ABSTRACT
Background: Internet-delivered Cognitive Behavioural Therapy (i-CBT) offers potential as an alternative, accessible, clinically and cost-effective treatment for post-traumatic stress disorder (PTSD), but little is known about its acceptability.
Objective: To review the available evidence to understand the acceptability of i-CBT for PTSD.
Method: We undertook a mixed-methods systematic review according to Cochrane Collaboration Guidelines, of randomised controlled trials (RCTs) of i-CBT for adults with PTSD. We examined included studies for measures of acceptability, and possible proxy indicators of acceptability, including dropout rates, which were meta-analysed as risk ratios (RRs).
Results: Ten studies with 720 participants were included. We found i-CBT to be acceptable according to specific acceptability measures, and suggestions for acceptability according to some proxy measures of i-CBT programme usage. There was, however, evidence of greater dropout from i-CBT than waitlist (RR 1.39, CI 1.03–1.88; 8 studies; participants = 585) and no evidence of a difference in dropout between i-CBT and i-non-CBT (RR 2.14, CI 0.97–4.73; participants = 132; 2 studies).
Conclusion: i-CBT appears a potentially acceptable intervention for adults with PTSD. We identified clinical and research questions, including the status of proxy indicators, and call for standardised, consistent treatment acceptability measurement.
HIGHLIGHTS
• A review of acceptability of internet-delivered CBT (i-CBT) for PTSD.• I-CBT is a potentially acceptable psychological treatment for PTSD.• Small number of studies limits generalisability of findings.• Standardised, consistent acceptability measurement is needed.
Antecedentes: La terapia cognitivo conductual entregada a través de internet (i-TCC) ofrece potencial como un tratamiento alternativo accesible, clínicamente eficaz y costo-efectivo para el trastorno de Estrés Postraumático (TEPT), pero se conoce poco acerca de su aceptabilidad.
Objetivo: Revisar la evidencia disponible para comprender la aceptabilidad de i-TCC para TEPT.
Método: Realizamos una revisión sistemática de métodos mixtos de acuerdo a las Guías de la Colaboración Cochrane, de estudios aleatorizados controlados (RCT por sus sigla en inglés) de i-TCC para adultos con TEPT. Examinamos los estudios incluídos buscando medidas de aceptabilidad, y posibles indicadores indirectos de aceptabilidad, incluyendo tasas de abandono, los que fueron meta-analizados como Riesgo Relativo (RR).
Resultados: Diez estudios con 720 participantes fueron incluídos. Encontramos que i-TCC era aceptable de acuerdo a medidas específicas de aceptabilidad y sugerencias de su aceptabilidad de acuerdo a algunas medidas indirectas del uso del programa de i-TCC. Hubo, sin embargo, evidencia de un mayor abandono desde i-TCC que Lista de Espera (RR 1.39, IC 1.03-1.88; 8 estudios, participantes = 585) y no hubo diferencia en abandono entre i-TCC y otras intervenciones a través de internet no TCC (RR 2.14, IC 0.97-4.73; participantes = 132; 2 estudios).
Conclusión: i-TCC aparece como una intervención potencialmente aceptable para adultos con TEPT. Identificamos preguntas clínicas y de investigación, incluyendo el estado de los indicadores indirectos, y la necesidad de medidas de aceptabilidad estandarizadas y consistentes.
背景:网上认知行为疗法(i-CBT)为创伤后应激障碍(PTSD)提供了一种更易获得和成本效果比更高的临床性替代治疗方法,但我们对其可接受性知之甚少。
目的:综述现有的证据,以了解i-CBT治疗PTSD的可接受性。
方法:我们根据Cochrane协作指南,对患有PTSD的成人的i-CBT随机对照试验(RCT)进行了混合方法系统综述。我们考查了所纳入的研究的可接受性指标(包括脱落率),并将这些指标元分析化为风险比(RRs)。
结果:根据纳入的10项包括720名参与者的研究,我们发现i-CBT在特定可接受性指标上表现尚可,并根据i-CBT使用的一些代理指标提出增加可接受性的建议。然而,有证据表明i-CBT的辍学率高于等候名单组(RR 1.39,CI 1.03-1.88; 8项研究;被试 = 585),并没有证据表明i-CBT和i-non-CBT之间的脱落率有差异( RR 2.14,CI 0.97-4.73;参与者= 132; 2项研究)。
结论:对于患有PTSD的成人i-CBT似乎是可接受的干预方法。我们还确认了临床和研究的相关问题,包括代理指标的状态。标准化的、一致的测量可接受性的指标亟待确立。
1. Introduction
Trauma-Focused Cognitive Behavioural Therapy (TF-CBT) is widely evidenced as an effective treatment of choice for PTSD (Bisson, Roberts, Andrew, Cooper, & Lewis, Citation2013), recommended in international clinical guidelines (Forbes, Creamer, Bisson, Cohen, Crow, Foa, … Ursano, Citation2010). TF-CBT includes therapies for PTSD sufferers that facilitate an individual to challenge his/her thoughts, beliefs and/or behaviour, and typically include psychoeducation, cognitive and exposure work, stress/relaxation management, and homework. Timely delivery of TF-CBT is important, not least in minimising further potential impact of PTSD, including the development of other mental/physical health problems, impaired functioning, and maladaptive coping mechanisms (Rauch et al., Citation2009; Roberts, Roberts, Jones, & Bisson, Citation2016).
Timely PTSD treatment, including TF-CBT, is not always feasible, with long treatment waiting lists resulting from a limited number of therapists qualified in its delivery (Lovell & Richards, Citation2000). Another barrier in accessing traditional PTSD treatments, such as TF-CBT is the commitment required for weekly face-to-face appointments over several months, something which may not be suitable for all patients (Maercker & Knaevelsrud, Citation2007). Furthermore, TF-CBT, for example, is not covered by national health services or health insurances in all countries (Kazlauskas et al., Citation2016), thereby excluding individuals, in such countries, who cannot afford such treatment.
Internet-delivered CBT (i-CBT), an alternative to therapist-delivered CBT, offers potential as an effective mode of delivery of CBT, promising increased treatment accessibility and cost-effectiveness (Gratzer & Khalid-Khan, Citation2016). I-CBT includes internet-based programmes to treat PTSD sufferers, using CBT or TF-CBT approaches, and may be self-guided or therapist-guided. I-CBT interventions for PTSD generally offer less therapist contact than in traditional face-to-face TF-CBT, and guidance varies across i-CBT interventions, for example a higher level of therapist involvement, feedback and encouragement, week-to-week, is required in the PTSD i-CBT intervention, Interapy (Lange, Rietdijk, Hudcovicova, van de Ven, J.-P.,Schrieken, B., & Emmelkamp, Citation2003), compared with the intervention, PTSD Online (Klein et al., Citation2010), which does not require weekly feedback from therapists. Effective across a range of mental health problems, including anxiety disorders and depression (Lewis, Pearce, & Bisson, Citation2012), i-CBT interventions have also been tested for PTSD, and found to be superior to waitlist and treatment-as-usual, in reducing symptoms of depression and PTSD, with greater effect when guided by a therapist (Lewis, Roberts, Bethell, Robertson, & Bisson, Citation2018). In recognition of the developing evidence base, guided i-CBT with a trauma-focus has featured amongst treatment recommendations in recent treatment guidelines for PTSD (ISTSS, Citation2018).
Treatment acceptability may influence adherence (Santana & Fontenelle, Citation2011) and outcome (Swift & Callahan, Citation2009), and a growing demand for patient choice in healthcare treatment, including PTSD treatment (Tarrier, Liversidge, & Gregg, Citation2006), suggests an increasing need for accurate information about treatment acceptability in addition to treatment efficacy. A facet of healthcare quality, acceptability is reported increasingly across the literature, however, explicit theories and definitions are lacking, and measurements vary widely. In a review of 43 studies across health care interventions, no explicit theory or definition for acceptability was found (Sekhon, Cartwright, & Francis, Citation2017), with over half (k = 23), of the studies assessing acceptability by objective measures of uptake/adherence, with dropout rates the most commonly relied on measure, which is reflected in the acceptability literature.
Most systematic reviews of psychological treatment for PTSD have focused on efficacy, with some reporting acceptability alongside, commonly with respect to dropout. For example, a Cochrane review (Bisson et al., Citation2013), considered dropout rates as a primary outcome, finding most of the 70 included studies reported dropout rates, with high rates across many studies. However, acknowledged by the authors themselves, interpreting acceptability based on dropout rate alone may be a limitation, with few studies providing explanations for dropouts. Furthermore, outcomes are inconsistently measured for individuals who dropout, and whilst this might in cases indicate treatment unacceptability, and non-improvement of symptoms, research has also shown significant improvement in symptomatology for individuals discontinuing from psychological treatment (Szafranski, Smith, Gros, & Resick, Citation2017). Few studies exist that have directly assessed acceptability of internet-based treatments for psychological disorders, as a whole, in terms of treatment preferences, expectations, usability, and satisfaction (Campos et al., Citation2018). It is important to understand more about acceptability of i-CBT interventions for PTSD given that it is a relatively new treatment in this population, and given that acceptability is a factor likely to affect implementation (Wallin, Mattsson, & Olsson, Citation2016). Therefore, in addition to understanding acceptability according to dropout, we also need to consider acceptability with respect to other factors that might be important, including usability, or tolerability, particularly important given it is an intervention with variable degrees of therapist contact, sometimes largely, sometimes solely, self-directed. To illustrate, it may be argued where there is a considerable reduction, or perhaps no engagement with a therapist, tolerability may be problematic, particularly when concerning exposure work in i-CBT with a trauma-focus, which may require an individual to recount distressing trauma memories (Pietrzak, Goldstein, Southwick, & Grant, Citation2011). Whilst research has shown alliance can be maintained throughout trauma-focused work (Capaldi, Asnaani, Zandberg, Carpenter, & Foa, Citation2016), clinicians frequently report concern about trauma interventions with exposure, for fear of disrupting therapeutic alliance.
1.1. Aim of the study
Acknowledging acceptability as multi-faceted, we decided to adopt Sekhon et al.’s definition of acceptability (Sekhon et al., Citation2017, p. 4): ‘a multi-faceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention’. Referring to this definition we aimed to determine if i-CBT is an acceptable psychological treatment for adults with PTSD, through reviewing and synthesising current knowledge.
2. Materials and methods
We undertook a mixed-method systematic review of randomised controlled trials (RCTs) of i-CBT for adults with PTSD. A protocol was published by PROSPERO, an international prospective register, in November 2017 (Simon, Bisson, Lewis, & Barawi, Citation2017). With no ‘gold standard’ operationalised acceptability measure, we examined studies using any standardised measure of acceptability, self-reported, or clinician-administered, and commonly reported proxy indicators of acceptability, including treatment non-uptake and dropout, adverse effects, and standardised measures of satisfaction.
2.1. Selection criteria
Included studies were RCTs; randomised cross-over trials; and cluster-randomised trials of i-CBT for PTSD, for optimal confidence interpreting findings, given the rigorous methodology/reporting expected of these designs. For consistency with other reviews of psychological therapies for PTSD (Lewis et al., Citation2018), studies were eligible if at least 70% of participants were diagnosed with PTSD according to DSM/ICD criteria, and if participants were aged 16 years or older. There was no restriction on the index trauma; severity or duration of symptoms; or length of time since trauma. Included studies allowed co-morbidity if PTSD was the primary diagnosis and a reduction in PTSD symptoms was the primary aim of the intervention. Studies of i-CBT were eligible, including therapies delivered online and through mobile applications, with or without therapist guidance, and if they provided up to a maximum of 5 h of therapist guidance, delivered face-to-face or remotely. There were no restrictions on number of interactions with a therapist or length of the online programme. Eligible comparator interventions were face-to-face psychological therapy; waitlist/minimal attention/repeated assessment/usual care; and non-CBT internet-delivered psychological therapy. Sample size and publication status were not used to determine inclusion. Studies not published in English were excluded.
2.2. Search strategy
The search strategy used for a review of the efficacy of i-CBT for PTSD (Lewis et al., Citation2018), was adopted for the current review. Search terms were identified and a systematic search of the Cochrane Common Mental Disorders Group (CCMDG) clinical trials registers databases was performed for studies published up to 2 March 2018 (see Appendix A for full search strategy terms). These databases are updated weekly from searches of OVID MEDLINE (from 1950), Embase (from 1974), and PsycINFO (from 1967), quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), and review-specific searches of additional databases. Reference lists of studies and systematic reviews identified in the search were checked and we searched the World Health Organization’s International Clinical Trials Registry Platform, to identify additional unpublished/ongoing studies. We contacted authors of included studies to identify unpublished/submitted studies and conducted a search of the Published International Literature on Traumatic Stress (PILOTS) database. Abstracts of studies identified in the search and full-text publications of potentially eligible studies were screened independently by two authors and whilst we put in place a procedure to resolve any disagreements with the input of a third reviewer, full inter-rater agreement meant that this was not required.
2.3. Data extraction
A pre-designed data extraction form enabled systematic extraction of information on study methodology, participant characteristics, interventions, outcomes, and data on treatment uptake and dropout. Primary measures of interest were: 1) standardised measure(s) of acceptability, self-reported or clinician-administered, at any time point; 2) non-uptake rate, defined as percentage of individuals offered but not taking treatment; 3) dropout or lost to follow-up rate from baseline and prior to treatment completion, as a percentage; 4) adverse effects, indicated by increased PTSD symptoms from baseline to last available follow-up, measured using a standardised scale, for example the Clinician Administered Scale for PTSD (CAPS-5) (Weathers et al., Citation2018), or any other adverse effect reported from baseline including increased self-harm and suicide; 5) any standardised measure of satisfaction administered from baseline; and 6) i-CBT programme usage, for example module completion/logons/self-reported usage/homework completion. Measures of acceptability, including proxy indicators, were the main outcomes of interest, rather than the primary outcomes of the included studies themselves, which was a reduction in PTSD symptoms in every case.
2.4. Data synthesis
Sufficient quantitative data were available across all studies for meta-analyses to be conducted for dropout, as a proxy of acceptability. Data were entered into the Cochrane Collaboration’s Review Manager 5 (RevMan-5) software (Review Manager (RevMan), Citation2014). Categorical outcomes were analysed as risk ratios (RRs), using 95% confidence intervals. Clinical heterogeneity was assessed by looking at variability in the experimental and control interventions, participants, settings, and outcomes. To further assess heterogeneity, the I2 statistic and the chi-squared test of heterogeneity, as well as visual inspection of the forest plots were used. We intended to pool using a fixed-effect meta-analysis where homogeneity was present, and with random-effects meta-analysis where heterogeneity was present, and we planned to generate funnel plots to assess reporting bias if a meta-analysis included more than 10 studies (Higgins & Green, Citation2011).
Given the likely limited number of included studies with insufficiently similar acceptability measures, we also adopted a narrative synthesis methodology to bring together evidence, an approach described as a form of ‘trustworthy story-telling’, and ‘taking a textual approach to the process of synthesis’ (Popay et al., Citation2006, p. 5). This allowed us to organise and describe extracted data which was interpreted and refined by three of the authors, written up in a story-telling narrative.
We assessed included studies for risk of bias using Cochrane criteria (Higgins et al., Citation2011). This examines sequence allocation for randomisation; allocation concealment; blinding of assessors; incomplete outcome data; selective outcome reporting; and any other notable threats to validity (for example, premature termination of the study, non-manualised intervention).
Two researchers independently assessed each study and any discrepancies were discussed with a third researcher with the aim of reaching a unanimous decision. Data extraction and synthesis were conducted in line with Cochrane Collaboration Guidelines (Higgins et al., Citation2011), and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher, Liberati, Tetzlaff, & Altman, Citation2009).
3. Results
presents the study selection flow. At the initial search, 983 studies were identified as potentially eligible. Abstracts were considered, and we obtained full text copies for 66 studies deemed as potentially relevant, and Appendix B lists references to excluded studies. Ten RCTs of 720 participants met the Review’s inclusion criteria.
3.1. Characteristics of included studies
Supplementary Table 1 presents a summary of included studies. Studies compared i-CBT with a waitlist control group, treatment as usual (TAU) or minimal attention control group (k = 8), and with an i-non-CBT psychological intervention (k = 2). Studies were conducted in five countries: Australia (k = 1) (Spence et al., Citation2011); Iraq (k = 1) (Knaevelsrud, Brand, Lange, Ruwaard, & Wagner, Citation2015); Sweden (k = 1) (Ivarsson et al., Citation2014); UK (k = 1) (Lewis et al., Citation2017); and USA (k = 6) (Engel et al., Citation2015; Krupnick et al., Citation2017; Kuhn et al., Citation2017; Littleton, Grills, Kline, Schoemann, & Dodd, Citation2016, Litz et al., Citation2007; Miner et al., Citation2016). Three studies recruited in clinical settings via clinician referrals (Engel et al., Citation2015; Krupnick et al., Citation2017; Lewis et al., Citation2017), these studies also recruited via media, website and promotional material advertising, which was the method used by the remaining seven studies. The sample size ranged from 34 to 159 with a mean of 70.1 (SD = 40.29). Trauma type varied, with three studies concerning service members with military and terrorist-related trauma (Engel et al., Citation2015; Krupnick et al., Citation2017; Litz et al., Citation2007), and one study concerning civilians with war-related trauma (Knaevelsrud et al., Citation2015), reporting moderate to severe PTSD symptoms, overall. Six studies reported individuals with fairly consistent PTSD severities of mild to moderate level, one study concerning rape trauma (Littleton et al., Citation2016), the others including a range of traumatic events taking place in the community (Ivarsson et al., Citation2014; Kuhn et al., Citation2017; Lewis et al., Citation2017; Miner et al., Citation2016; Spence et al., Citation2011).
The majority of studies excluded individuals receiving treatment elsewhere, with current psychosis, substance dependence, active suicidal ideation, and individuals who had recently changed type/dosage of their mental health medication. Three studies excluded individuals with comorbid depression where depression presented immediately prior to the traumatic event (Litz et al., Citation2007), and where symptoms of severe depression presented at assessment (Lewis et al., Citation2017; Spence et al., Citation2011), and another excluded individuals with gross cognitive impairment (Krupnick et al., Citation2017). Two studies did not exclude based on comorbidity, nor suicidal ideation (Kuhn et al., Citation2017; Miner et al., Citation2016). Participants across all studies were aged over 16, the mean ranging from 22 to 46 years, with a mean across studies of 42.05 (SD = 8.72), weighted mean 31.77. Nine studies included female and male participants, the remaining study reporting 100% female participants (Littleton et al., Citation2016). The percentage of female participants across studies was 66.33% (SD = 32.58), weighted mean of 23.46%.
All participants of included studies met diagnostic criteria for PTSD, according to DSM-5 (k = 4) (Engel et al., Citation2015; Lewis et al., Citation2017; Litz et al., Citation2007; Miner et al., Citation2016), and DSM-IV (k = 6) (Ivarsson et al., Citation2014; Knaevelsrud et al., Citation2015; Krupnick et al., Citation2017; Kuhn et al., Citation2017; Littleton et al., Citation2016; Spence et al., Citation2011). Outcome measures were clinician-administered scales in half of the studies, with self-report measures used in the remaining studies.
Included studies examined the following i-CBT programmes: Delivery of Self Training and Education for Stressful Situations (DESTRESS) (k = 2); INTERAPY (k = 1); PTSD Coach (k = 2); From Survivor to Thriver (k = 1); Spring (Lewis, Roberts, Vick, & Bisson, Citation2013) (k = 1); Warriors Internet Recovery & Education (WIRED) (k = 1); a non-specified internet-based CBT (k = 2). PTSD Coach was the only stand-alone programme, with no guidance, examined by two included studies, and the extent/nature of guidance for the guided programmes examined by the remaining studies was widely variable. Only one study reported face-to-face guidance, comprising an hour-long introductory session and fortnightly 30-min appointments thereafter, face-to-face or by phone, according to patient preference, with a trauma therapist, amounting to a mean therapist input per participant of 147.53 min (SD = 57.01) (Lewis et al., Citation2017). The remainder of studies reported limited email/telephone check-in contact, for example one study reported ‘brief check-ins’ by Clinical Psychology students, approximately once fortnightly (Littleton et al., Citation2016). Of the eight studies of guided i-CBT, six reported guiding clinician qualifications, and three reported their training on the i-CBT programme. Three studies used non-trauma-focused i-CBT programmes: DESTRESS (primary care version) and PTSD Coach. The i-CBT programmes were trauma-focused in the other studies, and the common components were: psychoeducation; distress management techniques; cognitive restructuring/trauma processing; and relapse prevention. Duration of treatment ranged from 4 weeks (Miner et al., Citation2016) to 14 weeks (Littleton et al., Citation2016), averaging 8.3 weeks (SD = 2.65), across studies.
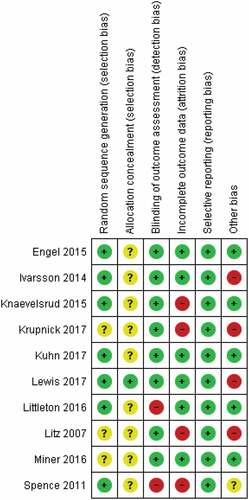
3.2. Methodological quality of studies
presents the risk of bias assessments. Method of sequence allocation was judged to pose ‘low’ risk of bias for seven studies, the remainder rated ‘unclear’ due to insufficient details. Allocation concealment was judged ‘low’ risk for three studies, the remainder rated ‘unclear’. The outcome assessor was aware of the participant’s allocation in two of the studies, with the remaining studies using blinded-raters or self-report questionnaires delivered in a way that could not be influenced by members of the research team. Incomplete outcome data were judged to be ‘high’ risk for four studies, and the remainder were felt to have dealt with dropouts appropriately. Selective reporting was judged ‘low’ risk across studies. We could not rule out potential researcher allegiance, since treatment originators evaluated i-CBT in all but one of the studies. Sample sizes were often small, however, all studies presented objectives.
Figure 2. Methodological quality of included studies.
3.3. Measures of acceptability
Not one of the studies used a standardised/validated acceptability measure; however, three used measures developed specifically for their studies (Krupnick et al., Citation2017; Miner et al., Citation2016; Spence et al., Citation2011). Questions addressed whether individuals had learned new tools/skills/techniques to manage symptoms, whether they would recommend the programme to a friend with PTSD, and opinions/experience using the programme. Qualitative data were collected from participants randomised to the experimental treatment arms in three studies, that compared to waitlist, and responses were noted as ‘extremely enthusiastic’ in one of these studies (Krupnick et al., Citation2017), with moderate to high acceptability responses also reported in the other studies (Miner et al., Citation2016; Spence et al., Citation2011). For example in one study, nearly 83% of participants in the i-CBT arm reported they had learned new tools to cope with their symptoms (Miner et al., Citation2016). Similarly, acceptability was found in another study, assessed in the experimental treatment group using the Distress/Endorsement Validation Scale (DEVS) (Devilly, Citation2004), with 76% of individuals reporting they would recommend the treatment to others (Knaevelsrud et al., Citation2015).
3.4. Treatment satisfaction
Post-treatment satisfaction was measured in the experimental treatment arms in two studies, and found to be high (Littleton et al., Citation2016; Spence et al., Citation2011): one used the Satisfaction with Therapy and Therapist Scale-Revised (STTS-R), measuring satisfaction with one’s therapist and with treatment received (Oei & Green, Citation2008); the other used a measure of satisfaction, based on a standardised Credibility/Expectancy questionnaire, measuring satisfaction with the programme, and quality of correspondence with therapist, and treatment modules.
3.5. Therapeutic alliance
Eight studies examined i-CBT programmes guided by a therapist, the other two being stand-alone programmes (Kuhn et al., Citation2017; Miner et al., Citation2016). We did not set out to look at therapeutic alliance, given research on therapeutic alliance in i-CBT is growing but limited (Maercker & Knaevelsrud, Citation2007); however, it is widely considered an essential ingredient in psychotherapy (Bordin, Citation1979), and was measured post-treatment in the experimental treatment arm in one guided i-CBT study (Littleton et al., Citation2016), using the Working Alliance Inventory-Short form (WAI-S) (Horvath & Greenberg, Citation1989). Strong alliance was reported across three areas of measurement: agreement of therapeutic tasks; bond between therapist and client; and mutual endorsement of therapeutic goals.
3.6. Non-uptake and dropout
Five studies reported non-uptake, defined as the number of individuals offered but not taking up treatment (Engel et al., Citation2015; Lewis et al., Citation2017; Littleton et al., Citation2016; Litz et al., Citation2007; Spence et al., Citation2011). Non-uptake for two studies comparing i-CBT with active treatment comparators reported 18.60% for i-CBT, and 0% for optimised care (Engel et al., Citation2015), and 15.22% for i-CBT, and 14.63% for psycho-education website comparison (Littleton et al., Citation2016). Non-uptake in the remaining studies that reported this information did not differentiate between experimental arms, and overall there was insufficient data to conduct meaningful non-uptake meta-analyses.
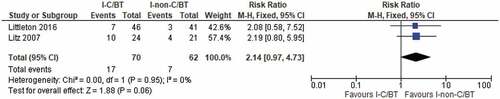
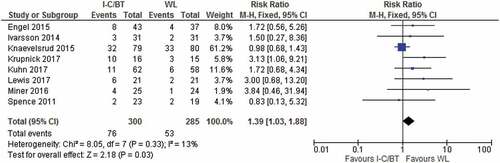
Dropout ranged from 8.69% to 62.5% and was higher in the i-CBT intervention across all but two of the studies, both studies of guided, trauma-focused i-CBT interventions compared to waitlist (Knaevelsrud et al., Citation2015; Spence et al., Citation2011). There was statistically significant evidence for greater dropout from i-CBT compared with waitlist/TAU/minimal attention (k = 8; n = 585; RR 1.39; CI 1.03–1.88), as shown in . There was no evidence of greater dropout from i-CBT than i-non-CBT (k = 2; n = 132; RR 2.14; CI 0.97–4.73), as shown in . Interestingly, dropout was higher for i-CBT, compared with waitlist/usual care/minimal attention for two of the three included studies that concerned non-trauma-focused i-CBT programmes (Kuhn et al., Citation2017; Miner et al., Citation2016), as can be seen in .
Figure 3. Dropout forest plots for i-CBT vs waitlist/usual care/minimal attention.
Two studies attempted to record dropout reasons with rates. Knaevelsrud et al. (Citation2015) reported few responses with some individuals noting technical problems, lack of privacy to use the programme undisturbed. Lewis et al. (Citation2017 reported eight participants dropped out (19.05%), with two individuals reporting a lack of time to dedicate to the programme, two finding the programme difficult, one feeling symptoms had improved, and three individuals did not provide a reason.
3.7. I-CBT programme usage
Programme usage was reported by most studies, in a range of formats, including information on module/homework completion, logons, and self-reported usage. Three studies reported the percentage of individuals completing all programme modules, from 35% to 38.71% (Engel et al., Citation2015; Ivarsson et al., Citation2014; Lewis et al., Citation2017). Two studies examining PTSD Coach found mean, self-reported weekly usages of 2.65 times per week (SD = 1.03) and 2.27 days per week (SD = 1.76), in the treatment groups (Kuhn et al., Citation2017; Miner et al., Citation2016). Engel el at (Engel et al., Citation2015) reported 65% of participants completed at least 6 of the 18 expected logins, with 35% completing all logins. Spence et al. (Citation2011), reported the highest level of engagement, with a mean of 6.74 ‘lessons’ completed (SD = 0.54), the total number of lessons being seven, strong homework compliance, with 81% reporting 20 min or more daily homework practice, and participants downloaded the majority (85%) of the additional resources available.
3.8. Adverse effects
Only two studies reported the presence/absence of adverse effects. One study (Littleton et al., Citation2016) noted two individuals in the intervention condition reported a clinically significant increase in depression symptoms post-treatment, with one of these individuals also reporting a clinically significant increase in anxiety symptoms. It is, however, difficult to attribute this to i-CBT as, sadly, these individuals had also both experienced the death of an immediate family member during treatment. Three additional individuals reported clinically significant increases in anxiety at post-treatment. With respect to the control condition, one individual experienced a clinically significant increase in depression symptoms between post-treatment and follow-up. No studies reported increased PTSD symptoms from baseline to last available follow-up.
4. Discussion
Encouragingly, high levels of i-CBT acceptability were reported for treatment group participants according to measures of acceptability, satisfaction and therapeutic alliance, and usage of the i-CBT programmes was promising, indicating acceptability.
Contrastingly, lower levels of acceptability were inferred through non-uptake and dropout rates. Non-uptake was higher in the i-CBT groups in two studies reporting this information in both the i-CBT and active treatment comparison groups, 18.60% (Engel et al., Citation2015), and 15.22% (Littleton et al., Citation2016), suggesting a considerable proportion of individuals not engaging with i-CBT interventions for PTSD. Combined dropout across all 10 studies was greater for i-CBT, though comparable to dropout reported for face-to-face therapy (Klein et al., Citation2009).
The findings are not atypical of some of the uptake and dropout literature for PTSD. A review of barriers to uptake of computerised-CBT (Waller & Gilbody, Citation2009), reports high acceptability among individuals participating in studies, yet low uptake rates, with explanations suggested, including perceived stigma around research participation. With respect to dropout, high dropout rates were reported in the range of 14–62% in a systematic review of eMental health interventions for PTSD, with 40 included studies (Gaebel et al., Citation2017). Comparable dropout rates have been shown for i-CBT, face-to-face and other internet-interventions for PTSD (Klein et al., Citation2009), though overall, PTSD clinical trial dropout rates are notably variable in the literature, with several possible explanations, including potential research participation burden, completing lengthy questionnaires (Sanders et al., Citation2012), and level of perseverance in contacting hard to reach participants. Tolerability for PTSD treatment is another potential explanation, perhaps impacted by varying levels of therapeutic alliance (Imel, Laska, Jakupcak, & Simpson, Citation2013). Higher dropout has been demonstrated for TF-CBT compared with CBT non-trauma-focused, and compared to waitlist/usual care (Bisson et al., Citation2013, Citation2007). It is possible that elements of the trauma-focused i-CBT interventions in the included studies may have increased distress levels, albeit possibly temporarily, resulting in some dropout. Indeed, a study of the guided i-CBT PTSD Online (Klein et al., Citation2009), found high alliance ratings, despite low/moderate levels of programme satisfaction, the authors suggesting ‘participants may have found some of the program content difficult (e.g. exposure modules); however communication with their therapist was strong and may have mediated these effects’ (p.129). However, tolerability is unlikely to be the sole explanation, given the finding of higher dropout for i-CBT, compared with waitlist/usual care/minimal attention, for two of the three included studies concerning non-trauma-focused i-CBT programmes (Miner, Kuhn), as can be seen in .
4.1. Strengths and limitations
We found several limitations of the research on i-CBT acceptability. Though we report acceptability of i-CBT for PTSD, according to specific acceptability measures and suggestions for acceptability according to i-CBT programme usage, the lack of standardised measures of acceptability across the literature in general (Sekhon et al., Citation2017), is one limitation. Additionally, only participants in the experimental arms of the included studies were asked questions regarding acceptability, a limitation likely to affect many studies across the literature. And a study reporting high levels of satisfaction and working alliance did not obtain this information from individuals who did not complete the post-treatment assessment (Littleton et al., Citation2016). Acknowledged by the authors themselves, this is a limitation, and again is one which will likely affect many studies across the literature. Due to wide variability in measurement/reporting of i-CBT programme usage across the literature, also evident across the included studies, from self-report questions to direct login information, it was not possible to make direct comparisons between studies to draw a clear conclusion. Similarly, the wide variability in the nature/extent/quality of guidance, and the guiding clinicians training in the programmes, so often seen in the literature, and evident in the present review, also make it difficult to meaningfully synthesise information and draw firm conclusions. All programmes were based on cognitive-behavioural approaches, with common components of psychoeducation, distress management techniques, cognitive restructuring/trauma processing, and relapse prevention, though there was still some heterogeneity across i-CBT programmes, so we must be cautious in our interpretation of the findings. However, we considered this clinical heterogeneity alongside the statistical homogeneity of dropout data and were able to pool data using fixed-effect meta-analyses (Higgins & Green, Citation2011).
The contrasting picture of lower levels of acceptability according to dropout rates might be explained by the limited usefulness as dropout an indicator for acceptability (Szafranski et al., Citation2017). Despite being the most commonly reported indicator of acceptability in the present review, and reflected elsewhere in the literature (Sekhon et al., Citation2017), it is difficult to interpret dropout given the lack of reported reasons. Only four studies in the present review reported reasons or provided reference to their attempted collection (Knaevelsrud et al., Citation2015; Krupnick et al., Citation2017; Lewis et al., Citation2017; Spence et al., Citation2011), and the picture was similar for non-uptake. Arguably an individual might drop out of treatment due to a perceived sense of feeling better, or conversely might engage with a treatment despite perceiving it to be unacceptable. Of course, dropout must indicate treatment unacceptability, and non-improvement of symptoms, in some cases, however research has shown improvement in symptomatology for a considerable proportion (35.85–55.56%) of individual(s) who discontinued psychotherapy for PTSD and depression (Szafranski et al., Citation2017).
For optimal confidence interpreting findings, eligibility was limited to RCTs, given the rigorous methodology/reporting expected of this design, though we accept the inclusion of other designs may have provided additional acceptability information. We followed rigorous Cochrane Collaboration guidelines (Higgins et al., Citation2011), with two authors independently screening abstracts/relevant papers, against inclusion criteria, extracting data and rating risk of bias. Risks of bias were identified, limiting our confidence in the quality of the studies.
We included comparison groups of face-to-face and non-CBT internet-delivered psychological therapy; waitlist/minimal attention/repeated assessment/usual care, and we acknowledge the potential limitation of the comparison group heterogeneity. The number of included studies was small, and given that we included only published papers, we must acknowledge the possible influence of publication bias. Also, we excluded studies not published in English, limiting generalisability. Whilst there were enough studies to calculate meta-analysis of dropout (Valentine, Pigott, & Rothstein, Citation2010), it may be argued that the meta-analyses comparisons lack statistical power, given that power was not calculated a priori (Hedges & Pigott, Citation2001), and we did not consider it appropriate to conduct post-hoc power analysis (Hoenig & Heisey, Citation2001). There was an insufficient number of studies to investigate reporting bias.
Several studies relied on PTSD diagnosis based on self-report measures, and the predominant methods of recruitment were media/website advertising, potentially limiting generalisability of the findings since not all participants were necessarily treatment-seeking. Nonetheless, our review did not restrict on sample size, index trauma, time since trauma, severity/duration of symptoms, and we decided to include studies with a minimum of 70% of individuals with a PTSD diagnosis, as well as allowing for comorbidity, so there is good reason to believe our findings could be cautiously generalised to clinical populations.
4.2. Clinical/treatment implications
Guided i-CBT has featured amongst treatment recommendations in recent treatment guidelines for PTSD (ISTSS, Citation2018), and offers promise as another treatment of choice, addressing the growing demand for patient choice in healthcare treatment, including PTSD treatment (Tarrier et al., Citation2006). Understanding the clinical utility of i-CBT for individuals with PTSD is of critical importance, and must give weight to acceptability, widely recognised as vital in the roll-out of health care interventions (Craig & Petticrew, Citation2013). I-CBT for individuals with PTSD offers potential as a cost-effective, timely and accessible treatment choice, especially for individuals who might have difficulty committing to standard treatment of weekly appointments (Maercker & Knaevelsrud, Citation2007), potentially reducing long waiting lists in mental health services.
Treatment uptake, retention and adherence reflect the broader domains of behaviour constituting engagement; therefore, clinicians might consider adopting strategies that might be influential in engaging individuals with PTSD in an i-CBT intervention. These might include motivational/shared decision-making strategies, and enhancing patient/clinician communication, for example facilitating trauma information disclosure, through establishing a strong therapeutic alliance (Capaldi et al., Citation2016; Christensen, Griffiths, & Farrer, Citation2009; Kehle-Forbes & Kimerling, Citation2017; Maercker & Knaevelsrud, Citation2007). Clinical practice might also consider the integration of such interventions within stepped-care models (Ebert et al., Citation2018), appreciating its value as a form of treatment in its own right, whilst also emphasising the ongoing role of individual therapy for more complex presentations (Waller & Gilbody, Citation2009).
4.3. Research implications
Further research is required in the growing field of i-CBT, which recognises acceptability as a priority outcome in itself, and as an additional factor likely to affect its implementation as a treatment intervention (Kaltenthaler et al., Citation2008). We need to further understand factors associated with i-CBT treatment acceptability and efficacy, including acceptability’s potential role as a mediator of treatment outcome, in order to facilitate the development of optimised i-CBT for PTSD targeted to individuals who might benefit most (Klein et al., Citation2010).
The growing literature points towards advantages of guided, over unguided i-CBT in PTSD (Lewis et al., Citation2012). Indeed, guided interventions were used in the two included studies in the present review that showed lower attrition in the i-CBT group, compared with waitlist (Knaevelsrud et al., Citation2015; Spence et al., Citation2011). However, the study with most guidance (Lewis et al., Citation2017) showed greater dropout in the immediate i-CBT group, and whilst there may be several explanations, therapist input per se does not seem to be the answer and further research is required to understand the relationship between guidance in i-CBT interventions and treatment acceptability.
To develop knowledge in the field of treatment acceptability, and to inform the development of acceptable i-CBT programmes for PTSD, we put forward recommendations. Firstly, the development and routine use of validated, reliable acceptability measures that include measures of treatment satisfaction, therapeutic alliance, intervention usage and adherence. Also, standardised methodology for assessment and reporting of acceptability in mental health and psychological treatment studies. And for further exploration of the reliability of proxy measures of acceptability, particularly dropout. Routine, standardised collection of non-uptake and dropout, including reasons, would be an important step in understanding clinical trial participation generally, as well as in understanding the picture in terms of PTSD treatment acceptability. These recommendations would lead to new studies which may be directly comparable, enabling a clearer understanding of key factors that determine the acceptability of i-CBT.
5. Conclusion
Overall, i-CBT appears a potentially acceptable intervention for adults with PTSD. Despite indications of lower levels of acceptability according to dropout rates, higher levels of acceptability were indicated for treatment group participants according to measures of acceptability, and i-CBT programme usage. We identified clinical and research questions, including the status of proxy indicators, and call for standardised, consistent treatment acceptability measurement, to lead to acceptable and effective i-CBT interventions for PTSD.
Supplemental Material
Download Zip (78.9 KB)Acknowledgments
We would like to acknowledge the input and support of the Cochrane Collaboration and the National Centre for Mental Health.
Disclosure statement
Jonathan Bisson, Catrin Lewis and Neil Roberts developed the web-based guided self-help programme Spring; the intellectual property rights for Spring are held by Cardiff University and these co-authors may benefit financially if Spring were to be commercialised in the future.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Bisson, J., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological treatments for chronic post-traumatic stress disorder - Systematic review and meta-analysis. British Journal of Psychiatry, 190(2), 97–12.
- Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews (online), 12, CD003388.
- Bordin, E. S. (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16(3), 252–260.
- Campos, D., Mira, A., Bretón-López, J., Castilla, D., Botella, C., Baños, R. M., & Quero, S. (2018). The acceptability of an Internet-based exposure treatment for flying phobia with and without therapist guidance: Patients’ expectations, satisfaction, treatment preferences, and usability. Neuropsychiatric Disease and Treatment, 14, 879–892.
- Capaldi, S., Asnaani, A., Zandberg, L. J., Carpenter, J. K., & Foa, E. B. (2016). Therapeutic alliance during prolonged exposure versus client‐centered therapy for adolescent posttraumatic stress disorder. Journal of Clinical Psychology, 72(10), 1026–1036.
- Christensen, H., Griffiths, K. M., & Farrer, L. (2009). Adherence in internet interventions for anxiety and depression. Journal of Medical Internet Research, 11(2), e13.
- Craig, P., & Petticrew, M. (2013). Developing and evaluating complex interventions: Reflections on the 2008 MRC guidance. International Journal of Nursing Studies, 50(5), 585–587.
- Devilly, G. J. (2004). An approach to psychotherapy toleration: The Distress/Endorsement Validation Scale (DEVS) for clinical outcome studies. Journal of Behavior Therapy and Experimental Psychiatry, 35(4), 319–336.
- Ebert, D. D., Van Daele, T., Nordgreen, T., Karekla, M., Compare, A., Zarbo, C., … Baumeister, H. (2018). Internet- and mobile-based psychological interventions: Applications, efficacy, and potential for improving mental health a report of the EFPA E-health taskforce. European Psychologist, 23(2), 167–187.
- Engel, C. C., Litz, B., Magruder, K. M., Harper, E., Gore, K., Stein, N., … Coe, T. R. (2015). Delivery of self training and education for stressful situations (DESTRESS-PC): A randomized trial of nurse assisted online self-management for PTSD in primary care. General Hospital Psychiatry, 37(4), 323–328.
- Forbes, D., Creamer, M., Bisson, J. I., Cohen, J. A., Crow, B. E., Foa, E. B., … Ursano, R. J. (2010). A guide to guidelines for the treatment of PTSD and related conditions. Journal of Traumatic Stress, 23(5), 537–552.
- Gaebel, W., Großimlinghaus, I., Mucic, D., Maercker, A., Zielasek, J., & Kerst, A. (2017). EPA guidance on eMental health interventions in the treatment of posttraumatic stress disorder (PTSD). European Psychiatry, 41, 140–152.
- Gratzer, D., & Khalid-Khan, F. (2016). Internet-delivered cognitive behavioural therapy in the treatment of psychiatric illness. Canadian Medical Association Journal, 188(4), 263–272.
- Hedges, L. V., & Pigott, T. D. (2001). The power of statistical tests in meta-analysis. Psychological Methods, 6(4), 203–217.
- Higgins, J. P. T., Altman, D. G., Gotzsche, P. C., Juni, P., Moher, D., Oxman, A. D., … Sterne, J. A. C. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343(7829), d5928-d5928.
- Higgins, J. P. T., & Green, S. (Eds.). (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Retrieved from http://handbook.cochrane.org. G
- Hoenig, J. M., & Heisey, D. M. (2001). The abuse of power: The pervasive fallacy of power calculations for data analysis. The American Statistician, 55(1), 19–24.
- Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the working alliance inventory. Journal of Counseling Psychology, 36(2), 223–233.
- Imel, Z. E., Laska, K., Jakupcak, M., & Simpson, T. L. (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404.
- ISTSS. (2018). Posttraumatic stress disorder prevention and treatment guidelines: Methodology and recommendations. Retrieved from http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_PreventionTreatmentGuidelines_FNL.pdf.aspx
- Ivarsson, D., Blom, M., Hesser, H., Carlbring, P., Enderby, P., Nordberg, R., & Andersson, G. (2014). Guided internet-delivered cognitive behavior therapy for post-traumatic stress disorder: A randomized controlled trial. Internet Interventions, 1(1), 33–40.
- Kaltenthaler, E., Sutcliffe, P., Parry, G., Beverley, C., Rees, A., & Ferriter, M. (2008). The acceptability to patients of computerized cognitive behaviour therapy for depression: A systematic review. Psychological Medicine, 38(11), 1521–1530.
- Kazlauskas, E., Javakhishvilli, J., Meewisse, M., Merecz-Kot, D., Şar, V., Schäfer, I., … Gersons, B. P. R. (2016). Trauma treatment across Europe: Where do we stand now from a perspective of seven countries. European Journal of Psychotraumatology, 7(1), 29450.
- Kehle-Forbes, S., & Kimerling, R. (2017). Patient engagement in PTSD treatment, in PTSD research quarterly (pp. 1–10). Vermont, USA: National Center for PTSD.
- Klein, B., Mitchell, J., Abbott, J., Shandley, K., Austin, D., Gilson, K., … Redman, T. (2010). A therapist-assisted cognitive behavior therapy internet intervention for posttraumatic stress disorder: Pre-, post- and 3-month follow-up results from an open trial. Journal of Anxiety Disorders, 24(6), 635–644.
- Klein, B., Mitchell, J., Gilson, K., Shandley, K., Austin, D., Kiropoulos, L., … Cannard, G. (2009). A therapist-assisted internet-based CBT intervention for posttraumatic stress disorder: Preliminary results. Cognitive Behaviour Therapy, 38(2), 121–131.
- Knaevelsrud, C., Brand, J., Lange, A., Ruwaard, J., & Wagner, B. (2015). Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: Randomized controlled trial. Journal of Medical Internet Research, 17(3), e71.
- Krupnick, J., Green, B. L., Amdur, R., Alaoui, A., Belouali, A., Roberge, E., … Dutton, M. A. (2017). An internet-based writing intervention for PTSD in veterans: A feasibility and pilot effectiveness trial (vol 9, pg 461, 2016). Psychological Trauma-Theory Research Practice And Policy, 9(4), 461–470.
- Kuhn, E., Kanuri, N., Hoffman, J. E., Garvert, D. W., Ruzek, J. I., & Taylor, C. B. (2017). A randomized controlled trial of a smartphone app for posttraumatic stress disorder symptoms. Journal of Consulting and Clinical Psychology, 85(3), 267.
- Lange, A., Rietdijk, D., Hudcovicova, M., van de Ven, J.-P., Schrieken, B., & Emmelkamp, P. M. G. (2003). Interapy: A controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. Journal of Consulting and Clinical Psychology, 71(5), 901–909.
- Lewis, C., Pearce, J., & Bisson, J. I. (2012). Efficacy, cost-effectiveness and acceptability of self-help interventions for anxiety disorders: Systematic review. The British Journal of Psychiatry: The Journal of Mental Science, 200(1), 15–21.
- Lewis, C., Roberts, N., Vick, T., & Bisson, J. I. (2013). Development of a guided self-help (GSH) program for the treatment of mild-to-moderate posttraumatic stress disorder (PTSD). Depression and Anxiety, 30(11), 1121–1128.
- Lewis, C., Roberts, N. P., Bethell, A., Robertson, L., & Bisson, J. I. (2018). Internet‐based cognitive and behavioural therapies for post‐traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews 2018.
- Lewis, C. E., Farewell, D., Groves, V., Kitchiner, N. J., Roberts, N. P., Vick, T., & Bisson, J. I. (2017). Internet-based guided self-help for posttraumatic stress disorder (PTSD): Randomized controlled trial. Depression and Anxiety, 34(6), 555–565.
- Littleton, H., Grills, A. E., Kline, K. D., Schoemann, A. M., & Dodd, J. C. (2016). The From Survivor to Thriver program: RCT of an online therapist-facilitated program for rape-related PTSD. Journal of Anxiety Disorders, 43, 41–51.
- Litz, A., Engel, C. C., Bryant, R. A., & Papa, A. (2007). Randomized, controlled proof-of-concept trial of an internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Plant Disease, 91,1676–1684.
- Lovell, K., & Richards, D. (2000). Multiple Access Points and Levels of Entry (MAPLE): Ensuring choice, accessibility and equity for CBT services. Behavioural and Cognitive Psychotherapy, 28(4), 379–391.
- Maercker, A., & Knaevelsrud, C. (2007). Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: A randomized controlled clinical trial. BMC Psychiatry, 7(1), 13.
- Miner, A., Kuhn, E., Hoffman, J. E., Owen, J. E., Ruzek, J. I., & Taylor, C. B. (2016). Feasibility, acceptability, and potential efficacy of the PTSD coach app: A pilot randomized controlled trial with community trauma survivors. Psychological Trauma-Theory Research Practice And Policy, 8(3), 384–392.
- Moher D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ, 339,b2535.
- Oei, T. P. S., & Green, A. L. (2008). The Satisfaction With Therapy and Therapist Scale-Revised (STTS-R) for group psychotherapy: Psychometric properties and confirmatory factor analysis. Professional Psychology: Research and Practice, 39(4), 435–442.
- Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the USA: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Anxiety Disorders, 25(3), 456–465.
- Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Britten, N., … Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews: Final report. Swindon: ESRC Methods Programme.
- Rauch, S. A. M., Grunfeld, T. E. E., Yadin, E., Cahill, S. P., Hembree, E., & Foa, E. B. (2009). Changes in reported physical health symptoms and social function with prolonged exposure therapy for chronic posttraumatic stress disorder. Depression and Anxiety, 26(8), 732–738.
- Review Manager (RevMan).(2014). Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration.
- Roberts, N. P., Roberts, P. A., Jones, N., & Bisson, J. I. (2016). Psychological therapies for post-traumatic stress disorder and comorbid substance use disorder. Cochrane Database of Systematic Reviews.
- Sanders, C., Rogers, A., Bowen, R., Bower, P., Hirani, S., Cartwright, M., … Newman, S. P. (2012). Exploring barriers to participation and adoption of telehealth and telecare within the whole system demonstrator trial: A qualitative study. BMC Health Services Research, 12(1), 220.
- Santana, L., & Fontenelle, L. F. (2011). A review of studies concerning treatment adherence of patients with anxiety disorders. Patient Preference and Adherence, 5, 427–439.
- Sekhon, M., Cartwright, M., & Francis, J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services Research, 17.
- Simon, N., Bisson, J. I., Lewis, C. E., & Barawi, K. (2017). Acceptability of internet-based cognitive behavioural therapy as a psychological treatment for post traumatic stress disorder (PTSD): A systematic review. Retrieved fom http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017069732
- Spence, J., Titov, N., Dear, B. F., Johnston, L., Solley, K., Lorian, C., … Schwenke, G. (2011). Randomized controlled trial of Internet-delivered cognitive behavioral therapy for posttraumatic stress disorder. Depression and Anxiety, 28(7), 541–550.
- Swift, J. K., & Callahan, J. L. (2009). The impact of client treatment preferences on outcome: A meta‐analysis. Journal of Clinical Psychology, 65(4), 368–381.
- Szafranski, D. D., Smith, B. N., Gros, D. F., & Resick, P. A. (2017). High rates of PTSD treatment dropout: A possible red herring? Journal of Anxiety Disorders, 47(C), 91–98.
- Tarrier, N., Liversidge, T., & Gregg, L. (2006). The acceptability and preference for the psychological treatment of PTSD. Behaviour Research and Therapy, 44(11), 1643–1656.
- Valentine, J. C., Pigott, T. D., & Rothstein, H. R. (2010). How many studies do you need?: A primer on statistical power for meta-analysis. Journal of Educational and Behavioral Statistics, 35(2), 215–247.
- Waller, R., & Gilbody, S. (2009). Barriers to the uptake of computerized cognitive behavioural therapy: A systematic review of the quantitative and qualitative evidence. Psychological Medicine, 39(5), 705–712.
- Wallin, E. E. K., Mattsson, S., & Olsson, E. M.G. (2016). The preference for internet-based psychological interventions by individuals without past or current use of mental health treatment delivered online: A survey study with mixed-methods analysis. JMIR Mental Health, 3(2), e25.
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., … Marx, B. P. (2018). The clinician-administered PTSD scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395.