ABSTRACT
Background: Longitudinal studies examining mental health trajectories in refugees and asylum seekers are scarce.
Objectives: To investigate trajectories of psychological symptoms and wellbeing in refugees and asylum seekers, and identify factors associated with these trajectories.
Method: 912 asylum seekers and refugees from the control arm of three trials in Europe (n = 229), Turkey (n = 320), and Uganda (n = 363) were included. We described trajectories of psychological symptoms and wellbeing, and used trauma exposure, age, marital status, education, and individual trial as predictors. Then, we assessed the bidirectional interactions between wellbeing and psychological symptoms, and the effect of each predictor on each outcome controlling for baseline values.
Results: Symptom improvement was identified in all trials, and for wellbeing in 64.7% of participants in Europe and Turkey, versus 31.5% in Uganda. In Europe and Turkey domestic violence predicted increased symptoms at post-intervention (ß = 1.36, 95% CI 0.17–2.56), whilst murder of family members at 6-month follow-up (ß = 1.23, 95% CI 0.27–2.19). Lower wellbeing was predicted by murder of family member (ß = −1.69, 95% CI −3.06 to −0.32), having been kidnapped (ß = −1.67, 95% CI −3.19 to −0.15), close to death (ß = −1.38, 95% CI −2.70 to −0.06), and being in the host country ≥2 years (ß = −1.60, 95% CI −3.05 to −0.14). In Uganda at post-intervention, having been kidnapped predicted increased symptoms (ß = 2.11, 95% CI 0.58–3.65), and lack of shelter (ß = −2.51, 95% CI −4.44 to −0.58) and domestic violence predicted lower wellbeing (ß = −1.36, 95% CI −2.67 to −0.05).
Conclusion: Many participants adapt to adversity, but contextual factors play a critical role in determining mental health trajectories.
HIGHLIGHTS
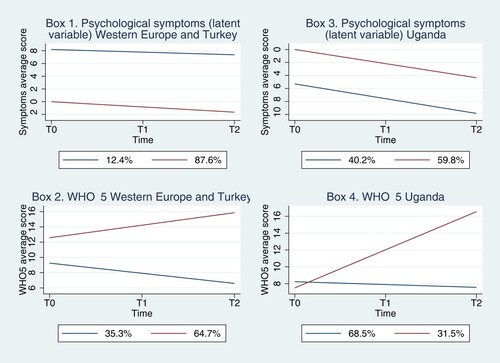
Psychological symptoms improved in all participants and the trajectories went in similar directions. For wellbeing, the majority of participants in Western Europe and Turkey improved over time, while this proportion was smaller in Uganda.
Asylum seekers and refugees have the capacity to adapt to traumatic events and ongoing adversity, but contextual factors play a critical role in determining mental health trajectories.
Future interventions should focus on reinforcing wellbeing and ‘positive’ psychological outcomes, and targeting the social determinants of mental health.
Antecedentes: Estudios longitudinales que examinan las trayectorias de la salud mental en los refugiados y solicitantes de asilo son escasos.
Objetivos: Investigar las trayectorias de los síntomas psicológicos y el bienestar en refugiados y solicitantes de asilo, e identificar factores asociados a estas trayectorias.
Métodos: Se incluyeron 912 solicitantes de asilos y refugiados del brazo control de tres ensayos clínicos en Europa (n = 229), Turquía (n = 320) y Uganda (n = 363). Describimos las trayectorias psicológicas de los síntomas y el bienestar, y utilizamos la exposición traumática, la edad, el estado marital, la educación y el juicio individual como predictores. Después, evaluamos las interacciones bidireccionales entre el bienestar y los síntomas psicológicos, y el efecto de cada uno de los predictores en cada resultado controlando por los valores iniciales.
Resultados: Se identificó una mejoría en los síntomas en todos los ensayos, y del bienestar en el 64.7% de los participantes en Europa y Turquía, versus el 31.5% en Uganda. En Europa y en Turquía, la violencia doméstica predijo el incremento de síntomas de después de la intervención (ß = 1.36, 95% CI 0.17 a 2.56), mientras que el homicidio de algún miembro familiar a los 6 meses de seguimiento (ß = 1.23, 95% CI 0.27 a 2.19). Un menor bienestar fue predicho por el homicidio de algún miembro de la familia (ß = −1.69, 95% CI −3.06 a −0.32), haber sido secuestrado (ß = −1.67, 95% CI −3.19 a −0.15), haber estado próximo a la muerte (ß = −1.38, 95% CI −2.70 a −0.06), y estar en el país de acogida ≥2 años (ß = −1.60, 95% CI −3.05 a −0.14). En Uganda, después de la intervención, haber sido secuestrado predijo un aumento de los síntomas (ß =2.11, 95% CI 0.58 a 3.65), y la falta de refugio (ß = −2.51, 95% CI −4.44 a −0.58) y la violencia doméstica predijo un menor bienestar (ß = −1.36, 95% CI −2.67 a −0.05).
Conclusión: Muchos participantes se adaptan a la adversidad, pero los factores contextuales juegan un papel crítico en determinar las trayectorias de la salud mental.
背景:研究难民和寻求庇护者心理健康轨迹的纵向研究很少。
目的:考查难民和寻求庇护者心理症状和幸福感的轨迹,并确定这些轨迹的相关因素。
方法:包括来自欧洲(n = 229)、土耳其(n = 320)和乌干达(n = 363)三个试验控制组的 912 名寻求庇护者和难民。我们描述了心理症状和幸福感的轨迹,并使用创伤暴露、年龄、婚姻状况、教育和个人试验作为预测因素。然后,我们评估了幸福感和心理症状之间的双向交互作用,以及每个预测变量对控制基线值后每个结果的影响。
结果:在所有试验中都发现症状有所改善,欧洲和土耳其有 64.7% 参与者的健康状况得到改善,而乌干达有 31.5%。在欧洲和土耳其,家庭暴力预测干预后症状会增加(ß = 1.36,95% CI 0.17 至 2.56),和在 6 个月的随访中家庭成员被谋杀(ß = 1.23,95% CI 0.27 至 2.19)。家庭成员被谋杀 (ß = −1.69, 95% CI −3.06 to −0.32)、被绑架 (ß = −1.67, 95% CI −3.19 to −0.15)、濒临死亡 (ß = −1.38,95% CI −2.70 到 –0.06),和在东道国 ≥2 年(ß = −1.60,95% CI −3.05 到 −0.14)预测了更低的幸福感。乌干达组干预后,被绑架预测了更高的症状(ß = 2.11,95% CI 0.58 至 3.65),缺乏庇护所(ß = −2.51,95% CI −4.44 至 −0.58)和家庭暴力预测了更低的幸福感(ß = −1.36, 95% CI −2.67 至 −0.05)。
结论:许多参与者适应逆境,但背景因素在确定心理健康轨迹方面起着关键作用
1. Introduction
Refugees and asylum seekers are exposed to multiple potentially traumatic events (PTEs) before migration, during displacement and transition to a new country, and after resettlement. Experience of PTEs may generate a wide range of consequences: from psychopathology, as repeatedly found by research linking PTE exposure with increased levels of posttraumatic stress disorder (PTSD) and depression (Charlson et al., Citation2019; Sijbrandij, Citation2018; Steel et al., Citation2009), to resilience and posttraumatic growth (Giacco et al., Citation2018). In addition, research has focused on the mental health impact of ongoing, chronic stressors in conflict-affected populations, such as poverty and gender-based violence in refugee camps, as well as post-migration living difficulties, including socioeconomic, language acquisition, discrimination (Hajak et al., Citation2021), and legal challenges after migration to new countries (Hynie, Citation2018; Silove et al., Citation2020). Research conducted with individuals exposed to PTEs and chronic, ongoing stressors has shown a higher prevalence of common mental disorders, such as PTSD, depressive, and anxiety disorders (Turrini et al., Citation2017; Turrini et al., Citation2019; Van Ginneken et al., Citation2021). However, a proportion of individuals do not develop mental health disorders, though their psychological wellbeing may still be affected (Giacco et al., Citation2018; Giacco & Priebe, Citation2018; Priebe et al., Citation2016; Van der Boor et al., Citation2020).
Only few studies have investigated temporal changes in mental health symptoms in cohorts of forcibly displaced population groups (Bryant et al., Citation2018; Lenferink et al., Citation2022; Strømme et al., Citation2020; Tomasi et al., Citation2022; Wu et al., Citation2021). While some studies identified persisting or increased levels of mental health problems over the first one to two years after resettlement in a new country (LeMaster et al., Citation2018; Lie, Citation2002; Roth & Ekblad, Citation2006), others found a decrease in mental ill health at one year (Cooper et al., Citation2019; Mollica et al., Citation2007; Müller et al., Citation2019).
One way to provide robust information on prototypical trajectories of psychosocial outcomes among refugees and asylum seekers exposed to PTEs is to use integrative data analysis techniques, which can combine participant information from individual data sets into one large data set, and to statistically harmonise data so that they can be analyzed jointly. Integrative data analysis allows researchers to apply consistent analyses (e.g. latent class growth analysis) to obtain robust estimates of symptom trajectories, and to calculate the proportion of individuals within each trajectory type (Curran & Hussong, Citation2009).
In this study, we applied integrative data analysis and growth mixture models to individual-participant data from the control groups of three large randomised controlled trials (RCTs) conducted with a similar study design and involving refugees and asylum seekers. Our objective was to evaluate the trajectories of psychological outcomes and wellbeing, and to identify factors associated with these trajectories. We had a twofold hypothesis: first, that included participants can be grouped across different types of symptom and wellbeing trajectories over time, including spontaneous improvement; second, that exposure to multiple PTEs is associated with higher levels of psychological symptoms and decreased wellbeing, and that specific types of PTEs were associated with different symptom and wellbeing trajectories.
2. Methods
2.1. Participants and measures
An individual participant dataset with repeated observations on a sample of 912 adult (> 18 years) refugees and asylum seekers followed for six months was used. The dataset pooled the care-as-usual arm (i.e. not receiving any psychological interventions but routinely delivered support and/or care according to local regulations) data from three RCTs with a similar design involving asylum seekers and refugees resettled in Western European countries (Italy, Germany, Austria, Finland, England and Scotland), Turkey, and Uganda (Acarturk et al., Citation2022; Purgato et al., Citation2021; Tol et al., Citation2020). In Western Europe and Turkey participants were included if they had increased psychological distress (General Health Questionnaire ≥ 3 (Goldberg, Citation1992)), in the absence of any diagnosed mental disorders according to the MINI Neuropsychiatric interview (Sheehan et al., Citation1998). In Uganda participants were screened for at least moderate level of psychological distress (cutoff ≥5 on the Kessler 6 (Kessler et al., Citation2010)). The protocol of the present study was registered within the Open Science Framework (https://osf.io/8atsq).
Exposure to PTEs was measured at baseline using the Harvard Trauma Questionnaire (HTQ)-part I (Mollica et al., Citation1992), considered both in terms of global scale score and in terms of individual items. The HTQ-part I enquires about a variety of trauma events that may affect refugee mental health. The scoring represents the amount of lifetime traumatic events experienced by the participants (higher score is associated with high number of traumatic events). Outcome measures were self-administered tools, adopted in the RCTs to measure psychological symptoms and wellbeing. PTSD was assessed with the PTSD Checklist for DSM-5 (PCL-5) (Weathers et al., Citation2013), a 20-item questionnaire that measures PTSD symptom severity (score zero to 80) and symptom severity by cluster (intrusions, avoidance, negative changes in thoughts and mood, and changes in arousal) and with PCL-6 (Blanchard et al., Citation1996), a 6-item version of the instrument using a 5-point scale. Depression was measured with the Patient Health Questionnaire, 9-item version (PHQ-9) (Kroenke et al., Citation2001) which has a 4-point scale (score 0–27). Functional impairment was assessed with the WHO Disability Assessment Schedule 2.0 (WHODAS) (World Health Organization, Citation2010). Wellbeing was assessed with the WHO-5 Wellbeing Index (WHO-5) (Topp et al., Citation2015) that contains five questions using a 6-point scale (score 0–25). Scores at WHODAS, PHQ9 and PCL-5 and −6 were used to develop a latent variable representing psychological symptoms, while for wellbeing we used the WHO-5 scores. Psychological symptoms and wellbeing were measured at baseline (T0), post-intervention (T1), and 6-month follow-up (T2).
2.2. Statistical analysis
We followed the GRoLTS-Checklist for reporting latent growth analyses (Van de Schoot et al., Citation2017). Pathway models of trajectories of psychological symptoms and wellbeing measures were developed taking into consideration observed and unobserved confounders, through inclusion of individual-level variables and of models allowing for residual variances of the growth factors. The average value of the slope for each class for the chosen models was estimated, together with its standard error, confidence interval, and p-value of the test for null slope. Through the pathway models we described the relationships between the HTQ-part I score, age, marital status, educational level, individual trial, and psychological outcomes or subjective wellbeing over time.
We assessed for each follow-up: (1) the dependence of psychological symptoms and wellbeing on their own lagged values (i.e. past value to predict future one), and on the lagged value of the other outcome (wellbeing for symptoms and vice-versa); (2) the relationship between individual PTE exposure level, age, marital status, educational level, work status, length of stay in the host country, and psychological symptoms or wellbeing. Outcome measures were a latent variable representing psychological symptoms (identified through fixing factor loading of the PCL-5 score to 1 and a multiple-indicator growth model, with the mean of the intercept growth factor fixed at zero in the last class and free to be estimated in the other classes) and WHO-5. We followed Jung and Wickrama (Citation2008) in analyzing pathway models without covariates first, by performing Generalised Mixture Models (GMMs) and Latent Growth Class Analysis (LCGA, a special case of GMM, assuming a null variance for intercept and slope) with one, two and three classes for the WHO-5 score, and Multiple-Indicator GMMs (MIGMMs) and LCGA (MILCGA) for the latent symptom construct. The candidate models were examined based on the criteria described in Jung and Wickrama (Citation2008) and in Ram and Grimm (Citation2009). In particular, among models without covariates, we excluded single-class models in case they showed a worse fit (i.e. higher values) than their related two- and three-class models in at least one of the information criteria: Bayesian Information Criteria (BIC), Akaike Information Criteria (AIC), and Adjusted BIC. As for two- and three-class models, we considered as criteria for model inadmissibility: (1) non-significance in all the likelihood-ratio tests (LRTs) against the corresponding model with one class less: Vuong-Lo-Mendell-Rubin LRT (VLMR-LRT), Adjusted Lo-Mendell-Rubin LRT (ALRT) (Lo et al., Citation2001; Vuong, Citation1989) and Bootstrap LRT (BLRT) (McLachlan & Peel, Citation2000); (2) estimated probability for the least represented class below 0.1; (3) a lowest estimated average latent class posterior probability of accurate prediction below 0.8. As a further fit index, we also reported entropy: higher values correspond to a better model fit, but no cut-off criteria are set (Jung & Wickrama, Citation2008).
Admissible models were then reconsidered conditionally on covariates HTQ-part I scores, age in years, educational level (as divided into: no schooling/primary education/secondary education), trial ID (Western Europe, Turkey, Uganda) and dummy variables, respectively, for whether the person was married, unemployed, and in the hosting country for more than two years. To avoid convergence issues and in line with focusing on changes from baseline, covariates were used as predictors of both latent class membership (in logistic regressions in the case of 2 classes and in multi-logistic regressions in case of 3 classes) and of slope (in latent variable regressions), but not of intercepts. In case of admissibility of multiple models, the same criteria were adopted to select the best one.
Conditional models allowing for residual intercept and slope variance were defined as ‘random-effect’, while those with no residual intercept and slope variance as ‘fixed-effect’ models (Wardenaar, Citation2020); thus, the competing models were named Fixed-Effect Generalised Mixture Models (FEGMMs) and Random-Effect Generalised Mixture Models (REGMMs) for the WHO-5 score, and Multiple-Indicator FEGMMs (MIFEGMMs) and Multiple-Indicator REGMMs (MIREGMMs) for the latent symptom construct.
In all cases, linear growth was assumed. In the case of random-effect analyses, equal variances of both the intercept and the slope across classes were assumed, to avoid convergence issues (Jung & Wickrama, Citation2008). Such models were discarded as misspecified in case of a negative and statistically significant residual variance of either the intercept or the slope (using the one-sided test, following Kolenikov and Bollen (Citation2012)). On the contrary, a negative but not statistically significant residual variance of one of these two parameters was interpreted as lack of remaining individual variation (Soloski & Durtschi, Citation2020), so its variance was fixed to 0 (in case they both were negative, the model was discarded as dropping both variance parameters reduced it to the fixed-effect one).
Then, we assessed the reciprocal effect of WHO-5 and psychological symptoms in a cross-lagged model, where each outcome was predicted by its lagged value and by the lagged value of the other outcome, controlling for covariates. Finally, we evaluated the effect of each predictor on each outcome in a model controlling for the baseline value of each outcome. In these models, we used each HTQ-part I item as predictor, and allowed psychological symptoms and WHO-5 values not included in the same regression to correlate. In case of lack of convergence, factor loadings of the latent variable indicators were fixed to their values in the model without covariates. For all clinical scales, in case of missing items, the Corrected Item Mean Substitution method (Huisman, Citation1999) was used (i.e. the item mean across participants weighted by the subject’s mean of completed items), using information from all other individuals. In all models, in order to avoid listwise deletion of observations with missing values, the Full Information Maximum Likelihood approach was adopted. Moreover, to prevent results to depend from the chosen reference category, statistical significance of education was assessed through a global Wald test. Statistical analyses were conducted using the software Mplus (Muthén & Muthén, Citation2017) and Stata (StataCorp, Citation2021).
3. Results
3.1. Trajectories of psychological symptoms and wellbeing over time
A total of 912 refugees and asylum seekers from three RCTs (Western Europe n = 229, Turkey n = 320, and Uganda n = 363) were included in the analysis. Descriptive statistics of clinical and sociodemographic variables are reported in . Due to substantial differences between the populations included in the trial conducted in Uganda and the other two trials in terms of clinical and socio-demographic variables, the Uganda dataset was analyzed separately. A two-class model emerged in all trajectories in both the datasets; in particular, fixed-effect models were selected in all cases, apart for the analysis of wellbeing in Uganda, where a random-effect model was chosen, but with a null slope residual variance. Thus, results of the two-class FEMIGMM analysis are described below for psychological symptoms, while for wellbeing two different two-class models were adopted: FEGMM in the case of Western Europe and Turkey and REGMM with no slope residual variance for Uganda (results of the model-selection procedure are described in the supplemental material).
Table 1. Socio-demographic and clinical characteristics at baseline.
In the case of psychological symptoms, both trajectory analyses found that the two identified latent classes already showed a relevant difference at T0, that was kept at subsequent timepoints. The majority of participants in Western Europe and Turkey, and in Uganda significantly improved over time (p < .001) (, boxes 1 and 3).
Trajectory analysis for wellbeing showed different patterns in the two classes in the sample from Western Europe and Turkey, one identifying a class with increasing and one with decreasing wellbeing over time, with the class with a significant increasing trend already showing better values at baseline (, box 2). In Uganda the trajectories of the two classes of participants showed a pattern similar to Western Europe and Turkey, with one trajectory significantly increasing (p< .001) and one decreasing (p = .165), with the class with increasing trend showing slightly worse values at T0 but markedly better values at T1 and T2 (, box 4).
3.2. Factors associated with psychological symptoms
For the outcome ‘psychological symptoms’ a lower HTQ-part I score was associated with increased probability of belonging to the class with less symptoms in Western Europe. The Turkish trial showed a contrasting effect in the sense that a lower HTQ-part I score was associated with a lower probability of being in the class with more symptoms but at the same time with an increase of symptoms over time. We identified an association between secondary-level education and likelihood to be in the class with higher level of symptoms, but with symptoms decreasing over time for participants with a higher level of education (). In Uganda, HTQ-part I score was associated with a higher probability to belong to the class with a higher level of symptoms ().
Table 2. Psychological symptoms. Logistic regression to predict class membership and linear regression to predict slope.
Results of the cross-lagged models are reported in the supplemental material (Table 6). In short, results highlighted evidence of persistence (i.e. a significant effect of each outcome on its delayed value) and a negative effect of lagged values of the symptoms construct on WHO-5 for Western Europe and Turkey, but not for Uganda. No significant effect was found for cross-lagged effects of WHO-5 scores on symptoms construct for Western Europe and Turkey, and Uganda controlling for covariates.
3.3. Factors associated with wellbeing
In Western Europe and Turkey, length of stay in the host country was associated with increased probability of belonging to the class with lower wellbeing, but was associated with an improvement over time. On the contrary, a higher HTQ-part I score (i.e. more traumatic events) and a low educational level (i.e. having no schooling) were significantly associated to a worsening of wellbeing over time (). In Uganda, age and having a primary-level education versus no schooling were significantly associated with wellbeing. Older age was associated with increased probability of belonging to the class improving over time, but, within each class, to a worsening of wellbeing, while the opposite occurred for primary-level education (although education did not reach global statistical significance in the model to predict class membership) ().
Table 3. WHO-5. Logistic regression to predict class membership and linear regression to predict slope.
Table 4. Predictors of WHO-5 and psychological symptoms (latent variable) at T1 and T2.
3.4. Traumatic events and other predictors of psychological symptoms and wellbeing over time
The frequency of each individual traumatic experience assessed with the HTQ-part I is reported in the supplemental material (Box 1). We assessed the effect of individual items of HTQ-part I and sociodemographic predictors on psychological symptoms and wellbeing at T1 and T2 in a model controlling for the outcome values at T0.
In Western Europe and Turkey, having experienced domestic violence was a significant predictor of increased level of symptoms at T1, while having experienced the murder of family members or friends was a predictor of increased symptoms at T2. The latter also emerged as a predictor of lower wellbeing, together with having been kidnapped, having been close to death, and being in the host country for more than two years. Being part of the Turkish trial was identified as a predictor of lower wellbeing at T2. No significant predictors of the level of wellbeing at baseline were found ().
In Uganda, having been kidnapped was associated with a higher level of psychological symptoms at T1, while older age was associated with a lower level of wellbeing both at T1 and T2. A lower level of wellbeing was also predicted by having experienced lack of shelter and by having undergone domestic violence. No significant conditional association with symptoms at T2 was found.
4. Discussion
The present study described the trajectories of psychological symptoms and wellbeing in a large sample of refugees and asylum seekers over a period of six months, and analyzed the impact of traumatic events on mental health, measured as psychological symptoms and wellbeing. We found that psychological symptoms significantly improved over time, and this improvement was observed in all three samples. Despite the clinical differences between the two samples, characterised by more serious symptomatology at baseline with stronger improvement at follow-up in Uganda, the trajectories followed similar pathways. This result is in line with, and significantly expands, the findings of prior systematic reviews and meta-analyses on prevalence rates of mental disorders in refugees that also found that the majority of participants did not report clinically relevant psychopathology levels after resettlement in the host country (Fazel et al., Citation2005; Henkelmann et al., Citation2020; Steel et al., Citation2009). Consistently, a recent longitudinal study on 613 Syrian and Iraqi refugees resettled in Australia identified a ‘no symptoms’ trajectory that was maintained over a period of six months, highlighting the capacity of this population group to adapt to multiple traumatic experiences and ongoing adversity (Lenferink et al., Citation2022).
Our finding on wellbeing, with one trajectory showing improvement over time observed in both samples, and one indicating only slightly decreasing wellbeing, supports our interpretation that refugees have the capacity to adapt positively to new contexts, and to maintain relatively stable levels of wellbeing despite the prolonged exposure to traumatic experiences. The higher proportion of participants improving in wellbeing in the European and Turkey sample might be related to the higher economic resources available and the higher opportunities to access to healthcare interventions. In this perspective, countries in which there are opportunities for receiving health and social services, employment, or other ways of smoothing traumatic experiences, may have contributed to improving psychological wellbeing. This might be related to the role that generating income has in lowering worries and uncertainty for the future for individuals and their families. On the contrary, being chronically exposed to environmental stresses such as poverty, insecure food and sanitation, temperature extremes, and challenging sleep environments might have contributed to a lower proportion of people with increased wellbeing over time in Uganda (Ridley et al., Citation2020). In line with this hypothesis, an association between higher HTQ-part I score and lower educational level (i.e. having no schooling), and worsening of wellbeing over time, was observed. In Uganda, older age was associated with increased probability of belonging to the class improving over time, but, within each class, to a worsening of wellbeing, while the opposite occurred for primary-level education (although education did not reach global statistical significance in the model to predict class membership).
Another important finding is that length of stay in the host country was associated with increased probability of belonging to the class with lower wellbeing, but with a better outcome in terms of wellbeing change over time. This might be related to a gradual increase in social integration and support and a decrease in language barriers over time, together with a decrease in exposure to serious and multiple traumatic events. This finding aligns with a systematic review of resilience and psychological outcomes in conflict-affected migrants identified an association between strong social and family support and increased resilience and lower levels of psychological problems (Siriwardhana et al., Citation2014). Traumatic events during the pre-migratory phase are risk factors that received most attention in the literature, as many of them have been identified to be strongly associated with mental disorders (Lindencrona et al., Citation2008; Mollica et al., Citation1997; Uphoff et al., Citation2020).
Having a lower HTQ-part I score was associated with increased probability to belong to the class with less psychological symptoms in Western Europe and Turkey. Interestingly, conditionally on other predictors, participants of the Turkish trial showed a lower probability of being in the class with more symptoms, but at the same time they were more likely to show an increase of symptoms over time. This might be related to the instability of the Turkish context in the period between 2018 and 2020. However, this might also be related to the impact of trauma and daily post-migration stressors (e.g. uncertainty regarding asylum status, loss of social support networks, relationship difficulties) on wellbeing, especially considering how these multiple experiences impact on what is meaningful to the person (Miller & Rasmussen, Citation2010; White & Van der Boor, Citation2021). Moreover, the participants in Turkey were predominantly Syrian refugees with very recent experience of the ongoing Syrian conflict that may have affected the trajectories. We identified an association between secondary-level education and likelihood to be in the class with higher level of symptoms, that is in line with the hypothesis that awareness and full understanding of the trauma might worsen psychological status (Tang et al., Citation2017), and with the hypothesis that people with a higher education level are more likely to suffer from role loss in the country of resettlement (Porter & Haslam, Citation2005). Participants in this class, however, improved over time, probably because of the decreased exposure to serious traumatic events and the ability to cope with challenges. Consistently, in Uganda HTQ-part I score was associated with a higher probability to belong to the class with a higher level of symptoms.
Several limitations should be considered while interpreting our findings. Firstly, we used self-report measures instead of instruments administered by clinicians, and this could have affected the estimates of psychological symptoms and wellbeing (Lim et al., Citation2018). Secondly, our findings do not reflect the full clinical range of psychological outcomes. Although depression, PTSD symptoms and functional impairment are the most common psychological problems in this population group (Turrini et al., Citation2017), there are other conditions as alcohol and substance use disorders, anxiety disorders, and prolonged grief that might warrant clinical and scientific attention (Bryant et al., Citation2019; Bryant et al., Citation2021; Nguyen et al., Citation2022; Vasic et al., Citation2021). Further, our sample was composed of asylum seekers and refugees of different cultures (i.e. African, Syrian, Iraqi, Pakistani, Afghani), which may raise an issue of cross-cultural comparability, as traumatic events – despite being similar - might be experienced differently in different systems or under different circumstances, and the existential meanings associated with these experiences have not been explored here (Miller & Rasmussen, Citation2017; Purgato et al., Citation2017). Moreover, participants were recruited in trials, thus are not representative of the whole refugee populations and so we cannot draw any firm conclusions regarding the size of the trajectory classes. They were screened for distress at entry, and this may impact the intercept, which in turn influences the trajectories. Finally, all participants received ‘enhanced care as usual’, that is more than what asylum seekers and refugees normally receive outside the experimental context.
Notwithstanding these limitations, this is, to the best of our knowledge, one of the largest long-term follow-up studies of symptom and wellbeing trajectories in asylum seekers and refugees. Notably, findings may provide important insights on the choice and implementation of psychological interventions. For example, culturally appropriate community-based interventions based on empathetic understanding and shared experience might be delivered for improving specific outcomes as communication and subjective wellbeing. Clinically, despite the identified trajectories indicated spontaneous improvement in most cases, asylum seekers and refugees are exposed to multiple traumatic events and ongoing post-migration stressors and are still vulnerable to increased psychological symptoms, so that psychological programmes need also to target posttraumatic stress arising from exposure to traumatic events. Offering inclusive and accessible promotion and prevention interventions for strengthening mental health and ensuring timely diagnosis and interventions might contribute to a shift from a treatment perspective to a prevention/promotion perspective in mental health. Through a prevention approach, mental health programmes for refugees may enhance protective resources by building upon existing individual strengths and social protective factors to stop, lessen, or delay possible negative individual mental health and behavioural sequelae (Uphoff et al., Citation2020). Additionally, factors like age, educational level, and length of stay in the host country may play a key role in affecting psychological conditions. Our findings of a spontaneous improvement in psychological symptoms indicate that interventions should focus on reinforcing wellbeing and ‘positive’ psychological outcomes. Other and complementary strategies may include universal prevention interventions, interventions targeting the social determinants of mental health, like facilitation to the access to basic or legal services in the host countries, general assistance overcoming barriers to integration, development of social connections and improvement or facilitation of the resettlement process (Hynie, Citation2018; White & Van der Boor, Citation2021).
Supplemental Material
Download MS Word (59.1 KB)Acknowledgements
Authors are grateful to the Department of Excellence (Dipartimento di Eccellenza) project, Department of Neuroscience, Biomedicine and Movement Sciences of the University of Verona. MP, CB, WT, and FT designed this study and drafted the protocol with inputs from PC and MS. All the authors contributed to the recruitment of participants, follow-up assessments, and/or commenting on/editing and revising the drafts of this work. FT, MP, WT and CB planned the statistical analyses. FT performed all of the statistical analyses with inputs from MP and CB.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
This study was conducted using data from three RCTs with a similar design involving asylum seekers and refugees resettled in Western European countries, Turkey, and Uganda (Acarturk et al., Citation2022; Purgato et al., Citation2021; Tol et al., Citation2020). The present manuscript uniquely examine the individual-participant data from the control groups of these three large RCTs.
Additional information
Funding
References
- Acarturk, C., Uygun, E., Ilkkursun, Z., Carswell, K., Tedeschi, F., Batu, M., Eskici, S., Kurt, G., Anttila, M., Au, T., Baumgartner, J., Churchill, R., Cuijpers, P., Becker, T., Koesters, M., Lantta, T., Nosè, M., Ostuzzi, G., Popa, M., … Barbui, C. (2022). Effectiveness of a WHO self-help psychological intervention for preventing mental disorders among Syrian refugees in Turkey: A randomized controlled trial. World Psychiatry, 21(1), 88–95. https://doi.org/10.1002/wps.20939
- Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., & Forneris, C. A. (1996). Psychometric properties of the PTSD checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. https://doi.org/10.1016/0005-7967(96)00033-2
- Bryant, R. A., Bawaneh, A., Giardinelli, L., Awwad, M., Al-Hayek, H., & Akhtar, A. (2021). A prevalence assessment of prolonged grief disorder in Syrian refugees. World Psychiatry, 20(2), 302–303. https://doi.org/10.1002/wps.20876
- Bryant, R. A., Edwards, B., Creamer, M., O'Donnell, M., Forbes, D., Felmingham, K. L., Silove, D., Steel, Z., McFarlane, A. C., van Hooff, M., Nickerson, A., & Hadzi-Pavlovic, D. (2019). A population study of prolonged grief in refugees. Epidemiology and Psychiatric Sciences, 29, e44. https://doi.org/10.1017/S2045796019000386
- Bryant, R. A., Edwards, B., Creamer, M., O'Donnell, M., Forbes, D., Felmingham, K. L., Silove, D., Steel, Z., Nickerson, A., McFarlane, A. C., Van Hooff, M., & Hadzi-Pavlovic, D. (2018). The effect of post-traumatic stress disorder on refugees’ parenting and their children's mental health: A cohort study. The Lancet Public Health, 3(5), e249–e258. https://doi.org/10.1016/S2468-2667(18)30051-3
- Charlson, F., van Ommeren, M., Flaxman, A., Cornett, J., Whiteford, H., & Saxena, S. (2019). New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. The Lancet, 394(10194), 240–248. https://doi.org/10.1016/S0140-6736(19)30934-1
- Cooper, S., Enticott, J. C., Shawyer, F., & Meadows, G. (2019). Determinants of mental illness among humanitarian migrants: Longitudinal analysis of findings from the first three waves of a large cohort study. Frontiers in Psychiatry, 10, 545. https://doi.org/10.3389/fpsyt.2019.00545
- Curran, P. J., & Hussong, A. M. (2009). Integrative data analysis: The simultaneous analysis of multiple data sets. Psychological Methods, 14(2), 81–100. https://doi.org/10.1037/a0015914
- Fazel, M., Wheeler, J., & Danesh, J. (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. The Lancet, 365(9467), 1309–1314. https://doi.org/10.1016/S0140-6736(05)61027-6
- Giacco, D., Laxhman, N., & Priebe, S. (2018). Prevalence of and risk factors for mental disorders in refugees. Seminars in Cell & Developmental Biology, 77, 144–152. https://doi.org/10.1016/j.semcdb.2017.11.030
- Giacco, D., & Priebe, S. (2018). Mental health care for adult refugees in high-income countries. Epidemiology and Psychiatric Sciences, 27(2), 109–116. https://doi.org/10.1017/S2045796017000609
- Goldberg, D. (1992). General Health Questionnaire (GHQ-12). NFER-Nelson.
- Hajak, V. L., Sardana, S., Verdeli, H., & Grimm, S. (2021). A systematic review of factors affecting mental health and well-being of asylum seekers and refugees in Germany. Frontiers in Psychiatry, 12, Article 643704. https://doi.org/10.3389/fpsyt.2021.643704
- Henkelmann, J. R., de Best, S., Deckers, C., Jensen, K., Shahab, M., Elzinga, B., & Molendijk, M. (2020). Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: Systematic review and meta-analysis. BJPsych Open, 6(4), e68. https://doi.org/10.1192/bjo.2020.54
- Huisman, M. (1999). Item Nonresponse: Occurrence, Causes, and Imputation of Missing Answers to Test Items. DSWO Press.
- Hynie, M. (2018). The social determinants of refugee mental health in the post-migration context: A critical review. The Canadian Journal of Psychiatry, 63(5), 297–303. https://doi.org/10.1177/0706743717746666
- Jung, T., & Wickrama, K. A. (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. https://doi.org/10.1111/j.1751-9004.2007.00054.x
- Kessler, R. C., Green, J. G., Gruber, M. J., Sampson, N. A., Bromet, E., Cuitan, M., Furukawa, T. A., Gureje, O., Hinkov, H., Hu, C. Y., Lara, C., Lee, S., Mneimneh, Z., Myer, L., Oakley-Browne, M., Posada-Villa, J., Sagar, R., Viana, M. C., & Zaslavsky, A. M. (2010). Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO World Mental Health (WMH) survey initiative. International Journal of Methods in Psychiatric Research, 19(Suppl 1), 4–22. https://doi.org/10.1002/mpr.310
- Kolenikov, S., & Bollen, K. A. (2012). Testing negative error variances: Is a Heywood case a symptom of misspecification? Sociological Methods & Research, 41(1), 124–167. https://doi.org/10.1177/0049124112442138
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- LeMaster, J. W., Broadbridge, C. L., Lumley, M. A., Arnetz, J. E., Arfken, C., Fetters, M. D., Jamil, H., Pole, N., & Arnetz, B. B. (2018). Acculturation and post-migration psychological symptoms among Iraqi refugees: A path analysis. American Journal of Orthopsychiatry, 88(1), 38–47. https://doi.org/10.1037/ort0000240
- Lenferink, L., Liddell, B. J., Byrow, Y., O'Donnell, M., Bryant, R. A., Mau, V., McMahon, T., Benson, G., & Nickerson, A. (2022). Course and predictors of posttraumatic stress and depression longitudinal symptom profiles in refugees: A latent transition model. Journal of Psychiatric Research, 146, 1–10. https://doi.org/10.1016/j.jpsychires.2021.12.009
- Lie, B. (2002). A 3-year follow-up study of psychosocial functioning and general symptoms in settled refugees. Acta Psychiatrica Scandinavica, 106(6), 415–425. https://doi.org/10.1034/j.1600-0447.2002.01436.x
- Lim, G. Y., Tam, W. W., Lu, Y., Ho, C. S., Zhang, M. W., & Ho, R. C. (2018). Prevalence of depression in the community from 30 countries between 1994 and 2014. Scientific Reports, 8(1), 2861. https://doi.org/10.1038/s41598-018-21243-x
- Lindencrona, F., Ekblad, S., & Hauff, E. (2008). Mental health of recently resettled refugees from the Middle East in Sweden: The impact of pre-resettlement trauma, resettlement stress and capacity to handle stress. Social Psychiatry and Psychiatric Epidemiology, 43(2), 121–131. https://doi.org/10.1007/s00127-007-0280-2
- Lo, Y., Mendell, N. R., & Rubin, D. B. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. https://doi.org/10.1093/biomet/88.3.767
- McLachlan, G., & Peel, D. (2000). Wiley series in probability and statistics. Finite Mixture Models, 420–427. John Wiley & Sons, Inc. http://dx.doi.org/10.1002/0471721182
- Miller, K. E., & Rasmussen, A. (2010). War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science & Medicine, 70(1), 7–16. https://doi.org/10.1016/j.socscimed.2009.09.029
- Miller, K. E., & Rasmussen, A. (2017). The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiology and Psychiatric Sciences, 26(2), 129–138. https://doi.org/10.1017/S2045796016000172
- Mollica, R. F., Caridad, K. R., & Massagli, M. P. (2007). Longitudinal study of posttraumatic stress disorder, depression, and changes in traumatic memories over time in Bosnian refugees. Journal of Nervous & Mental Disease, 195(7), 572–579. https://doi.org/10.1097/NMD.0b013e318093ed2c
- Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard trauma questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. https://doi.org/10.1097/00005053-199202000-00008
- Mollica, R. F., Poole, C., Son, L., Murray, C. C., & Tor, S. (1997). Effects of war trauma on Cambodian refugee adolescents’ functional health and mental health status. Journal of the American Academy of Child & Adolescent Psychiatry, 36(8), 1098–1106. https://doi.org/10.1097/00004583-199708000-00017
- Muthén, L., & Muthén, B. (2017). Mplus user’s guide (eight edition)[Computer software manual]. Los Angeles, CA.
- Müller, L., Gossmann, K., Hartmann, F., Büter, K. P., Rosner, R., & Unterhitzenberger, J. (2019). 1-year follow-up of the mental health and stress factors in asylum-seeking children and adolescents resettled in Germany. BMC Public Health, 19(1), 908. https://doi.org/10.1186/s12889-019-7263-6
- Nguyen, T. P., Guajardo, M., Sahle, B. W., Renzaho, A., & Slewa-Younan, S. (2022). Prevalence of common mental disorders in adult Syrian refugees resettled in high income western countries: A systematic review and meta-analysis. BMC Psychiatry, 22(1), 15. https://doi.org/10.1186/s12888-021-03664-7
- Porter, M., & Haslam, N. (2005). Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. JAMA, 294(5), 602–612. https://doi.org/10.1001/jama.294.5.602
- Priebe, S., Giacco, D., & El-Nagib, R. (2016). Public health aspects of mental health among migrants and refugees: A review of the evidence on mental health care for refugees, asylum seekers and irregular migrants in the WHO European region [Internet]. Copenhagen: WHO Regional Office for Europe.
- Purgato, M., Carswell, K., Tedeschi, F., Acarturk, C., Anttila, M., Au, T., Bajbouj, M., Baumgartner, J., Biondi, M., Churchill, R., Cuijpers, P., Koesters, M., Gastaldon, C., Ilkkursun, Z., Lantta, T., Nosè, M., Ostuzzi, G., Papola, D., Popa, M., Roselli, V., … Barbui, C. (2021). Effectiveness of self-help plus in preventing mental disorders in refugees and asylum seekers in Western Europe: A multinational randomized controlled trial. Psychotherapy and Psychosomatics, 90(6), 403–414. https://doi.org/10.1159/000517504
- Purgato, M., Tol, W. A., & Bass, J. K. (2017). An ecological model for refugee mental health: Implications for research. Epidemiology and Psychiatric Sciences, 26(2), 139–141. https://doi.org/10.1017/S204579601600069X
- Ram, N., & Grimm, K. J. (2009). Growth mixture modeling: A method for identifying differences in longitudinal change Among unobserved groups. International Journal of Behavioral Development, 33(6), 565–576. https://doi.org/10.1177/0165025409343765
- Ridley, M., Rao, G., Schilbach, F., & Patel, V. (2020). Poverty, depression, and anxiety: Causal evidence and mechanisms. Science, 370(6522): eaay0214. https://doi.org/10.1126/science.aay0214
- Roth, G., & Ekblad, S. (2006). A longitudinal perspective on depression and sense of coherence in a sample of mass-evacuated adults from Kosovo. The Journal of Nervous and Mental Disease, 194(5), 378–381. https://doi.org/10.1097/01.nmd.0000217882.70120.38
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(Suppl 20), 22–57.
- Sijbrandij, M. (2018). Expanding the evidence: Key priorities for research on mental health interventions for refugees in high-income countries. Epidemiology and Psychiatric Sciences, 27(2), 105–108. https://doi.org/10.1017/S2045796017000713
- Silove, D., Mohsin, M., Klein, L., Tam, N. J., Dadds, M., Eapen, V., Tol, W. A., da Costa, Z., Savio, E., Soares, R., Steel, Z., & Rees, S. J. (2020). Longitudinal path analysis of depressive symptoms and functioning among women of child-rearing age in postconflict Timor-Leste. BMJ Global Health, 5(3), e002039. https://doi.org/10.1136/bmjgh-2019-002039
- Siriwardhana, C., Ali, S. S., Roberts, B., & Stewart, R. (2014). A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Conflict and Health, 8(1), 13. https://doi.org/10.1186/1752-1505-8-13
- Soloski, K. L., & Durtschi, J. A. (2020). Identifying different ways people change: A latent basis growth mixture model example identifying nonlinear trajectories of binge drinking. Journal of Marital and Family Therapy, 46(4), 638–660. https://doi.org/10.1111/jmft.12382
- StataCorp. (2021). Stata Statistical Software: Release 17. StataCorp LLC.
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Ommeren, M. (2009). Association f torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549. https://doi.org/10.1001/jama.2009.1132
- Strømme, E. M., Haj-Younes, J., Hasha, W., Fadnes, L. T., Kumar, B., Igland, J., & Diaz, E. (2020). Changes in health among Syrian refugees along their migration trajectories from Lebanon to Norway: A prospective cohort study. Public Health, 186, 240–245. https://doi.org/10.1016/j.puhe.2020.07.016
- Tang, B., Deng, Q., Glik, D., Dong, J., & Zhang, L. (2017). A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. International Journal of Environmental Research and Public Health, 14(12), 1537. https://doi.org/10.3390/ijerph14121537
- Tol, W. A., Leku, M. R., Lakin, D. P., Carswell, K., Augustinavicius, J., Adaku, A., Au, T. M., Brown, F. L., Bryant, R. A., Garcia-Moreno, C., Musci, R. J., Ventevogel, P., White, R. G., & van Ommeren, M. (2020). Guided self-help to reduce psychological distress in south Sudanese female refugees in Uganda: A cluster randomised trial. The Lancet Global Health, 8(2), e254–e263. https://doi.org/10.1016/S2214-109X(19)30504-2
- Tomasi, A. M., Slewa-Younan, S., Narchal, R., & Rioseco, P. (2022). Professional mental health help-seeking amongst Afghan and Iraqi refugees in Australia: Understanding predictors five years post resettlement. International Journal of Environmental Research and Public Health, 19(3), 1896. https://doi.org/10.3390/ijerph19031896
- Topp, C. W., Østergaard, S. D., Søndergaard, S., & Bech, P. (2015). The WHO-5 well-being index: A systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167–176. https://doi.org/10.1159/000376585
- Turrini, G., Purgato, M., Acarturk, C., Anttila, M., Au, T., Ballette, F., Bird, M., Carswell, K., Churchill, R., Cuijpers, P., Hall, J., Hansen, L. J., Kösters, M., Lantta, T., Nosè, M., Ostuzzi, G., Sijbrandij, M., Tedeschi, F., Valimaki, M., … Barbui, C. (2019). Efficacy and acceptability of psychosocial interventions in asylum seekers and refugees: Systematic review and meta-analysis. Epidemiology and Psychiatric Sciences, 28(4), 376–388. https://doi.org/10.1017/S2045796019000027
- Turrini, G., Purgato, M., Ballette, F., Nosè, M., Ostuzzi, G., & Barbui, C. (2017). Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. International Journal of Mental Health Systems, 11(1), 51. https://doi.org/10.1186/s13033-017-0156-0
- Uphoff, E., Robertson, L., Cabieses, B., Villalón, F. J., Purgato, M., Churchill, R., & Barbui, C. (2020). An overview of systematic reviews on mental health promotion, prevention, and treatment of common mental disorders for refugees, asylum seekers, and internally displaced persons. Cochrane Database of Systematic Reviews, 9, 9: CD013458. https://doi.org/10.1002/14651858.CD013458.pub2
- Van de Schoot, R., Sijbrandij, M., Winter, S. D., Depaoli, S., & Vermunt, J. K. (2017). The GRoLTS-checklist: Guidelines for reporting on latent trajectory studies. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 451–467. https://doi.org/10.1080/10705511.2016.1247646
- Van der Boor, C. F., Amos, R., Nevitt, S., Dowrick, C., & White, R. G. (2020). Systematic review of factors associated with quality of life of asylum seekers and refugees in high-income countries. Conflict and Health, 14(1), 48. https://doi.org/10.1186/s13031-020-00292-y
- Van Ginneken, N., Chin, W. Y., Lim, Y. C., Ussif, A., Singh, R., Shahmalak, U., Purgato, M., Rojas-García, A., Uphoff, E., McMullen, S., Foss, H. S., Thapa Pachya, A., Rashidian, L., Borghesani, A., Henschke, N., Chong, L. Y., & Lewin, S. (2021). Primary-level worker interventions for the care of people living with mental disorders and distress in low- and middle-income countries. The Cochrane Database of Systematic Reviews, 8, 8: CD009149. https://doi.org/10.1002/14651858.CD009149.pub35
- Vasic, J., Grujicic, R., Toskovic, O., & Pejovic Milovancevic, M. (2021). Mental health, alcohol and substance use of refugee youth. Frontiers in Psychiatry, 12, Article 713152. https://doi.org/10.3389/fpsyt.2021.713152
- Vuong, Q. H. (1989). Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica: Journal of the Econometric Society, 57(2), 307–333. https://doi.org/10.2307/1912557
- Wardenaar, K. J. (2020). Latent class growth analysis and growth mixture modeling using R: A tutorial for two R-packages and a comparison with Mplus. https://doi.org/10.31234/osf.io/m58wx
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5).
- White, R. G., & Van der Boor, C. (2021). Enhancing the capabilities of forcibly displaced people: A human development approach to conflict- and displacement-related stressors. Epidemiology and Psychiatric Sciences, 30, e34. https://doi.org/10.1017/S2045796021000263
- World Health Organization. (2010). Measuring health and disability. Manual for WHO Disability Assessment Schedule WHODAS 2.0.
- Wu, S., Renzaho, A., Hall, B. J., Shi, L., Ling, L., & Chen, W. (2021). Time-varying associations of pre-migration and post-migration stressors in refugees’ mental health during resettlement: A longitudinal study in Australia. The Lancet Psychiatry, 8(1), 36–47. https://doi.org/10.1016/S2215-0366(20)30422-3