ABSTRACT
Background: Research indicates that intensive trauma-focused therapy can be effective in alleviating symptoms of post-traumatic stress disorder (PTSD) and borderline personality disorder (BPD). However, these studies have relied on self-report of BPD symptoms and follow-up data are scarce.
Objective: The purpose of this feasibility study was to determine the effects of an intensive trauma-focused treatment programme on the severity of PTSD and BPD symptoms and the diagnostic status up to a 12-month follow-up.
Methods: A total of 45 (60% female) individuals meeting the diagnostic criteria of both PTSD and BPD participated in an intensive eight-day trauma-focused treatment programme which combined prolonged exposure and EMDR therapy in an inpatient treatment setting. Severity of PTSD and BPD symptoms were assessed at pre-treatment, post-treatment, 6 months, and 12 months after treatment (CAPS-5, BPDSI-IV). Diagnostic status was determined using clinical interviews (CAPS-5 and SCID-5-P) at pre-treatment and 12-month follow-up.
Results: Of all participants, 93.3% had been exposed to physical abuse, and 71.1% to sexual abuse prior to the age of 12 years. PTSD and BPD symptom severity significantly decreased from pre- to post-treatment (Cohen's ds: 1.58 and 0.98, respectively), and these results were maintained at 6- (ds: 1.20 and 1.01) and 12-month follow-up (ds: 1.53 and 1.36). Based upon CAPS-5, 69.2% no longer met the diagnostic criteria of PTSD at 12-month follow-up, while according to the SCID-5-P 73.1% no longer fulfilled the diagnostic criteria of BPD at that time. No significant worsening of symptoms occurred.
Conclusion: The findings of this study, which is the first to examine the effects of psychotherapeutic treatment of PTSD on the presence of a borderline personality disorder one year after treatment, add support to the notion that a brief intensive trauma-focused treatment can be a valuable option for individuals suffering from both PTSD and BPD.
HIGHLIGHTS
Investigated the effects of trauma-focused treatment on BPD.
First study that evaluated the status of BPD diagnosis one year after treatment.
Trauma-focused treatment proved to be a feasible and safe treatment for patients diagnosed with both PTSD and BPD.
Antecedentes: Las investigaciones indican que la terapia intensiva centrada en el trauma puede ser eficaz para aliviar los síntomas del trastorno de estrés postraumático (TEPT) y el trastorno límite de la personalidad (TLP). Sin embargo, estos estudios se han basado en el autoinforme de los síntomas del TLP y los datos de seguimiento son escasos.
Objetivo: El propósito de este estudio de viabilidad fue determinar los efectos de un programa de tratamiento intensivo centrado en el trauma sobre la gravedad de los síntomas de TEPT y TLP y el estado de diagnóstico hasta un seguimiento de 12 meses.
Método: Un total de 45 personas (60% mujeres) que cumplían con los criterios diagnósticos de TEPT y TLP participaron en un programa de tratamiento intensivo de ocho días centrado en el trauma que combinaba exposición prolongada y terapia EMDR en un entorno de tratamiento para pacientes hospitalizados. La gravedad de los síntomas de TEPT y TLP se evaluó antes del tratamiento, después del tratamiento, 6 meses y 12 meses después del tratamiento (CAPS-5, BPDSI-IV). El estado de diagnóstico se determinó mediante entrevistas clínicas (CAPS-5 y SCID-5-P) antes del tratamiento y a los 12 meses de seguimiento.
Resultados: Del total de participantes, el 93,3% había estado expuesto a maltrato físico y el 71,1% a abuso sexual antes de los 12 años. La gravedad de los síntomas de TEPT y TLP disminuyó significativamente desde el pretratamiento hasta el postratamiento (ds de Cohen: 1,58 y 0,98, respectivamente), y estos resultados se mantuvieron a los 6 meses (ds: 1,20 y 1,01) y 12 meses de seguimiento (ds: 1.53 y 1.36). Según el CAPS-5, el 69,2% ya no cumplía los criterios diagnósticos de TEPT a los 12 meses de seguimiento, mientras que según el SCID-5-P, el 73,1% ya no cumplía los criterios diagnósticos de TLP en ese momento. No se produjo un empeoramiento significativo de los síntomas.
Conclusión: Los hallazgos de este estudio, que es el primero en examinar los efectos del tratamiento psicoterapéutico del TEPT en la presencia de un trastorno límite de la personalidad un año después del tratamiento, respaldan la noción de que un tratamiento intensivo breve centrado en el trauma puede ser un opción valiosa para las personas que sufren de TEPT y TLP.
联
背景:研究表明,聚焦创伤的强化治疗可有效缓解创伤后应激障碍 (PTSD) 和边缘型人格障碍 (BPD) 的症状。然而,这些研究依赖于 BPD 症状的自我报告,跟踪数据很少。
目的:本可行性研究旨在确定聚焦创伤的强化治疗方案对 PTSD 和 BPD 症状严重程度以及长达 12个月随访时诊断状态的影响。
方法:共有 45 名(60% 女性)同时符合 PTSD 和 BPD 诊断标准的人参加了为期 8 天的聚焦创伤强化治疗计划,该计划在住院治疗环境中结合了延长暴露和 EMDR 治疗。在治疗前、治疗后、治疗后 6个月和 12个月评估 PTSD 和 BPD 症状的严重程度(CAPS-5、BPDSI-IV)。在治疗前和 12个月的随访中使用临床访谈(CAPS-5 和 SCID-5-P)确定诊断状态。
结果:在所有参与者中,93.3% 的人在 12岁之前曾遭受过身体虐待,71.1% 的人曾遭受过性虐待。 PTSD 和 BPD 症状严重程度从治疗前到治疗后显著降低(Cohen’s d:分别为 1.58 和 0.98),这些结果在 6个月(d:1.20 和 1.01)和 12个月的随访(d: 1.53 和 1.36)维持。根据 CAPS-5,69.2% 在 12个月的随访时不再符合 PTSD 诊断标准,而根据 SCID-5-P,73.1% 在那时不再符合 BPD 诊断标准。没有出现显著的症状恶化。
结论:本研究首次考查了 PTSD 心理治疗对治疗一年后边缘型人格障碍存在的影响,其研究结果进一步支持了以下观点,即简短密集的聚焦创伤治疗对于同时患有 PTSD 和 BPD 的人可以是一个有价值的选择。
1. Introduction
Post-traumatic stress disorder (PTSD) is a severe mental illness that can occur after having been exposed to traumatic events; resulting in intrusions, avoidance tendencies, hyperarousal and negative mood and cognitions (American Psychiatric Association, Citation2013). Research shows that approximately half of individuals diagnosed with PTSD also meet the criteria for at least one personality disorder, with the relationship between PTSD and Borderline Personality Disorder (BPD) being particularly strong (Dunn et al., Citation2004; Goldstein et al., Citation2016). BPD is characterised by a profound pattern of instability in interpersonal relationships, self-image and affect, and high impulsivity, beginning in early adulthood and manifested in various situations (American Psychiatric Association, Citation2013). Evidence suggests that 25–30% of adults meeting the criteria for PTSD also meet the criteria for BPD. Likewise, 30–70% of adults diagnosed with BPD also fulfil the diagnostic criteria for PTSD at some point in their lives (Frías & Palma, Citation2015). This suggests that PTSD and BPD are related and overlapping mental health conditions on a continuum of post-traumatic syndromes that begins with childhood abuse or other forms of traumatic victimisation, and then progresses with increasing morbidity, from PTSD to BPD (Ford & Courtois, Citation2021).
Although PTSD and BPD share many similarities and, in terms of symptoms, may be on the same continuum, guidelines regarding the treatment of both mental illnesses differ significantly. On the one hand, regarding the treatment of PTSD, the National Institute for Health and Care Excellence (NICE, Citation2018) recommends about 8–12 sessions of trauma-focused cognitive behavioural therapy or EMDR therapy, possibly supplemented with antidepressants (NICE, Citation2018). Conversely, the NICE guidelines for treatment of BPD recommend psychotherapy as the treatment of choice, rather than brief psychological interventions of less than three months duration (NICE, Citation2015). Experts also recommend some restraint in using trauma-focused treatment for patients with PTSD and BPD, especially in the case of multiple or chronic traumas (Zlotnick et al., Citation2003). As a result, patients with PTSD and comorbid BPD may receive insufficient or no trauma-focused treatment at all (De Jongh et al., Citation2016).
A meta-analysis that included 14 studies (Slotema et al., Citation2020), and a recent study by Rosner et al. (Citation2019) on the treatment of PTSD in individuals with BPD, showed that they can also benefit from trauma-focused treatment. However, most of the studies did not contain a trauma-focused treatment for PTSD as a stand-alone intervention, and only examined the effect of treatment on PTSD symptoms which was added to, or integrated with, the treatment of BPD (see e.g. Harned et al., Citation2018). Also, there are few studies that have examined treatment effects on symptoms of BPD. To our knowledge, thus far, only four studies have examined the effects of a trauma-focused treatment approach in individuals with PTSD and co-morbid BPD, in which the effect on characteristic symptoms of BPD was also established (Zeifman et al., Citation2021). One RCT found a significant decrease in self-reported BPD symptom severity of both disorders in an integrated PTSD-Borderline treatment programme using cognitive processing therapy (Bohus et al., Citation2020). Two controlled studies (Pabst et al., Citation2014; Steuwe et al., Citation2016) pertained to the effectiveness of Narrative Exposure Therapy (NET), and one uncontrolled study, to intensive treatment, using a combination of prolonged exposure and EMDR therapy, measured through self-report (De Jongh et al., Citation2020). All studies showed promising results in reducing symptoms associated with BPD. The study of De Jongh and his colleagues (Citation2020) included 72 patients with severe PTSD due to multiple traumas. Assessments took place at pre- and post-treatment using the Borderline Symptom List, BSL-23 (Bohus et al., Citation2009). Treatment resulted in a decrease of PTSD symptoms and a significant decrease of BPD symptoms (Cohen's d = 0.70), while none of the patients experienced a worsening of symptoms in response to treatment. These findings suggest that an intensive trauma-focused treatment is a feasible and safe treatment for PTSD patients with clinically elevated symptoms of BPD and that BPD symptoms are likely to decrease along with the alleviation of PTSD symptoms. A limitation of this study, however, was that borderline symptoms were measured through self-report only, whereas no BPD diagnosis was established before and after treatment, and follow-up data were lacking (De Jongh et al., Citation2020). As to the latter, of our knowledge, no prior research has reassessed the diagnostic status of patients in terms of the presence of a personality disorder following psychotherapeutic treatment one year after treatment, nor regarding the treatment of PTSD, or any other Axis I disorder. Markovitz and his colleagues were the first to evaluate psychotherapy effects on personality disorder stability (Markowitz et al., Citation2015). Forty-seven patients with chronic PTSD and a personality disorder received 14 weeks of either prolonged exposure, interpersonal psychotherapy, or relaxation therapy. It appeared that 56% of the treatment responders re-evaluated 26 weeks after treatment no longer met the diagnostic criteria for a personality disorder Unfortunately, BPD was a study exclusion in this trial. To fill this knowledge gap in the literature, the purpose of the current study was to determine the effects associated with a brief intensive trauma-focused treatment on the severity of PTSD and BPD in individuals diagnosed with both PTSD and BPD. Based upon the results of our previous study (De Jongh et al., Citation2020) it was hypothesised that in individuals diagnosed with both PTSD and BPD, the severity of PTSD and BPD symptoms in patients with both PTSD and BPD would significantly decrease from pre- to post-treatment, at 6- and 12-month follow-up, resulting in a loss of both the PTSD and BPD diagnoses. To examine participants’ safety and potential negative reactions to the intervention, the proportion of those experiencing PTSD or BPD symptom worsening and the dropout rate would also be assessed.
2. Method
2.1. Participants
Participants were recruited from individuals referred for treatment to Psychotrauma Expertise Centrum (PSYTREC), a mental health care centre in Bilthoven, The Netherlands, by their general practitioner, psychologist, psychiatrist or mental health centre staff. They took part in PSYTREC's intensive treatment programme for PTSD during the period from February 2020 until January 2021. No inclusion took place at the beginning of the COVID-19 period (April 2020–July 2020). Prior to treatment, patients were assessed to determine whether they met the inclusion criteria i.e. (1) minimum of 18 years old, (2) diagnosed with PTSD according to the DSM-5 (American Psychiatric Association, Citation2013), (3) ability to understand and speak the Dutch language, (4) no attempted suicide within three months prior to treatment, (5) assignment to the 8-day intensive treatment programme, and (6) diagnosed with borderline personality disorder (BPD) according to DSM-5 (APA, Citation2013).
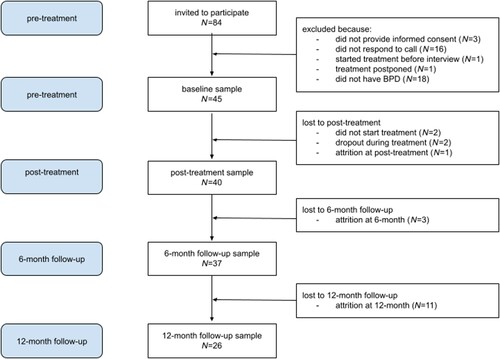
A total of 84 patients were invited to participate in the study, based on the scoring algorithm; trait > = 4 and distress > 1 of the Assessment DSM-4 Personality Disorder, ADP-4, borderline items, which had been administered during the intake phase. All eligible patients were requested to fill out a consent form, after which an appointment was made for the administration of the SCID-5-P. Three patients refused consent and 16 did not respond. If an individual met the criteria for BPD on the SCID-5-P, the BPDSI-IV was administered. For one patient the treatment was expedited and started before the SCID-5-P and BPDSI-IV were performed, and for another treatment was postponed for a year, prohibiting inclusion in the study. Eighteen individuals did not meet the criteria of BPD as assessed with the SCID-5-P. The total number of patients finally included in the study was 45. After inclusion, two patients did not start treatment upon their request, and as a result, they no longer met the inclusion criteria and were excluded from the study. There were also two dropouts during treatment. One person withdrew due to the death of a family member shortly before the start of the treatment. Since they could not optimally benefit from the treatment protocol at that time, commencement was postponed. The second exclusion concerned a patient whose treatment was converted to a 4-day protocol due to a communication error, therefore making them ineligible for this study. In addition, one patient who did not respond to the post-treatment follow-up was also excluded. At the 6-month measurement, one patient indicated that she no longer wished to participate in the study and two patients could no longer be reached. During the 12-month follow-up measurement, 11 patients could no longer be reached and were labelled as attrition. The patient flow is presented in . An ethical exemption from the research protocol was given, drawn from the Medical Ethics Review Committee of VU University Medical Centre (registered with the US Office for Human Research Protections [OHRP] as IRB00002991, FWA number FWA00017598).
2.2. Procedure
During intake, the Clinician-Administered PTSD Scale for the DSM-5 (CAPS-5; Boeschoten et al., Citation2018) was administered to determine the PTSD diagnosis and severity. After the intake, participants completed the Assessment of DSM-IV Personality Disorders questionnaire (ADP-4; borderline subscale) online at home. Those scoring above four on the ADP-4 (Schotte et al., Citation1998) were invited to participate in the study. After obtaining informed consent, the structured clinical interview for DSM-5 personality disorders (SCID-5-P) borderline subscale was administered to establish a BPD classification (First et al., Citation2016). If BPD criteria were met, the Borderline Personality Disorder Symptom Index (BPDSI-IV) was also administered to determine the severity of the BPD (Arntz et al., Citation2003). At post-treatment and at 6-month follow-up, the BPDSI-IV and CAPS-5 were repeated, and at 12-month follow-up, the BPDSI-IV, CAPS-5 and SCID-5-P were again administered along with the SCID 5 P. All interviews were conducted by telephone by a trained researcher.
2.3. Treatment programme
For two consecutive periods of four days a week, patients received an individual 90-minute prolonged exposure (PE) session in the morning and an individual 90-minute eye movement desensitisation and reprocessing (EMDR) therapy session in the afternoon (De Jongh et al., Citation2020; Voorendonk et al., Citation2020). All treatment sessions were administered by clinical psychologists who were trained in the application of both EMDR and PE therapy protocols. The PE session followed a modified version of the protocol of Foa and Hembree (Citation2008). According to this protocol, patients are repeatedly confronted with their traumatic memories (imaginal exposure) and stimuli that relate to these traumatic memories (exposure in vivo).
EMDR therapy was performed according to guidelines by Shapiro (Citation2001) and the Dutch version of the EMDR standard protocol (De Jongh & Ten Broeke, Citation2019). In EMDR therapy, patients imagine the most disturbing part of a traumatic event, while straining their working memory capacities by visually following the therapist's finger movements or other working memory-demanding elements to maximise the working memory load. The version of EMDR therapy used was EMDR 2.0 (see Matthijssen et al., Citation2021). This new therapy variant uses the same (standard EMDR) protocol but utilises a higher dose with regard to the working memory load than regular EMDR therapy. No emotion regulation skills training or relaxation were applied before or during treatment (see De Jongh et al., Citation2016, for the rationale). The second phase of the standard EMDR protocol (i.e. safe place exercise section) was, therefore, removed to avoid disarranging elements of stabilisation and trauma-focused treatment. The patients also conducted physical activities four times per day for a total of six hours, provided by professional physical trainers, as well as, two hours of psychoeducation. The physical activities and psychoeducation took place in groups. After four days of treatment, patients went home for three days and then returned for four days of treatment at the clinic. However, during the COVID pandemic, there was a hybrid version developed, with 4-days’ in-person and 4-days’ online treatment. Only four of the 45 patients in this study took part in the hybrid version. Previous research has shown that intensive trauma-focused treatment of two sessions a day delivered by home-based telehealth is feasible, safe and effective (Bongaerts et al., Citation2021).
2.4 . Measurements
2.4.1. PTSD symptoms
To measure symptom severity and to establish a PTSD diagnosis over the past month, the Dutch version of the CAPS-5 (Boeschoten et al., Citation2018; Weathers et al., Citation2018) was administered at pre-treatment, post-treatment, 6 and at 12-months follow-up. The CAPS-5 contains 20 DSM-5 PTSD symptoms, clustered in four subscales (re-experiencing, avoidance, negative cognitions and mood, hyperarousal). Patients’ PTSD symptoms severity were measured over the past month using 5-point scales for frequency (range 0 = ‘never’ to 4 = ‘almost daily’) and intensity (range 0 = ‘none’ to 4 = ‘extremely’). According to the basic CAPS-5 symptom scoring rule (SEV2 rule), a symptom is present if its severity is rated with 2 or higher (Weathers et al., Citation2018). PTSD severity scores were calculated by summing up items 1–20, with an overall scoring range between 0 and 80. Cronbach's alpha of the CAPS-5 in the present study was 0.58 and interrater reliability (ICC) 0.81. Loss of PTSD diagnosis on the CAPS-5 was determined at post-treatment, and at 6- and 12-month follow-up. Loss of diagnosis was defined as no longer meeting the full classification criteria for PTSD (Boeschoten et al., Citation2018; Weathers, Citation2017).
2.4.2. Borderline symptoms
The ADP-4 (Schotte et al., Citation1998; Schotte & De Doncker, Citation2000) was used to assess the severity of patients’ borderline symptoms at pre-treatment. The ADP-4 has 94 items representing the DSM-IV criteria for 12 personality disorders. In this study, only ten BPD items were used. Each of the 10 items is assessed on two levels: a trait score and a distress score. These two assessments provide both dimensional scales and a categorical diagnostic evaluation (Schotte et al., Citation1998). The trait score measures the presence of the criterion using a 7-point scale. The distress score assesses whether the trait has caused distress to the person or others and indicates this on a 3-point score. More specifically, an item scores ‘positive’ or ‘pathological’, and represents a DSM-5 criterion, only when simultaneously a trait score of 5 (‘rather agree’), 6 (‘agree’) or 7 (‘totally agree’) and a distress score of 2 (‘somewhat’) or 3 (‘most certainly’) are obtained.
BPD diagnosis was assessed at pre-treatment and 12-month follow-up with the borderline subscale of the SCID-5-P (First et al., Citation2016), a semi-structured interview for DSM-5 personality disorder diagnoses. The criteria are each rated on a 3-point scale from absent, sub-threshold to threshold.
To measure the symptom severity of the BPD, the BPDSI-IV (Arntz et al., Citation2003) was administered at pre-treatment, post-treatment, 6- and 12-month follow-up. This semi-structured interview measures the frequency of borderline symptoms over three months prior to administration. The BPDSI-IV consists of 9 subscales each rated on an 11-point scale ranging from 0 (never) to 10 (daily). Self-image-items form an exception and are rated on 5-point Likert scales, ranging from 0 (absent) to 4 (dominant, clear and well-defined not knowing who he/she is), multiplied with 2.5. Each subscale contains different items that represent expressions of the personality traits on which the 9 criteria of the DSM-5 diagnosis of BPD are based (abandonment, relationships, self-image, impulsivity, parasuicide, suicide (plans/attempts), mood swings, emptiness, outbursts of anger and dissociation/paranoid ideas). The final score was determined by dividing the sum of the scores by the number of items (range 0–90). Cronbach's alpha of the BPDSI-IV in the present study was 0.85 and interrater reliability (ICC) 0.81.
2.4.3. Comorbidity and type of trauma
To assess comorbidity at pre-treatment the Dutch version of Mini-International Neuropsychiatric Interview (MINI; Overbeek et al., Citation1999; Sheehan et al., Citation1998) was used. This is a structured diagnostic interview used to assess psychiatric disorders and suicide risk.
During the first intake, the Life Events Checklist for DSM-5 (LEC-5; Boeschoten et al., Citation2014) was administered to inventory the type of traumas.
2.5. Statistical analysis
To control for significant differences on baseline characteristics between the group excluded from analyses at 6-month follow-up (n = 8) and the completers sample (n = 37), chi-square tests and independent samples t-tests were performed for gender, mean age, baseline CAPS-5 and BPDSI-IV scores. Two repeated measures ANOVA were used to determine the change in CAPS-5 and BPDSI-IV symptom scores over time (pre, post, 6- and 12-month follow-up). Preceding analyses on CAPS-5 indicated no violations of assumptions of normality, homogeneity of variance, independence and sphericity. However, preceding analyses on BPDSI-IV indicate violation of the assumption of sphericity (χ(2) = 0.77, p = .010). Therefore, a Greenhouse-Geisser correction was applied (Field, Citation2009). We performed two mixed-design ANOVAs on CAPS-5 and BPDSI-IV scores to determine whether gender had an impact on the results. We computed effect sizes according to the guidelines of Cohen (Citation1988). An effect of 0.2 reflects a small effect, 0.5 a medium, and 0.8 or greater a large effect. A reliable index of change (RCI) was calculated for the CAPS-5 and BPDSI-IV to determine whether patients experienced a clinical worsening or an improvement of symptoms beyond what can be attributed to measurement error (Evans et al., Citation1998). Pooled standard deviations of pre- and post- and 6-month follow-up measurements have been used (Lancaster et al., Citation2019) in combination with test-retest reliability information from previous research (Arntz et al., Citation2003; Weathers Citation2017). To determine the relative effects of the treatment on the different symptom domains at pre- to post-treatment, we performed repeated measures ANOVAs on all BPDSI-IV subscales. Loss of PTSD diagnosis on the CAPS-5 was determined at post-treatment 6- and 12-month follow-up. Loss of diagnosis was defined as no longer fulfilling the SEV2 rule in combination with the DSM-5 algorithm (Boeschoten et al., Citation2018; Weathers Citation2017). At 12 months, we also determined the number of patients who lost their BPD diagnosis according to the SCID-5-P, for which a descriptive analysis was performed. Besides the primary analyses on the completers’ samples, an intent-to-treat (ITT) sample (n = 45) was exploratively analysed where last observations were carried forward. All statistical analyses were performed with SPSS version 25. The level of significance for all statistical analyses in this study was set at α = .05.
3. Results
3.1. Patient flow and sample characteristics
The baseline sample consisted of 45 patients. Of this group, 87% (n = 39) were female with an average age of 41.10 years (SD = 12.74). The patients had been exposed to a variety of traumatic events; that is, 93.3% (n = 42) had been exposed to physical abuse such as being attacked, punched or kicked; 53.3% (n = 24) had witnessed sudden violent death, such as murder of suicide; 71.1% (n = 32) experienced sexual abuse prior to the age of 12 years; and 22.2% (n = 10) to sexual abuse after the age of 12. Baseline characteristics of the total sample are displayed in . No differences could be detected between the group which completed the 6-month measurement (n = 37), and the group who did not complete the follow-up at 6 months (n = 8) on any of the baseline characteristics (all ps > .404).
Table 1. Baseline characteristics of patients with post-traumatic stress disorder and a comorbid borderline personality disorder.
3.2. Change in PTSD symptom severity and diagnostic status at post-treatment, 6-months, and 12-month follow-up (CAPS-5)
The CAPS-5 scores showed a significant decrease from pre- to post-treatment (F(1, 37) = 94.40, p < .001), see . Although we found a significant increase of CAPS-5 scores from post-treatment to 6-month follow-up (F(1, 37) = 6.44, p = .016), the decrease from pre-treatment to 6-month follow-up remained significant (t(37) = 7.32, p < .001). No significant interaction effect between time and gender was found (F[2,70] = 1.379, p = .259). Overall, 21 patients (56.8%) showed reliable symptom improvement on the CAPS-5 from pre- to 6-month follow-up (RC index > 17.05), with an average decrease of 19.89 points (SD = 16.53). In mean scores and effect sizes are displayed. Based upon the CAPS-5, 25 patients (67.6%) no longer fulfilled the diagnostic criteria of PTSD at post-treatment and thus lost their PTSD diagnosis. While at 6-month follow-up 21 patients (56.8%) did not fulfil the diagnostic criteria of PTSD. No significant decrease from 6-month follow up to 12-month follow-up was found t(26) = .85, p = .404. Overall, 17 patients (65.4%) showed reliable symptom improvement from pre- to 12-month follow-up (RC index > 15.73), with an average decrease of 23.31 points (SD = 15.21). Based on the CAPS-5, 18 out of 26 patients (69.2%) no longer fulfilled the diagnostic criteria of PTSD at 12-month follow-up. The intent-to-treat sample (n = 45) resulted in the same pattern of results as the completers’ samples.
Figure 2. Means of CAPS-5 scores over time at pre- (n = 45), post-treatment (n = 40), 6-month follow-up (n = 37) and 12-month follow-up (n = 26). CAPS-5 = Clinician-Administered PTSD Scale.
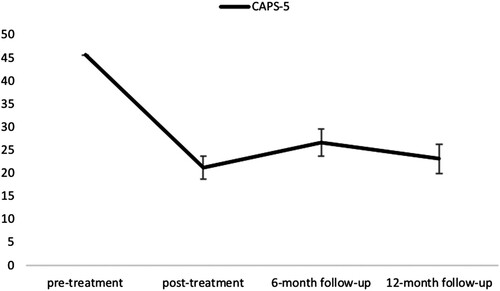
Table 2. CAPS-5 and BPDSI-IV scores at pre-treatment, post-treatment, 6-month follow-up and 12-month follow-up.
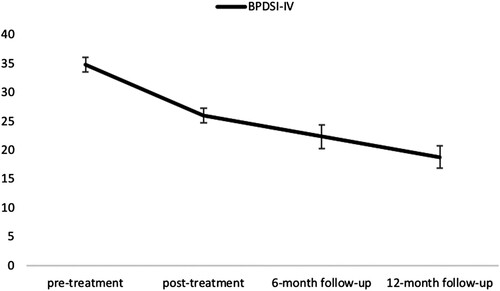
3.3. Change in BPD symptom severity and diagnostic status at post-treatment, 6-month, and 12-month follow-up (BPDSI-IV and SCID-5-P)
Patients’ BPDSI-IV scores showed a significant decrease from pre- to post-treatment (F(1, 37) = 41.99, p < .001), see . In addition, there was a further significant reduction in BPDSI-IV scores from post-treatment to 6-month follow-up (F(1,37) = 5.30, p = .027). No significant time by gender interaction regarding the BPDSI-IV score was found (F[1.63, 57.01] =, p = .225). Overall, 21 patients (46.7%) showed reliable symptom improvement on the BPDSI-IV from pre- to 6-month follow-up (RC index > 10.40), with an average decrease of 12.67 points (SD = 12.54). No significant decrease from 6-month follow up to 12-month follow up was found t(26) = 1.69, p = .104. Overall, 13 patients (50.0%) showed reliable symptom improvement on the BPDSI-IV from pre- to 12-month follow-up (RC index > 13.30), with an average decrease of 14.07 points (SD = 10.50). In mean scores and effect sizes are displayed. Patients’ BPDSI-IV scores showed a significant decrease from pre- to post-treatment regarding all nine subscales all (ps < .022), indicating that the therapy affected all clusters of the personality disorder to a comparable extent. Based upon the SCID-5-P, 19 out of 26 patients (73.1%) no longer fulfilled the diagnostic criteria of BPD at 12-month follow-up. Between the results of the intent-to-treat analyses and the completers’ analyse, no differences were found.
3.4. Patient safety
Two patients dropped out during the 8-day treatment which proved to be unrelated to the application of the therapeutic interventions. The mother of one patient died a day before the start of the treatment, leaving her unable to focus properly on the treatment. There was a communication error in the planning of the treatment of the other patient, which resulted in converting the treatment to the 4-day programme, as a result of which they no longer met the inclusion criteria of the study. In addition, no significant worsening of symptoms occurred, based upon either the CAPS-5 nor BPDSI-IV scores from pre- to post-treatment (CAPS-5 > 15.45; BPDSI-IV >12.29).
4. Discussion
The effects of trauma-focused treatment on symptoms characteristic of borderline personality disorder (BPD) have barely been studied. The present study not only examined the effect of a brief intensive trauma-focused treatment on the severity of PTSD and BPD symptoms, but also addressed the diagnostic status of patients by assessing the diagnostic criteria of both PTSD and BPD. This makes it the first study to have examined the effects of psychotherapeutic treatment of an Axis I disorder on the presence of an Axis II personality disorder one year after treatment, and supports the importance of conducting a randomised controlled trial in this area.
The main outcome of this study shows that although patients fulfilled the diagnostic criteria of both mental health conditions, compared to pre-treatment, the symptoms of PTSD and BPD decreased significantly after treatment, at 6-month follow-up and one year after treatment. More specifically, almost 70% no longer met the diagnostic criteria of PTSD at 12-month follow-up, while 73% no longer fulfilled the diagnostic criteria of BPD at that time. During the eight-day treatment, only two patients dropped out, for reasons which appeared to be unrelated to treatment. More importantly, no adverse effects of treatment or significant symptom worsening occurred.
The treatment programme is brief and intensive (16 sessions within 8 days) and does not contain elements of pre-treatment emotion regulation or other stabilising interventions. It consists of a combination of two evidence-based trauma-focused therapies for PTSD (EMDR and exposure therapy in combination with physical activities and psychoeducation). These have shown good results with large effect sizes for the treatment of severe (Van Woudenberg et al., Citation2018) or Complex PTSD (Voorendonk et al., Citation2020) as well as for symptoms typically related to BPD (De Jongh et al., Citation2020). The results of the present study are in line with these previous findings in that both PTSD and BPD symptoms decreased after intensive trauma-focused treatment and show that these results also persist in the long term. In addition, these findings are in accordance with those supporting positive treatment effects of trauma-focused treatment in individuals with both PTSD and BPD (Bohus et al., Citation2020; Slotema et al., Citation2020). However, the difference is that our treatment programme was a short-term intensive trauma-focused treatment without any form of emotion regulation or relaxation introduced prior to treatment. Accordingly, the results further support previous findings that comorbid psychopathological symptoms decrease after successful intensive trauma-focused treatment (van Minnen et al., Citation2015), and that trauma-focused treatment is a viable option for individuals with symptoms of BPD (Hafkemeijer et al., Citation2020; Hendriks et al., Citation2018).
The results are remarkable in that eight days of treatment, consisting of a total of 16 sessions of 90 minutes’ duration, showed such a high degree of effectiveness both in terms of effect size of the reduction in BPD symptoms, and in the proportion of people who no longer met the diagnostic criteria of BPD one year after treatment (73%).
Even though it is unclear whether participants received treatment during the follow-up period (and if so, what type), the effect size of the treatment on symptoms on BPD from pre-treatment to one year following treatment (Cohen's d = 1.36) is notable. Particularly, in light of meta-analytic findings showing that BPD treatments typically yield small to medium effect sizes for BPD symptoms (Cristea et al., Citation2017). Furthermore, the three comparable trauma-focused studies in this area involved much longer treatment periods (2.5 years, Pabst et al., Citation2014; 1 year, Bohus et al., Citation2020; 10 weeks, Steuwe et al., Citation2016). The result is even more remarkable when we compare these findings with those from non-trauma-focused residential therapy programmes that are completely focused on the treatment of BPD (e.g. Masland et al., Citation2019). The effect size of the BPD symptom measure (Zanarini rating scale for BPD) used to determine the effectiveness of the interventions, was much lower (Cohen's d = 0.71) and involved approximately 56 h of weekly structured therapy over four months.
An explanation for the finding that PTSD severity as well as BPD symptoms decreased might be related to the fact that both diagnoses overlap in their constructs. Clearly, PTSD and BPD show an overlap in criteria such as affective instability and interpersonal dysfunction (Ford & Courtois, Citation2021). The relationship between these mental health conditions in the present study was further illustrated by the association between the difference scores of the CAPS-5 and the BPDSI-IV from pre-treatment to 6-month follow-up (Rho = .573, p < .000, two-tailed). What these, and other results teach us, is that if people develop pathology configured by the impact of adverse childhood experiences, and the clinician appropriately targets the memories that gave rise to these symptoms, the pathology is amenable to change (Hafkemeijer et al., Citation2021).
Several limitations of the present study need to be mentioned. The most important limitation concerns the uncontrolled elements which make it impossible to determine how much of patients’ improvements are due to the effect of treatment itself. A more definitive conclusion on the effectiveness of trauma-focused treatment in people with BPD will have to wait for the results of a large randomised controlled trial that is currently being conducted (Hofman et al., Citation2022). Another uncontrolled element in our study was that we did not measure whether patients might have received other treatment for PTSD or BPD (nor in this case, the type of treatment) during the intervening period prior to our 12 -month post treatment follow-up, and whether this might have been a factor in their recovery. Therefore, we do not definitively know whether the loss in BPD diagnosis at 12 months is completely the result of our treatment programme. In addition, we did not assess other co-occurring personality disorders (e.g. avoidant PD) which may have had an impact on the outcomes. Further, our treatment programme was provided on an inpatient basis, so it is not known whether these results can be generalised to outpatient treatment programmes, albeit that outpatient trauma-focussed treatment outcomes suggest similar results (Hafkemeijer et al., Citation2020). Another important limitation relates to the quality of our follow-up data, as we could only analyse a sub-sample for the 12-month follow-up. Indeed, some of the patients could not be traced or did not respond to our repeated attempts to follow up with them. Therefore, the findings of this study should be interpreted with caution. This certainly also holds true for the dropout rate of patients. Although dropout during treatment was relatively low (4%) and ower than average for PTSD studies (16%; Lewis et al., Citation2020), during the follow-up period there appeared to be a relatively high degree of attrition, which is not uncommon in this type of trial. Clearly, assessing the reliability of the long-term results is difficult because the exact reasons for those refusing follow-up measurements cannot be determined. Reassuringly, we found no difference in initial treatment success between those from whom we were able to collect all measurements and those from whom we could not. The question is, therefore, whether the latter group were people who were dissatisfied with the treatment or, for example, did not have the time or desire to engage in a diagnostic interview in excess of an hour. Although it is conceivable that treatment with a trauma focus could cause exacerbation of symptoms, this was by no means the case in those who were diagnosed with BPD during therapy. Therefore, it is less logical to assume that the attrition between 6 and 12 months is attributable to the eight days of therapy. Despite these limitations, the main strength of this study, compared to previous studies is that this is the first study to have established a BPD diagnosis in addition to BPD symptom change, one year after completion of treatment.
In conclusion, the results of the present study support the notion that most patients with both PTSD and BPD benefitted strongly from intensive trauma-focused treatment. This suggests that intensive trauma-focused treatment poses no significant risks for patients with both PTSD and BPD and that BPD patients should not be discouraged from undergoing evidence-based trauma-focused treatment.
Acknowledgement
The authors thank Frances Klaff for her help in editing the last version of the manuscript.
Disclosure statement
Agnes Van Minnen receives income for published book chapters on PTSD and for the training of postdoctoral professionals in prolonged exposure. Ad de Jongh receives income from published books on EMDR therapy and for the training of postdoctoral professionals in this method. The other authors do not have competing interests.
Data availability statement
Data available on request due to privacy/ethical restrictions. The data that support the findings of this study are available on request from the corresponding author, AdJ. The data are not publicly available due to their containing information that could compromise the privacy of research participants. Furthermore, participants were not asked to give consent of saving their data in a public data repository.
Correction Statement
This article was originally published with errors, which have now been corrected in the online version. Please see Correction (http://dx.doi.org/10.1080/20008066.2024.2355062)
References
- American Psychiatric Association, A. P. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
- Arntz, A., van den Hoorn, M., Cornelis, J., Verheul, R., van den Bosch, W. M. C., & de Bie, A. J. H. T. (2003). Reliability and validity of the borderline personality disorder severity index. Journal of Personality Disorders, 17(1), 45–59. https://doi.org/10.1521/pedi.17.1.45.24053
- Boeschoten, M. A., Bakker, A., Jongedijk, R. A., & Olff, M. (2014). Life event checklist for DSM-5 (LEC-5)-Dutch version. Diemen, The Netherlands: Arq Psychotrauma ExpertGroep. https://doi.org/10.1037/e566912010-001
- Boeschoten, M. A., Van der Aa, N., Bakker, A., Ter Heide, F. J. J., Hoofwijk, M. C., Jongedijk, R. A., & Olff, M. (2018). Development and evaluation of the Dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). European Journal of Psychotraumatology, 9(1), 1546085. https://doi.org/10.1080/20008198.2018.1546085
- Bohus, M., Kldeindienst, N., Hahn, C., Muller-Engelmann, M., Ludascher, P., Steil, R., Fydrich, T., Kuehner, C., Resick, P.A., Stiglmayr, C. & Schmahl, C. (2020). Dialectical behavior therapy for posttraumatic stress disorder (DBT- PTSD) compared with cognitive processing therapy (CPT) in complex presentations of PTSD in women survivors of childhood abuse: A randomized clinical trial. JAMA Psychiatry, 77(12), 1235–1245. https://doi.org/10.1001/jamapsychiatry.2020.2148
- Bohus, M., Kleindienst, N., Limberger, M. F., Stieglitz, R.-D., Domsalla, M., Chapman, A. L., Steil, R., Philipsen, A., & Wolf, M. (2009). The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology, 42(1), 32–39. https://doi.org/10.1159/000173701
- Bongaerts, H., Voorendonk, E. M., van Minnen, A., & de Jongh, A. (2021). Safety and effectiveness of intensive treatment for complex PTSD delivered via home-based telehealth. European Journal of Psychotraumatology, 12(1), 1860346. https://doi.org/10.1080/20008198.2020.1860346
- Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences (2nd ed.). Lawrence Erlbaum Associates, Publishers.
- Cristea, I. A., Gentili, C., Cotet, C. D., Palomba, D., Barbui, C., & Cuijpers, P. (2017). Efficacy of psychotherapies for borderline personality disorder: A systematic review and meta-analysis. JAMA Psychiatry, 74(4), 319–328. https://doi.org/10.1001/jamapsychiatry.2016.4287
- De Jongh, A., Groenland, G. N., Sanches, S., Bongaerts, H., Voorendonk, E. M., & Van Minnen, A. (2020). The impact of brief intensive trauma-focused treatment for PTSD on symptoms of borderline personality disorder. European Journal of Psychotraumatology, 11(1), 1721142. https://doi.org/10.1080/20008198.2020.1721142
- De Jongh, A., Resick, P. A., Zoellner, L. A., van Minnen, A., Lee, C. W., Monson, C. M., Foa, E. B., Wheeler, K., Broeke, E. T., Feeny, N., Rauch, S. A. M., Chard, K. M., Mueser, K. T., Sloan, D. M., van der Gaag, M., Rothbaum, B. O., Neuner, F., de Roos, C., Hehenkamp, L. M. J., … Bicanic, I. A. E. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33(5), 359–369. https://doi.org/10.1002/da.22469
- De Jongh, A., & Ten Broeke, E. (2019). Handboek EMDR: Een geprotocolleerde behandelmethode voor de gevolgen van psychotrauma [Handbook EMDR: A protocoled treatment method for the consequences of psychotrauma]. Pearson Assessment and Information B.V.
- Dunn, N. J., Yanasak, E., Schillaci, J., Simotas, S., Rehm, L. P., Souchek, J., Menke, T., Ashton, C., & Hamilton, J. D. (2004). Personality disorders in veterans with posttraumatic stress disorder and depression. Journal of Traumatic Stress, 17(1), 75–82. https://doi.org/10.1023/b:jots.0000014680.54051.50
- Evans, C., Margison, F., & Barkham, M. (1998). The contribution of reliable and clinically significant change methods to evidence-based mental health. Evidence-Based Mental Health, 1(3), 70–72. https://doi.org/10.1136/ebmh.1.3.70
- Field, A. (2009). Discovering Statistics Using SPSS. SAGE Publications.
- First, M. B., Williams, J. B. W., Benjamin, L. S., & Spitzer, R. L. (2016). SCID-5-PD: Structured clinical interview for DSM-5 personality disorders. American Psychiatric Association Publishing.
- Foa, E., & Hembree, E. (2008). Treatment of prolonged exposure therapy (PE). PsycEXTRA Dataset. https://doi.org/10.1037/e517302011-034.
- Ford, J. D., & Courtois, C. A. (2021). Complex PTSD and borderline personality disorder. Borderline Personality Disorder and Emotion Dysregulation, 8(1), 1–21. https://doi.org/10.1186/s40479-021-00155-9
- Frías, Á, & Palma, C. (2015). Comorbidity between post-traumatic stress disorder and borderline personality disorder: A review. Psychopathology, 48(1), 1–10. https://doi.org/10.1159/000363145
- Goldstein, R. B., Smith, S. M., Chou, S. P., Saha, T. D., Jung, J., Zhang, H., Pickering, R. P., Ruan, W. J., Huang, B., & Grant, B. F. (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the national epidemiologic survey on alcohol and related conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. https://doi.org/10.1007/s00127-016-1208-5
- Hafkemeijer, L., de Jongh, A., van der Palen, J., & Starrenburg, A. (2020). Eye movement desensitization and reprocessing (EMDR) in patients with a personality disorder. European Journal of Psychotraumatology, 11(1), 1838777. https://doi.org/10.1080/20008198.2020.1838777
- Hafkemeijer, L., Starrenburg, A., van der Palen, J., Slotema, K., & de Jongh, A. (2021). Does EMDR therapy have an effect on memories of emotional abuse, neglect and other types of adverse events in patients with a personality disorder? Preliminary data. Journal of Clinical Medicine, 10(19), 4333. https://doi.org/10.3390/jcm10194333
- Harned, M. S., Wilks, C. R., Schmidt, S. C., & Coyle, T. N. (2018). Improving functional outcomes in women with borderline personality disorder and PTSD by changing PTSD severity and post-traumatic cognitions. Behaviour Research and Therapy, 103, 53–61. https://doi.org/10.1016/j.brat.2018.02.002
- Hendriks, L., Kleine, R. A. D., Broekman, T. G., Hendriks, G. J., & Minnen, A. V. (2018). Intensive prolonged exposure therapy for chronic PTSD patients following multiple trauma and multiple treatment attempts. European Journal of Psychotraumatology, 9(1), 1425574. https://doi.org/10.1080/20008198.2018.1425574
- Hofman, S., Hafkemeijer, L., De Jongh, A., Starrenburg, A., & Slotema, K. (2022). Trauma-focused EMDR for personality disorders among outpatients (TEMPO): Study protocol for a randomized controlled trial. Trials, 23(1), 1–15. https://doi.org/10.1186/s13063-022-06082-6
- Lancaster, C. L., Gros, D. F., Mullarkey, M. C., Badour, C. L., Killeen, T. K., Brady, K. T., & Back, S. E. (2019). Does trauma-focused exposure therapy exacerbate symptoms among patients with comorbid PTSD and substance use disorders? Behavioural and Cognitive Psychotherapy, 48(1), 38–53. https://doi.org/10.1017/s1352465819000304
- Lewis, C., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1709709. https://doi.org/10.1080/20008198.2019.1709709
- Markowitz, J. C., Petkova, E., Biyanova, T., Ding, K., Suh, E. J., & Neria, Y. (2015). Exploring personality diagnosis stability following acute psychotherapy for chronic posttraumatic stress disorder. Depression and Anxiety, 32(12), 919–926. https://doi.org/10.1002/da.22436
- Masland, S. R., Cummings, M. H., Null, K. E., Woynowskie, K. M., & Choi-Kain, L. W. (2019). Changes in post-traumatic stress disorder symptoms during residential treatment for borderline personality disorder: A longitudinal cross-lagged study. Borderline Personality Disorder and Emotion Dysregulation, 6(1), 1–9. https://doi.org/10.1186/s40479-019-0113-4
- Matthijssen, S. J. M. A., Brouwers, T. C., van Roozendaal, C., Vuister, T. C. M., & De Jongh, A. (2021). The effect of EMDR versus EMDR 2.0 on emotionality and vividness of aversive memories in a non-clinical sample. European Journal of Psychotraumatology, 12(1), 1956793. https://doi.org/10.1080/20008198.2021.1956793
- Minnen, A., van Zoellner, L. A., Harned, M. S., & Mills, K. (2015). Changes in comorbid conditions after prolonged exposure for PTSD: A literature review. Current Psychiatry Reports, 17(2), 1–16. https://doi.org/10.1007/s11920-014-0542-0
- National Institute for Health and Care Excellence (NICE). (2018). Post-traumatic stress disorder. London, UK: National Collaborating Centre for Mental Health. https://www.nice.org.uk/guidance/ng116.
- National Institute for Health and Clinical Excellence (NICE). (2015). Personality disorders: Borderline and antisocial. London, UK: National Collaborating Centre for Mental Health. www.nice.org.uk/guidance/qs88.
- Overbeek, T., Schruers, K., & Griez, E. (1999). Mini International Neuropsychiatric Interview, Nederlandse Versie 5.0.0. Maastricht University.
- Pabst, A., Schauer, M., Bernhardt, K., Ruf-Leuschner, M., Goder, R., Elbert, T., & Seeck-Hirschner, M. (2014). Evaluation of narrative exposure therapy (NET) for borderline personality disorder with comorbid posttraumatic stress disorder. Clinical Neuropsychiatry, 11(4), 108–117.
- Rosner, R., Rimane, E., Frick, U., Gutermann, J., Hagl, M., Renneberg, B., Schreiber, F., Vogel, A., & Steil, R. (2019). Effect of developmentally adapted cognitive processing therapy for youth with symptoms of posttraumatic stress disorder after childhood sexual and physical abuse: A randomized clinical trial. JAMA Psychiatry, 76(5), 484–491. https://doi.org/10.1001/jamapsychiatry.2018.4349
- Schotte, C. K. W., & De Doncker, D. (2000). De ADP-IV: Een vragenlijst voor een therapeutisch georiënteerde diagnostiek van persoonlijkheidsstoornissen. Psychopraxis, 2(6), 267–273.
- Schotte, C. K. W., de Doncker, D., Vankerckhoven, C., Vertommen, H., & Cosyns, P. (1998). Self-report assessment of the DSM-IV personality disorders. Measurement of trait and distress characteristics: The ADP-IV. Psychological Medicine, 28(5), 1179–1188. https://doi.org/10.1017/s0033291798007041
- Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols and procedures (2nd ed.). Guilford Press.
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R. & Dunbar, G. C. (1998). The mini-international neuropsychiatric interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–33.
- Slotema, C. W., Wilhelmus, B., Arends, L. R., & Franken, I. H. A. (2020). Psychotherapy for posttraumatic stress disorder in patients with borderline personality disorder: A systematic review and meta-analysis of its efficacy and safety. European Journal of Psychotraumatology, 11(1), 1796188. https://doi.org/10.1080/20008198.2020.1796188
- Steuwe, C., Rullkotter, N., Ertl, V., Berg, M., Neuner, F., Beblo, T., & Driessen, M. (2016). Effectiveness and feasibility of narrative exposure therapy (NET) in patients with borderline personality disorder and posttraumatic stress disorder – A pilot study. BMC Psychiatry, 16(1), 254. https://doi.org/10.1186/s12888-016-0969-4
- Van Woudenberg, C., Voorendonk, E. M., Bongaerts, H., Zoet, H. A., Verhagen, M., Van Minnen, A., Lee, C. W., & De Jongh, A. (2018). The effectiveness of an intensive treatment programme combining prolonged exposure and EMDR for severe posttraumatic stress disorder (PTSD). European Journal of Psychotraumatology, 9(1), 1487225. https://doi.org/10.1080/20008198.2018.1487225
- Voorendonk, E. M., De Jongh, A., Rozendaal, L., & Van Minnen, A. (2020). Trauma-focused treatment outcome for complex PTSD patients: Results of an intensive treatment programme. European Journal of Psychotraumatology, 11(1), 1783955. https://doi.org/10.1080/20008198.2020.1783955
- Weathers, F. W. (2017). Redefining posttraumatic stress disorder for DSM-5. Current Opinion in Psychology, 14, 122–126. https://doi.org/10.1016/j.copsyc.2017.01.002
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., Keane, T. M., & Marx, B. P. (2018). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. https://doi.org/10.1037/pas0000486
- Zeifman, R. J., Landy, M. S. H., Liebman, R. E., Fitzpatrick, S., & Monson, C. M. (2021). Optimizing treatment for comorbid borderline personality disorder and posttraumatic stress disorder: A systematic review of psychotherapeutic approaches and treatment efficacy. Clinical Psychology Review, 86, 102030. https://doi.org/10.1016/j.cpr.2021.102030
- Zlotnick, C., Johnson, D. M., Yen, S., Battle, C. L., Sanislow, C. A., Skodol, A. E., Grilo, C. M., McGlashan, T. H., Gunderson, J. G., Bender, D. S., Zanarini, M. C., & Tracie Shea, M. (2003). Clinical features and impairment in women with borderline personality disorder (BPD) with posttraumatic stress disorder (PTSD), BPD without PTSD, and other personality disorders with PTSD. Journal of Nervous & Mental Disease, 191(11), 706–713. https://doi.org/10.1097/01.nmd.0000095122.29476.ff