?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Objective: Due to traumatic experiences and highly prevalent post-migration stressors, refugees are vulnerable for developing psychopathology. To date, research has mainly evaluated trauma-focused therapies, targeting post traumatic stresss symptoms. Treatments targeting post-migration stressors are relatively understudied. The present cohort study evaluated the potential effectiveness of 7ROSES, a transdiagnostic intervention that aims to increase self-efficacy among treatment-seeking refugees in dealing with post-migration stressors. Because it can be applied by non-specialist health care workers, it can be disseminated on a large scale, thereby increasing options for psychosocial support for refugees.
Method: Forty-nine refugees (65% male, average age: 36.02 years, SD = 8.52) with psychopathology were included. Before and after participation in 7ROSES, self-efficacy was measured using the General Self-Efficacy Scale (GSES), and general psychopathology using the Brief Symptom Inventory (BSI).
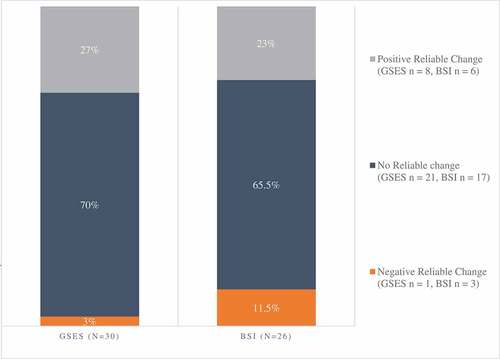
Results: Completers analysis yielded a significant increase in GSES scores (Z = −2.16, p = .03) and significant decrease in BSI scores (Z = −2.05, p = .04) with medium-small effects (both r = −.28). Intent-to-treat analysis, using predictive mean matching imputation, yielded significant results for the GSES (p = .012) but not for the BSI (p = .14) with small effects (GSES r = .14, BSI r = .12). Reliable change indices established negative change in 3%, no change in 70%, and positive change in 27% based on the GSES; percentages were 11.5%, 65.5%, and 23%, respectively, based on the BSI.
Conclusion: Findings provide preliminary evidence that 7ROSES could improve self-efficacy and general mental health in refugees with psychopathology.
HIGHLIGHTS
• 7ROSES is a new low-intensity transdiagnostic treatment.• 7ROSES aims to empower refugees with psychopathology in coping with post-migration problems.• Around a quarter of 7ROSES participants reported an increased self-efficacy and mental health improvement.
Objetivo: Debido a las experiencias traumáticas y los estresores post-migración altamente prevalentes, los refugiados son vulnerables al desarrollo de psicopatología. Hasta la fecha, la investigación ha evaluado principalmente las terapias centradas en el trauma, dirigidas a los síntomas de estrés postraumático. Los tratamientos dirigidos a los estresores posteriores a la migración han sido relativamente poco estudiados. El presente estudio de cohorte evaluó la efectividad potencial de 7ROSES, una intervención transdiagnóstica que tiene como objetivo aumentar la autoeficacia entre los refugiados que buscan tratamiento para tratar los factores estresantes posteriores a la migración. Debido a que puede ser aplicada por trabajadores de la salud no especializados, puede ser difundida a gran escala, aumentando así las opciones de apoyo psicosocial para los refugiados.
Método: Se incluyeron 49 refugiados (65% hombres, edad promedio: 36.02 años, DE = 8.52) con psicopatología. Antes y después de la participación en 7ROSES, se midió la autoeficacia utilizando la Escala General de Autoeficacia (GSES en su sigla en inglés) y la psicopatología general utilizando el Inventario Breve de Síntomas (BSI en su sigla en inglés).
Resultados: El análisis de los refugiados que completaron la intervención arrojó un aumento significativo en las puntuaciones de GSES (Z = −2.16, p = .03) y una disminución significativa en las puntuaciones de BSI (Z = −2.05, p = .04) con efectos medio-pequeños (ambos r = −.28). El análisis por intención de tratar, utilizando la imputación predictiva de correspondencia de medias, arrojó resultados significativos para el GSES (p = .012) pero no para el BSI (p = .14) con efectos pequeños (GSES r = .14, BSI r = .12). Los índices de cambio confiables establecieron un cambio negativo en el 3%, ningún cambio en el 70%, y un cambio positivo en el 27% basado en el GSES; los porcentajes fueron 11.5%, 65.5%, y 23%, respectivamente, basados en el BSI.
Conclusión: Los resultados proporcionan evidencia preliminar de que 7ROSES podría mejorar la autoeficacia y la salud mental general en refugiados con psicopatología.
目标:由于创伤经历和十分普遍的移民后应激源,难民很容易患上精神疾病。至今,研究主要评估以创伤后应激症状为靶点的创伤焦点疗法。针对移民后应激源的治疗方法相对研究较少。本队列研究评估了7ROSES的潜在效力。7ROSES是一种跨诊断干预措施,旨在提高寻求治疗的难民在应对移民后应激源时的自我效能感。因其可由非专业医护人员使用,故可广泛传播,从而为难民增加了心理社会支持的选项。
方法:本研究纳入49名患有精神疾病的难民(男性占65%,平均年龄:36.02岁,标准差为8.52)。在难民参与7ROSES前后,使用《一般自我效能感量表》(GSES)和《简明症状量表》(BSI)分别测量其自我效能感和一般精神疾病情况。
结果:完整数据的分析显示GSES评分显著提高(Z = −2.16,p = .03),BSI评分显著降低(Z = −2.05,p = .04),效应量均为中小(两者 r = - .28)。使用预测均值配对插补后进行的意向分析显示GSES结果显著(p = .012),但BSI结果不显著(p = .14),效应量均较小(GSES:r = .14,BSI :r = .12)。可靠的变化指数确定了基于GSES的评分3%有负向改变,70%无变化,27%有正向改变;分别对应基于BSI的评分为11.5%,65.5%和23%。
结论:结果为7ROSES可提高患精神疾病的难民的自我效能感和一般心理健康提供了初步证据。
1. Introduction
Global political instability and armed conflicts worldwide created a massive influx of refugees into Europe. In 2016, 1.2 million individuals applied for asylum in the European Union (UNHCR, Citation2017). Although displaced persons entering a host country are usually referred to as either ‘refugees’, ‘asylum seekers’, ‘victims of human trafficking’ or ‘undocumented refugees’, in this paper we will refer to the entire group as ‘refugees’. Refugees are considered a high-risk population for the development of psychopathology (Steel et al., Citation2009). It is estimated that one in three refugees is affected by depression, post traumatic stress disorder (PTSD), or an anxiety disorder (Turrini et al., Citation2017), which appear to be chronic in the long-term (Bogic, Njoku, & Priebe, Citation2015). A refugee background doubles the risk of developing non-affective psychoses compared to other migrants (Hollander et al., Citation2016). Other mental disorders are less researched among refugees, but there are indications that they have an elevated risk of medically unexplained physical symptoms (Rohlof, Knipscheer, & Kleber, Citation2014), substance abuse (Ezard, Citation2012), and attempted suicides (Kalt, Hossain, Kiss, & Zimmerman, Citation2013) compared to non-displaced populations. There is an urgent need for timely, targeted, and effective psychological treatments for these health problems.
Importantly, there are indications that traumatized refugees benefit less from treatment compared to other traumatized groups (Ter Heide & Smid, Citation2015); their residual post-treatment symptom severity scores are often above clinical thresholds (Palic & Elklit, Citation2011). Substantial research on adequate psychological treatments for resettled refugees is limited to trauma-focused therapies (TFT) (Giacco & Priebe, Citation2018), and indicating that TFTs are substantially more effective in the general population (d = 1.08–1.40; Cusack et al., Citation2016) than in refugees (g = 0.25–1.01; Lambert & Alhassoon, Citation2015). These findings highlight a need for credible treatment alternatives, besides TFTs, to help improve refugee wellbeing.
In current guideline-informed interventions (e.g., American Psychological Association [APA], Citation2017), little attention is paid to post-migration sources of stress which refugees experience (Miller & Rasmussen, Citation2010; Strang & Ager, Citation2010; Turrini et al., Citation2017), despite their impact on refugee health and well-being (Chu, Keller, & Rasmussen, Citation2013; Li, Liddell, & Nickerson, Citation2016; Porter & Haslam, Citation2005; Priebe, Giacco, & El-Nagib, Citation2016). Examples of such stressors are poverty, unsafe living conditions, loss of social network (Lambert & Alhassoon, Citation2015), discrimination, and insecurity about legal status (Laban, Gernaat, Komproe, van der Tweel, & De Jong, Citation2005). Post-migration stressors predict late-onset PTSD (Bryant, O’Donnell, Creamer, McFarlane, & Silove, Citation2013), negatively impact treatment outcome in refugees (Buhmann, Citation2014; Whitsett & Sherman, Citation2017) and predict depression and anxiety (Schick et al., Citation2018). Addressing post-migration stressors in psychological treatments for resettled refugees has been recommended (Kronick, Citation2017; Slobodin & De Jong, Citation2015). However, it remains to be investigated whether such an approach improves the wellbeing of individuals (Hynie, Citation2018; Tribe, Sendt, & Tracy, Citation2017).
Accordingly, 7ROSES, a novel method was developed to empower treatment-seeking refugees to cope with (trauma-related) psychopathology and post-migration stressors. The current study aims to describe 7ROSES, evaluate its potential to improve self-efficacy and mental health, and provide a treatment case description to understand the first evaluation results in practical terms.
1.1. The intervention: Seven Recovery-Oriented Survivor Empowerment Strategies (7ROSES)
Eight European rehabilitation centres for torture and trauma survivors collaboratively developed the transdiagnostic ‘Method for the Empowerment of Trauma Survivors’ (METS). METS is deliverable in multiple contexts as a flexible toolkit. It can be applied by non-specialist mental health professionals (e.g., social workers, non-specialized psychologists, non-specialized doctors), which reduces provision costs and fosters dissemination.
METS was developed for refugees exposed to traumatic events, facing post-migration challenges on a social level and suffering from psychological distress. METS takes a perspective on empowerment as a process of psycho-social change through increased self-efficacy, the belief in one’s own capacity to adequately act towards ongoing and upcoming stressors. Instead of providing practical support, METS focusses on creating coping resources and developing skills to tolerate or to change negative circumstances, depending on the situation of the participant. Coping with the consequences and impact of traumatic experiences is also an element of the approach, but unlike TFT, METS does not focus on the content of traumatic experiences. The primary aim is to promote self-efficacy, which has been shown to be a sustainable way to reduce psychopathology and increase rehabilitation factors among refugees (Sulaiman-Hill & Thompson, Citation2013). In addition, a high level of self-efficacy is associated with greater tolerance to trauma-related distress among tortured refugees (Morina et al., Citation2018) and better treatment response for trauma-related psychopathology (Livanou et al., Citation2002). The second aim is to reduce the psychological burden of post-migration stresses.
The ‘CHIME framework of recovery’ (Leamy, Bird, Le Boutillier, Williams, & Slade, Citation2011) provided the empirical framework for METS. CHIME is an acronym referring to Connectedness, Hope, Identity, Meaning and Empowerment. The framework shifts the focus in mental health care from illness-based to strengths-based and emphasizes self-control and rehabilitation (Slade, Citation2013). To adjust CHIME to the specific challenges of displaced trauma survivors, expert input was collected during a meeting with experts from all collaborating rehabilitation centres. The applicability of CHIME for the target group was evaluated and discussed until consensus was reached. It resulted in recommendations to extend the framework with two themes: Recognition (R) and Safety (S). Findings from two separate focus groups of displaced refugee trauma survivors concurred with the expert input regarding the need for the themes Recognition and Safety, creating the CHIME+RS framework.
In line with the CHIME+RS themes, the experts collected and developed exercises suitable to be included in the method. For each of the CHIME+RS themes, two sessions were defined, each comprising several exercises. Consequently, it will take a minimum of 9 sessions (including introduction and closing session) to address all themes at least once. Except for the introduction and closing session, the order of sessions is flexible, and determined by the present needs of the participants. (See Appendix A for an overview of the sessions). All exercises focus on increasing self-efficacy, connected with the topic of the session. The exercises can be divided into three categories: practical tools to approach daily problems (e.g., goal planning, during the ‘Hope’ theme), exercises to increase emotional holding (e.g., identifying hopeful messages and ensuring their availability in challenging conditions, during the ‘Connectedness’ theme), and, lastly, exercises to increase awareness of personal (e.g., making a social network circle, during the ‘Connectedness’ theme) or cultural (e.g., identifying and performing a group-ritual, during the ‘Recognition’ theme) resources. The first two categories increase self-efficacy by the introduction of new coping techniques. The last category promotes self-efficacy by encouraging the (re-)vitalization of coping resources that decreased due to forced migration. Also, the order of the sessions is controlled by participants, which can contribute to experienced control and therewith increase self-efficacy (Ajzen, Citation2002). At the beginning of each session a Topic Selection is performed, in which participants identify which CHIME+RS themes are relevant in their lives since the last session. Subsequently, one of the CHIME+RS themes is chosen by the participants.
Each session has the following fixed elements: discussing homework progress (at the beginning of a session), a physical exercise (e.g., breathing exercises, mirroring each other’s movements), topic selection and corresponding exercises, planning homework (at the end of a session). Appendix A for an overview of the session. To give the method a positive connotation, METS was named Seven Recovery Oriented Survivor Empowerment Strategies (7ROSES) in the Netherlands.
2. Methods
2.1. Design
Considering the novelty of 7ROSES, its feasibility was tested using an observational cohort design. A feasibility study is recommended to determine the potential effectiveness of novel approaches and enhance the likelihood of success for future stringent effectiveness studies using RCT designs, thereby saving time and costs (Orsmond & Cohn, Citation2015). Self-efficacy and psychopathology severity were selected as outcome measures.
2.2. Setting
The study was conducted at an outpatient treatment facility located in the Amsterdam region of the Netherlands. It specializes in the treatment of complex trauma-related psychopathology among displaced victims of interpersonal violence (refugees, asylum seekers, and victims of human trafficking) with present post-migration stressors (e.g., poor social network, lack of daytime activities, insecurity concerning one’s residence permit, living in an unsafe environment). Due to its specialist nature the treatment centre receives national referrals for patients with complex psychopathology and high social distress.
2.3. Participants
Fifty-three patients (n = 53) adult patients were approached to participate in 7ROSES, based on their treatment indication. Four refused and 49 agreed to participate. They were referred from primary health care settings with suspected trauma-related psychopathology. Inclusion criteria were: 1) current psychopathology based on the DSM-5 (APA, Citation2013), and 2) social problems due to post-migration living conditions (e.g., lack of work, lack of social network, problems regarding residence permit, insecure housing situation). Exclusion criteria were: 1) acute psychosis, and 2) unwillingness to participate in the 7ROSES trial. Prior psychological treatment and parallel psychopharmacological treatment were not considered as exclusion criteria. All inclusion and exclusion criteria were checked during a multidisciplinary intake. Because our study was the first to evaluate 7ROSES there was no previous information available for conducting a reliable sample size calculation. Therefor inclusion for the 7ROSES pilot was performed without a pre-set up number of participants.
2.4. Procedure
Inclusion took place from March to December 2017, during the first execution of 7ROSES. DSM-5 diagnoses and social problems were established during a multi-disciplinary intake by two trained clinicians. 7ROSES was indicated before, or after other psychological treatments, like trauma focussed therapy. All patients were individually informed about the intended trial by a clinician trained in the 7ROSES method. Participation in the study was voluntary. All patients signed an informed consent before participating.
Self-report questionnaires were administered at a maximum of three weeks before the first treatment session (T1) and at the end of the closing session (T2). Participants who were absent during the closing session were invited for the administration of the second measurement within two weeks after the closing session. The patient’s own clinician, or a supervised master-level psychology student, administered the questionnaires. Participants missing more than half (four sessions) of the treatment were considered ‘dropouts’.
The questionnaires were administered as part of the routine treatment evaluation, which is standard to all patients in treatment at the facility in question. For secondary scientific purposes, all data was archived anonymously. Because all questionnaires were primarily administered for diagnostic purposes, and secondary for data analysis, the institutional review board of Leiden University stated that there was no need for review of the ethical merits.
2.5. Measures
Two questionnaires were selected from the battery of questionnaires that are routinely administered to monitor treatment outcomes. As 7ROSES aims to increase self-efficacy by encouraging personal and cultural resources and increase practical skills and emotional holding, the General Self-Efficacy Scale (GSES) (Schwarzer & Jerusalem, Citation1995) was used to compare the levels of self-efficacy before and after 7ROSES participation. The GSES measures optimistic self-beliefs about one’s ability to cope with a variety of life demands. Respondents are asked to rate 10 statements (4 point scale, ranging from ‘not at all true’ to ‘exactly true’) on how they currently judge themselves. (e.g., ‘I can solve most problems if I invest the necessary effort.’). The questionnaire is available in thirty-two languages. Its internal consistency and multicultural validity are good (Luszczynska, Scholz, & Schwarzer, Citation2005; Nilsson, Hagell, & Iwarsson, Citation2015). Cronbach’s alpha for the present study was good (α = .869).
The second questionnaire was a measure of psychopathology. This questionnaire was selected because all participants suffer from the undermining effect of psychopathology, and self-efficacy, which 7ROSES aims to increase, tends to positively impact mental health. The Brief Symptom Inventory (BSI) (Derogatis & Melisaratos, Citation1983) was used to evaluate changes in general mental health problems. The BSI is a multi-dimensional symptom inventory instructing participants to rate the frequency of fifty-three psychiatric and somatic problems experienced ‘during the past week including today’ on 5-point scales, ranging from ’not at all’ to ‘extremely’. An example item is: ‘trouble remembering things’. The instrument has good psychometric properties in both general (De Beurs, Citation2011) and refugee populations (Raghavan, Rosenfeld, & Rasmussen, Citation2017). Cronbach’s alpha for the present study was excellent (α = .921).
2.6. Treatment
7ROSES comprised nine weekly group sessions of 2.5 hours: one introduction session, seven treatment sessions addressing all CHIME+RS themes, and one closing session. To facilitate the group process, a maximum of three different languages were allowed per group. Registered interpreters were available for participants who were not skilled in a language spoken by the clinicians (Dutch, English, Dari, or French). Eight groups were run with 5 to 8 participants per group.
2.7. Professionals
All clinicians involved were experienced in working with refugees suffering from trauma-related mental health problems. Their professional backgrounds were: social worker (n = 2) and master level psychologist (n = 5). Monthly supervision was provided by two psychologists involved in the development of 7ROSES. During these supervision sessions the professionals shared how 7ROSES was conducted, by discussing which sessions and exercises were performed. Also, they presented problems they met during the execution of 7ROSES. This concerned both problems regarding the exercises and participants’ progress during 7ROSES. Between each monthly supervision session the supervisors were also available for ad hoc questions and problems in line with the weekly treatment sessions that occurred in a higher sequence than the supervision sessions.
2.8. Statistical analysis
SPSS Statistics version 20 was used to perform the statistical analyses (IBM, Armonk, N.Y., U.S.A.). The treatment outcomes were calculated using completer and intent-to-treat analyses to improve the reliability of the findings (Vink, Frank, Pannekoek, & Buuren, Citation2014). The assumptions on skewness and kurtosis were violated in the completer data. Therefore, the non-parametric Wilcoxon Signed Rank Test was used to analyse GSES and BSI treatment changes.
For the intent-to-treat analysis, we imputed 6% (T1) and 35% (T2) of the BSI data and 12% (T1) and 31% (T2) of the GSES data using predictive mean matching imputation (PMMI) with 100 iterations for each imputation. Thirty-five imputation data sets were used, to make the number of imputations equal to or greater than the percentage of missing data (White, Royston, & Wood, Citation2011). Missing data were considered missing at random (MAR). The computed data met the assumptions on skewness and kurtosis. Therefore, a paired t-test calculated differences between T1 and T2 on both outcomes in the intent-to-treat analysis. The significance threshold was set at p < .05 and rank correlation effect sizes (r) were calculated (Rosenthal, Citation1991) for completer and intent-to-treat analysis. Reliable change indices (RCIs) assess whether GSES and BSI individual changes for study completers reflect clinically relevant changes. RCIs were computed based on the standard error of difference (and standard the error of the instrument (
), in accordance with the procedure reported by Jacobson and Truax (Citation1991). This was calculated as
=
√ 1 – α;
=
and RCI = ±1.96 *
. The SD and α from T1 were used for the calculations (GSES: SD = .59, α = .869, BSI: SD = .64, α = .921). RCI values above 1.96 or below −1.96 confirm with 95% certainty that the change is due to treatment improvement or deterioration instead of a measurement error.
3. Results
3.1. Participants
Characteristics of the participants are listed in . Participants originated from Iran (7), Armenia (5), Afghanistan, Syria, Iraq (all 4, respectively), Sierra Leone (3), Congo, Uganda, Eritrea, Nigeria (all 2, respectively), Mali, Palestine, Guinee, Russia, Surinam, Burundi, Morocco, Ivory Coast, Nepal, Ethiopia, Pakistan, Togo, Argentina, and Gambia (all 1, respectively). Consequently, participants spoke 11 different languages. Thirty-two (65%) participants needed an interpreter. Seventeen (35%) participants were diagnosed with one, twenty-six (53%) with two, and six (12%) with three mental health disorders, respectively. There was no significant difference between participants with or without an interpreter on pre, post or change scores for both outcome measures tapping self-efficacy and general psychopathology.
Table 1. Baseline participant characteristics (N = 49).
3.2. Drop-out versus completers
There was no significant difference between dropouts (n = 12) and completers (n = 37) on gender, age, duration of stay in the Netherlands, or schooling. The average session adherence among the drop-out group was 2.67 (SD = 1.85); in the completers group this was 6.96 (SD = 1.12). Drop-outs originated from Armenia, Afganisthan (all 2, respectively), Palestine, Syria, Burundi, Nepal, Maroc, Iraq, Iran and Gambia (all 1, respectively). Countries of origin were diverse, suggesting that dropout was not associated with specific countries or cultural reasons.
3.3. Treatment changes
presents the outcomes for completer and intent-to-treat samples. In the completer sample several questionnaires were missing (GSES: n = 8, BSI: n = 12), and findings were computed with the available data only. Completers analyses (Wilcoxon Signed Rank Test) yielded a significant increase in GSES scores (Z = −2.16, p = .03) and significant decrease in BSI scores (Z = −2.05, p = .04) with medium to small effects (both r = −.28). Intent-to-treat analyses (Paired Sample T-test), using predictive mean matching imputation, yielded significant results for the GSES (p = .012) but not for the BSI (p = .14) with small effects (r = .14 and r = .12, for GSES and BSI, respectively).
Table 2. Findings group treatment changes.
3.4. Individual treatment changes
RCIs were calculated for the GSES and BSI for each treatment completer included at T1 and T2. Reliable change indices established negative change in 3%, no change in 70%, and positive change in 27% based on the GSES; percentages were 11.5%, 65.5%, and 23%, respectively, based on the BSI. See for an overview of the findings.
3.5. Case description
To guarantee anonymization, this case description was inspired on several participants. Consequently, this description can not be traced back to one individual participant. Carlos is a 22-year old patient originating from Iran, where he studied at a university. He had a satisfactory social life and was passionate about learning new things. When he became involved in an illegal political activist group he got into trouble with the Iranian authorities. He experienced several traumatic events (physical and psychological torture) in Iran and developed mental health problems. After a period of imprisonment he fled to the Netherlands.
Carlos resided in the Netherlands for 17 months and was involved in an asylum procedure. He was afraid that his asylum request would be rejected and that he would have to return to Iran. He was not able to fully express himself in Dutch or English which complicated communication with people he was depending on, like his lawyer.
The asylum seeker centre where he lived was located at great distance from his social network. It took over an hour by public transport to reach people he felt familiar with. Also, his budget was restricted and the costs for public transportation were relatively high. Carlos was not allowed to work during the asylum procedure. He used to go to Dutch lessons, but when his course ended he did not know how to find a follow-up course. Carlos’ lack of control over his environment and future in the Netherlands made him feel hopeless. His mental health problems undermined his capacity to organize and prioritize affairs that could improve his situation. During intake he was diagnosed with PTSD and comorbid depression. He was indicated for 7ROSES because he wanted to change his social situation, but felt unable to do so by himself.
Each session started with a topic selection. The group discussed which topic was most relevant to them, according to how their week had proceeded. In some sessions the discussion resulted in an integration of different subjects (e.g. stress about procedure, loneliness and mood problems) into one topic (e.g. empowerment) which fitted the different problems. In other sessions the desired topics varied. During the first session the group decided to apply ‘the majority of votes principle’, but respected the minority by offering them to pick their topic the following session.
The first session after the opening meeting was on Connectedness. Carlos performed an exercise on small talk, by doing a role play, and a successive group discussion on challenges in social interaction. He revealed that, while trusting others was difficult for him, he desired to expand his confidence in others to decrease the loneliness he often felt. After this discussion he became more open to group members. He made more eye contact and started to make jokes. His homework assignment was to invite somebody in the asylum seeker centre to join him to the supermarket, which went well. As 7ROSES progressed, it generally became easier for him to make new social contacts, which reduced the feelings of isolation he reported during intake.
During the following session on Identity, Carlos filled out the ‘strengths matrix’ exercise to identify several personal qualities. During the exercise, he reconnected to his ability and eagerness to learn new things. This week Carlos connected to the group even more, during the break he brought tea for all group members. After the session, he started to write down all unfamiliar Dutch words he heard, and immediately ask for a translation. This enabled him to improve his language skills and increase his sense of control.
During the session on Empowerment, Carlos was encouraged to replace a negative coping strategy (withdrawing; staying alone in his room) with a positive one (seeking social support; talking to a friend). His personal resources (his ability to seek for help and his present social network) were highlighted and additionally embedded in his daily life. It was noteworthy that Carlos was strongly engaged in the topic selection of this session, and was able to convince group members to choose his topic.
During the session on Meaning, Carlos identified which values were important in his life. His homework assignment was to apply these values in daily life. He realized that although spirituality was important to him, he hardly responded to this value. This insight connected him to a group member who felt strengthened through her religion. Together they discussed how spirituatlity helps to accept difficult parts of life. Carlos planned to pick up church visits.
Carlos missed the following session on Recognition due to problems with travel expenses.
During the session on Safety Carlos was involved in the ‘keeping yourself safe’ exercise. The aim was to objectify current threats and possible safety measures. The threats he listed were connected to the ASC and his asylum procedure. He realized that it would increase his safety to find somebody to translate important conversations for him. This resulted in an action plan on finding a volunteer who could help him translate and practice difficult conversations. During the session on Hope, Carlos was challenged to define one desire and think about all the specific actions required to realize this. His desire was to sleep more. His roommate often left early in the morning, when Carlos was still in bed, leaving the door unlocked. This felt unsafe for Carlos and consequently he always woke up early in the morning. Because he didn’t sleep well in general, it was hard for him to fall asleep afterwards. With help from the group he defined all actions necessary (find a translator, the right words, the right timing) to have a productive discussion with his roommate. After the session Carlos left together with one group member to travel together, since they found out they lived in the same area.
At the end of 7ROSES Carlos was satisfied with the treatment. He felt that he regained self-esteem by talking about his past strengths, and increased his trust in others due to the positive group process. The practitioners noticed that Carlos developed openess to group members, and his ability to express his needs to them. These experiences helped him to actively address issues in his life that he wanted to change and were in his domain of control.
4. Discussion
To the best of our knowledge, this is the first study that evaluated a self-efficacy-oriented treatment method for resettled refugees. The study objectives were to establish changes in self-efficacy and general mental health in refugees with psychopathology after participation in 7ROSES. The findings indicated a modest increase in self-efficacy and minimal improvement of general mental health (i.e., symptom reduction). Changes in self-efficacy and psychopathology symptoms were modest, and the intent-to-treat sample yielded no significant changes in general mental health.
7ROSES provision went along with reliable clinical improvement in approximately one out of every four participants. This is a salient finding since the 7ROSES treatment comprised only nine sessions, which is low compared to the average of seventeen sessions displayed in a recent meta-analysis of fourteen treatment studies with resettled refugees (Nosè et al., Citation2017). Testing the results of a longer version of 7ROSES could be a valuable next step, since generally greater treatment effects can be expected with the provision of more treatment sessions (e.g., Karatzias et al., Citation2007).
This study demonstrated the feasibility of 7ROSES for refugees diagnosed with psychopathology, like the case description illustrates, with the aim to improve self-efficacy and to reduce mental distress for completers. However, it also indicated that the method did not go along with significant clinical improvement for most participants. Moreover, 3 participants reported a deterioration of symptoms and 1 of self-efficacy. Although these findings are in contradiction with the treatment aims, they are in accordance with reported deterioration rates from a previous treatment study with a comparable sample and setting (Ter Heide, Mooren, van de Schoot, de Jongh, & Kleber, Citation2016).
Based on the current findings, it would be premature however to suggest provision of 7ROSES as a stand-alone treatment in clinical settings. Instead, it seems suitable for provision within multi-model interventions. 7ROSES might best be delivered prior to guideline-recommended therapies, since self-efficacy may contribute to the effectiveness of successive treatments (Livanou et al., Citation2002). Patients who recover sufficiently after 7ROSES may opt to end treatment, while others proceed with specialized (more intensive) approaches like TFT. This stepwise approach may prevent patient overtreatment and at the same time increase the available treatment capacity of organizations, since 7ROSES does not require specialized professionals.
The current study has several limitations. First, given the lack of a control group, it is uncertain to what extent changes in self-efficacy and general mental health were caused by 7ROSES. The impact of group process characteristics, for example, which usually tends to support mental health within the target group (Bunn, Goesel, Kinet, & Ray, Citation2015), could not be controlled for. Also, a possible role of natural recovery processes (e.g. Gerger, Munder, & Barth, Citation2014) cannot be excluded, although the prevalence of psychopathology in refugees in naturalistic settings remains high in the long term (Bogic et al., Citation2015), and even tends to increase in the face of post-migratory stressors (Laban, Gernaat, Komproe, Schreuders, & De Jong, Citation2004). Some may argue that the current observational study lacks a strong design that would include a control group, such as a RCT. An observational design was chosen because 7ROSES is a novel method. It is recommended to perform an observational feasibility study for any new method prior to any RCT (Orsmond & Cohn, Citation2015). Second, long-term effects of 7ROSES still need to be examined. Third, post-treatment questionnaires were administered at the end of the closing session, which may have affected post-treatment outcomes for the BSI. This questionnaire instructed participants to evaluate their general mental health during ‘the past week including today’, thereby including a 7ROSES session in the period of evaluation. Despite its limitations, the current time point was chosen to avoid extra travelling for the participants who often have a limited budget. Fourth, 94% of all participants were diagnosed with PTSD, though PTSD was not an outcome measure in the current study. Although the BSI identifies psychological distress in trauma exposed individuals (Al-Krenawi, Lev-Wiesel, & Sehwail, Citation2007) and reflects a posttraumatic symptom constellation (Raghavan et al., Citation2017), the effect of 7ROSES on PTSD symptoms, therefore, remains uncertain. Fifth, prior psychological treatments and parallel psychopharmoca treatments were not exclusion criteria. Therefore, reported improvements in self-efficacy could be (partially) due to these interventions.
Lastly, data on post-migration stressors were missing. Although 7ROSES is focused on internal factors (self-efficacy), it aims to increase the resilience towards the negative impact of external factors (post-migration stressors). Hence, findings on external factors would display if 7ROSES impacts either the participants’ ability to deal with post-migration stressors, their actual social situation, or both. For future treatment studies examining 7ROSES it is recommended to follow a Randomized Controlled Trial (RCT) design. The best control condition fur such an RCT is questionable, since 7ROSES aims to increase self-efficacy, while previously established treatments (e.g. Turrini et al., Citation2017) for the target population primarily focus on reduction in PTSD and depression. Hence, before comparing 7ROSES to established interventions it is necessary to determine if it impacts PTSD and depression symptom levels. Additionally, we encourage future researchers to include post migrations stressor scales, and to perform a follow-up measurement.
Notwithstanding these limitations, this study also has various strengths. First, findings were analysed on an individual level, next to group changes, to demonstrate the clinical potential of 7ROSES. Second, the selection bias was minimal since all present patients with psychopathology and present daily stressors were indicated for 7ROSES, within the timeframe of the study. Only four participants refused study participation. Consequently, the treatment groups were heterogeneous with substantial individual differences on social, cultural, and clinical level. The procedures and study-sample represent clinical practice, which usually is a challenge in researching the population in question (Enticott et al., Citation2017). Therefore, findings can be generalized to comparable settings. Meanwhile, a heterogeneis sample complicates the drawing of conclusions on subgroups level.
5. Conclusion
This study provides preliminary evidence for a self-efficacy oriented treatment for resettled refugees. Since group changes were small, we should remain modest about 7ROSES’ potential. However, around a quarter of all participants showed improved self-efficacy and general mental health after participation. Therefore, while also considering the complexity in dealing with traumatized refugees and the non-specialist nature of the method, this finding is relevant to clinicians and researchers working with refugee populations.
While the relevance of self-efficacy for the target population has been established before (Morina et al., Citation2018; Sulaiman-Hill & Thompson, Citation2013), this study is the first to indicate that psychological treatment may promote self-efficacy in refugees. Therewith it responds to the critique (Lambert & Alhassoon, Citation2015; Miller & Rasmussen, Citation2010) on the domination of PTSD as a focus in treatment methods for refugees. Moreover, this study is a first step in establishing the clinical utility of 7ROSES for a highly vulnerable population.
Clinical impact statement
Refugees are vulnerable for developing mental health problems, like posttraumatic stress disorder (PTSD), because of experienced traumas and post-migration problems (like housing problems or loss of social network). This study evaluated the effect of a transdiagnostic treatment, 7ROSES, that empowers refugees with psychopathology in coping with post-migration problems. The outcomes of this study indicate potential effects of 7ROSES. Around a quarter of all refugees who participated reported an increased self-efficacy and mental health improvement after participation. As this is a low-intensity transdiagnostic treatment method which can be provided by non-specialists, it may be accessible for many individuals.
Acknowledgments
We thank all clients for their willingness to participate in the study. We thank all partners for their contribution in the METS project: FWC (Cyprus); CRC (Cyprus); XENION (Germany); BAfF (Germany); IRC (Italy), MRCC Craiova (Rumania); and ICAR Foundation (Romania). We thank Jacky June ter Heide for proofreading the manuscript. We thank Laura van Driem for editing the text. We thank Niels van der Aa and Gerko Vink for their (methodological) advice.
Data availability statement
Data can be requested from the first author for secondary analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ajzen, I. (2002). Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal ofApplied Social Psychology, 32(4), 665–12.
- Al-Krenawi, A., Lev-Wiesel, R., & Sehwail, M. (2007). Psychological symptomatology among Palestinian male and female adolescents living under political violence from 2004-2005. Community Mental Health, 43, 49–56.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
- Association, American Psychological. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Washington, DC: American Psychological Association.
- Bogic, M., Njoku, A., & Priebe, S. (2015). Long-term mental health of war-refugees: A systematic literature review. BMC International Health and Human Rights, 15(1). doi:10.1186/s12914-015-0064-9
- Bryant, R. A., O’Donnell, M. L., Creamer, M., McFarlane, A. C., & Silove, D. (2013). A multisite analysis of the fluctuating course of posttraumatic stress disorder. JAMA Psychiatry (chicago, Ill.), 70(8), 839–846.
- Buhmann, C. B. (2014). Traumatized refugees: Morbidity, treatment and predictors of outcome. Danish Medical Journal, 61(8), 1–29.
- Bunn, M., Goesel, C., Kinet, M., & Ray, F. (2015). Group treatment for survivors of torture and severe violence: A literature review. Torture: Quarterly Journal on Rehabilitation of Torture Victims and Prevention of Torture, 26(1), 45–67.
- Chu, T., Keller, A. S., & Rasmussen, A. (2013). Effects of post-migration factors on PTSD outcomes among immigrant survivors of political violence. Journal of Immigrant and Minority Health, 15(5), 890–897.
- Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., … Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141.
- De Beurs, E. (2011). Brief symptom inventory 18-BSI 18-handleiding (herziene editie). Leiden: PITS BV.
- Derogatis, L. R., & Melisaratos, N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13(3), 595–605.
- Enticott, J. C., Shawyer, F., Vasi, S., Buck, K., Cheng, I. H., Russell, G., … Meadows, G. (2017). A systematic review of studies with a representative sample of refugees and asylum seekers living in the community for participation in mental health research. BMC Medical Research Methodology, 17(1), 17–37.
- Ezard, N. (2012). Substance use among populations displaced by conflict: A literature review. Disasters, 36(3), 533–557.
- Gerger, H., Munder, T., & Barth, J. (2014). Specific and nonspecific psychological interventions for PTSD symptoms: A meta-analysis with problem complexity as a moderator. Journal of Clinical Psychology, 70(7), 601–615.
- Giacco, D., & Priebe, S. (2018). Mental health care for adult refugees in high-income countries. Epidemiology and Psychiatric Sciences, 27(2), 109–116.
- Hollander, A. C., Dal, H., Lewis, G., Magnusson, C., Kirkbride, J. B., & Dalman, C. (2016). Refugee migration and risk of schizophrenia and other non-affective psychoses: Cohort study of 1.3 million people in Sweden. BMJ, 352. doi:10.1136/bmj.i1030
- Hynie, M. (2018). The social determinants of refugee mental health in the post-, migration context: A critical review. The Canadian Journal of Psychiatry, 63(5), 297–303.
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19.
- Kalt, A., Hossain, M., Kiss, L., & Zimmerman, C. (2013). Asylum seekers, violence and health: A systematic review of research in high-income host countries. American Journal of Public Health, 103(3), 30–42.
- Karatzias, A., Power, K., McGoldrick, T., Brown, K., Buchanan, R., Sharp, D., & Swanson, V. (2007). Predicting treatment outcome on three measures for post-traumatic stress disorder. European Archives of Psychiatry and Clinical Neuroscience, 257(1), 40–46.
- Kronick, R. (2017). Mental health of refugees and asylum seekers: Assessment and intervention. The Canadian Journal of Psychiatry, 63, 290–296.
- Laban, C. J., Gernaat, H. B., Komproe, I. H., Schreuders, B. A., & De Jong, J. T. (2004). Impact of a long asylum procedure on the prevalence of psychiatric disorders in Iraqi asylum seekers in The Netherlands. The Journal of Nervous and Mental Disease, 192(12), 843–851.
- Laban, C. J., Gernaat, H. B., Komproe, I. H., van der Tweel, I., & De Jong, J. T. (2005). Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. The Journal of Nervous and Mental Disease, 193(12), 825–832.
- Lambert, J. E., & Alhassoon, O. M. (2015). Trauma-focused therapy for refugees: Meta- analytic findings. Journal of Counseling Psychology, 62(1), 28–37.
- Leamy, M., Bird, V., Le Boutillier, C., Williams, J., & Slade, M. (2011). Conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. The British Journal of Psychiatry, 199(6), 445–452.
- Li, S. S. Y., Liddell, B. J., & Nickerson, A. (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18, 82.
- Livanou, M., Baosglu, M., Marks, I. M., De Silva, P., Noshirvani, H., Lovell, K., & Thrasher, S. (2002). Beliefs, sense of control and treatment outcome in post-traumatic stress disorder. Psychological Medicine, 32(1), 157–165.
- Luszczynska, A., Scholz, U., & Schwarzer, R. (2005). The general self-efficacy scale: Multicultural validation studies. The Journal of Psychology, 139(5), 439–457.
- Miller, K. E., & Rasmussen, A. (2010). War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science & Medicine, 70(1), 7–16.
- Morina, N., Bryant, R. A., Doolan, E. L., Martin‐Sölch, C., Plichta, M. M., Pfaltz, M. C., … Nickerson, A. (2018). The impact of enhancing perceived self‐efficacy in torture survivors. Depression and Anxiety, 35(1), 58–64.
- Nilsson, M. H., Hagell, P., & Iwarsson, S. (2015). Psychometric properties of the general self- efficacy scale in Parkinson’s disease. Acta Neurologica Scandinavica, 132(2), 89–96.
- Nosè, M., Ballette, F., Bighelli, I., Turrini, G., Purgato, M., Tol, W., … Barbui, C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta- analysis. PLoS One, 12, e0171030.
- Orsmond, G. I., & Cohn, E. S. (2015). The distinctive features of a feasibility study: Objectives and guiding questions. OTJR: Occupation, Participation and Health, 35(3), 69–177.
- Palic, S., & Elklit, A. (2011). Psychosocial treatment of posttraumatic stress disorder in adult refugees: A systematic review of prospective treatment outcome studies and a critique. Journal of Affective Disorders, 131(1), 8–23.
- Porter, M., & Haslam, N. (2005). Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. JAMA, 294(5), 602–612.
- Priebe, S., Giacco, D., & El-Nagib, R. (2016). Public health aspects of mental health among migrants and refugees: A review of the evidence on mental health care for refugees, asylum seekers and irregular migrants in the WHO European region. Copenhagen: WHO Regional Office for Europe..
- Raghavan, S. S., Rosenfeld, B., & Rasmussen, A. (2017). Measurement invariance of the Brief Symptom Inventory in survivors of torture and trauma. Journal of Interpersonal Violence, 32(11), 1708–1729.
- Rohlof, H. G., Knipscheer, J. W., & Kleber, R. J. (2014). Somatization in refugees: A review. Social Psychiatry Psychiatric Epidemiology, 49, 1793–1804.
- Rosenthal, R. (1991). Meta-analytic procedures for social research (Vol. 6). Newbury Park, CA: SAGE Publications.
- Schick, M., Morina, N., Mistridis, P., Schnyder, U., Bryant, R. A., & Nickerson, A. (2018). Changes in post-migration living difficulties predict treatment outcome in traumatized refugees. Frontiers in Psychiatry, 9, 476.
- Schwarzer, R., & Jerusalem, M. (1995). Generalized self-efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: Nfer-Nelson.
- Slade, M., Leamy, M., Bird, V., Le Boutillier, C., Thornicroft, G., Ruggeri, M., & Goldberg, D. (2013). Mental health services and recovery. Improving mental health care: The global challenge. Chichester: Wiley, 40–56. doi:10.1192/bjp.bp.114.155978
- Slobodin, O., & De Jong, J. T. (2015). Mental health interventions for traumatized asylum seekers and refugees: What do we know about their efficacy? International Journal of Social Psychiatry, 61(1), 17–26.
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & Van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549.
- Strang, A., & Ager, A. (2010). Refugee integration: Emerging trends and remaining agendas. Journal of Refugee Studies, 23(4), 589–607.
- Sulaiman-Hill, C. M., & Thompson, S. C. (2013). Learning to fit in: An exploratory study of general perceived self-efficacy in selected refugee groups. Journal of Immigrant and Minority Health, 15(1), 125–131.
- Ter Heide, F. J. J., Mooren, T. M., van de Schoot, R., de Jongh, A., & Kleber, R. J. (2016). Eye movement desensitisation and reprocessing therapy v. stabilisation as usual for refugees: Randomised controlled trial. The British Journal of Psychiatry, 209(4), 311–318.
- Ter Heide, F. J. J., & Smid, G. E. (2015). Difficult to treat? A comparison of the effectiveness of treatment as usual in refugees and non-refugees. BJPsych Bulletin, 39(4), 182–186.
- Tribe, R. H., Sendt, K. V., & Tracy, D. K. (2017). A systematic review of psychosocial interventions for adult refugees and asylum seekers. Journal of Mental Health, 1–15. doi:10.1080/09638237.2017.1322182
- Turrini, G., Purgato, M., Ballette, F., Nosè, M., Ostuzzi, G., & Barbui, C. (2017). Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. International Journal of Mental Health Systems, 11, 51.
- UNHCR. (2017, 15 June). Figures at a Glance Statistical Yearbook. Retrieved from http://www.unhcr.org/figures-at-a-glance.html
- Vink, G., Frank, L. E., Pannekoek, J., & Buuren, S. (2014). Predictive mean matching imputation of semicontinuous variables. Statistica Neerlandica, 68(1), 61–90.
- White, I. R., Royston, P., & Wood, A. M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30, 377–399.
- Whitsett, D., & Sherman, M. F. (2017). Do resettlement variables predict psychiatric treatment outcomes in a sample of asylum-seeking survivors of torture? International Journal of Social Psychiatry, 63(8), 674–685.