ABSTRACT
Background: Many youth with posttraumatic stress symptoms (PTSS) do not receive evidence-based care. Internet- and Mobile-Based Interventions (IMIs) comprising evidence-based trauma-focused components can address this gap, but research is scarce. Thus, we investigated the feasibility of a trauma-focused IMI for youth with PTSS.
Methods: In a one-arm non-randomized prospective proof-of-concept study, 32 youths aged 15–21 years with clinically relevant PTSS (CATS ≥ 21) received access to a trauma-focused IMI with therapist guidance, comprising nine sessions on an eHealth platform accessible via web-browser. We used a feasibility framework assessing recruitment capability, sample characteristics, data collection, satisfaction, acceptability, study management abilities, safety aspects, and efficacy of the IMI in PTSS severity and related outcomes. Self-rated assessments took place pre-, mid-, post-intervention and at 3-month follow-up and clinician-rated assessments at baseline and post-intervention.
Results: The sample mainly consisted of young adult females with interpersonal trauma and high PTSS levels (CATS, M = 31.63, SD = 7.64). The IMI sessions were found useful and comprehensible, whereas feasibility of trauma processing was perceived as difficult. Around one-third of participants (31%) completed the IMI’s eight core sessions. The study completer analysis showed a significant reduction with large effects in self-rated PTSS at post-treatment [t(21) = 4.27; p < .001; d = 0.88] and follow-up [t(18) = 3.83; p = .001; d = 0.84], and clinician-rated PTSD severity at post-treatment [t(21) = 4.52; p < .001; d = 0.93]. The intention-to-treat analysis indicated significant reductions for PTSS at post-treatment and follow-up with large effect sizes (d = −0.97– –1.02). All participants experienced at least one negative effect, with the most common being the resurfacing of unpleasant memories (n = 17/22, 77%).
Conclusion: The study reached highly burdened young adults. The IMI was accepted in terms of usefulness and comprehensibility but many youths did not complete all sessions. Exploration of strategies to improve adherence in trauma-focused IMIs for youth is warranted, alongside the evaluation of the IMI's efficacy in a subsequent randomized controlled trial.
HIGHLIGHTS
Youth often lack access to evidence-based care after trauma. This study assessed the feasibility of a trauma-focused internet- and mobile-based intervention with therapist guidance.
The intervention was accepted by youths, and the preliminary evaluation of participant responses suggests its efficacy.
Future studies should examine strategies to improve adherence and the IMI’s efficacy in a RCT.
Antecedentes: Muchos jóvenes con síntomas de estrés postraumáticos (PTSS en su sigla en inglés) no reciben atención basada en la evidencia. Las intervenciones en línea y por medio de dispositivos móviles (IMIs en su sigla en inglés) que incluyen componentes centrado en el trauma basados en la evidencia pueden abordar esta brecha, pero la investigación es escasa. Así, investigamos la factibilidad de una IMI centrada en el trauma para jóvenes con PTSS.
Métodos: En un estudio de prueba del concepto futuro no aleatorizado de un brazo, 32 jóvenes de 15 a 21 años con PTSS clínicamente relevante (CATS ≥ 21) recibieron acceso a la IMI centrada en el trauma con la guía de un terapeuta, incluyendo nueve sesiones en una plataforma eHealth de acceso por medio de página web. Usamos un marco de factibilidad para evaluar la capacidad de reclutamiento, las características de la muestra, la recolección de datos, satisfacción, aceptabilidad, habilidades de la gestión del estudio, aspectos de seguridad, y la eficacia de la IMI en la severidad de los PTSS y los resultados relacionados. Se realizaron las evaluaciones de autoinforme antes, en la mitad, y luego de la intervención y a los tres meses de seguimiento y las evaluaciones calificadas por los clínicos a nivel basal y después de la intervención.
Resultados: La muestra consistió principalmente de mujeres adultas jóvenes con trauma interpersonal y altos niveles de PTSS (CATS, M = 31.63, DE = 7.64). Las sesiones de la IMI se consideraron útiles y comprehensivas, mientras que la factibilidad del procesamiento del trauma fue percibida como difícil. Alrededor de uno de cada tres participantes (31%) completaron las ocho sesiones centrales de la IMI. El análisis de quienes completaron el estudio, mostró una reducción significativa con efectos grandes en los PTSS autoinformados después del tratamiento [t(21) = 4.27; p < .001; d = 0.88] y seguimiento [t(18) = 3.83; p = .001; d = 0.84], y la severidad del TEPT calificado por el clínico luego del tratamiento [t(21) = 4.52; p < .001; d = 0.93]. El análisis de intención de tratar indicó reducciones significativas para los PTSS después del tratamiento y seguimiento con efectos de tamaño grande (d = −0.97– −1.02). Todos los participantes experimentaron por lo menos un efecto negativo, siendo el más común el resurgimiento de recuerdos desagradables (n = 17/22, 77%).
Conclusión: El estudio alcanzó a adultos jóvenes con alta carga. Las IMI fueron aceptadas en términos de la utilidad y compresibilidad pero muchos jóvenes no completaron todas las sesiones. Se garantiza la exploración de las estrategias para mejorar la adherencia en las IMIs centrada en el trauma para jóvenes, al mismo tiempo que la evaluación de la eficacia de las IMI en un ensayo controlado aleatorio subsecuente.
| List of Abbrevations | ||
| (S)AEs | = | Potential (Serious) Adverse Events |
| APOI | = | Attitudes towards Psychological Online Interventions Questionnaire |
| AUDIT | = | Alcohol use disorders identification test |
| CAPS-CA-5 | = | Clinician-Administered PTSD Scale for DSM-5 |
| CATS | = | Child and Adolescent Trauma Screen |
| CPTCI-SF | = | Child posttraumatic cognitions inventory short version |
| CSQ | = | Client satisfaction questionnaire |
| CSQ-I | = | Client Satisfaction Questionnaire, version adapted for Internet interventions |
| CUDIT-R | = | Cannabis use disorder identification test-revised |
| GAD-7 | = | Generalized anxiety disorder assessment |
| IMIs | = | Internet – and Mobile-Based Interventions |
| i-tf-CBT | = | Internet-based trauma-focused cognitive behavioural therapy |
| KIDSCREEN | = | Health-Related Quality of Life Questionnaire for Children and Young People |
| Kinder-DIPS | = | Diagnostic Interview for Mental Disorders for Children |
| M | = | Mean |
| MMRM | = | Multivariate mixed effect models for repeated measures |
| NEQ | = | Negative Effects Questionnaire |
| PHQ-9 | = | Patient health questionnaire |
| PTSD | = | Posttraumatic stress disorder |
| PTSS | = | Posttraumatic stress symptoms |
| SD | = | Standard Deviation |
| RCI | = | Reliable change index |
| RCT | = | Randomized controlled trial |
| SITBI | = | Self-Injurious Thoughts and Behaviours Interview |
| tf-CBT | = | Trauma-focused cognitive behavioural therapy |
1. Theoretical background
Posttraumatic Stress Disorder (PTSD) in adolescents and young adults can be effectively treated with trauma-focused psychotherapy, as recommended in national and international treatment guidelines (ISTSS Guidelines Committee, Citation2019; Lethbridge & Australia, Citation2020; Rosner, Gutermann, et al., Citation2020). Trauma focus implies that cognitive, behavioural, or emotion-focused treatment components are used to facilitate the processing of the traumatic event(s) (Schnurr, Citation2017). Common components of evidence-based trauma-focused treatments for PTSD include psychoeducation, emotion regulation and coping skills, exposure, cognitive processing, restructuring, and/or meaning-making (Kooij et al., Citation2022; Schnyder et al., Citation2015). In youth, trauma-focused cognitive behavioural therapy (tf-CBT) as one form of trauma-focused therapy, has proven effective in reducing posttraumatic stress symptoms (PTSS) with high effect sizes compared to waitlist (d = 1.17; Mavranezouli et al., Citation2020) and medium effect sizes compared to treatments as usual (d = 0.52; Thielemann et al., Citation2022).
Despite available evidence-based approaches, youth with PTSS often remain untreated or receive non-evidence-based interventions (Chen et al., Citation2010; Vogel et al., Citation2021). Youth report barriers hindering face-to-face treatment, such as difficulties trusting others, discomfort with self-disclosure, and the sense of having no influence on the therapy process (Ellinghaus et al., Citation2021; Truss et al., Citation2022). Further, youth seem to prefer self-help, struggle with navigating the healthcare system, and face long waiting times due to a lack of available therapists, especially in terms of trauma-focused therapy (Bundes Psychotherapeuten Kammer, Citation2018; Ellinghaus et al., Citation2021; Gulliver et al., Citation2010; Müller et al., Citation2019).
Internet- and Mobile-based Interventions (IMIs) provide a promising opportunity to overcome structural and attitudinal barriers and expand treatment options. They are easily accessible, and provide greater anonymity, self-direction, and self-control than traditional treatment approaches (Boulos et al., Citation2014). Meta-analytic evidence supports the efficacy of IMIs for common mental health disorders in youth, e.g. depression and anxiety disorders (Ebert et al., Citation2015; Grist et al., Citation2019; Wu et al., Citation2023). In adults, trauma-focused internet-based CBTs (i-tf-CBTs) have been shown to be effective and non-inferior to face-to-face tf-CBT in meta-analyses (Bisson et al., Citation2022; Simon et al., Citation2021). Furthermore, i-tf-CBTs were found to be superior to non-trauma-focused internet-based cognitive behavioural stress management therapy in adults with PTSD in one study (Ehlers et al., Citation2023). They are meanwhile included in the treatment guidelines from the International Society for Traumatic Stress Studies (ISTSS Guidelines Committee, Citation2019). However, such treatment recommendations are lacking for youth. Meanwhile, a systematic review on IMIs for youth experiencing trauma identified only six studies of those four were Randomized Controlled Trials (RCTs) and none evaluated a trauma-focused IMI for youth with clinically relevant PTSS (Schulte, Harrer, et al., Citation2024). The meta-analytic results furthermore did not provide conclusive support for the overall efficacy of IMIs in addressing youth PTSS, as only small within-group effects but no between-group effects were found (Schulte, Harrer, et al., Citation2024). Given the limited evidence on efficacy and uncertainty about how an IMI for youth should be designed, it is crucial to first test the feasibility of a trauma-focused IMI in a proof-of-concept study, before moving on to a RCT.
1.1. Objectives
This one-arm proof-of-concept study investigated the feasibility of a trauma-focused IMI with therapist guidance for youth aged 15–21 years with clinically relevant PTSS (score ≥ 21 on the Child and Adolescent Trauma Screen; CATS; Sachser et al., Citation2022). It aimed to evaluate different feasibility dimensions based on a formal feasibility framework to inform the decision on whether to conduct a subsequent large-scale RCT (Orsmond & Cohn, Citation2015).
2. Methods
2.1. Trial design
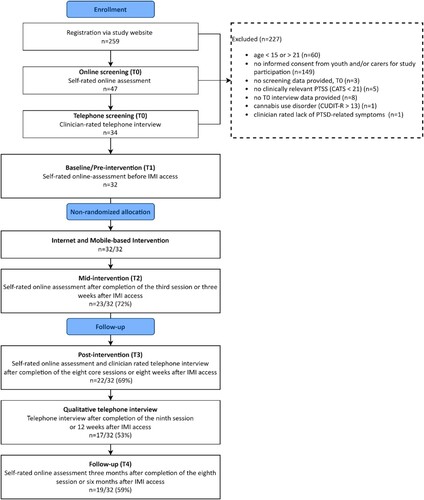
The study was conducted with a total sample of 32 participants. Self-rated online assessments took place at screening (T0), baseline/pre-intervention (T1), mid-intervention (T2), post-intervention (T3), and follow-up (T4) via the survey tool Limesurvey (Limesurvey GmbH., Citation2020). Clinician-rated telephone assessments were conducted at T0 and T3 (). The study reporting follows the CONSORT guidelines for randomized pilot and feasibility trials and the complementary recommendations for reporting non-randomized pilot and feasibility studies (Eldridge et al., Citation2016; Lancaster & Thabane, Citation2019). This study was preregistered (GCTR, DRKS00023341), ethically approved (Ethics Committee of the German Psychological Society, EbertDavidDaniel2020-09-16-VA), and the study protocol was published (Schulte et al., Citation2022). This work is part of the collaborative BestForCan project, which aims at disseminating the TF-CBT developed by Cohen and colleagues (Cohen et al., Citation2009) for children, adolescents, and young adults after child abuse and neglect (Rosner, Barke, et al., Citation2020) funded by the Federal Ministry of Education and Research (BMBF) under Grant (number 01KR1804).
Figure 1. Study flow.
Note. CATS = Child and Adolescent Trauma Screen, Sachser et al., Citation2022, CUDIT-R = Cannabis Use Disorder Identification Test-Revised, Adamson et al., Citation2010, IMI = Internet-and mobile-based intervention. PTSD = Posttraumatic Stress Disorder, PTSS = Posttraumatic Stress Symptoms.
2.2. Participants and procedure
We included youth aged 15–21 years with clinically relevant PTSS (CATS-score ≥ 21; Sachser et al., Citation2022). We chose this age range to include youth in the transitional phase aligning with German healthcare practices, where youth up to the age of 21 can receive treatment from child therapists. The diagnosis of a clinical PTSD was assessed with all participants using the Clinician-Administered PTSD Scale for DSM-5 – Child and Adolescent Version (CAPS-CA- 5; Pynoos et al., Citation2015); however, a PTSD diagnosis was not a requirement for inclusion. Participants had to reside in secure living conditions and provide written informed consent (minors required consent from both caregivers or the legal guardian). The study also required access to a laptop/computer with internet connectivity and sufficient German reading and writing skills. We excluded individuals with a history of psychotic disorder or acute psychosis (measured by adapted items from the Diagnostic Interview for Mental Disorders for Children; Kinder-DIPS; Schneider et al., Citation2017), acute suicidality (measured with items adapted from the Self-Injurious Thoughts and Behaviours Interview; SITBI; Nock et al., Citation2007), alcohol use disorder (score > 8 on the Alcohol Use Disorders Identification Test; AUDIT; Saunders et al., Citation1993) or cannabis use disorder (score > 13 on the Cannabis Use Disorder Identification Test-Revised; CUDIT-R > 13; Adamson et al., Citation2010). Further, we excluded youth who recently started or planned to change medication within the next 10 weeks, and those currently receiving psychotherapy or being on a waiting list starting psychotherapy within the next 10 weeks. Individuals with comorbidities beyond these criteria were not excluded.
Interested individuals filled out a contact form on the study webpage (http://hellobetter.de/star-studie/) and subsequently received study information via e-mail. After providing written informed consent via e-mail, study applicants completed an initial online screening and participated in a semi-structured clinical telephone interview conducted by a licensed psychotherapist to assess study eligibility. To be included, applicants had to create a stepped crisis and emergency plan during the telephone interview, including coping skills, the involvement of significant others, and emergency contacts in case of suicidal or non-suicidal self-injurious thoughts or behaviours. Additionally, participants consented to a suicide prevention contract for the study period, agreeing to adhere to the crisis and emergency plan, and refrain from engaging in any suicidal behaviours. After completing the baseline assessment (T1), participants were included in the study and received access to the IMI via an individual link ().
2.3. Trauma-focused internet- and mobile-based intervention
The IMI is based on face-to-face tf-CBT and involves key components of different evidence-based manualized treatments for PTSD, namely psychoeducation, emotion/affect regulation and coping skills, imaginal exposure, cognitive processing and restructuring, and meaning/making (Dorsey et al., Citation2011; Schnyder et al., Citation2015). The IMI comprises three thematic units spread across nine sessions: (1) safety and coping skills, (2) trauma processing, and (3) consolidation/integration. These sessions consist of eight core sessions and one booster session scheduled four weeks after the completion of the core sessions. Trauma processing was conducted by writing a trauma narrative (see for an overview of content of each session). Each session is expected to last between 30 and 60 minutes. Participants are encouraged to complete one session per week, spanning a total of 12 weeks. The sessions consisted of written content accessible via a web browser on an eHealth platform. All sessions included pictures, videos, audio, and three fictional case descriptions together with drop-down sections providing options to read more about specific topics. Additionally, there was a diary function accessible via mobile phone, where participants could reflect on the implementation and usefulness of conducted exercises and plan activities in terms of behavioural activation. The IMI was designed as a self-help intervention. Still, participants were guided through the IMI by an eCoach, a psychologist with a master’s degree in training to become a psychological psychotherapist. The eCoach sent semi-standardized feedback on completed sessions and adherence reminders. Furthermore, youth had the opportunity to schedule a telephone contact with licensed therapists if needed. The IMI is described in detail in the study protocol (Schulte et al., Citation2022).
Table 1. Overview of the session content of the IMI.
2.4. Assessments
Feasibility was assessed based on a formal feasibility framework (Orsmond & Cohn, Citation2015) comprising five different dimensions: (1) recruitment capability and characteristics of the resulting sample; (2) procedures for data collection and outcome measurement; (3) satisfaction and acceptability of the IMI and study procedures; (4) resources and ability to manage and implement the study and the IMI; and (5) participants’ preliminary responses to the IMI, i.e. in terms of symptom severity.
Recruitment capability and sample characteristics. We collected data on recruitment (e.g. number of individuals applying for study participation; source of recruitment) and sociodemographics (e.g. age, gender, residence, education) at T1.
Data collection procedures and outcome measurement. We asked participants to evaluate the data collection procedures using self-developed items related to item comprehensibility, assessment-associated stress, and time required for data collection at T3.
Satisfaction and acceptability. The Client Satisfaction Questionnaire (CSQ; Boß et al., Citation2016) in its version adapted for Internet interventions (CSQ-I; eight items, score range: 8–32; α = .95) was applied to measure treatment satisfaction at T3; scores exceeding 23 indicate high satisfaction (Attkisson & Zwick, Citation1982). The Attitudes towards Psychological Online Interventions Questionnaire (APOI; 16 items; score range: 16–80; Schröder et al., Citation2015) was used to assess intervention acceptability at T1 and T3. Intervention adherence was assessed by the number of completed sessions, and objective user data (e.g. number of logins) from the secure web-based e-health platform. Additionally, self-reported engagement and acceptance were assessed with self-developed items at T3. The acceptability of individual sessions was evaluated with four self-report items after each online session considering its usefulness, feasibility, comprehensibility, and aesthetics. To measure study adherence, we considered the number of completed online assessments (k = 5) and telephone assessments (k = 3). Data on help-seeking was assessed with self-developed items.
Resources and study management abilities. eCoaches documented the time dedicated to eCoaching, e.g. time spent learning the manual or providing feedback. We tracked data on the time spent for clinical interviews and additional support through psychotherapists, e.g. in telephone consultations. We also tracked time and counted the e-mails sent for study administration.
Symptom severity. The CATS-2 DSM-5 scale (20 items; score range: 0–60, α = .81; Sachser et al., Citation2022) was used to assess PTSS at each time point (T1-T4). The 15-item screen for exposure to potentially traumatic events of the CATS was applied to check for traumatic events at T0. Diagnosis of PTSD was assessed with the CAPS-CA-5 by licensed psychotherapists (20-item DSM-5 scale; score range: 0–80; α = .76; Pynoos et al., Citation2015). With the Patient Health Questionnaire (PHQ-9; item 09 was removed resulting in 8 items used; score range: 0–24; α = .73; Kroenke et al., Citation2001), depressive symptoms were assessed at each time point (T1-T4). The Generalized Anxiety Disorder Assessment (GAD-7; 7 items; score range: 0–21; α = .89; Spitzer et al., Citation2006) was used to assess anxiety symptoms at T1-T4. The KIDSCREEN-10-Index (10 items; score range: 0–40; α = .67; Ravens-Sieberer et al., Citation2010) was utilized to measure health-related quality of life at T1-T4. The Child Posttraumatic Cognitions Inventory Short Form (CPTCI-SF; ten items; score range: 10–40; α = .67; McKinnon et al., Citation2016) was employed to assess posttraumatic cognitions at T1 and T3.
Potential risks and negative effects. The Negative Effects Questionnaire (NEQ, Rozental et al., Citation2016) was used to assess the frequency (score range: 0–20), impact (score range: 0–80; α = .68), and attribution (to treatment or other circumstances) of negative effects during the treatment period (T3 and T4). Suicide item 9 of the Beck Depression Inventory-II was used to assess suicidality at T2 and T4 (single item; range: 0–3; BDI II item 09; Hautzinger et al., Citation2006). We systematically assessed other potential negative events and their relationship with intervention participation using a list of self-developed items about (serious) adverse events at each T1-T4.
2.5. Management of negative events
To oversee negative events, predefined potential (Serious) Adverse Events ((S)AEs) were actively monitored throughout the study. A systematic, step-by-step manual outlining procedures for managing (S)AEs was developed and adhered to. Regular reports on all (S)AEs were provided to an independent Data Safety Monitoring Board, which could propose recommendations for their management (details on safety management in Schulte et al., Citation2024; Citation2022).
2.6. Data analysis
All analyses adhered to the guidelines for reporting non-randomized pilot and feasibility studies (Lancaster & Thabane, Citation2019). We report descriptive statistics for all outcomes of the feasibility dimensions at each time point. The evaluation of objective user data and satisfaction with the single sessions of the IMI was based on the intervention completer sample. The primary analyses regarding the preliminary evaluation of participant’s responses to the intervention in terms of i.e. PTSS, depressive and anxiety symptoms, and health-related quality of life were based on per protocol principle, including study completer data. We reported within-group differences between time points (i.e. T1 and T2, T1 and T3, T1 and T4, T3 and T4) using a two-sided t-test for dependent groups. We reported Cohen’s d within-group-effect sizes using the sample standard deviation of the mean difference adjusted by a correction factor as the denominator and their 95% CIs (Hedges & Olkin, Citation1985). To test for reliable improvement and deterioration of PTSS on a single-person level, we calculated the reliable change index (RCI) (Jacobson & Truax, Citation2004) based on study completer data. Besides, we reported the percentage of participants with PTSS scores below the cut-off for probable PTSD at T3 and T4 (≤ 21, CATS, Sachser et al., Citation2022), and the percentage of participants who lost PTSD diagnosis from T1 to T3. Additionally to the primary analysis, we used multivariate mixed effect models for repeated measures (MMRM) to consider dropout (intention-to-treat analysis) and to assess the longitudinal relationship between each preliminary outcome and time (i.e. T1-T4) (Mallinckrodt et al., Citation2008), while using the ‘Kenward-Roger’ method to construct confidence intervals (Kenward & Roger, Citation1997). We estimate effect sizes for MMRM results using the standard deviation of the sample at T1 as the denominator. Analyses were performed using IBM SPSS Statistics (Version 27), and R statistics software (version 4.3.1) (R Core Team, Citation2022). The significance level for all analyses was set to 0.05 and reported p-values are two-sided.
3. Results
3.1. Recruitment capability and sample characteristics
Participants were recruited via online (e.g., social media posts on Facebook, Instagram, and TikTok) and offline (e.g., flyers in schools, clinics, counselling centres, and youth welfare offices) strategies (see ). Between 14 July 2021, and 13 January 2023, a total of 259 individuals applied for study participation. Of the 199 individuals meeting the age criterion and receiving study information (77%, n = 199/259), 41% were minors (41%, n = 82/199) and the remaining were aged between 18 and 21 years (59%, n = 117/199). Overall, only a quarter (25%, n = 50/199) provided informed consent with the majority of them being aged 18–21 (88%, n = 44/50). After a positive screening, 32 individuals with three of them being minor (9%, n = 3/32) received access to the IMI (see reasons for exclusion in ). The recruitment process lasted 18 months yielding an average rate of 1.78 included cases per month. Most participants stated becoming aware of the study through their relatives (28%, n = 9/32) or Instagram (25%, n = 8/32). The most common reason for participation in an IMI study was a preference for self-help (63%, n = 20/32), followed by perceived attractiveness of an IMI (44%, n = 14/32), or overly long waiting times for on-site psychotherapy (41%, n = 13/32) ().
Table 2. Sociodemographic data at baseline.
Most participants were female (87%, n = 28/32) with a mean age of 19.1 years (SD = 1.7, range: 15–21). PTSS severity in the sample was high (CATS: M = 32.63, SD = 5.94, range: 22–44) and the majority fulfilled a PTSD diagnosis (CAPS CA 5: 66%, n = 21/32). Half of the participants never had any prior mental health treatment (50%, n = 16/32) (). The participants experienced, on average, two traumatic events (SD = 1.15, range:1–5), with the most common events being exposure to sexualized violence (63%, n = 20/32), bullying (28%, n = 9/32), family violence (25%, n = 8/25), other stressful events (25%, n = 8/32), sudden death of a loved person (19%, n = 6/32), or a medical event (13%, n = 4/32). The frequency of single potentially traumatic events (CATS) and additional sociodemographic variables are attached in the Appendix.
3.2. Data collection procedures and outcome measurement
Youth providing data at T4 stated that the questions in the online assessments were understandable (84%, n = 16/19) or partly understandable (16%, n = 3/19). Most of them indicated that they had enough time to participate in the assessments (84%, n = 16/19). The self-estimated time commitment for participating in the online assessments was deemed appropriate by most participants (84%, n = 16/19). The dropout rate from the study’s online- and telephone assessments increased over time with 28% at T2, 31% at T3, up to 47% for T4 (). At the designated self-rated online assessments, a minority of individuals had finished the core sessions of the IMI (T3: n = 5/22, 23%; T4: n = 9/19, 47%, see Appendix).
3.3. Satisfaction and acceptability
Satisfaction data was provided by 69% (n = 22/32) of the sample. From those, ninety-one percent of participants (n = 20/22) expressed satisfaction with the intervention, with 86% (n = 19/22) willing to recommend the IMI to a friend in need and 77% (n = 17/22) indicating that the intervention met their needs, resulting in an overall high satisfaction score (M = 26, SD = 5.83, range: 8–32). The IMI was rated as compatible (45%, n = 10/22) or partly compatible (55%, n = 12/22) with daily life and the majority rated the time available for session completion as enough (45%, n = 10/22) or, partly enough (36%, n = 8/22). Only four participants indicated not having had enough time (18%, n = 4/22). The ratings of the individual sessions indicated that youths mostly found them to be useful (M = 95%), understandable (M = 94%), and aesthetically pleasing (M = 94%). The sessions on the trauma narrative were predominantly rated as challenging (M = 80%), whereas the other sessions were considered easily manageable (M = 82%). The participants’ positive attitudes towards IMIs in general were high at T1 (APOI total scale: M = 59.56, SD = 5.56, n = 32) and still high at T3 (APOI total scale: M = 52.91, SD = 9.42, n = 22), but significantly less positive compared to T1 [t(21) = 3.98; p < .001, d = 0.83; 95%-CI = .35–1.33] (see Appendix for descriptive statistics of the APOI subscales).
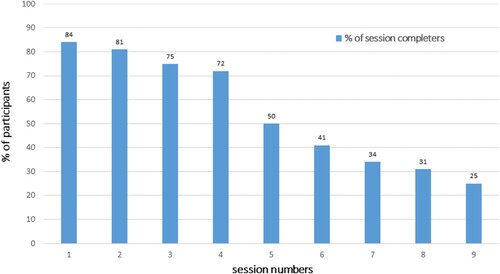
All individuals (100%, n = 32/32) logged into the IMI at least once. However, four of them (13%, n = 4/32) did not proceed to actively engage with the IMI, and one participant (3%, n = 1/32) solely utilized the diary function but never started completing the sessions. Reasons for not starting intervention completion included finding the intervention unhelpful (20%, n = 1/5), lack of motivation and time constraints (20%, n = 1/5), and a broken laptop (20%, n = 1/5). The first stabilization phase of the IMI (1–3) was completed by 75% of participants (n = 24/32). Among the four who discontinued the IMI during the stabilization phase, two reported initiating on-site psychotherapy instead (50%, n = 2/4). Forty-one percent of participants also completed the second phase (4–6), where trauma processing was conducted (41%, n = 13/32). Reasons for discontinuation in the second phase included experiencing symptom remission (10%, n = 1/10), finding the intervention unhelpful or too stressful (20%, n = 2/10), preferring personal contact (10%, n = 1/10), starting on-site psychotherapy (10%, n = 1/10), or external stressors (10%, n = 1/10). The last and third phase (7–8), with consolidation and integration of the traumatic event, was completed by 31% of participants (n = 10/32), whereas reasons for discontinuation were available in two cases describing symptom remission (67%, n = 2/3). All sessions including the ninth booster session were completed by 25% (n = 8/32) ().
Figure 2. Completion rates of IMI sessions in % (n = 32).
Note. Session numbers 1–3 deal with safety and coping skills. Sessions 4–6 deal with trauma processing. Session 7–9 deal with consolidation/integration of the traumatic event(s), with session 9 being a booster-session.
On average, participants logged into the IMI 37.35 times (SD = 29.31, range:4–115, n = 32) and used the intervention for 121 days (SD = 119, range:13–554, n = 32). The diary feature was employed by 21 participants (66%, n = 21/3, M = 27.1, SD = 24.66, range: 1–72, n = 21). Participants received on average 10.25 messages from their eCoach (SD = 5.69, range: 1–22, n = 32), while 22 participants (69%, n = 22/32) actively used the chat function to contact the eCoach (M = 5.82, SD = 5.13, range: 1–21, n = 22). Overall, participants required 43 minutes for session completion (SD = 16).
All participants (100%, n = 32/32) had sought help before study participation, mostly from friends or close relatives (75%, n = 24/32), or parents and family members (56%, n = 18/32). More than half of the sample also sought professional help before study start by psychological counselling centres (59%, n = 19/32) or a therapist (53%, n = 17/32). After participating in the study and the IMI, 73% (n = 16/22) of participants expressed an increased likelihood of seeking general help and 73% (n = 16/22) stated more likely considering on-site psychotherapists in the future.
3.4. Resources and study management abilities
Interviewers spent an average of 2.49 hours at T0 (k = 37, range: 1.5–3.25) and 1.99 hours at T3 (k = 23, range: 1–2.75) conducting interviews. eCoaches took an average of 1.5 hours (range: 1–4) to learn the manual. Each session feedback took approximately 18 minutes (range: 10–25). eCoaches who were already acquainted with eCoaching in general rated the overall effort for guidance as low. Twelve participants (38%, n = 12/32) opted for telephone consultations, totalling 14 clinical consultation sessions lasting 1.7 hours on average (range: 1.25–3), focusing mainly on resource activation and emotion regulation. In total, 7.9 hours of therapeutic resources were acquired per participant, including 4.48 hours for clinical assessments, and 3.44 hours for therapist guidance through the intervention and the study. The study team sent 1569 e-mails to participants, 298 to interviewers, and 170 to eCoaches for study administration and negative effect management, which dedicated approximately 1.5 hours per day (range: 20 minutes to 3 hours).
3.5. Symptom severity
The evaluation of the symptom scores in the study completer sample showed a decrease of PTSS and PTSD severity over all time points (T2-T4, ). Furthermore, depressive symptoms, symptoms of anxiety, and posttraumatic cognitions were lower at post-assessment time points (T3, T4) compared to baseline (T1). Health-related quality of life improved over all time points ().
Table 3. Means and Standard Deviations for participant responses to the IMI for all time points in the study completer sample
In the per-protocol analyses with the study completer sample, significant small to medium effects were observed in PTSS via CATS from T1 to T2 [t(22) = 2.27, p = .033, d = 0.46], large effects from T1 to T3 [t(21) = 4.27, p < .001, d = 0.88] and T1 to T4 [t(18) = 3.83; p = .001; d = 0.84]. Clinician-rated PTSD severity significantly decreased from T1 to T3 [t(21) = 4.52; p < .001; d = 0.93]. There were no significant differences in depressive symptoms from T1 to T2 [t(22) = −0.01, p = .913]. At T3 [t(21) = 3.48; p = .002; d = 0.71] and T4 [t(18) = 2.34; p = .031; d = 0.51], depressive symptoms were significantly lower compared to T1. Symptoms of anxiety did not change significantly from T1 to T2 [t(22) = −1.53; p = .139] and T1 to T3 [t(21) = 1.61; p = .123]. At T4, anxiety symptoms were significantly lower compared to T1 [t(18) = 2.44, p = .025, d = 0.54]. Health-related quality of life did not change significantly from T1 to T2 [t(22) = −0.80; p = .434], but was significantly higher at T3 [t(21) = −2.26; p = .034; d = −0.47] and T4 [t(18) = −2.85; p = .011; d = −0.63] compared to T1. There were no significant differences in any outcome from T3 to T4. Posttraumatic cognitions did not change on a significant level from T1 to T3 [t(df) = 2.07(21); p = .052] ().
Table 4. Participant responses from Pre (T1) to Post-Treatment (T3), Pre-Treatment (T1) to Follow-Up (T4), and Post-Treatment (T3) to Follow-Up (T4) in a per-protocol analysis with study completer data.
Intention-to-treat analysis via MMRM models indicated a significant reduction in PTSS via CATS from T1 to T2 [β = – 3.43; SE = 1.33; t(df) = 2.59(24.33); p = .016], T1 to T3 [β = – 7.44; SE = 1.81; t(df) = 4.12(23.56); p < .005], and T1 to T4 [β = – 7.78; SE = 1.96; t(df) = 3.96(23.96); p < .005], with small to large effect sizes (d = −0.45 to – 1.02). PTSD severity via CAPS-CA-5 was significantly reduced at T3 compared to T1 [β = – 10.08; SE = 2.13; t(df) = 4.74(21.24); p < .001] with large effect size (d = −1.31). Concerning depressive symptoms, MMRM analysis demonstrated a significant reduction from T1 to T3 [β = – 3.01; SE = 0.91; t(df) = 3.29(23.85); p = .003] and T1 to T4 [β = – 2.29; SE = 0.96; t(df) = 2.39(23.45); p = .025] with small effect sizes (d = −0.58 to –0.76). The same pattern was found for health-related quality of life from T1 to T3 [β = 3.81; SE = 1.39; t(df) = 2.74(23.8); p = .011] and T1 to T4 [β = 4.71; SE = 1.31; t(df) = 3.59(22.5); p = .001] with medium effect sizes (d = 0.77–0.95). For symptoms of anxiety, a significant reduction was observed from T1 to T4 [β = –2.48; SE = 0.84; t(df) = 2.95(23.57); p = .007] with medium effect size (d = −0.6) ().
Table 5. Longitudinal relationship between outcomes and time (T1 to T2, T1 to T3, T1 to T4) in a multivariate model repeated measures (MMRM) analysis.
The RCI indicated reliable improvement in PTSS for 32% of cases from T1 to T3 (n = 7/22, 32%), and 37% from T1 to T4 (n = 7/19, 37%). None of the participants showed reliable deterioration of PTSS from T1 to T3 or T1 to T4 according to RCI scores. PTSS scores were below the cut-off (< 21 for probable PTSD) in 41% of cases at T3 (n = 9/22, 41%) and in 63% at T4 (n = 12/22, 63%) (see Appendix eFigure 1, 2, 3 for individual trajectories of PTSS). Regarding PTSD diagnosis, 45% of participants (n = 10/22) no longer met the criteria for PTSD diagnosis at T3.
3.6. Potential risks and negative effects
All participants at T3 (100%, n = 22/22) reported experiencing negative effects during the study, with the most common being the resurfacing of unpleasant memories (77%, n = 17/22), more unpleasant feelings (68%, n = 15/22), increased stress (68%, n = 15/22), and heightened worries (59%, n = 13/22) (see Appendix). Overall, there were 120 instances of negative effects at T3 experienced by participants (M = 6.4, SD = 4.2, range:1–20 per participant), of which 82 (59%) instances (M = 3.7, SD = 3.99, range: 0–18 per participant) were attributed to the IMI. The impact of the negative effects was generally rated as low (M = 13.8; SD = 9.86; range: 1–39, n = 22). In total, six participants reported the presence of suicidal thoughts or behaviours at some time point (19%, n = 6/32). Of those six, three cases at T2 (13%, n = 3/23) and four cases at T4 (21%, n = 4/19) reported thoughts of killing themselves without intent, while one participant (5%, n = 1/19) expressed a desire to do so at T4. Throughout the study, there were 17 incidents of adverse events, including suicidality, in 12 participants (38%, n = 12/32). Four of these 17 incidents were related to the intervention due to elevated symptom burden. There were five incidents of serious adverse events in five participants (15%, n = 5/32), all of them not being related to the intervention. All negative effects were closely monitored according to the safety management concept and forwarded to the Data Safety Monitoring Board.
4. Discussion
This study evaluated the feasibility of a trauma-focused IMI with therapist guidance for youth with clinically relevant PTSS. Recruitment proved successful but time-consuming with over half of the applicants not providing informed consent, and only one in twelve being eligible. The sample, predominantly young women, had an underrepresentation of minors. The majority of participants had experienced interpersonal traumatic events, with elevated PTSS levels and almost two-thirds received a PTSD diagnosis. Data collection procedures were deemed appropriate and half the sample completed all assessments. Each participant required around seven hours of therapeutic resources including eCoaching, mostly for clinical study assessment. Satisfaction with the IMI was high, with online sessions well-accepted. However, the trauma processing sessions were perceived as difficult. A quarter of the participants discontinued treatment at this stage, with reasons including finding the intervention too stressful, starting on-site psychotherapy and symptom remission. Self-rated PTSS significantly decreased from T1 to T3 (d = 0.88) and from T1 to T4 (d = 0.88). Reliable improvement was evident for 37% of cases from T1 to T3 (n = 7/22) and 37% of cases from T1 to T4 (n = 7/19). Clinician-rated PTSD severity significantly decreased from T1 to T3 (d = 0.93) among study completers. Significant improvements with small to large effects were observed post-treatment and at follow-up for all outcomes in the intention-to-treat analysis. Despite experiencing treatment content, some individuals did not benefit from the IMI. Negative effects were observed, the majority of which were primarily linked to the IMI and characterized by resurfacing unpleasant memories and unpleasant feelings. All (S)AEs were promptly addressed, and no clinically significant deterioration in PTSS occurred.
Recruiting via social media enabled the use of precise targeting, potentially contributing to reaching a wider pool of participants, including those who had never received treatment before, as a large proportion of young people use the internet and social media to search for health information (Rideout & Fox, Citation2018). However, limitations of social media recruiting like selection bias and self-selection when solely using social media recruitment should be noted. Therefore, we supplemented our approach with offline recruitment strategies, reaching out to counselling centres, youth clinics, and schools via flyers. Despite high initial study interest, there were few youth who provided informed consent, indicating barriers to youth treatment initiation in this study. Trust issues, fear of negative responses, and questioning the validity of trauma response could be factors that may have impeded personal data disclosure and led to waning interest after reviewing inclusion criteria in the consent form (Truss et al., Citation2022). For minors, reasons such as parental separation or institutional placement leading to difficulties in providing informed consent from both, caretakers or legal guardians, could have posed significant barriers. Furthermore, the sample exhibited elevated symptom strain compared to national and international samples of traumatized children and adolescents, with CATS scores ranging between 25.66 and 30.75, and 54% fulfilling PTSD diagnosis in CAPS-CA DSM 5 (Sachser et al., Citation2022). Yet, the symptom profile resembled those in IMI studies for adults with PTSD, where trauma-focused IMIs have effectively treated individuals with interpersonal and multiple traumas and severe, or even chronic, PTSD (Ehlers et al., Citation2023; Spence et al., Citation2014). Compared to face-to-face tf-CBT for youth, with completion rates ranging from 60% to 90% (Cohen & Mannarino, Citation1998; Peters et al., Citation2021), and therapist-assisted i-tf-CBTs for adults, which showed a mean completion rate of 77% (Simon et al., Citation2021), the completion rate in this study was lower. Over half of the dropouts occurred during the trauma processing phase. This contrasts with findings in i-tf-CBTs for adults, where neither increased dropout rates during trauma processing nor differences between study groups receiving trauma-focused versus non-trauma-focused IMIs were reported (Ehlers et al., Citation2023; Spence et al., Citation2014). Weekly phone calls with a trained tf-CBT therapist in these studies may have strengthened the therapeutic alliance and session engagement commitment. Therapeutic resources for the IMI were considerably lower compared to the recommended resources for face-to-face first-line therapies (NICE, Citation2005), typically involving 8–12 sessions lasting 50–90 minutes each. Required resources in this study were similar to those in i-tf-CBTs for adults, ranging from 2.5 hours (Lewis et al., Citation2017; Spence et al., Citation2014) to half of the ‘usual therapist time’ (Ehlers et al., Citation2023). The effect sizes for the PTSS reduction in the intention-to-treat analysis (d = −1.31, n = 32) are lower compared to those found in a recent study on a i-tf-CBTs for adults with PTSD (d = 2.22, n = 100; Ehlers et al., Citation2023). However, they are comparable to the within-group effects found in a face-to-face tf-CBT feasibility study on youth with interpersonal trauma (d = −0.83, n = 20; Peters et al., Citation2021). This suggests that i-tf-CBT might be effective for young adults, but more research is needed to understand mechanisms of action in the online setting to achieve similar efficacy findings as seen in adults. No comparable studies were found to compare the effect sizes found in the study completer analysis. Some individuals showed a worsening in PTSS symptoms, however, not clinically significant, which was not observed in the findings of IMI studies on adults or, if present, was limited to one up to three cases (Ehlers et al., Citation2023; Lewis et al., Citation2017; Spence et al., Citation2014). Direct comparison to other studies and interpreting negative effects is limited due to scarce research in youth and adults. A single identified study on youth with various mental disorders reported similar findings, indicating that all participants experienced at least one negative effect, with 67% attributing at least one negative effect to psychotherapy (Watson et al., Citation2023). Consistent with our results, the most prevalent negative effects associated with the intervention were unpleasant memories and increased stress (Watson et al., Citation2023), suggesting that these effects might be common effects of psychotherapy rather than specifically relatable to i-tf-CBTs.
4.1. Limitations
Several limitations should be considered when interpreting the study findings. First, selection bias might have occurred due to the requirement for minors to obtain informed consent from both legal guardians, possibly resulting in an underrepresentation of underage participants and potentially affecting the generalizability of the results to younger samples. Moreover, the chosen recruitment strategy might have led to a predominantly young adult, female sample with interpersonal traumatic experiences, which further limits the generalizability of the findings. Second, as a feasibility study without a control group and randomization, the results of participant responses are preliminary, and no conclusions can be drawn on the efficacy of the IMI. Furthermore, the dropout rates for study assessments must be considered when interpreting the findings. Satisfaction scores were obtained from study completers and were not imputed, potentially introducing attrition bias. Third, we utilized one single item to assess suicidality, which is not recommended for safety management procedures (Schulte & Sextl-Plötz, et al., Citation2024) and our safety management did not include symptom deterioration, although representing a possible negative effect of an intervention (Rozental et al., Citation2014). Fourth, the assessors conducting the interviews at post-assessment were not masked to treatment allocation due to the nature of the study. Further, in some cases, the assessors were involved in the intervention progress as they conducted therapeutic telephone consultations during intervention participation. Fifthly, our study lacks a clear definition of feasibility thresholds in the form of progression criteria to proceed with an RCT. While there is development of traffic light systems to guide feasibility studies, clear evidence-based thresholds for feasibility criteria have yet to be established (Herbert et al., Citation2019).
4.2. Future research
Future research should enhance accessibility to study participation, particularly for minors. Introducing more youth-friendly communication options, such as secure data-based chat programmes, could facilitate addressing concerns related to data security, trauma exposure, or consent issues from legal guardians. Besides, exploring participation possibilities for minors without requiring consent from legal guardians, while considering data security and ethical considerations, seems to be crucial. In some cases, an offending parent might still retain the right of custody, so the likelihood of potential participants having the offending caregiver sign the consent form will be close to zero. Tailoring recruitment strategies, to better engage youth with accidental or single trauma, could involve targeting settings like hospitals or law enforcement departments. In adults, trauma-focused treatment is recommended as the preferred choice in digital interventions, as it proves superior to non-trauma-focused approaches (Ehlers et al., Citation2023). Exploring whether and how the specific effects of trauma-focused interventions can be achieved in youth should be the focus of future research. In the first step, the key components contributing to symptom improvement should be identified. Therefore, future research should rigorously measure PTSS to inform a more targeted intervention approach. Further, strategies to enhance adherence, such as facilitating access to the IMI via a smartphone app, shortening the length of the sessions, rearranging the session sequence and starting with exposure early on, as well as expanding therapeutic guidance through scheduled calls or video sessions to promote commitment in engagement, should be investigated. Young individuals facing challenges in completing the IMI sessions may benefit from a stepped-care approach, beginning with a low-threshold IMI as the initial step and progressing to more intensive interventions as needed, such as referral to face-to-face therapy. Blended approaches might be particularly promising for youth uncomfortable working on trauma independently. For efficacy evaluation, conducting an RCT is pivotal. Regarding negative effects, future research should focus on distinguishing between those due to treatment and those inherent in the treatment process (Watson et al., Citation2023). Negative experiences may result in premature discontinuation and render therapy unhelpful for some individuals. Conversely, one study provides initial evidence that others may perceive these experiences as integral to the therapeutic process and recovery (Watson et al., Citation2023). Subsequent studies should explore whether negative effects truly bear negative implications, enabling researchers to inform participants comprehensively about the short- and long-term consequences of such experiences. Furthermore, the safety management concept should be expanded on procedures for dealing with symptom deterioration or absence of change. Finally, future pilot studies should define formal progression criteria, for instance, akin to a traffic light system (Avery et al., Citation2017). This predefined system enables to identify feasibility dimensions to be adapted before moving on to a subsequent trial (orange) as well as dimensions clearly rejecting trial progression (red) more quickly and objectively (Avery et al., Citation2017; Herbert et al., Citation2019).
4.3. Conclusion
This study is the first to investigate the feasibility of a trauma-focused IMI with therapist guidance for youth with PTSD, making a significant contribution to the literature on empirically tested IMIs for youth with PTSD. The study found feasibility in recruitment, data collection, and safety. The IMIs online session were deemed useful, aesthetically pleasing, and comprehensible by those who completed them. However, a notable number of youths discontinued the intervention. Further investigation into strategies aimed at improving adherence, including expanding therapeutic guidance or rearranging the sequence of online session, is warranted. The results also suggest potential efficacy in PTSS symptom change, underscoring the need for a randomized controlled trial to rigorously evaluate the efficacy of i-tf-CBTs.
Authors’ contributions
CeS drafted the study's original design for the grant application and advised CS and AZ on the design of the intervention. AZ and CS developed and implemented the intervention, conducted the study, and drafted the manuscript. DE is the principal investigator of the study.
Ethics approval and consent to participate
The DGPs approved the research protocol (DGPs, the Society, EbertDavidDaniel2020-09-16-VA). The consent to participate is available in German and was reviewed by the Institutional Review Board. The study is registered in the German Clinical Trial Registry (GCTR, DRKS00023341), Registered on 20 July 2021, https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00023341.
StOP_Revision_Appendix_2024_04_12.docx
Download MS Word (441.4 KB)Disclosure statement
Christina Schulte (CS), Cedric Sachser (CeS), and Rita Rosner (RR) have nothing to disclose. David Daniel Ebert (DE) reports receiving fees from Get.On Institute, personal fees from Sanofi, personal fees from Novartis, personal fees from Minddistrict, personal fees from Lantern, personal fees from Schoen Kliniken, personal fees from Ideamed, grants from EU H2020, grants from BMBF, outside the submitted work; and Dr. Ebert has served as a consultant to/on the scientific advisory boards of Sanofi, Novartis, Minddistrict, Lantern, Schoen Kliniken, Ideamed and German health insurance companies (BARMER, Techniker Krankenkasse) and several federal chambers for psychotherapy. He is also a stakeholder in the Institute for Health Training Online (formerly GET.ON, now HelloBetter), which aims to implement scientific findings related to digital health interventions into routine care. HelloBetter distributes the Internet platform for the digital intervention under study. Anna-Carlotta Zarski (AZ) reports to have received fees for lectures or workshops and for expert videos for an internet-based intervention for sexual dysfunctions.
Data availability statement
The data that support the findings of this study are available from the corresponding author, [ChS], upon request.
Additional information
Funding
References
- Adamson, S. J., Kay-Lambkin, F. J., Baker, A. L., Lewin, T. J., Thornton, L., Kelly, B. J., & Sellman, J. D. (2010). An improved brief measure of cannabis misuse: The Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug and Alcohol Dependence, 110(1–2), 137–143. https://doi.org/10.1016/j.drugalcdep.2010.02.017
- Attkisson, C. C., & Zwick, R. (1982). The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning, 5(3), 233–237. https://doi.org/10.1016/0149-7189(82)90074-X
- Avery, K. N. L., Williamson, P. R., Gamble, C., Francischetto, E. O., Metcalfe, C., Davidson, P., Williams, H., & Blazeby, J. M. (2017). Informing efficient randomised controlled trials: Exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open, 7(2), e013537. https://doi.org/10.1136/bmjopen-2016-013537
- Bisson, J. I., Ariti, C., Cullen, K., Kitchiner, N., Lewis, C., Roberts, N. P., Simon, N., Smallman, K., Addison, K., Bell, V., Brookes-Howell, L., Cosgrove, S., Ehlers, A., Fitzsimmons, D., Foscarini-Craggs, P., Harris, S. R. S., Kelson, M., Lovell, K., McKenna, M., … Williams-Thomas, R. (2022). Guided, internet based, cognitive behavioural therapy for post-traumatic stress disorder: Pragmatic, multicentre, randomised controlled non-inferiority trial (RAPID). BMJ, 377, e069405. https://doi.org/10.1136/bmj-2021-069405
- Boß, L., Lehr, D., Reis, D., Vis, C., Riper, H., Berking, M., & Ebert, D. D. (2016). Reliability and validity of assessing user satisfaction with web-based health interventions. Journal of Medical Internet Research, 18(8), e234. https://doi.org/10.2196/jmir.5952
- Boulos, K. M. N., Brewer, A. C., Karimkhani, C., Buller, D. B., & Dellavalle, R. P. (2014). Mobile medical and health apps: State of the art, concerns, regulatory control and certification. Online Journal of Public Health Informatics, 5(3), 229. https://doi.org/10.5210/ojphi.v5i3.4814
- Bundes Psychotherapeuten Kammer. (2018). Ein Jahr nach der Reform der Psychotherapie-Richtlinie – Wartezeiten 2018. Studie - Ein Jahr nach der Reform der Psychotherapie-Richtlinie. https://api.bptk.de/uploads/20180411_bptk_studie_wartezeiten_2018_c0ab16b390.pdf.
- Chen, L. P., Murad, M. H., Paras, M. L., Colbenson, K. M., Sattler, A. L., Goranson, E. N., Elamin, M. B., Seime, R. J., Shinozaki, G., Prokop, L. J., & Zirakzadeh, A. (2010). Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clinic Proceedings, 85(7), 618–629. https://doi.org/10.4065/mcp.2009.0583
- Cohen, J. A., & Mannarino, A. P. (1998). Interventions for sexually abused children: Initial treatment outcome findings. Child Maltreatment, 3(1), 17–26. https://doi.org/10.1177/1077559598003001002
- Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2009). Traumafokussierte kognitive Verhaltenstherapie bei Kindern und Jugendlichen. Springer-Medizin-Verl.
- Dorsey, S., Briggs, E. C., & Woods, B. A. (2011). Cognitive-Behavioral treatment for posttraumatic stress disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 20(2), 255–269. https://doi.org/10.1016/j.chc.2011.01.006
- Ebert, D. D., Zarski, A. C., Christensen, H., Stikkelbroek, Y., Cuijpers, P., Berking, M., & Riper, H. (2015). Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. https://doi.org/10.1371/journal.pone.0119895.
- Ehlers, A., Wild, J., Warnock-Parkes, E., Grey, N., Murray, H., Kerr, A., Rozental, A., Thew, G., Janecka, M., Beierl, E. T., Tsiachristas, A., Perera-Salazar, R., Andersson, G., & Clark, D. M. (2023). Therapist-assisted online psychological therapies differing in trauma focus for post-traumatic stress disorder (STOP-PTSD): A UK-based, single-blind, randomised controlled trial. The Lancet Psychiatry, 10(8), 608–622. https://doi.org/10.1016/S2215-0366(23)00181-5
- Eldridge, S. M., Chan, C. L., Campbell, M. J., Bond, C. M., Hopewell, S., Thabane, L., Lancaster, G. A., Altman, D., Bretz, F., Campbell, M., Cobo, E., Craig, P., Davidson, P., Groves, T., Gumedze, F., Hewison, J., Hirst, A., Hoddinott, P., Lamb, S. E., … Tugwell, P. (2016). CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. The BMJ, 355, i5239. https://doi.org/10.1136/bmj.i5239
- Ellinghaus, C., Truss, K., Liao Siling, J., Phillips, L., Eastwood, O., Medrano, C., & Bendall, S. (2021). „I’m tired of being pulled from pillar to post”: A qualitative analysis of barriers to mental health care for trauma-exposed young people. Early Intervention in Psychiatry, 15(1), 113–122. https://doi.org/10.1111/eip.12919
- Grist, R., Croker, A., Denne, M., & Stallard, P. (2019). Technology delivered interventions for depression and anxiety in children and adolescents: A systematic review and meta-analysis. Clinical Child and Family Psychology Review, 22(2), 147–171. https://doi.org/10.1007/s10567-018-0271-8
- Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), 1–9. https://doi.org/10.1186/1471-244X-10-113
- Hautzinger, M., Keller, F., & Kühner, C. (2006). Beck depressions-inventar (BDI-II).
- Hedges, L., & Olkin, I. (1985). Statistical methods for meta-analysis. Academic Press. https://books.google.com/books?hl=de&lr=&id=7GviBQAAQBAJ&oi=fnd&pg=PP1&dq=Statistical+Methods+for+Meta-Analysis&ots=DxSSuP55dD&sig=ODipKj-0SLpVkPh5ZDZ4B4WzTe0.
- Herbert, E., Julious, S. A., & Goodacre, S. (2019). Progression criteria in trials with an internal pilot: An audit of publicly funded randomised controlled trials. Trials, 20(1), 493. https://doi.org/10.1186/s13063-019-3578-y
- ISTSS Guidelines Committee. (2019). ISTSS PTSD prevention and treatment guidelines methodology and recommendations.
- Jacobson, N. S., & Truax, P. (2004). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. In Methodological issues & strategies in clinical research (S. 631–648). American Psychological Association. https://doi.org/10.1037/10109-042.
- Kenward, M. G., & Roger, J. H. (1997). Small sample inference for fixed effects from restricted maximum likelihood. Biometrics, 53(3), 983–997. https://doi.org/10.2307/2533558
- Kooij, L. H., van der Pol, T. M., Daams, J. G., Hein, I. M., & Lindauer, R. J. L. (2022). Common elements of evidence-based trauma therapy for children and adolescents. European Journal of Psychotraumatology, 13(1), 2079845. https://doi.org/10.1080/20008198.2022.2079845
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- Lancaster, G. A., & Thabane, L. (2019). Guidelines for reporting non-randomised pilot and feasibility studies. Pilot and Feasibility Studies, 5(1), 114. https://doi.org/10.1186/s40814-019-0499-1
- Lethbridge, R., & Australia, P. (2020). Australian guidelines for the treatment of acute stress disorder, posttraumatic stress disorder, and complex PTSD. https://files.magicapp.org/guideline/d3e9d012-66ed-471d-9794-dd94eb90e631/published_guideline_4120-3_0.pdf.
- Lewis, C., Farewell, D., Groves, V., Kitchiner, N. J., Roberts, N. P., Vick, T., & Bisson, J. I. (2017). Internet-based guided self-help for posttraumatic stress disorder (PTSD): Randomized controlled trial. Depression and Anxiety, 34(6), 555–565. https://doi.org/10.1002/da.22645
- Limesurvey GmbH. (2020). LimeSurvey: An open source survey tool (version 5.4.11) [Software]. http://www.limesurvey.org siehe https://community.limesurvey.org/licence-trademark.
- Mallinckrodt, C. H., Lane, P. W., Schnell, D., Peng, Y., & Mancuso, J. P. (2008). Recommendations for the primary analysis of continuous endpoints in longitudinal clinical trials. Drug Information Journal : DIJ / Drug Information Association, 42(4), 303–319. https://doi.org/10.1177/009286150804200402
- Mavranezouli, I., Megnin-Viggars, O., Daly, C., Dias, S., Stockton, S., Meiser-Stedman, R., Trickey, D., & Pilling, S. (2020). Research review: Psychological and psychosocial treatments for children and young people with post-traumatic stress disorder: A network meta-analysis. Journal of Child Psychology and Psychiatry, 61(1), 18–29. https://doi.org/10.1111/jcpp.13094
- McKinnon, A., Smith, P., Bryant, R., Salmon, K., Yule, W., Dalgleish, T., Dixon, C., Nixon, R. D. V., & Meister-Stedman, R. (2016). An update on the clinical utility of the children’s posttraumatic cognitions inventory. Journal of Traumatic Stress, https://doi.org/10.1002/jts.22096
- Müller, M., Klewer, J., & Karutz, H. (2019). Ambulante psychotherapeutische Versorgungssituation von traumatisierten Kindern und Jugendlichen in Deutschland. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie, 47(4), 314–322. https://doi.org/10.1024/1422-4917/a000580
- NICE. (2005). The management of PTSD in adults and children in primary and secondary care. In National Clinical Practice Guideline Number 26. National Clinical Practice Guidelines Number 26: Gaskell and the British Psychological Society. https://ci.nii.ac.jp/naid/20001012650/.
- Nock, M. K., Holmberg, E. B., Photos, V. I., & Michel, B. D. (2007). Self-Injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. https://doi.org/10.1037/1040-3590.19.3.309
- Orsmond, G. I., & Cohn, E. S. (2015). The distinctive features of a feasibility study: Objectives and guiding questions. OTJR Occupation, Participation and Health, 35(3), 169–177. https://doi.org/10.1177/1539449215578649
- Peters, W., Rice, S., Cohen, J., Murray, L., Schley, C., Alvarez-Jimenez, M., & Bendall, S. (2021). Trauma-focused cognitive–behavioral therapy (TF-CBT) for interpersonal trauma in transitional-aged youth. Psychological Trauma: Theory, Research, Practice, and Policy, 13(3), 313–321. https://doi.org/10.1037/tra0001016
- Pynoos, R. S., Weathers, F. W., Steinberg, A. M., Marx, B. P., Layne, C. M., Kaloupek, D. G., Schnurr, P. P., Keane, T. M., Blake, D. D., Newman, E., Nader, K. O., & Kriegler, J. A. (2015). Clinician-Administered PTSD Scale for DSM-5—Child/Adolescent Version. In Ptsd.va.gov.
- R Core Team. (2022). R: A language and environment for statistical computing. [Software]. R Foundation for Statistical Computing. https://www.R-project.org/.
- Ravens-Sieberer, U., Erhart, M., Rajmil, L., Herdman, M., Auquier, P., Bruil, J., Power, M., Duer, W., Abel, T., Czemy, L., Mazur, J., Czimbalmos, A., Tountas, Y., Hagquist, C., & Kilroe, J. (2010). Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Quality of Life Research, 19(10), 1487–1500. https://doi.org/10.1007/s11136-010-9706-5
- Rideout, V., & Fox, S. (2018). Digital health practices, social media use, and mental well-being Among teens and young adults in the U.S. A National Survey Sponsored by Hopelab and Well Being Trust. https://assets.hopelab.org/wp-content/uploads/2020/08/a-national-survey-by-hopelab-and-well-being-trust-2018.pdf.
- Rosner, R., Barke, A., Albrecht, B., Christiansen, H., Ebert, D. D., Lechner-Meichsner, F., Muche, R., Zarski, A. C., & Steil, R. (2020). BEST FOR CAN–bringing empirically supported treatments to children and adolescents after child abuse and neglect: Study protocol. European Journal of Psychotraumatology, 11(1), 1837531. https://doi.org/10.1080/20008198.2020.1837531
- Rosner, R., Gutermann, J., Landolt, M. A., Plener, P., & Steil, R. (2020). Die neue S3-Leitlinie Posttraumatische Belastungsstörung (PTBS). Trauma & Gewalt, 14(2), 132–142. https://doi.org/10.21706/tg-14-2-132
- Rozental, A., Andersson, G., Boettcher, J., Ebert, D. D., Cuijpers, P., Knaevelsrud, C., Ljótsson, B., Kaldo, V., Titov, N., & Carlbring, P. (2014). Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interventions, 1(1), 12–19. https://doi.org/10.1016/j.invent.2014.02.001
- Rozental, A., Kottorp, A., Boettcher, J., Andersson, G., & Carlbring, P. (2016). Negative effects of psychological treatments: An exploratory factor analysis of the negative effects questionnaire for monitoring and reporting adverse and unwanted events. PLoS One, 11(6), e0157503. https://doi.org/10.1371/journal.pone.0157503
- Sachser, C., Berliner, L., Risch, E., Rosner, R., Birkeland, M. S., Eilers, R., Hafstad, G. S., Pfeiffer, E., Plener, P. L., & Jensen, T. K. (2022). The child and Adolescent Trauma Screen 2 (CATS-2) – validation of an instrument to measure DSM-5 and ICD-11 PTSD and complex PTSD in children and adolescents. European Journal of Psychotraumatology, 13(2), 2105580. https://doi.org/10.1080/20008066.2022.2105580
- Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
- Schneider, S., Pflug, V., In-Albon, T., & Margraf, J. (2017). Kinder-DIPS Open Access: Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter. In Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum (Nummer December). Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum. https://doi.org/10.13154/rub.101.90.
- Schnurr, P. P. (2017). Focusing on trauma-focused psychotherapy for posttraumatic stress disorder. Current Opinion in Psychology, 14, 56–60. https://doi.org/10.1016/j.copsyc.2016.11.005
- Schnyder, U., Ehlers, A., Elbert, T., Foa, E. B., Gersons, B. P. R., Resick, P. A., Shapiro, F., & Cloitre, M. (2015). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology, 6(1)), https://doi.org/10.3402/ejpt.v6.28186
- Schröder, J., Sautier, L., Kriston, L., Berger, T., Meyer, B., Späth, C., Köther, U., Nestoriuc, Y., Klein, J. P., & Moritz, S. (2015). Development of a questionnaire measuring attitudes towards psychological online interventions-the APOI. Journal of Affective Disorders, 187, 136–141. https://doi.org/10.1016/j.jad.2015.08.044
- Schulte, C., Harrer, M., Sachser, C., Weiss, J., & Zarski, A.-C. (2024a). Internet- and mobile-based psychological interventions for post-traumatic stress symptoms in youth: A systematic review and meta-analysis. Npj Digital Medicine, 7(1), 1–10. https://doi.org/10.1038/s41746-024-01042-7
- Schulte, C., Sextl-Plötz, T., Baumeister, H., Titzler, I., Sander, L. B., Sachser, C., Steubl, L., & Zarski, A.-C. (2024). What to do when the unwanted happens? Negative event management in studies on internet- and mobile-based interventions for youths and adults with two case reports. Internet Interventions, 35, 100710. https://doi.org/10.1016/j.invent.2024.100710
- Schulte, C., Zarski, A.-C., Sachser, C., Rosner, R., & Ebert, D. D. (2022). Internet- and mobile-based trauma-focused intervention for adolescents and young adults with posttraumatic stress disorder: A study protocol of a proof-of-concept feasibility study. European Journal of Psychotraumatology, 13(2), 2101345. https://doi.org/10.1080/20008198.2022.2101345
- Simon, N., Robertson, L., Lewis, C., Roberts, N. P., Bethell, A., Dawson, S., & Bisson, J. I. (2021). Internet-based cognitive and behavioural therapies for post-traumatic stress disorder (PTSD) in adults. The Cochrane Database of Systematic Reviews, 5(5), CD011710. https://doi.org/10.1002/14651858.CD011710.pub3
- Spence, J., Titov, N., Johnston, L., Jones, M. P., Dear, B. F., & Solley, K. (2014). Internet-based trauma-focused cognitive behavioural therapy for PTSD with and without exposure components: A randomised controlled trial. Journal of Affective Disorders, 162, 73–80. https://doi.org/10.1016/j.jad.2014.03.009
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- Thielemann, J. F. B., Kasparik, B., König, J., Unterhitzenberger, J., & Rosner, R. (2022). A systematic review and meta-analysis of trauma-focused cognitive behavioral therapy for children and adolescents. Child Abuse & Neglect, 134, 105899. https://doi.org/10.1016/j.chiabu.2022.105899
- Truss, K., Liao Siling, J., Phillips, L., Eastwood, O., & Bendall, S. (2022). Barriers to young people seeking help for trauma: A qualitative analysis of internet forums. Psychological Trauma : Theory, Research, Practice and Policy, 15, S163–S171. https://doi.org/10.1037/tra0001344
- Vogel, A., Steil, R., Comteße, H., Eilers, R., Renneberg, B., & Rosner, R. (2021). Routineversorgung für Jugendliche und junge Erwachsene mit Posttraumatischer Belastungsstörung nach sexualisierter und physischer Gewalt in Deutschland. Kindheit und Entwicklung, 30(3), 183–191. https://doi.org/10.1026/0942-5403/a000346
- Watson, P. N., Leroux, E., Chowdhury, M., Mehra, K., Henderson, J., Szatmari, P., & Hawke, L. (2023). Unexpressed wishes and unmet needs: A mixed methods study of youth negative experiences in psychotherapy. Journal of Child and Family Studies, 32(2), 424–437. https://doi.org/10.1007/s10826-022-02431-w
- Wu, Y., Fenfen, E., Wang, Y., Xu, M., Liu, S., Zhou, L., Song, G., Shang, X., Yang, C., Yang, K., & Li, X. (2023). Efficacy of internet-based cognitive-behavioral therapy for depression in adolescents: A systematic review and meta-analysis. Internet Interventions, 34, 100673. https://doi.org/10.1016/j.invent.2023.100673
