ABSTRACT
Background: There is room for improvement regarding the treatment of severe post-traumatic stress disorder (PTSD). Intensifying treatment to increase patient retention is a promising development. Objective: The aim of this study was to determine the effectiveness of an intensive trauma-focused treatment programme over 8 days for individuals suffering from severe PTSD. Method: Treatment was provided for 347 PTSD patients (70% women; mean age = 38.32 years, SD = 11.69) and consisted of daily sessions of prolonged exposure and eye movement desensitization and reprocessing (EMDR) therapy (16 sessions in total), physical activity, and psycho-education. All participants had experienced multiple traumas, including sexual abuse (74.4%), and suffered from multiple comorbidities (e.g. 87.5% had a mood disorder). Suicidal ideation was frequent (73.9%). PTSD symptom severity was assessed by both clinician-rated [Clinician Administered PTSD Scale (CAPS)] and self-report [PTSD Symptom Scale Self Report (PSS-SR) and Impact of Event Scale (IES)] inventories. For a subsample (n = 109), follow-up data at 6 months were available. Results: A significant decline in symptom severity was found (e.g. CAPS intention-to-treat sample Cohen’s d = 1.64). At post-treatment, 82.9% showed a clinically meaningful response and 54.9% a loss of diagnosis. Dropout was very low (2.3%). Conclusions: Intensive trauma-focused treatment programmes including prolonged exposure, EMDR therapy, and physical activity can be effective for patients suffering from severe PTSD and are associated with low dropout rates.
Antecedentes: Hay un margen de mejora con respecto al tratamiento del trastorno de estrés postraumático severo (TEPT). Intensificar el tratamiento para aumentar la retención de paciente es un desarrollo prometedor.
Objetivo: Determinar la efectividad de un programa de tratamiento intensivo centrado en trauma durante 8 días para personas que presentan TEPT severo.
Método: Se proporcionó tratamiento a 347 pacientes con TEPT (70,0% mujeres, edad media = 38,32 años, DE = 11,69) y consistió en sesiones diarias de exposición prolongada y terapia EMDR (16 sesiones en total), actividad física, y psico-educación. Todos los participantes habían experimentado múltiples traumas, incluido abuso sexual (74,4%), y padecían múltiples comorbilidades (por ejemplo, 87,5% trastorno anímico). La ideación suicida fue frecuente (73,9%). La gravedad de los síntomas de TEPT fue evaluada tanto por el clínico con inventarios calificados (CAPS) como por auto-reporte (PSS-SR y IES). Para una submuestra (N=109) se dispuso de datos de seguimiento a los seis meses.
Resultados: Se encontró una disminución significativa en la gravedad de los síntomas (por ejemplo, en la muestra CAPS ITT d = 1,64 de Cohen). En el post tratamiento, el 82,9% mostró una respuesta clínicamente significativa y el 54,9% una pérdida del diagnóstico. El abandono fue muy bajo (2,3%).
Conclusiones: Los programas intensivos de tratamientos centrados en trauma, incluido la terapia de exposición prolongada, la terapia EMDR y la actividad física, pueden ser efectivos para los pacientes que sufren de trastorno de estrés postraumático severo y se asocian con bajas tasas de abandono.
背景:对重度创伤后应激障碍(PTSD)的治疗还有待改进。有希望通过加强治疗来增加病人保留率。
目标:确认强化创伤中心治疗方案对重度创伤后应激障碍患者在8天以内的有效性。
方法:为347名PTSD患者(70.0%女性,平均年龄38.32岁,SD = 11.69)提供治疗,包括每天进行的延长暴露和EMDR治疗(总共16次)、体力劳动和心理教育。 所有参与者都经历过多次创伤,包括性虐待(74.4%),并患有多种合并症(例如87.5%有情绪障碍)。 自杀意念频繁出现(73.9%)。 同时使用临床医生评分(CAPS)和自我报告(PSS-SR和IES)的工具评估PTSD症状的严重程度。 六个月后搜集了一个子样本(N = 109)的追踪数据。
结果:症状的严重程度显著下降(例如,CAPS ITT-样本Cohen’s d = 1.64)。治疗后82.9%表现出有临床意义的反应,54.9%不再符合诊断标准。 脱落率非常低(2.3%)。
结论:延长暴露、EMDR治疗和体力活动等强化创伤治疗计划对于患有重度创伤后应激障碍的病人有效,并有较低的脱落率。
1. Introduction
Trauma-focused cognitive behavioural therapy (CBT), such as prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) therapy, have been found to be among the most effective treatments for post-traumatic stress disorder (PTSD) (Gerger et al., Citation2014). International treatment guidelines, such as those published by the International Society for Traumatic Stress Studies (International Society for Traumatic Stress Studies Board of Directors, Citation2012) and the World Health Organization (World Health Organization, Citation2013), recommend these therapies as first line treatments for PTSD.
During the past 10 years, intensive treatments for PTSD have emerged to increase retention and to accommodate more rapid recovery from symptoms of PTSD. For example, Ehlers and her colleagues (Citation2014) compared intensive cognitive therapy, consisting of 18 hours of therapy in a period of 5–7 working days to the same treatment delivered in weekly sessions over 3 months. All 121 clients had been exposed to traumatic events in adulthood. They found that symptom reduction and attrition were equivalent in both groups, in that 73% of the intensive cognitive therapy group and 77% of the standard cognitive therapy group recovered from PTSD, with attrition rates of 3.3% and 3.2%, respectively. Furthermore, another study found that more frequent scheduling of sessions over a shorter duration of time resulted in greater reductions in symptoms during the course of treatment (Gutner, Suvak, Sloan, & Resick, Citation2016). Thus, intensive application of trauma-focused therapy seems to be well tolerated in patients with PTSD, enabling faster symptom reduction with similar, or even better, results, while reducing the risk that patients drop out prematurely.
The question is whether this also holds true for other trauma-focused therapies and for those who have experienced multiple interpersonal traumas, including childhood sexual abuse, veterans, and patients suffering from multiple (severe) comorbidities. Indeed, several studies investigating the feasibility of intensive CBT in these populations have shown positive results regarding the treatment of PTSD (e.g. Hendriks, De Kleine, Broekman, Hendriks, & Van Minnen, Citation2018; Zoellner et al., Citation2017; for a review see Hendriks, De Kleine, Hendriks, & Van Minnen, Citation2016). In a meta-analysis, EMDR was found to be effective for complex trauma (Chen et al., Citation2018) but little is known about the effects of intensive EMDR therapy. A pilot study by Bongaerts, Van Minnen, and De Jongh (Citation2017) assessed the effectiveness of an intensive EMDR treatment programme for seven patients, consisting of 8 days of EMDR administered in morning and afternoon sessions of 90 minutes each, interspersed with physical activity and psycho-education. In this study, individuals meeting the criteria of the proposed diagnosis of complex PTSD (Maercker et al., Citation2013) showed a significant decrease in PTSD symptoms, while no adverse effects, symptom exacerbation, or dropout occurred. More recently, a pilot study investigating the feasibility and preliminary effectiveness of an intensive 5 day inpatient PTSD treatment programme consisting of EMDR, yoga, and supportive components also demonstrated a significant reduction in PTSD symptoms for nine of 11 patients (Zepeda Méndez, Nijdam, Ter Heide, Van Der Aa, & Olff, Citation2018). None of the patients dropped out because of intolerability and no serious harm or adverse events occurred. Taken together, the above studies, although usually with small sample sizes, suggest that established trauma-focused therapies delivered in an intensive format have the potential to be a safe and effective treatment alternative for patients suffering from severe forms of PTSD with multiple comorbidities. It is therefore important to study the effect of these intensive trauma-focused treatments with larger groups of patients.
An important question warranting investigation is whether combining two evidence-based trauma-focused therapies would have an additive effect on short- and long-term outcomes. For instance, in some previous studies exposure-based treatments were combined with cognitive-based therapies (for a meta-analysis, see Watts et al., Citation2013), with good results. This may be particularly true for more complex cases. For example, patients with high levels of dissociation responded significantly better to a treatment programme that included both exposure-based and cognitive-based elements than to either therapy on its own (Resick, Suvak, Johnides, Mitchell, & Iverson, Citation2012). This effect may also hold true for PE and EMDR therapy. Because these therapies are likely to have different underlying working mechanisms (Lee, Taylor, & Drummond, Citation2006), it is conceivable that based upon patients’ personal features, preferences, and diagnostic profile, PE may be better suited to some individuals, whereas EMDR or a combination treatment will be better for others. The present study is, to our knowledge, the first to explore treatment effects when combining EMDR and PE.
Besides the two first line treatments for PTSD, EMDR and PE, research has shown that physical activity could be a promising way to improve treatment outcomes for people with PTSD. For example, a randomized controlled trial in 81 individuals with PTSD showed that the addition of three 30 minutes training sessions per week and a walking programme to usual care resulted in a stronger reduction in PTSD symptoms compared to usual care per se (Rosenbaum, Sherrington, & Tiedemann, Citation2015). In a meta-analysis by, it was found that adding physical activity to usual care for PTSD was more effective than control conditions (Rosenbaum, Vancampfort, Steel, Newby, Ward, & Stubbs, Citation2015).
The purpose of the present study was to extend upon the case series of Bongaerts et al. (Citation2017) on massed EMDR therapy combined with physical activity and psycho-education. Two trauma-focused therapies, PE and EMDR, were combined with psycho-education and physical activity into a single programme and delivered en masse in a brief time period. The effectiveness of this programme was tested on a relatively large patient sample containing individuals suffering from severe PTSD following exposure to multiple traumas, including childhood sexual abuse. It was hypothesized that this treatment programme would be associated with a significant decrease in PTSD symptoms, and that these results would be maintained at 6 month follow-up. In addition, we expected that given the intensive format, the dropout rate would be low.
2. Method
2.1. Participants
The 347 participants (70% women, mean age = 38.32 years, SD = 11.69) were referred by their general practitioner, psychologist, or psychiatrist to the Dutch psychotrauma expertise centre PSYTREC in 2016 for trauma-related problems. Inclusion criteria were: (1) being at least 18 years old, (2) having a diagnosis of PTSD according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR) (APA, Citation2000) as established with the Clinician Administered PTSD Scale (CAPS), (3) having sufficient knowledge of the Dutch language to complete the assessments, (4) never having had a conviction for sexual assault, and (5) no recent suicide attempts (within the past 3 months). All patients receiving treatment at the centre were instructed to complete all measurements used in this study as part of routine outcome measuring. Therefore, those who agreed to participate in this study did not receive any additional compensation.
2.2. Procedure
Patients first entered a diagnostic phase, in which the inclusion and exclusion criteria were checked. The PTSD diagnosis was established using the Dutch version of the CAPS-IV (Blake et al., Citation1995; Dutch version: Hovens, Luinge, & Van Minnen, Citation2005). To measure the severity of PTSD symptoms by self-report, we used the Dutch PTSD Symptom Scale Self Report (PSS-SR) (Foa, Riggs, Dancu, & Rothbaum, Citation1993; Mol et al., Citation2005) and the Dutch Impact of Event Scale (IES) (Horowitz, Wilner, & Alvarez, Citation1979; Van Der Ploeg, Mooren, Kleber, Van Der Velden, & Brom, Citation2004). Patients’ exposure to traumatic events was identified using a self-report version of the modified Interview for Traumatic Events in Childhood (ITEC) (Lobbestael, Arntz, Harkema-Schouten, & Bernstein, Citation2009). Comorbid anxiety and mood disorders, as well as suicidal ideation, were diagnosed using the Mini-International Neuropsychiatric Interview Plus (MINI Plus) (Overbeek, Schruers, & Griez, Citation1999; Sheehan et al., Citation1998). If the inclusion criteria were met, the patient was invited to sign a treatment contract and informed consent for research purposes.
Patients’ information about trauma history and PTSD symptoms was used to develop a personal case conceptualization that included memories of traumatic events fulfilling the DSM-IV Criterion A of PTSD. The most disturbing memories were targeted first. Each day, one specific memory was processed; that is, the memory targeted with PE in the morning session was also targeted with EMDR in the afternoon.
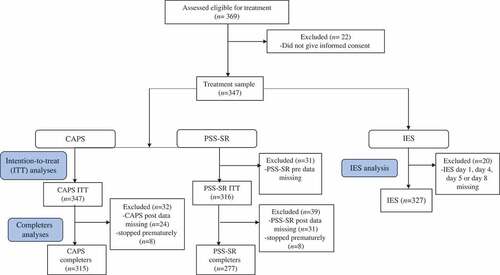
Nine days after the last day of treatment, patients were invited for post-treatment assessment of their PTSD symptoms. For a subsample (n = 109), 6 month follow-up measures were also available. At the beginning of this programme follow-up data were not collected but this became routine after a period of time. The CAPS was administered at the centre or by telephone, as was the PSS-SR. For patient flow, see .
Figure 1. Flow diagram. CAPS, Clinician Administered PTSD Scale; PSS-SR, PTSD Symptom Scale Self Report; IES, Impact of Event Scale; ITT, intention-to-treat.
The study was performed in accordance with the precepts and regulations for research as stated in the Declaration of Helsinki and the Dutch Medical Research on Humans Act (WMO, Citation2001) concerning scientific research. That is, all data were collected using the standard assessment instruments and routine outcome monitoring procedure of PSYTREC, the study lacked random allocation, and no additional ‘physical infringement of the physical and/or psychological integrity of the individual’ was to be expected (World Medical Association, Citation2001).
2.3. Treatment
Treatment consisted of a combination of two manualized evidence-based treatments for PTSD: PE in the morning and EMDR therapy (both 90 minute individual sessions) in the afternoon. Each treatment day, patients’ information about the morning PE session was delivered to the therapist of the afternoon EMDR session in a multidisciplinary meeting. Also, each day, patients were offered four physical activities (each lasting 90 minutes) in a group format, both indoor and outdoor (e.g. walking, badminton, and archery). Patients were invited to participate at their own intensity level. Patients with a physical impairment could also participate in the treatment, and received adjusted physical activities (e.g. table tennis, walking). In the evening, patients attended the psycho-education programme. In sum, patients received 3 hours of individual trauma-focused treatment, 6 hours of physical activity in groups, and 2 hours of group psycho-education per day (for an overview, see ). The treatment was provided over 2 weeks with 4 treatment days in each week. For practical reasons (e.g. travel time), during the treatment days, patients stayed at the clinic. In between these two treatment weeks, patients stayed at home. The treatment programme did not contain a stabilization phase.
Figure 2. Overview of a day in the treatment programme. EMDR, eye movement desensitization and reprocessing; PE, prolonged exposure.
For the PE sessions, a modified version of the PE protocol by Foa, Hembree, and Rothbaum (Citation2007) was used. During the PE sessions, patients were exposed to the memories of the traumatic events, by means of imagining the memories as vividly as possible and describing these in detail, aloud, and in the present tense, for at least 60 minutes. In vivo material that reminded the patient of the traumatic event was incorporated in the PE sessions in accordance with the concept of deepened extinction (for information, see Craske, Treanor, Conway, Zbozinek, & Vervliet, Citation2014). For that purpose, patients were asked to gather material for in vivo exposure, such as trauma-related pictures, sounds, clothing, and perfumes. Because of the intensive treatment format and full day-planning, patients did not receive audio-recordings of their sessions, and no homework assignments were required.
EMDR therapy was delivered according to a manualized, eight-phase EMDR standard (three-pronged) protocol (De Jongh & Ten Broeke, Citation2013; Shapiro, Citation2001). No relaxation or emotion regulation skills training was applied prior to the processing of their memories (for the rationale see De Jongh et al., Citation2016). To avoid confounding of elements of stabilization and trauma-focused therapy, the second phase (i.e. safe place exercise section) was removed from the standard EMDR protocol. In case of anticipatory fear and avoidance behaviour, the ‘flashforward protocol’ (Logie & De Jongh, Citation2014) was applied, during which patients’ most horrible fantasies about the future (e.g. being raped, being attacked, or a psychotic decompensation due to therapy) were targeted. To facilitate processing, cognitive interweaves were applied during processing, as described by the originator (Shapiro, Citation2001, Citation2007). EMDR therapy was implemented with the use of rapid deployment of sets of eye movements offered by fingers or using a light bar. If needed, this was combined with earphones that presented a clicking sound, alternating from the left to the right ear, and/or two pulsators held in each hand that provided alternating bilateral tactile stimulation, all in order to maximize taxation of patients’ working memory (De Jongh, Ernst, Marques, & Hornsveld, Citation2013).
All therapists had a master’s degree in clinical psychology and were trained in PE therapy and EMDR therapy. Therapists were instructed to perform the therapies precisely according to the printed protocols. To prevent protocol drift, sessions were supervised at times. Furthermore, supervisors were also present during the daily multidisciplinary meetings to ensure that the therapies were delivered according to protocol. Psychologists rotated during individual treatment sessions, which means that patients had roughly 12–16 different therapists. The psycho-education during the evening sessions was carried out by trained psychologists. During psycho-education, information about PTSD and the rationale of the various components of the programme were presented, explained, and discussed.
2.4. Assessment instruments
The primary outcome measure was the severity of PTSD symptoms as measured by the CAPS (Dutch version: Hovens et al., Citation2005). This provides ratings of the 17 DSM-IV-TR-based PTSD symptoms on a frequency scale (0–4) and an intensity scale (0–4). For each symptom, a maximum score of 8 can be attained, resulting in a total CAPS score ranging from 0 to 136. To determine a PTSD diagnosis status, the ‘1, 2’ rule was applied; that is, a frequency score of ≥ 1 and an intensity score of ≥ 2 are required for a particular symptom to meet this criterion (Weathers, Keane, & Davidson, Citation2001; Weathers, Ruscio, & Keane, Citation1999). The CAPS has excellent reliability (>.90), yielding consistent scores across items, raters, and testing situations. It provides excellent convergent and discriminant validity (>.90), diagnostic utility, and sensitivity to clinical change (Weathers et al., Citation2001). At post-treatment measurement, the past-week version of the CAPS was used. The CAPS is appropriate for assessment at both 1 month and 1 week intervals, and the scores yielded from both are comparable (Weathers et al., Citation2001).
The Dutch version of the MINI Plus (Overbeek et al., Citation1999; Sheehan et al., Citation1998) was used to assess comorbid anxiety, mood disorders, and suicidal ideation. Therefore, only the sections concerning these disorders and suicidal ideation were administered. The MINI Plus is a structured, well-validated diagnostic interview used to determine DSM-IV and International Classification of Diseases, 10th revision (ICD-10) diagnoses in a systematic way (Van Vliet & De Beurs, Citation2007). The kappa coefficient, sensitivity, and specificity have been found to be good (>.70) to very good (>.80) for most diagnoses. The inter-rater and test–retest reliability also appear to be good (>.70) (Lecrubier et al., Citation1997).
A modified self-report version of the ITEC (Lobbestael et al., Citation2009) was used as an inventory of the trauma characteristics. This includes information about the age of trauma, the offender(s), and the frequency of the traumatic events. For all the subscales, the reliability of the original ITEC appears to be good (Lobbestael et al., Citation2009).
Self-reported PTSD symptoms were measured with the PSS-SR (Foa et al., Citation1993; Dutch translation: Mol et al., Citation2005). The PSS-SR is a 17-item questionnaire used to assess the frequency of the PTSD symptoms using a four-point Likert scale (0–3, total range 0–51) covering three domains: re-experiencing, avoidance, and arousal. It has a satisfactory internal consistency (α > .90) and a high test–retest reliability (r > .70) (Foa et al., Citation1993).
The Dutch IES (Horowitz et al., Citation1979; Van Der Ploeg et al., Citation2004) was used to assess post-traumatic stress symptoms during the course of the treatment programme. According to the authors of the Dutch validation study of the Impact of Event Scale – Revised (IES-R), the original IES was more appropriate than the IES-R (Olde, Kleber, Van Der Hart, & Pop, Citation2006). Therefore, the IES (15-item version) was used. This is a self-report questionnaire that measures trauma-related intrusions and avoidance behaviour. Participants are asked to indicate whether the concerning item is present on a six-point scale, ranging from ‘not at all’ (0), ‘rarely’ (1), and ‘sometimes’ (3) to ‘often’ (5) (total range 0–75). The IES was adapted for the present study to determine the presence of PTSD symptoms that occurred in the previous 24 hours, rather than the past 7 days. The IES was administered every morning of the treatment days.
2.5. Data analyses
Before analyses were performed, the data were screened for data-entry errors and outliers. The extent of missing data was assessed and assumptions for the analyses were checked. All analyses were performed with IBM SPSS Statistics for Windows (version 23). Means, standard deviations, and frequency distributions for demographic and baseline clinical variables were calculated to describe sample characteristics. Person mean imputation was used to impute missing values if missing data did not exceed 10% of the total number of items of a questionnaire (Hawthorne & Elliott, Citation2005). Both the CAPS and the PSS-SR were assessed at baseline, 9 days after the intervention (post-treatment), and at 6 month follow-up. Treatment results as indexed by the CAPS and PSS-SR at pre- and post-treatment were tested using paired sampled t-tests. Analyses were performed both for intention-to-treat (ITT) sample, where last observations were carried forward (LOCF), and for completers. For the IES analysis, we used the scores at day 1 (start of treatment), day 4 (end of first treatment week), day 5 (first day of second treatment week), and day 8 of the treatment (last treatment day). If values were missing, these were imputed with IES scores as measured 1 day before (e.g. day 4 with day 3, and day 8 with day 7) or 1 day after (day 1 with day 2, and day 5 with day 6) to minimize missing data. This resulted in IES data for 327 patients. A repeated measures analysis of variance (ANOVA) using a Huynh–Feldt correction was performed to determine treatment effect during treatment. In a subsample, CAPS (n = 109) and PSS-SR (n = 98), 6 month follow-up data were analysed with repeated measures ANOVA using a Greenhouse–Geisser correction, and repeated contrasts (pre- to post-treatment) and (post-treatment to 6 months). Within effect sizes were calculated using Cohen’s d. Clinically significant symptom change on the CAPS at post-treatment was determined using four categories (i.e. ‘no response’, ‘response’, ‘loss of diagnosis’, and ‘remission’), following the definition of Schnurr and Lunney (Citation2016). To this end, ‘response’ was defined as a reduction on the CAPS of 10 or more points; ‘loss of diagnosis’ as ‘response’ plus no longer having a PTSD diagnosis based on the ‘1, 2’ rule, plus a CAPS severity score of < 45; and ‘remission’ as ‘loss of diagnosis’ plus a CAPS severity score of < 20. In addition, for the purpose of this study, patients who had an increase of 10 points or more on the CAPS were defined as ‘symptom worsening’.
3. Results
3.1. Patient flow and sample characteristics
In total, 347 patients (70% women) were included in this study, with a mean age of 38.3 years (SD = 11.69). Eight of them (2.3%) dropped out before the end of the treatment (see for the flow of the patients). Reasons for dropout were: unwilling to continue (e.g. homesickness, n = 5), being sent home because of inappropriate behaviour (n = 2), and premature PTSD symptom relief (n = 1). Patients’ characteristics are presented in . The treatment sample represented a severe PTSD patient population, indicated by the fact that they had been exposed to a wide variety of multiple traumas, including sexual abuse, the high comorbidity rates (91.2% had one or more comorbidities), that more than a quarter had dissociative symptoms, and that the majority (73.9%) had an elevated suicide risk. In addition, most patients (59.8%) had received trauma-focused treatment before the current treatment, indicating treatment resistance.
Table 1. Characteristics of the treatment sample (n = 347).
3.2. Treatment outcome at post-treatment: CAPS and PSS-SR scores
The means of the pre- and post-treatment data from the CAPS and PSS-SR for the ITT sample and completers are displayed in . For the ITT group, paired sample t-tests showed a significant decrease in CAPS scores [t(346) = 23.87, p = .000] and PSS-SR scores [t(315) = 18.29, p = .000] from pre- to post-treatment, with large effect sizes (all Cohen’s d > 1.3). For the completers, paired sample t-tests showed significant pre–post differences regarding both CAPS [t(314) = 26.15, p = .000] and PSS-SR scores [t(276) = 19.82, p = .000] with large effect sizes (all Cohen’s d > 1.5). The majority (82.9%) showed a clinically meaningful response to treatment, 54.9% of participants showed a loss of diagnosis, and 31.4% were in remission. However, 3.8% showed a clinically meaningful increase in PTSD symptoms.
Table 2. Clinician Administered PTSD Scale (CAPS) and PTSD Symptom Scale Self Report (PSS-SR) scores at pre- and post-treatment in the intention-to-treat (ITT) sample and the completers.
3.3. Course of PTSD symptoms across the 8 days of treatment
Mean IES scores at days 1, 4, 5, and 8 (n = 327) and the standard errors are displayed in . A one-way repeated measures ANOVA showed a significant decrease in IES scores over time [F(2.671,870.722) = 353.792, p = .000, ηp2 = .520]. Repeated contrasts showed significant decreases during the active treatment days in week 1 [day 1 to day 4; F(1,326) = 330.031, p = .000, ηp2 = .503] and week 2 [day 5 to day 8; F(1,326) = 162.771, p = .000, ηp2 = .333] with large effect sizes. During the days when patients were at home (no active treatment days) there was a significant, but very small decline in scores [day 4 to day 5; F(1,326) = 12.955, p = .000, ηp2 = .038], suggesting that decreases in PTSD symptoms were treatment and not time dependent.
3.4. Treatment outcome at 6 month follow-up
For a subsample of 109 completers, 6 month follow-up data were available for explorative analyses. The mean CAPS and PSS-SR total scores for this subsample are shown in . A one-way repeated measures ANOVA performed on the CAPS mean scores at pre- and post-treatment and 6 month follow-up yielded a significant decrease in CAPS scores over time [F(1.90,204.82) = 256.32, p = .000, ηp2 = .70]. Repeated contrasts showed a small, but significant increase in CAPS scores, from post-test to 6 month follow-up [F(1,108) = 8.04, p = .005, ηp2 = .07]. A one-way repeated measures ANOVA performed on the PSS-SR mean scores at pre- and post-treatment and 6 months showed a significant decrease in self-reported PTSD symptoms over time [F(1.86,180.67) = 141.32, p = .000, ηp2 = .59]. Repeated contrasts revealed no significant difference between the post-treatment and 6 month follow-up measurement [F(1,97) = 2.58, p = .111]. Pre-treatment to 6 months follow-up effect sizes were large, and compared to pre-treatment, at 6 month follow-up, 91.7% of the patients showed a clinically meaningful treatment response and 67% a loss of diagnosis, and 33.9% were in remission. However, 1.8% showed a clinically meaningful increase in PTSD symptoms.
Table 3. Clinician Administered PTSD Scale (CAPS) and PTSD Symptom Scale Self Report (PSS-SR) scores at pre-test, post-test and 6 month follow-up (6-FU).
4. Discussion
The results indicate that more than 80% of the patients with severe PTSD and multiple comorbidities showed a clinically meaningful response, while more than half of the patients lost their PTSD diagnosis following 8 days of treatment. These findings are in accordance with a wide array of previous studies on massed treatment showing the feasibility, safety, and effectiveness of such an approach (e.g. Ehlers et al., Citation2014; Hendriks et al., Citation2018, Citation2016; Zepeda Méndez et al., Citation2018; Zoellner et al., Citation2017).
Perhaps the most important advantage of an intensive treatment programme is retention. In the current study, the percentage of dropout (< 3%) is substantially lower than the average number of 22.2% in regular, weekly based trauma-focused treatments (Kline, Cooper, Rytwinsky, & Feeny, Citation2018). Presumably, this low number of dropouts is due to the condensed format of more frequently scheduled sessions delivered in a shorter time frame (Gutner et al., Citation2016), and the fact that the patients within a massed treatment format may have a clear view and perspective as to when treatment ends. Also, the patients stayed in the clinic during the treatment days, so that they did not have to travel, which may have contributed to the low attrition.
To the best of our knowledge, this is the first study to focus specifically on the effectiveness of a combination of EMDR and PE. The combination of EMDR and PE proved to be effective, in line with other studies that found combination treatments to be effective (Watts et al., Citation2013). Thus far, however, the combination of the therapies has only been within the category of CBT (e.g. combination of exposure therapy and cognitive therapy), and perhaps each of these treatment elements may have had more common underlying processes than differences. Given the different working mechanisms of the two treatments under study, PE and EMDR, our findings are intriguing. However, because we did not have a controlled design, it is unclear whether intensive monotherapy (either PE or EMDR) would have resulted in similar positive effects. Also, we do not know to what extent the sequence of the two therapy sessions (in the present study, on each day receiving PE as the first session and EMDR as the second) influenced our results.
Studies have shown non-trauma-specific interventions such as physical activities to be effective in reducing PTSD symptoms (Rosenbaum et al., Citation2015). However, the effect sizes in the current study are very large compared to the medium effect sizes typically found in this area (see meta-analysis by Rosenbaum et al., 2015), suggesting that our study may have had an additional effect that cannot solely be explained by the non-trauma-specific elements. Nevertheless, owing to the design of this study, it is impossible to tease out the unique contribution of the various treatment elements to treatment outcome. Therefore, more controlled dismantling research on this topic is warranted.
The current study has several weaknesses and strengths. The most important limitation of the study is that we did not control for a wide variety of factors that may have been responsible for the decrease in PTSD symptoms, such as time. However, we measured self-report PTSD symptoms on a daily basis and found that PTSD symptoms declined more during treatment days than during the weekend days. This suggests that decreases in PTSD symptoms were treatment and not time dependent. Furthermore, our treatment programme was found to be effective while not containing a stabilization phase. To this end, our results contribute to the current discussion about the necessity of stabilization of patients with severe PTSD due to childhood abuse (De Jongh et al., Citation2016). Yet, it cannot be ruled out that the intensive programme contributed to an environment and activities which go well beyond the psychotherapies. This may be an alternative explanation for the minimal weekend gains, reflecting the moralization provided by the therapeutic milieu and the supportive relationships within it. A further limitation of our study is that we were faced with missing data. Given that the clinic was only recently established, we adapted the process of data gathering during the course of the study. Some measurements were only introduced after some months, resulting in differences in the number of patients per specific measure. For example, we first implemented the CAPS, because this is the gold standard for diagnosing PTSD and an index of symptom severity, and later we added the PSS-SR and IES as self-report measures. These limitations were taken into account during analysis by choosing conservative ways of handling missing data (e.g. person mean imputation, LOCF and ITT). Related to this, we were not able to include more assessment instruments and measures of other disorders or symptoms despite the high level of comorbidity in this study. Future research could study possible mediators and moderators of the treatment effects. In previous studies using subsamples of our presented data, childhood sexual abuse (Wagenmans, Van Minnen, Sleijpen, & De Jongh, Citation2018) and dissociative subtype (Zoet, Wagenmans, Van Minnen, & De Jongh, Citation2018), we were not able to identify any moderators of treatment results, which implies that these patients can benefit from the treatment programme. Another limitation pertains to the quality of our follow-up data, as we could only analyse a subsample for the 6 month follow-up. Therefore, these findings should be interpreted with caution. For example, during the follow-up period, additional treatments as well as exposure to new traumatic events may have occurred. Thus, while the follow-up results are promising, any conclusion about the sustained benefits of this intensive treatment must await a follow-up with a full ITT sample and careful accounting for interim treatment(s). Despite the various limitations, one of the strengths of the present study is the relatively large sample consisting of a broad range of trauma histories, which optimizes the generalizability of the results. In addition, the use of both self-report measurements and a clinician-administered scale allowed us to assess effects according to both the patients and the therapists.
In conclusion, the present study shows that an intensive treatment format combining PE, EMDR, physical activity, and psycho-education is a potentially effective and safe treatment alternative for patients suffering from severe PTSD, complex trauma histories, and multiple comorbidities which can be translated to relative high effect sizes and a favourable retention rate. This means that implementing intensive treatment within mental health-care programmes could increase the likelihood that more people with severe PTSD benefit from treatment for this debilitating condition.
Disclosure statement
C.L. receives fees for providing training in trauma therapies at workshops and conferences. A. v. M. receives income for published book chapters on PTSD and for the training of postdoctoral professionals in prolonged exposure. A. d. J. receives income from published books on EMDR therapy and for the training of postdoctoral professionals in this method.
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
- Blake, D. D., Wheathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., & Keane, T. M. (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–10.
- Bongaerts, H., Van Minnen, A., & De Jongh, A. (2017). Intensive EMDR to treat PTSD patients with severe comorbidity: A case series. Journal of EMDR Practice and Research, 11, 84–95.
- Chen, R., Gillespie, A., Zhao, Y., Xi, Y., Ren, Y., & McLean, L. (2018). The efficacy of eye movement desensitization and reprocessing in children and adults who have experienced complex childhood trauma: A systematic review of randomized controlled trials. Frontiers in Psychology, 9. doi:10.3389/fpsyg.2018.00534
- Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., & Vervliet, B. (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23.
- De Jongh, A., Ernst, R., Marques, L., & Hornsveld, H. (2013). The impact of eye movements and tones on disturbing memories of patients with PTSD and other mental disorders. Journal of Behavior Therapy and Experimental Psychiatry, 44, 447–483.
- De Jongh, A., Resick, P. A., Zoellner, L. A., Van Minnen, A., Lee, C. W., Monson, ... Bicanic, I. A. E. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33, 359–369. doi:10.1002/da.22469
- De Jongh, A., & Ten Broeke, E. (2013). Handboek EMDR: Een geprotocolleerde behandelmethode voor de gevolgen van psychotrauma (Handbook EMDR: A protocolled treatment for the consequences of psychotrauma). Amsterdam: Pearson Assessment and Information B.V.
- Ehlers, A., Hackmann, A., Grey, N., Wild, J., Liness, S., Albert, I., … Clark, D. M. (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry, 171, 294–304.
- Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. New York, NY: Oxford University Press.
- Foa, E. B., Riggs, D. S., Dancu, C. V., & Rothbaum, B. O. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6, 459–473.
- Gerger, H., Munder, T., Gemperli, A., Nüesch, E., Trelle, S., Jüni, P., & Barth, J. (2014). Integrating fragmented evidence by network meta-analysis: Relative effectiveness of psychological interventions for adults with post-traumatic stress disorder. Psychological Medicine, 44, 3151–3164.
- Gutner, C. A., Suvak, M. K., Sloan, D. M., & Resick, P. A. (2016). Does timing matter? Examining the impact of session timing on outcome. Journal of Consulting and Clinical Psychology, 84, 1108–1115.
- Hawthorne, G., & Elliott, P. (2005). Imputing cross-sectional missing data: Comparison of common techniques. Australian and New Zealand Journal of Psychiatry, 39, 583–590.
- Hendriks, L., De Kleine, R., Hendriks, G.-J., & Van Minnen, A. (2016). Intensive cognitive-behavioral treatment of PTSD: An overview of massed outpatient treatment programmes. In C. Martin, V. Preedy, & V. Patel (Eds.). Comprehensive guide to post-traumatic stress disorder. Switzerland: Springer International Publishing.
- Hendriks, L., De Kleine, R. A., Broekman, T. G., Hendriks, G.-J., & Van Minnen, A. (2018). Intensive prolonged exposure therapy for chronic PTSD patients following multiple trauma and multiple treatment attempts. European Journal of Psychotraumatology, 9(1), 1425574.
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218.
- Hovens, H., Luinge, B. A., & Van Minnen, A. (2005). Het Klinisch Interview voor PTSS (KIP) (The Clinician Administered PTSD Scale (CAPS)). Nijmegen: Cure & Care publishers.
- International Society for Traumatic Stress Studies Board of Directors. (2012). The ISTSS expert consensus treatment guidelines for Complex PTSD in adults. Retrieved from: http://www.istss.org.
- Kline, A. C., Cooper, A. A., Rytwinski, N. K., & Feeny, N. C. (2018). Long-term efficacy of psychotherapy for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 59, 30–40.
- Lecrubier, Y., Sheehan, D. V., Weiller, E., Amorim, P., Bonora, I., Harnett Sheehan, K., … Dunbar, G. C. (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12, 224–231.
- Lee, C. W., Taylor, G., & Drummond, P. (2006). The active ingredient in EMDR; is it traditional exposure or dual focus of attention? Clinical Psychology & Psychotherapy, 13, 97–107.
- Lobbestael, J., Arntz, A., Harkema-Schouten, P., & Bernstein, D. (2009). Development and psychometric evaluation of a new assessment method for childhood maltreatment experiences: The interview for traumatic events in childhood (ITEC). Child Abuse & Neglect, 33, 505–517.
- Logie, R., & De Jongh, A. (2014). The ‘Flashforward procedure’: Confronting the catastrophe. Journal of EMDR Practice and Research, 8, 25–32.
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Reed, G. M., Ommeren, M. V., … Saxena, S. (2013). Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. The Lancet, 381, 1683–1685.
- Mol, S. S., Arntz, A., Metsemakers, J. F., Dinant, G. J., Vilters-Van Montfort, P. A., & Knottnerus, J. A. (2005). Symptoms of post-traumatic stress disorder after non-traumatic events: Evidence from an open population study. The British Journal of Psychiatry, 186, 494–499.
- Olde, E., Kleber, R. J., Van Der Hart, O., & Pop, V. J. M. (2006). Childbirth and posttraumatic stress responses: A validation study of the Dutch impact of event scale-revised. European Journal of Psychological Assessment, 22, 259–267.
- Overbeek, T., Schruers, K., & Griez, E. (1999). MINI: Mini International Neuropsychiatric Interview, (Dutch version 5.0. 0). (DSM-IV). Maastricht: University of Maastricht.
- Resick, P. A., Suvak, M. K., Johnides, B. D., Mitchell, K. S., & Iverson, K. M. (2012). The impact of dissociation on PTSD treatment with cognitive processing therapy. Depression and Anxiety, 1–12. doi:10.1002/da.21938
- Rosenbaum, S., Sherrington, C., & Tiedemann, A. (2015). Exercise augmentation compared with usual care for post-traumatic stress disorder: A randomized controlled trial. Acta Psychiatrica Scandinavica, 131(5), 350–359.
- Rosenbaum, S., Vancampfort, D., Steel, Z., Newby, J., Ward, P. B., & Stubbs, B. (2015). Physical activity in the treatment of Post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Research, 230, 130–136.
- Schnurr, P. P., & Lunney, C. A. (2016). Symptom benchmarks of improved quality of life in PTSD. Depression and Anxiety, 33, 247–255.
- Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures (2nd ed.). New York: Guilford Press.
- Shapiro, F. (2007). EMDR, Adaptive information processing, and case conceptualization. Journal of EMDR Practice and Research, 1, 68–87.
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, 22–33.
- Van Der Ploeg, E., Mooren, T. T. M., Kleber, R. J., Van Der Velden, P. G., & Brom, D. (2004). Internal validation of the Dutch version of the Impact of Event Scale. Psychological Assessment, 16, 16–26.
- Van Vliet, I. M., & De Beurs, E. (2007). Het Mini Internationaal Neuropsychiatrisch Interview (MINI), een kort gestructureerd diagnostisch interview voor DSM-IV en ICD-10-stoornissen (The Mini International Neuropsychiatric Interview (MINI), a short structured diagnostic interview for the DSM-IV and ICD-10-disorders). Tijdschrift Voor Psychiatrie, 49, 393–397.
- Wagenmans, A., Van Minnen, A., Sleijpen, M., & De Jong, A. (2018). The impact of childhood sexual abuse on the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology, 9, 1430962.
- Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Beeks, W. B., & Friedman, M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. Journal of Clinical Psychiatry, 74, 541–550.
- Weathers, F. W., Keane, T. M., & Davidson, J. R. (2001). Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety, 13, 132–156.
- Weathers, F. W., Ruscio, A. M., & Keane, T. M. (1999). Psychometric properties of nine scoring rules for the clinician-administered posttraumatic stress disorder scale. Psychological Assessment, 11, 124–133.
- World Health Organization. (2013). Guidelines for the management of conditions that are specifically related to stress. Geneva: WHO.
- World Medical Association. (2001). World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization, 79, 373.
- Zepeda Méndez, M., Nijdam, M. J., Ter Heide, F. J. J., Van Der Aa, N., & Olff, M. (2018). A five-day inpatient EMDR treatment programme for PTSD: Pilot study. European Journal of Psychotraumatology, 9(1), 1425575.
- Zoellner, L. A., Telch, M., Foa, E. B., Farach, F. J., McLean, C. P., Gallop, R., … Gonzalez-Lima, F. (2017). Enhancing extinction learning in posttraumatic stress disorder with brief daily imaginal exposure and methylene blue: A randomized control trial. The Journal of Clinical Psychiatry. doi:10.4088/CJP.16m10936
- Zoet, H., Wagenmans, A., Van Minnen, A., & De Jongh, A. (2018). Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology. doi:10.1080/20008198.2018.1468707