. Statistical analyses
All analyses were conducted using SPSS version 27. Independent t-tests and chi-square tests were used to investigate group differences. Paired t-tests were conducted to assess within-group difference between pre- and post-treatment scores on outcome measures, and Cohen’s d effect sizes were calculated using the corrected standard deviation of the difference as a standardizer. Effect sizes were interpreted according to common benchmarks suggested by Cohen (Cohen, Citation1977). To assess clinically significant change in PCL scores we used a threshold of 10 points, and a total score of 33 was used as a cut-off between the clinical and non-clinical range (Weathers et al., Citation2013).
To investigate the impact of complex PTSD on treatment effects we used multilevel mixed-models. To find the best fitting model we tested different models using the Akaike Information Criteria for model fit. Random effects of intercept and time, as well as different covariance structures, were included. To accommodate the different intervals between observations, time was defined as weeks since the first observation for each data point. Fulfilment of DSO criteria was added as a dichotomous predictor, to investigate the interaction of time x DSO. In all analyses, alpha was set at .05.
2. Results
2.1. Therapist
104 clinicians recruited participants for the current dataset. The therapists were predominately female (78.7%) and had a mean age of 41 years (SD 9.8). The majority were clinical psychologists (63.5%), while psychiatrists (10.8%), psychiatric nurses (13.5%), and clinical social workers (5.4%) composed the other common professional backgrounds. They reported a mean of 11.5 years (SD 8.7) of professional experience.
All the clinicians had acceptable mean levels of fidelity to be included in the dataset.
2.2. Patients
Sample characteristics can be seen in . A total of 196 recruited patients had more than two observations with at least a month between and were therefore included in the total intent-to-treat (ITT) sample (see ). 114 of the patients (58.2%) had been offered EMDR and 82 (41.8%) had been offered CT-PSTD. The mean number of observations per patient was 8.9 (SD 5.1). The participants were predominantly female and had a mean age of 37 years. A large majority were incapacitated from working full time and were on some form of sick leave or received welfare benefits.
Table 1. Patient characteristics.
Regarding trauma history, the most commonly endorsed SLESQ-item was psychological abuse from a parent, partner, or immediate family (61.3%), followed by sexual abuse (58.6%). When combining items, 68.8% reported some form of sexual assault, including sexual harassment, and 90.3% reported at least one form of interpersonal violence. Respondents reported a mean of 5.6 (SD 2.87) different types of traumatic experiences.
A little less than half of the total sample (n = 89) had completed the end-of-treatment self-report package and were included in the ‘completer’ sample (see ). 56 of completers (62.9%) had received EMDR, and 33 (37.1%) CT-PTSD. The mean number of observations was 9.3 (SD 4.7). Significantly more (Χ2 = 4.282; p = .046) completers had college-level education (43.2%) compared to non-completers (29.4%). Non-completers were also more likely to report exposure to childhood physical abuse (Χ2 = 4.510, p = .038). We observed no significant differences between completers and non-completers on any background variables or baseline symptoms.
2.3. Treatment outcome
Self-reported symptom levels on outcome measures are reported in . Using the first and last observation, the total sample (N = 196) reported high levels of PTSD symptoms before treatment, but a significant and large decrease was observed in the last observation (t = 12.54, df 195, p <.001, d = 0.98). Similar significant decreases were also observed for symptoms of depression (t = 7.68, df = 195, p >.001, d = 0.55) and anxiety (t = 6.07, df = 195, p >.001, d = 0.46), although with smaller pre-post effect sizes.
Table 2. Mean, Standard deviation and effect sizes from first to last observation.
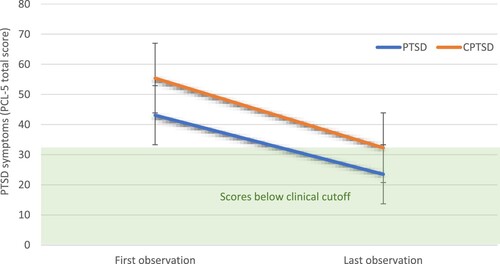
In the completer sample (n = 89) participants reported similar levels of symptoms before treatment, but larger decreases at the end of treatment. Pre-post effect sizes were large and significant for PTSD symptoms (t = 12.98, df = 88, p >.001, d = 1.52), symptoms of depression (t = 11.093, df = 88, p >.001, d = 0.89) and symptoms of anxiety (t = 8.557, df = 88, p >.001, d = 0.99). Of 89 completers, 66 (74.2%) reported a clinically significant improvement in PTSD symptoms of more than 10 points on the PCL, while only one patient reported a clinically significant deterioration. Of 82 patients with PCL scores above clinical cut-off (>33) before treatment, 49 (59.8%) transitioned to below cut-off after treatment. All but one of these also reported clinically significant improvement. Seven patients had pre-treatment PCL scores below the clinical cut-off, four of these also reported clinically significant improvements.
2.4. Complex PTSD
Almost seven out of ten participants fulfilled the criteria for Disturbances of Self-Organization (DSO) at the beginning of treatment according to ITQ scores, indicating CPTSD. These patients reported significantly more different types of trauma compared to patients without CPTSD (6.0 vs 5.0; t = −2.15 (182), p = .033). They were also more likely to report being exposed to interpersonal violence as adults (56.7% vs 37.3%; Χ2 = 6.068, p = .018) and psychological abuse outside of the family (62.2% vs 45.8%; Χ2 = 4.443, p = .040). No differences in demographic variables or treatment history were observed.
When applying mixed effect models with PCL scores as a dependent variable, the model with a fixed effect of intercept and time, and random effects of intercept and time provided the best model fit. Treatment condition (EMDR or CT-PTSD) was not a significant predictor and was therefore not included in the model.
In the ITT sample we observed a significant effect of time (−0.80, t = −5.973, p >.001) and DSO (9.62, t = 6.45, p > .001), but no significant interaction (0.079, t = 0.50, p = .621). These results indicate that although patients improved significantly over time, and patients with probable CPTSD had significantly higher PTSD symptoms at the start of treatment, the presence of probable CPTSD did not significantly interact with improvement. The same pattern, with a significant effect of time (−1.25, t = −6.286, p >.001) and DSO (8.2, t = 3.74, p > .001), but no significant interaction (0.16, t = 0.63, p = .532) emerged in the completer sample (see ).
Figure 2. Pre and post PCL-5 scores in ‘completers’ with and without CPTSD. Scores below the clincial cutoff (>33) are indicated with green shading.
When testing the same models with GAD-7 or PHQ-9 as dependent variables we observed similar results with no significant interactions, indicating that probable CPTSD did not influence outcomes in depression or anxiety.
3. Discussion
The main aim of the present study was to investigate the clinical outcomes of EBTs for PTSD, as delivered by therapists trained in a large-scale implementation effort in ordinary mental health care services. Our results show that delivery of these EBTs are associated with significant reductions in symptoms of PTSD and other types of distress in patients who complete the treatment, with within-person effect sizes comparable to those observed in research trials and other implementation studies (Eftekhari et al., Citation2013; Ehlers et al., Citation2013; Mavranezouli et al., Citation2020). Moreover, these results were achieved by therapists with standard training and supervision, predominantly treating patients with complex symptom presentations, comorbidity, and histories of multiple traumatic events.
Importantly we also show that the presence of complex symptoms as defined by the ICD-11 CPTSD diagnosis did not significantly affect treatment effects. Patients with probable CPTSD had higher PTSD symptoms both at the start and at the end of the treatment, indicating that longer treatment might be necessary to achieve positive end-states in this group, as recognized by the NICE guidelines (National Institute for Health and Care Excellence, Citation2018). However, the treatment was equally as effective in patients with probable CPTSD as in patients with PTSD in terms of the overall reduction in symptoms. Previous studies have similarly found that patients with CPTSD and PTSD had equal treatment-effect in intensive treatment (Voorendonk et al., Citation2020) and a clinical trial (Hoeboer et al., Citation2021), but to our knowledge, this is the first study to observe the same in ordinary clinical health care services.
Very few patients reported an increase in symptoms during treatment, indicating that the EBTs were safe and acceptable. However, the majority of recruited patients did not fill out the end of treatment measurements and might therefore not have completed the treatment. Unfortunately, we were prohibited from registering the number of sessions, termination of treatment, or reasons for termination. We therefore cannot distinguish between treatments where the patients dropped out or the therapist discontinued use of EBT, and treatments where patients or therapists stopped reporting data for other reasons. This makes it difficult to assess the safety and acceptability of the implemented treatment models. Although concerns have been raised about safety and risk of drop-out from trauma-focused treatments for PTSD, available research does not indicate that drop-out or adverse events are more common in such treatments when compared to other treatments (Imel et al., Citation2013; van den Berg et al., Citation2016). This should be further examined in future studies in ordinary clinical settings.
We observed that patients with lower education and a history of childhood physical abuse were less likely to complete the treatment. Lower education has been associated with drop-out from psychotherapy in other studies as well (Bennemann et al., Citation2022). Therapists might need to employ a more tailored approach to patients with lower education or a history of physical abuse to ensure their engagement in the treatment.
The results of this investigation should be interpreted in light of several limitations. Our sample consists of patients who have been diagnosed with PTSD, but no formal diagnostic procedure to diagnose PTSD or CPTSD was required. ICD-11 CPTSD status was determined only based on ITQ-DSO items, but PTSD was assessed with PCL-5 based on DSM-5. Some patients in our study may therefore not fulfil ICD-11 criteria for PTSD that are somewhat narrower than DSM-5 criteria. Also, no diagnostic interview was conducted at the end of treatment, so estimation of treatment effects is based on self-reported symptoms only. Furthermore, we did not have the opportunity to assess the participants after treatment and therefore cannot conclude if the treatment gains were maintained. And since the study did not include a control group, treatment effects cannot be disaggregated from time effects or be contrasted to other treatments.
Despite these limitations, this study supports the effectiveness of the EBTs for PTSD in routine care. The use of these treatment models in routine clinical service is associated with good treatment outcomes, also for patients with probable CPTSD. Since the data for this study was based on training cases, outcomes from and usage of the treatments might also improve further as therapists gain more experience and competence with their use. This supports the continued efforts to implement EBTs for PTSD at scale to ensure the availability of effective treatments for persons affected by trauma. Several studies have shown however, that EBPs for PTSD can be challenging to sustain after initial dissemination in clinics (Egeland et al., Citation2019; Rosen et al., Citation2016), and that continued support and supervision of therapists is necessary (Rakovshik & McManus, Citation2010). In the current study, a system-wide implementation strategy is employed using an evidence-based leadership-programme (Egeland et al., Citation2019; Skar et al., Citation2022) and further studies will investigate the long-term effectiveness of this strategy.
Author contribution statement
HB was involved in conceiving, designing and conducting the study, collecting data, performing data-analysis and writing the paper. ME was involved in conducting the study, collecting and analyzing data and writing the paper. NP and AB was involved in conduction the study, collecting data and wiriting the paper. KE was involved in conduction and leading the study, collecting data, and writing the paper.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to ethical approval and confidentiality agreements made with participants, but are available from the corresponding author on reasonable request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bækkelund, H., Karlsrud, I., Hoffart, A., & Arnevik, E. A. (2021). Stabilizing group treatment for childhood-abuse related PTSD: A randomized controlled trial. European Journal of Psychotraumatology, 12(1), 1859079. https://doi.org/10.1080/20008198.2020.1859079
- Bennemann, B., Schwartz, B., Giesemann, J., & Lutz, W. (2022). Predicting patients who will drop out of out-patient psychotherapy using machine learning algorithms. The British Journal of Psychiatry, 220(4), 192–201. https://doi.org/10.1192/bjp.2022.17
- Bisson, J. I., Berliner, L., Cloitre, M., Forbes, D., Jensen, T. K., Lewis, C., Monson, C. M., Olff, M., Pilling, S., Riggs, D. S., Roberts, N. P., & Shapiro, F. (2019). The international society for traumatic stress studies New guidelines for the prevention and treatment of posttraumatic stress disorder: Methodology and development process. Journal of Traumatic Stress, 32(4), 475–483. https://doi.org/10.1002/jts.22421
- Blackburn, I.-M., James, I. A., Milne, D. L., Baker, C., Standart, S., Garland, A., & Reichelt, F. K. (2001). The revised cognitive therapy scale (CTS-R): psychometric properties. Behavioural and Cognitive Psychotherapy, 29(4), 431–446. https://doi.org/10.1017/S1352465801004040
- Clark, D. M. (2018). Realizing the mass public benefit of evidence-based psychological therapies: The IAPT program. Annual Review of Clinical Psychology, 14(1), 159–183. https://doi.org/10.1146/annurev-clinpsy-050817-084833
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., Karatzias, T., & Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. https://doi.org/10.1111/acps.12956
- Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L., Gan, W., & Petkova, E. (2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry, 167(8), 915–924. https://doi.org/10.1176/appi.ajp.2010.09081247
- Cohen, J. (1977). Statistical power analysis for the behavioral sciences. Elsevier, https://doi.org/10.1016/C2013-0-10517-X
- Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., Feltner, C., Brownley, K. A., Olmsted, K. R., Greenblatt, A., Weil, A., & Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. https://doi.org/10.1016/j.cpr.2015.10.003
- de Bont, P. A., van den Berg, D. P., van der Vleugel, B. M., de Roos, C., Mulder, C. L., Becker, E. S., de Jongh, A., van der Gaag, M., & van Minnen, A. (2013). A multi-site single blind clinical study to compare the effects of prolonged exposure, eye movement desensitization and reprocessing and waiting list on patients with a current diagnosis of psychosis and co morbid post traumatic stress disorder: Study protocol for the randomized controlled trial treating trauma in psychosis. Trials, 14(1), 151. https://doi.org/10.1186/1745-6215-14-151
- Eftekhari, A., Ruzek, J. I., Crowley, J. J., Rosen, C. S., Greenbaum, M. A., & Karlin, B. E. (2013). Effectiveness of national implementation of prolonged exposure therapy in veterans affairs care. JAMA Psychiatry, 70(9), 949. https://doi.org/10.1001/jamapsychiatry.2013.36
- Egeland, K. M., Skar, A.-M. S., Endsjø, M., Laukvik, E. H., Bækkelund, H., Babaii, A., Granly, L. B., Husebø, G. K., Borge, R. H., Ehrhart, M. G., Sklar, M., Brown, C. H., & Aarons, G. A. (2019). Testing the leadership and organizational change for implementation (LOCI) intervention in Norwegian mental health clinics: A stepped-wedge cluster randomized design study protocol. Implementation Science, 14(1), 28. https://doi.org/10.1186/s13012-019-0873-7
- Ehlers, A. (2020). Cognitive therapy. In D. Forbes, J. I. Bisson, C. M. Monson, & L. Berliner (Eds.), Effective Treatments for PTSD 3rd ed. (pp. 255–271). Guilford Publications.
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. https://doi.org/10.1016/S0005-7967(99)00123-0
- Ehlers, A., Grey, N., Wild, J., Stott, R., Liness, S., Deale, A., Handley, R., Albert, I., Cullen, D., Hackmann, A., Manley, J., McManus, F., Brady, F., Salkovskis, P., & Clark, D. M. (2013). Implementation of cognitive therapy for PTSD in routine clinical care: Effectiveness and moderators of outcome in a consecutive sample. Behaviour Research and Therapy, 51(11), 742–752. https://doi.org/10.1016/j.brat.2013.08.006
- Ehlers, A., & Wild, J. (2015). Cognitive therapy for PTSD: Updating memories and meanings of trauma. In U. Schnyder, & M. Cloitre (Eds.), Evidence Based Treatments for Trauma-Related Psychological Disorders (pp. 161–187). Springer.
- Goodman, L. A., Corcoran, C., Turner, K., Yuan, N., & Green, B. L. (1998). Assessing traumatic event exposure: General issues and preliminary findings for the stressful life events screening questionnaire. Journal of Traumatic Stress, 11(3), 521–542. https://doi.org/10.1023/A:1024456713321
- Hem, C., Hussain, A., Wentzel-Larsen, T., & Heir, T. (2012). The Norwegian version of the PTSD checklist (PCL): construct validity in a community sample of 2004 tsunami survivors. Nordic Journal of Psychiatry, 66(5), 355–359. https://doi.org/10.3109/08039488.2012.655308
- Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391. https://doi.org/10.1002/jts.2490050305
- Hoeboer, C. M., de Kleine, R. A., Oprel, D. A. C., Schoorl, M., van der Does, W., & van Minnen, A. (2021). Does complex PTSD predict or moderate treatment outcomes of three variants of exposure therapy? Journal of Anxiety Disorders, 80), https://doi.org/10.1016/j.janxdis.2021.102388
- Imel, Z. E., Laska, K., Jakupcak, M., & Simpson, T. L. (2013). Meta-Analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, https://doi.org/10.1037/a0031474
- Karatzias, T., & Cloitre, M. (2019). Treating adults With complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. https://doi.org/10.1002/jts.22457
- Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 617–627. https://doi.org/10.1001/archpsyc.62.6.617
- Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J., Stein, D. J., Karam, E. G., Ruscio, A. M., Benjet, C., Scott, K., & Atwoli, L. (2017). Posttraumatic stress disorder in the world mental health surveys. Psychological Medicine, 47(13), 2260–2274. https://doi.org/10.1017/S0033291717000708
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- Lassemo, E., Sandanger, I., Nygård, J. F., & Sørgaard, K. W. (2017). The epidemiology of post-traumatic stress disorder in Norway: Trauma characteristics and pre-existing psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 52(1), 11–19. https://doi.org/10.1007/s00127-016-1295-3
- Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1729633. https://doi.org/10.1080/20008198.2020.1729633
- Maguen, S., Madden, E., Patterson, O. V., DuVall, S. L., Goldstein, L. A., Burkman, K., & Shiner, B. (2018). Measuring Use of evidence based psychotherapy for posttraumatic stress disorder in a large national healthcare system. Administration and Policy in Mental Health and Mental Health Services Research, 45(4), 519–529. https://doi.org/10.1007/s10488-018-0850-5
- Mavranezouli, I., Megnin-Viggars, O., Grey, N., Bhutani, G., Leach, J., Daly, C., Dias, S., Welton, N. J., Katona, C., El-Leithy, S., Greenberg, N., Stockton, S., & Pilling, S. (2020). Cost-effectiveness of psychological treatments for post-traumatic stress disorder in adults. Plos One, 15(4), e0232245. https://doi.org/10.1371/journal.pone.0232245
- McHugh, R. K., & Barlow, D. H. (2010). The dissemination and implementation of evidence-based psychological treatments: A review of current efforts. American Psychologist, 65(2), 73–84. https://doi.org/10.1037/a0018121
- Murray, H. (2017). Evaluation of a trauma-focused CBT training programme for IAPT services. Behavioural and Cognitive Psychotherapy, 1–16. https://doi.org/10.1017/S1352465816000606
- National Institute for Health and Care Excellence. (2018). Post-traumatic stress disorder. NICE. https://www.nice.org.uk/guidance/ng116/resources/posttraumatic-stress-disorder-pdf-66141601777861.
- Rakovshik, S. G., & McManus, F. (2010). Establishing evidence-based training in cognitive behavioral therapy: A review of current empirical findings and theoretical guidance. Clinical Psychology Review, 30(5), 496–516. https://doi.org/10.1016/j.cpr.2010.03.004
- Riggs, D. S., Willing, M. M. P., Mallonee, S., Rosen, C., Stirman, S. W., & Dorsey, S. (2020). Training and implementation of evidence–based psychotherapies for PTSD. In Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies, 3rd ed (pp. 469–491. The Guilford Press.
- Rosen, C. S., Matthieu, M. M., Wiltsey Stirman, S., Cook, J. M., Landes, S., Bernardy, N. C., Chard, K. M., Crowley, J., Eftekhari, A., Finley, E. P., & Hamblen, J. L. (2016). A review of studies on the system-wide implementation of evidence-based psychotherapies for posttraumatic stress disorder in the veterans health administration. Administration and Policy in Mental Health and Mental Health Services Research, 43(6), 957–977. https://doi.org/10.1007/s10488-016-0755-0
- Sele, P., Hoffart, A., Bækkelund, H., & Øktedalen, T. (2020). Psychometric properties of the international trauma questionnaire (ITQ) examined in a Norwegian trauma-exposed clinical sample. European Journal of Psychotraumatology, 11(1), 1796187. https://doi.org/10.1080/20008198.2020.1796187
- Shapiro, F. (2001). Eye Movement Desensitization and Reprocessing. Guildford Press.
- Shapiro, F., & Laliotis, D. (2015). EMDR therapy for trauma-related disorders. In U. Schnyder, & M. Cloitre (Eds.), Evidence Based Treatments for Trauma-Related Psychological Disorders (pp. 205–228). Springer.
- Shapiro, F., Russel, M. C., Lee, C., & Schubert, S. J. (2020). Eye movement desensitization and reprocessing therapy. In D. Forbes, J. I. Bisson, C. M. Monson, & L. Berliner (Eds.), Effective Treatments for PTSD Third edition (pp. 234–254). Guildford Press.
- Skar, A.-M. S., Braathu, N., Peters, N., Bækkelund, H., Endsjø, M., Babaii, A., Borge, R. H., Wentzel-Larsen, T., Ehrhart, M. G., Sklar, M., Brown, C. H., Aarons, G. A., & Egeland, K. M. (2022). A stepped-wedge randomized trial investigating the effect of the leadership and organizational change for implementation (LOCI) intervention on implementation and transformational leadership, and implementation climate. BMC Health Services Research, 22(1), 298. https://doi.org/10.1186/s12913-022-07539-9
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- van den Berg, D. P. G., de Bont, P. A. J. M., van der Vleugel, B. M., de Roos, C., de Jongh, A., van Minnen, A., & van der Gaag, M. (2016). Trauma-Focused treatment in PTSD patients With psychosis: Symptom exacerbation, adverse events, and revictimization. Schizophrenia Bulletin, 42(3), 693–702. https://doi.org/10.1093/schbul/sbv172
- Voorendonk, E. M., De Jongh, A., Rozendaal, L., & Van Minnen, A. (2020). Trauma-focused treatment outcome for complex PTSD patients: Results of an intensive treatment programme. European Journal of Psychotraumatology, 11(1), 1783955. https://doi.org/10.1080/20008198.2020.1783955
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. www.ptsd.va.gov.
- World Health Organization. (2019). International Classification of Diseases, Eleventh Revision (ICD-11). World Health Organization. https://icd.who.int/browse11.