ABSTRACT
Background: Childhood trauma and combat-related trauma are both associated with decreased psychosocial functioning. Coping strategies play an important role in the adjustment to traumatic events.
Objective: The present study examined childhood trauma and the mediating role of coping strategies in adult psychological symptoms in a non-clinical military population after deployment to Afghanistan. Additionally, the moderating role of coping strategies in vulnerability to combat events was explored.
Method: Participants (N = 932) were drawn from a prospective study assessing psychological complaints (SCL-90), early trauma (ETISR-SF), combat-related events and coping strategies (Brief COPE). Mediation analyses via joint significance testing and moderation analyses were performed.
Results: Childhood trauma is related to adult symptoms of general anxiety, depression and problems concerning interpersonal sensitivity through the mediation of self-blame as a coping strategy. Some evidence was found that self-blame moderated vulnerability to combat-related events resulting in psychological complaints, specifically symptoms of anxiety and depression.
Conclusions: Military personnel should be made aware of self-criticizing maladaptive belief systems when dealing with aversive events. Negative beliefs about oneself and distorted trauma-related cognitions may have a basis in childhood events. Self-blame cognitions may be a potential mechanism of change in empirically supported trauma interventions such as cognitive processing therapy.
HIGHLIGHTS
• Childhood trauma is related to adult psychological symptoms.• Self-blame as a coping strategy is a mediator between early trauma and adult. psychological symptoms• Self-criticizing maladaptive belief systems and active coping may be important targets for those exposed to combat.
Antecedentes: el trauma infantil y el trauma relacionado con el combate están asociados a una disminución del funcionamiento psicosocial. Las estrategias de afrontamiento desempeñan un papel importante en la adaptación a los eventos traumáticos.
Objetivo: El presente estudio examinó el trauma infantil y el rol mediador de las estrategias de afrontamiento en los síntomas psicológicos de adultos en una población militar no-clínica luego del despliegue en Afganistán. Adicionalmente, se exploró el rol moderador de las estrategias de afrontamiento en la vulnerabilidad a los eventos de combate.
Método: Los participantes (N = 932) fueron conducidos en un estudio prospectivo que evaluó las quejas psicológicas (SCL-90), el trauma temprano (ETISR-SF), eventos relacionados con el combate y las estrategias de afrontamiento (COPE breve). Se realizaron análisis de mediación mediante pruebas de significación conjunta y análisis de moderación.
Resultados: el trauma infantil se relaciona con síntomas de ansiedad generalizada, depresión y problemas relacionados con la sensibilidad interpersonal en adultos a través de la mediación de los sentimientos de culpa como estrategia de afrontamiento. Se encontró cierta evidencia de que los sentimientos de culpa moderaron la vulnerabilidad a los eventos relacionados con el combate resultando en quejas psicológicas, específicamente síntomas de ansiedad y depresión.
Conclusión: el personal militar debe estar al tanto de los sistemas de creencias desadaptativas autocríticas cuando trata con eventos aversivos. Las creencias negativas sobre uno mismo y las cogniciones distorsionadas relacionadas con el trauma podrían tener una base en eventos de la infancia. Las cogniciones auto-culpabilizantes pueden ser un mecanismo potencial de cambio en las intervenciones traumáticas con apoyo empírico, como la terapia de procesamiento cognitivo.
背景: 童年创伤和与战争有关的创伤都与心理社会功能下降有关。应对策略在创伤事件的适应中发挥着重要作用。
目的: 本研究考查了派遣到阿富汗的非临床军人中儿童创伤和成人心理症状的关系,以及应对的中介作用。此外,还探索了应对战略在战争事件脆弱性方面的调节作用。
方法: 被试(N = 932)一项前瞻性研究,对心理疾病(SCL-90)、早期创伤(ETISR-SF)、战斗相关事件和应对策略(Brief COPE)进行了评估。进行了调节分析和(联合显著性检验)中介分析。
结果: 童年创伤与成人焦虑、抑郁症状和人际敏感问题的有关,自责作为应对策略起了中介作用。一些证据表明,自责调节了与战斗相关的事件的脆弱性,导致心理问题(特别是焦虑和抑郁的症状)。
结论: 军人应注意到在处理负性事件时使用自我批评的适应不良的信念系统。关于自己的负面信念和与创伤相关的扭曲认知可能根源于儿童事件中。自责思维可能是实证支持的创伤干预(如认知加工治疗)的潜在变化机制。
Early traumatic experiences have the capacity to impair adult mental health in perceived well-being, daily activities and psychological distress (Nurius, Green, Logan-Greene, & Borja, Citation2015). In a review study, Passmann Carr, Severi Martins, Stingel, Lemgruber, and Juruena (Citation2013) concluded that childhood trauma can trigger and increase the recurrence of psychiatric disorders. Higher levels of depressive (Spatz Widom, DuMont, & Czaja, Citation2007) and anxiety symptoms are found in non-clinical samples of adults exposed to early life trauma (Chu, Williams, Harris, Bryant, & Gatt, Citation2013) as well as associations with schizotypal, antisocial, borderline and narcissistic personality disorders (Afifi et al., Citation2011). Moreover, several studies have found a graded relationship between the cumulative number of childhood traumatic events and increased health risks for alcohol and substance abuse, depression, adult diseases and suicide attempts later in life (Anda et al., Citation2006; Felitti et al., Citation1998; Min, Minnes, Kim, & Singer, Citation2013; Wu, Schairer, Dellor, & Grella, Citation2010). In clinical samples, the experience of multiple traumas in childhood was found to relate to adult disturbances in affective and interpersonal self-regulatory capacities (Cloitre et al., Citation2009). It is clear childhood trauma can leave its mark on adult life in many ways.
For example, this enduring impact of childhood trauma increases one’s vulnerability to developing psychopathology when adults are exposed to another traumatic event (Brewin, Andrews, & Valentine, Citation2000; McLaughlin, Conron, Koenen, & Gilman, Citation2010). Childhood trauma is also found to contribute to increased risks of anxiety and depression levels, more than adult trauma exposure (Chu et al., Citation2013). In addition, in healthy non-clinical samples, childhood trauma is associated with enduring maladaptive personality traits (Allen & Lauterbach, Citation2007; de Carvalho et al., Citation2015; Rademaker, Vermetten, Geuze, Muilwijk, & Kleber, Citation2008).
Relatively little is known, however, about how childhood trauma affects coping strategies in adults. Coping is defined as a range of cognitive and behavioural responses to manage appraised adversity and stressors (Lazarus & Folkman, Citation1984). Next to personality traits, coping is thought to play a prominent role in the adjustment to stress (Carver & Connor-Smith, Citation2010). Moreover, coping, relative to personality traits, may be modified more easily by interventions. Coping skills are also found to be associated with resilience (Iacoviello & Charney, Citation2014), thus acting on the healthy processing of stress. Several studies have identified coping to be associated with better psychological adjustment while others state the adaptive qualities of coping strategies also depend on the context of the stressor, such as its perceived controllability and severity (Clarke, Citation2006; Compas, Connor-Smith, Saltzman, Harding Thomsen, & Wadsworth, Citation2001; Folkman & Moskowitz, Citation2004; Rodrigues & Renshaw, Citation2010). In relation to traumatic events, disengagement coping strategies such as avoidance, denial and social withdrawal are found to be associated with psychological distress (Littleton, Horsley, John, & Nelson, Citation2007) and post-traumatic stress disorder (PTSD) (e.g. Stein et al., Citation2005). Few studies have examined the interrelationship of childhood trauma, coping strategies and adult psychological symptoms following adult adversities. For example, in a sample of adult female survivors of domestic violence, histories of traumatic events in childhood were related to feelings of guilt, avoidant coping and PTSD symptomatology (Street, Gibson, and Holohan (Citation2005). Yet, little is known about how childhood trauma relates to coping and symptomatology in military personnel.
During deployment, military personnel are often exposed to stress and traumatic events such as combat, injury and witnessing death or suffering. These events potentially cause significant risks of psychiatric diagnoses such as PTSD and other anxiety disorders, depression and substance use disorders (e.g. Hoge et al., Citation2004; Reijnen, Rademaker, Vermetten, & Geuze, Citation2015). Childhood trauma has been shown to play a role in mental health in combat veterans, being associated with adult trauma and increased symptomatology (Clancy et al., Citation2006) predicting mental health symptoms beyond the contribution of combat experiences (Cabrera, Hoge, Bliese, Castro, & Messer, Citation2007). Fritch, Mishkind, Reger, and Gahm (Citation2010) also found significant main effects of childhood physical abuse and combat-related trauma on mental health (anxiety, depression and PTSD) but no interaction between childhood abuse and combat exposure. Recently, research on combat trauma has begun to investigate the effect of coping responses in trauma exposure and mental health (Held, Owens, Schumm, Chard, & Hansel, Citation2011; Stein et al., Citation2005). However, it remains unknown whether early trauma adversely affects the ability to cope effectively with stressors such as deployment in later life.
The present study aims to further explore the mediating role of coping in effects of childhood trauma in a non-clinical military population. We hypothesize that early traumatic experiences are related to psychological symptoms in adult life via the development of specific maladaptive coping strategies. Moreover, we predict that the occurrence of psychological symptoms after experiencing adverse events during military deployment will be moderated by coping strategies.
1. Method
1.1. Participants and procedure
Data for the present study were collected from a non-clinical cohort study (Prospective Research in Stress during Military Operations; Veenman, Vermetten, de Kloet, Unck, & Westenberg, Citation2005) in the Dutch Armed Forces. Dutch military personnel was asked to volunteer and fill out a questionnaire prior to and after a four-month UN deployment to Afghanistan. To maximize the response rate, participants were contacted for a maximum of five times at each assessment by mail, email and telephone. The study was approved by the Instgitutional Review Board of the University Medical Center Utrecht, the Netherlands. Informed consent was provided by all participants. For the present study, 932 males were included. There was a relatively small subgroup of women participants (n= 93, 9%), which were not included in the main analyses due to the lower sample size and hence reduced statistical power. In order to provide information on this subgroup, analyses for the female participants have been provided as additional supplementary materials. The average age of male participants was 28.6 years old (SD = 9.1). For demographics see .
1.2. Measures
The Early Trauma Inventory Self Report – Short Form was used to assess self-reported potential traumatic childhood experiences before the age of 18 years (ETISR-SF; Bremner, Bolus, & Mayer, Citation2007; Bremner, Vermetten, & Mazure, Citation2000). Cronbach’s alphas of the original ETISR-SF range from .70 (General trauma) to .87 (Sexual abuse). It was translated into Dutch for a previous prospective study using the same data (Rademaker et al., Citation2008). The list contains 27 items (being answered with ‘yes’ or ‘no’) and was administered before deployment to Afghanistan. Experiences were divided into four subscales: General trauma (e.g. Were you involved in a serious accident?; Did you experience the death or serious injury of a sibling?), Physical abuse (e.g. Were you ever slapped in the face with an open hand?; Were you ever hit with an object that was thrown at you?), Emotional abuse (e.g. Were you often put down or ridiculed?; Were you often told you were no good?) and Sexual abuse (e.g. Were you ever touched on an intimate or private part of your body in a way that surprised you or made you feel uncomfortable?; Did anyone ever have genital sex with you against your will?). Psychometric properties of the ETISR-SF were explored by computing Cronbach’s alphas for the subscales. Internal consistency on the subscales was acceptable (Physical abuse α = .72; Emotional abuse α = .78; Sexual abuse α = .72) except for General Trauma (α = .51).
To assess specific coping styles in response to general stressors, participants were asked to fill out the Brief COPE (Carver, Citation1997) one year after deployment. Its 28 items result in 14 subscales: Active coping, Planning, Positive reframing, Acceptance, Humour, Religion, Using emotional support, Using instrumental support, Self-distraction, Denial, Venting, Substance use, Behavioural Disengagement and Self-blame. Cronbach’s alphas of the original Brief COPE range from .50 (Venting) to .90 (Substance abuse). In the current study, the internal consistency of the Brief COPE subscales was satisfactory except for Acceptance (α = .47) and Self-blame (α = .39). As the subscale Self-blame turned out to be of importance in our models, we ran analyses for each of the two items separately to further investigate effects.
Psychological symptoms and levels of distress were assessed one year after deployment using the Dutch revised Symptom Checklist, SCL-90-R (Arrindell & Ettema, Citation2003, Derogatis, Lipman, & Covi, Citation1973). This self-report questionnaire is comprised of 90 items that can be divided into eight subscales; General Anxiety, Agoraphobic, Depressive, Somatic Symptoms, Feelings of Insufficiency, Interpersonal Sensitivity and Distrust, Hostility and Sleep Problems. Cronbach’s alphas of the original SCL-90-R range from .90 and .77. In the current study, the internal consistency of the SCL-90 subscales was high, with alpha coefficients ranging from .92 for depressive symptoms to .76 for symptoms of sleep problems.
Combat-related events were assessed one month after deployment using the Deployment Experience Scale (DES; Reijnen et al., Citation2015). This checklist assesses 19 stressful experiences such as ‘Being shot at; Witnessed dead or wounded colleagues; and Experiencing lack of control’ (‘yes’ or ‘no’).
1.3. Analyses
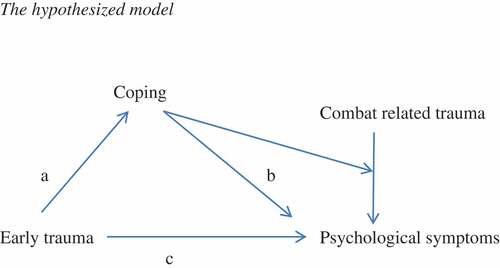
First, we hypothesized that early traumatic experiences are related to the development of psychological symptoms in adult life through the mediating role of specific coping strategies (). The conceptual model is that early traumatic experiences cause maladaptive changes in coping strategies, and these changes cause increases in psychological symptoms. To test our hypothesis we used mediation analyses via joint significance testing, which has been shown to be an appropriate method by MacKinnon, Lockwood, Hoffman, West, and Sheets (Citation2002) and MacKinnon, Fairchild, and Fritz (Citation2007) and has been previously used in clinical psychological studies (e.g. Gladwin et al., Citation2015). In joint significant tests, an independent variable (early trauma) must significantly predict a mediating variable (coping strategy), termed the a-path, which in turn must significantly predict an outcome variable (psychological symptoms) in a model including the independent variable, the b-path.
To deal with the problem of multiple testing we used a strategy in which a series of analysis steps was used, each of which applied Bonferroni correction to control familywise false positive rate for the tests used in that step. In subsequent steps only the variables surviving Bonferroni correction in the previous step were included, thus controlling the false positive rate over the whole analysis. The steps were: (1) F-tests for the c-paths from ETISR-SF subscale scores to each of the eight SCL-90 subscales; (2) for each of the significant SCL-90 subscales from step 1, the a-paths from ETISR-SF subscale scores to each of the 14 Brief COPE subscales; and (3) for all combinations of the significant SCL-90 and Brief COPE subscales from steps 1 and 2, the b-paths from Brief COPE subscales to SCL-90 subscales. Thus, the number of tests for which Bonferroni correction was applied in the first step was 8; in the second step, the number of SCL-90 scales found in the first step times 14; and in the third step, the number of SCL-90 scales found in the first step, 3, times the number of Brief COPE scales found in the second step, 1.
Second, we performed moderation analyses as the occurrence of psychological symptoms was assessed after military deployment and the possible moderating effect of coping strategy on the impact of stressful combat events on the development of psychological symptoms could be analysed ( displays the hypothesized model). We aim to test the idea that the effect of experiencing stressful combat events on symptoms is dependent on individual coping strategies. This thus ties in to and expands the previous mediation model. To do so, the interaction term was tested between combat events and any coping subscale (Brief COPE) found to be a significant mediating variable, within a regression model also containing the coping subscale and early trauma (ETISR-SF) predictors. Significant moderation effects would suggest that early trauma leads to a coping style that makes individuals vulnerable to stressful combat events. Combat stress events were measured as the sum of scores for all items concerning DES.
Finally, the sample contained missing data, which could distort results (Eekhout, de Boer, Twisk, de Vet, & Heymans, Citation2012). Therefore, in addition to the complete case analyses described above, critical tests were also performed using multiple imputation (Eekhout et al., Citation2012; Rubin, Citation1976, Citation1996). These analyses were done in R using the package MICE (van Buuren & Groothuis-Oudshoorn, Citation2011) implementing the method of Multiple Imputation by Chained Equations (Raghunathan, Lepkowski, van Hoewyk, & Solenberger, Citation2001). All variables used in the analyses (all ETISR-SF subscales, all SCL-90 subscales, all Brief COPE subscales and all combat events), as well as age, relationship status, rank and number of deployments, were used for multiple imputation.
2. Results
Of the full sample, 863 subjects filled out the questions on the ETISR-SF (see Supplementary materials ). Eighty-six percent of them had experienced one or more aversive event in childhood, 44% of them had been exposed to one or more forms of physical abuse (n = 381), sexual abuse had been experienced by 6% (n = 50) and 22% of them had been exposed to emotional abuse (n = 184).
Table 1. Demographic characters of participants (male, N = 932).
Mean scores and internal consistency of SCL-90 and Brief COPE are shown in Supplementary materials and . The mean number of experienced combat-related events was 4.54 (SD = 3.27). Of the participants, 65% saw people being shot at. Exposure to human suffering was experienced by 58% of the group. Exposure to dead or wounded colleagues or other persons was experienced by 46%. Forty-two percent reported having been shot at. Complete descriptives concerning combat events are shown in Supplementary materials .
Table 2. Results for the c-path F-test of regressions onto ETISR-SF per SCL-90 subscale.
Table 3. Regression coefficients for the a-path per ETISR-SF-subscale on Self-blame.
Table 4. Results for the b-path on General anxiety.
Regression analyses were used to assess which of the eight subscales of the SCL-90 were significantly related to subscales of the ETISR-SF, which was the criterion for including them in mediation analyses for tests of the a- and b-paths via coping. After Bonferroni correction (α = .05/8 = .0063), symptoms of general anxiety, depression and interpersonal sensitivity were significantly related and continued in the mediation analyses (see ). Depression and interpersonal sensitivity remained significant in the multiple imputation analyses.
In additional exploratory analyses, the separate influence of each ETISR-SF subscale to the development of the three significant SCL-90 symptom clusters was assessed by exploring subscale-specific coefficients. Emotional abuse appeared to play an important role in predicting symptoms of depression (b = .70, t= 2.56, p = .01) and interpersonal sensitivity (b = .72, t = 2.82, p = .005) but not on general anxiety (see Supplementary materials Tables 5, 6 and 7). To illustrate the pairwise relationships between emotional abuse and each of the dependent variables, we present the zero-order correlations in the tables.
Table 5. Results for the b-path on Symptoms of depression.
Table 6. Results for the b-path on Interpersonal sensitivity.
Second, regression analyses were used to assess the effect of ETISR-SF subscales on the development of coping strategies, the a-path of the mediation model (see Supplementary materials Table 8). After Bonferroni correction for multiple comparisons (α = .05/14 = .0036), self-blame as a coping strategy was found to be significantly related to early trauma experiences (R2 = .05, F(4, 459) = 6.47, p < .001), both in complete case and multiple imputation analyses. Also here, some additional exploratory analyses were performed. To assess the unique influence of each ETISR-SF subscale on the development of self-blame, coefficients in the regression model and pairwise correlations were explored. Emotional abuse and sexual abuse appeared to be most important in the development of self-blame (see ).
Finally, the b-path was analysed and corrected for multiple testing by Bonferroni correction (α = .05/3 = .017), with significant results for the self-blame subscale. The results of the regression analyses are given in , and . Early trauma, specifically emotional abuse, was related to the development of symptoms of general anxiety, depression and problems concerning interpersonal sensitivity through self-blame.
As self-blame was found to be a significant mediating variable in our analyses while the Cronbach’s alpha of the subscale had turned out to be poor, we conducted mediation analyses on the two items the subscale consists of. These items were ‘I have been criticizing myself’ and ‘I’ve been blaming myself for things that happened’. For both items, the mediation remained significant for all three selected symptoms (general anxiety, depression and interpersonal sensitivity and distrust). Emotional abuse was a significant predictor (both in terms of unique contribution and pairwise correlations) for both items and all symptoms. Some differences were found for the role of other ETISR-SF subscales (see Supplementary materials Table 9).
Finally, analyses were conducted to test whether self-blame moderates the relationship between combat-related events and symptoms of anxiety, depression or interpersonal sensitivity. To do so, the variables combat-related events and self-blame were centred and an interaction term was calculated as their product. Linear regression was performed with ETISR-SF subscales, combat-related events, self-blame and the interaction term as the predictors, and each of the three SCL-90 subscales anxiety, depression and interpersonal sensitivity as the dependent variable. The interaction effect on anxiety (b = 0.11, t = 3.09, p = .002) and on depression (b = 0.23, t = 3.32, p = .001) were significant, but not the interaction effect on interpersonal sensitivity (b = 0.09, t = 1.35, p= .177). Thus, self-blame was related to vulnerability to combat events: individuals with higher self-blame show a stronger increase in symptoms with combat-related events, specifically symptoms of anxiety and depression (see Supplementary materials Tables 10, 11 and 12). However, in these tests, multiple imputation analyses resulted in only nominally and not Bonferroni-corrected significant results.
3. Discussion
We aimed to explore the mediating role of coping strategies in linking childhood trauma to adult psychological symptoms in male veterans. Further, we investigated the moderating impact of coping strategies on the effects of combat experiences on mental health. First, we found that childhood trauma was related to symptoms of anxiety, depression and interpersonal sensitivity in adult life. This result supports the findings of previous studies about the long-term implications of traumatic childhood experiences on adult well-being (Chu et al., Citation2013; Nurius et al., Citation2015; Passmann Carr et al., Citation2013) and its association with depressive and anxious symptomatology (Sachs-Ericsson, Verona, Joiner, & Preacher, Citation2006). Second, we explored the association between childhood trauma and specific coping strategies in the adult life of military men. Our results showed that early trauma was related to self-blame as a coping strategy in adult life. This result confirms our initial hypothesis on the concurrence of childhood trauma and specific coping strategies. It is also in line with findings on self-criticism as a negative cognitive style that may emerge after parental verbal abuse (Sachs-Ericsson et al., Citation2006). It agrees with studies that posit that emotional abuse is related to self-criticism and low self-esteem (Finzi-Dottan & Karu, Citation2006; Sachs-Ericsson et al., Citation2006) which may lead to self-blaming tendencies (Gibb, Citation2002). Further, in the current study, self-blame was found to be related to symptoms of general anxiety, depression and problems concerning interpersonal sensitivity. In our mediation analyses, self-blame mediated the relationship of early trauma with adult psychological functioning. This is in line with existing literature on self-criticism as a mediator of the relationship between childhood verbal abuse and adult symptoms of depression and anxiety (Liem & Boudewyn, Citation1999; Sachs-Ericsson et al., Citation2006). It also supports recent findings about the role of self-blame in maintaining PTSD (LoSavio, Dillon, & Resick, Citation2017) and the inclusion of distorted trauma-related cognitions and negative beliefs about oneself as a symptom of PTSD in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (Citation2013).
Finally, we explored the moderating role of coping strategies in the development of psychological symptoms after combat exposure. Stressful events experienced during deployment were related to more symptoms of anxiety and depression. As we hypothesized, a trend was found on self-blame affecting vulnerability to combat-related events, making them more likely to cause psychological complaints. This supports studies that propose guilt-related cognitions prohibit an individual from successfully processing traumatic experiences (Held, Owens, Schumm, Chard & Hansel, Citation2011; Street et al., Citation2005).
There are several study limitations. First, whilst the Brief COPE has demonstrated reliability in other samples (Carver, Citation1997; Monzani et al., Citation2015) the internal consistency of the subscale self-blame in our study was poor. One explanation is that the subscale may have been negatively affected by the measurement procedure as prior to the Brief COPE, our participants were asked to fill out questions about which combat-related events they had experienced. Considering the self-blame subscale is asking if one ‘tends to criticize oneself’ and if one ‘is blaming himself for things that have happened’, it may be that respondents replied to the latter item with the combat events in mind instead of overall daily stressors. It is possible that the subscale was not measuring a self-blaming coping tendency but the reflection of the participant on specific combat events. When we further explored the subscale, results remained robust. However, these analyses were limited as they involved only a single item. Second, the drop-out of the second assessment is hard to explain as we were not able to contact those who didn’t respond. Possibly, this was due to lack of interest in continuing participation. On our treatment of missing data, we acknowledge that multiple imputation analyses on moderation resulted in only nominally and not Bonferroni-corrected significant results. This may be related to the likelihood that combat events will arise from different factors than those covered by the available variables. Future research may need to place a particular emphasis on acquiring full data on combat events or use additional variables that do predict risk for such events. Our results do suggest that self-blame plays a moderating role in psychological effects of combat events, and at least provide a strong basis for specific hypotheses in further studies. Third, we did not assess PTSD symptoms. We wanted to avoid a focus on PTSD because the sample was non-clinical and took a broader view of potential negative consequences of trauma on mental health (Nurius et al., Citation2015). Fourth, our data were retrospective and self-reported. Future research could use a semi-structured interview method to assess childhood trauma. This may help to reduce biases of recall and restricted scope and could help to detect the individual severity of the events, which is thought to be a strong predictor of greater symptomatology (Clemmons, Walsh, Dilillo, & Messman-Moore, Citation2007). Finally, we focused on the subgroup of males due to the sample size considerations and because gender effects were not the focus of the current study. This limits our findings to male veterans. Recent findings have suggested that gender differences are limited (Sexton, Raggio, McSweeney, Authier, & Rauch, Citation2017), yet we encourage further examination of this subject. The provided supplementary materials on the female participants may be helpful in this regard. Despite these disadvantages, an important strength of the present study is that we used data from a large prospective non-patient sample which improves generalization to other military populations. Future research should continue to longitudinally assess relationships between trauma, psychological symptoms and coping strategies as well as resiliency factors.
Our findings have clear clinical implications. First, in agreement with previous studies, we find that early trauma sets the stage for mental health symptoms, making prevention and early detection of childhood adversities a priority for child protection service agencies and measurement of early trauma an important component of risk assessment. Second, it should be considered whether, in preparation for deployment, military personnel should be made aware of self-blame cognitions when dealing with aversive events. Active coping skills, cognitive flexibility and maintaining a supportive social network could be cultivated to promote healthy processing and enhance resiliency (Iacoviello & Charney, Citation2014). After deployment, internalizing signals such as guilt, depression, low self-esteem and impoverished social skills (Passmann Carr et al., Citation2013) should not be overlooked. Finally, in the treatment of persistent psychological dysfunction following combat trauma we consider it to be meaningful to target self-blame cognitions, which may have a more profound basis in childhood events. Consistent with recent findings (Holliday, Holder, & Suris, Citation2018; LoSavio et al., Citation2017), we expect self-blame cognitions to be a potential mechanism of change in empirically supported trauma interventions such as cognitive processing therapy.
Supplemental Material
Download Zip (146.8 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplementary data for this article can be accessed here.
Additional information
Funding
References
- Afifi, T. O., Mather, A., Boman, J., Fleisher, W., Enns, M. W., MacMillan, H., & Sareen, J. (2011). Childhood adversity and personality disorders: Results from a nationally representative population-based study. Journal of Psychiatric Research, 45, 814–9.
- Allen, B., & Lauterbach, D. (2007). Personality characteristics of adult survivors of childhood trauma. Journal of Traumatic Stress, 20(4), 587–595.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) (pp. 5–25). Arlington, VA: American Psychiatric Publishing.
- Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., … Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186.
- Arrindell, W. A, & Ettema, J. H. M. (2003). Herziene handleiding bij een multidimensionele psychopathologie indicator [SCL-90: Revised manual for a multidimensional indicator of psychopathology]. Lisse, the Netherlands: Swets & Zeitlinger.
- Bremner, J. D., Bolus, R., & Mayer, E. A. (2007). Psychometric properties of the early trauma inventory self report. Journal of Nervous and Mental Disease, 195(3), 211–218.
- Bremner, J. D., Vermetten, E., & Mazure, C. M. (2000). Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: The early trauma inventory. Depression and Anxiety, 12, 1–12.
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766.
- Cabrera, O. A., Hoge, C. W., Bliese, P. D., Castro, C. A., & Messer, S. C. (2007). Childhood adversity and combat as predictors of depression and posttraumatic stress in deployed troops. American Journal of PreventiveMedicine, 33(2), 77–82.
- Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4, 92–100.
- Carver, C. S., & Connor-Smith, J. (2010). Personality and coping. Annual Review of Psychology, 61, 679–704.
- Chu, D. A., Williams, L. M., Harris, A. W. F., Bryant, R. A., & Gatt, J. M. (2013). Early life trauma predicts self-reported levels of depressive and anxiety symptoms in nonclinical community adults: Relative contributions of early life stressor types and adult trauma exposure. Journal of Psychiatric Research, 47, 23–32.
- Clancy, C. P., Graybeal, A., Tompson, W. P., Badgett, K. S., Feldman, M. E., Calhoun, P. S., … Beckham, J. C. (2006). Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: Association with current symptomatology. Journal of Clinical Psychiatry, 67, 1346–1353.
- Clarke, A. T. (2006). Coping with interpersonal stress and psychosocial health among children and adolescents: A meta-analysis. Journal of Youth and Adolescence, 35(1), 11–24.
- Clemmons, J. C., Walsh, K., Dilillo, D., & Messman-Moore, T. L. (2007). Unique and combined contributions of multiple child abuse types and abuse severity to adult trauma symptomatology. Child Maltreatment, 12(2), 172–181.
- Cloitre, M., Stolbach, B. C., Herman, J. L., van der Kolk, B., Pynoos, R., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptoms complexity. Journal of Traumatic Stress, 22(5), 399–408.
- Compas, B. E., Connor-Smith, J. K., Saltzman, H., Harding Thomsen, A., & Wadsworth, M. E. (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127(1), 87–127.
- de Carvalho, H. W., Pereira, R., Frozi, J., Bisol, L. W., Ottoni, G. L., & Lara, D. R. (2015). Childhood trauma is associated with maladaptive personality traits. Child Abuse and Neglect, 44, 18–25.
- Derogatis, L. R., Lipman, R. S., & Covi, L. (1973). SCL-90: An outpatient psychiatric rating scale – Preliminary report. Psychopharmacology Bulletin, 9, 13–28.
- Eekhout, I., de Boer, R. M., Twisk, J. W., de Vet, H. C., & Heymans, M. W. (2012). Missing data: A systematic review of how they are reported and handled. Epidemiology, 23(5), 729–732.
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258.
- Finzi-Dottan, R., & Karu, T. (2006). From emotional abuse in childhood to psychopathology in adulthood. A path mediated by immature defense mechanisms and self-esteem. The Journal of Nervous and Mental Disease, 194(8), 616–621.
- Folkman, S., & Moskowitz, J. T. (2004). Coping: Pitfalls and promise. Annual Review of Psychology, 55, 745–774.
- Fritch, A. M., Mishkind, M., Reger, M. A., & Gahm, G. A. (2010). The impact of childhood abuse and combat-related trauma on post deployment adjustment. Journal of Traumatic Stress, 23(2), 248–254.
- Gibb, B. E. (2002). Childhood maltreatment and negative cognitive styles: A quantitative and qualitative review. Clinical Psychology Review, 22, 223–246.
- Gladwin, T. E., Rinck, M., Eberl, C., Becker, E. S., Lindenmeyer, J., & Wiers, R. W. (2015). Mediation of cognitive bias modification for alcohol addiction via stimulus-specific alcohol avoidance association. Alcoholism, Clinical and Experimental Research, 39(1), 101–107.
- Held, P., Owens, G. P., Schumm, J. A., Chard, K. M., & Hansel, J. E. (2011). Disengagement coping as a mediator between trauma-related guilt and PTSD severity. Journal of Traumatic Stress, 24(6), 708–715.
- Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22.
- Holliday, R., Holder, N., & Suris, A. (2018). Reductions in self-blame cognitions predict PTSD improvements with cognitive processing therapy for military sexual trauma-related PTSD. Psychiatry Research, 263, 181–184.
- Iacoviello, B. M., & Charney, D. S. (2014). Psychological facets of resilience: Implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. European Journal of Psychotraumatology, 5, Article ID 23970.
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer.
- Liem, J. H., & Boudewyn, A. C. (1999). Contextualizing the effects of childhood sexual abuse on adult self- and social functioning: An attachment theory perspective. Child Abuse & Neglect, 23, 1141–1157.
- Littleton, H., Horsley, S., John, S., & Nelson, D. V. (2007). Trauma coping strategies and psychological distress: A meta-analysis. Journal of Traumatic Stress, 20(6), 977–988.
- LoSavio, S. T., Dillon, K. H., & Resick, P. A. (2017). Cognitive factors in the development, maintenance, and treatment of post-traumatic stress disorder. Current Opinion in Psychology, 14, 18–22.
- MacKinnon, D. P., Fairchild, A. J., & Fritz, M. S. (2007). Mediation analysis. Annual Review of Psychology, 58, 593.
- MacKinnon, D. P., Lockwood, C. M., Hoffman, J. M., West, S. G., & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104.
- McLaughlin, K. A., Conron, K. J., Koenen, K. C., & Gilman, S. E. (2010). Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: A test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine, 40, 1647–1658.
- Min, M. O., Minnes, S., Kim, H., & Singer, L. T. (2013). Pathways linking childhood maltreatment and adult physical health. Child Abuse & Neglect, 37, 361–373.
- Monzani, D., Steca, P., Greco, A., D’Addario, M., Cappelletti, E., & Pancani, L. (2015). The situational version of the Brief COPE: Dimensionality and relationships with goal-related variables. Europe’s Journal of Psychology, 11(2), 295–310.
- Nurius, P. S., Green, S., Logan-Greene, P., & Borja, S. (2015). Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse and Neglect, 45, 143–153.
- Passmann Carr, C., Severi Martins, C. M., Stingel, A. M., Lemgruber, V. B., & Juruena, M. F. (2013). The role of early life stress in adult psychiatric disorders: A systematic review according to childhood trauma subtypes. The Journal of Nervous and Mental Disease, 201(12), 1007–1020.
- Rademaker, A. R., Vermetten, E., Geuze, E., Muilwijk, A., & Kleber, R. J. (2008). Self-reported early trauma as a predictor of adult personality: A study in a military sample. Journal of Clinical Psychology, 64(7), 863–875.
- Raghunathan, T. W., Lepkowski, J. M., van Hoewyk, J., & Solenberger, P. A. (2001). Multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology, 27, 85–95.
- Reijnen, A., Rademaker, A. R., Vermetten, E., & Geuze, E. (2015). Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: A 2-year longitudinal analysis. European Psychiatry: The Journal of the Association of European Psychiatrists, 30, 341–346.
- Rodrigues, C. S., & Renshaw, K. D. (2010). Associations of coping processes with posttraumatic stress disorder symptoms in national guard/reserve service members deployed during the OEF-OIF era. Journal of Anxiety Disorders, 24, 694–699.
- Rubin, D. B. (1976). Inference and missing data. Biometrika, 63, 581–592.
- Rubin, D. B. (1996). Multiple imputation after 18+ years. Journal of the American Statistical Association, 91, 473–489.
- Sachs-Ericsson, N., Verona, E., Joiner, T., & Preacher, K. J. (2006). Parental verbal abuse and the mediating role of self-criticism in adult internalizing disorders. Journal of Affective Disorders, 93, 71–78.
- Sexton, M. B., Raggio, G. A., McSweeney, L. B., Authier, C. C., & Rauch, S. A. M. (2017). Contrasting gender and combat versus military sexual traumas: Psychiatric symptom severity and morbidities in treatment-seeking veterans. Journal of Women’s Health, 26(9), 933–940.
- Spatz Widom, C., DuMont, K., & Czaja, S. J. (2007). A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry, 64, 49–56.
- Stein, A. L., Tran, G. Q., Lund, L. M., Haji, U., Dashevsky, B. A., & Baker, D. G. (2005). Correlates for posttraumatic stress disorder in Gulf War veterans: A retrospective study of main and moderating effects. Journal of Anxiety Disorders, 19, 861–876.
- Street, A. E., Gibson, L. E., & Holohan, D. R. (2005). Impact of childhood traumatic events, trauma-related guilt, and avoidant coping strategies on PTSD symptoms in female survivors of domestic violence. Journal of Traumatic Stress, 18(3), 245–252.
- van Buuren, S., & Groothuis-Oudshoorn, K. (2011). MICE: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67.
- Veenman, M., Vermetten, E., de Kloet, C., Unck, F. A. W., & Westenberg, H. G. M. (2005). Prospectief medisch-biologisch onderzoek naar parameters bij stressgerelateerde aandoeningen [Prospective medical-biological research of parameters in stress-related health problems]. Nederlands Militair Geneeskundig Tijdschrift, 58, 60–63.
- Wu, N. S., Schairer, L. C., Dellor, E., & Grella, C. (2010). Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders. Addictive Behaviors, 35(1), 68–71.