ABSTRACT
Background: Given the unprecedented number of traumatized refugee minors in Europe and the increased prevalence of mental disorders such as PTSD in this vulnerable population, new methodologies that help us to better understand their symptomatology are crucial. Network analysis might help clinicians to both understand which symptoms might trigger other symptoms, and to identify relevant targets for treatment. However, to date only two studies have applied the network analysis approach to an (adult) refugee population and only three studies examined this approach in children and adolescents.
Objective: The aim of this study is to explore the network structure and centrality of DSM-5 PTSD symptoms in a cross-sectional sample of severely traumatized refugee minors.
Method: A total of N = 419 (Mage = 16.3; 90.7% male) unaccompanied (79.9%) and accompanied (20.1%) refugee minors were recruited in five studies in southern Germany. PTSD symptoms were assessed using the Child and Adolescent Trauma Screen (CATS). The network was estimated using state-of-the-art regularized partial correlation models using the R-package qgraph.
Results: The most central symptoms were nightmares, physiological and psychological reactivity, and concentration problems. The strongest connections between symptoms were established for psychological and physiological reactivity, irritability/anger and self-destructive/reckless behaviour, intrusions and nightmares, nightmares and sleep disturbance, and between concentrations problems and sleep disturbance.
Conclusion: This study furnishes information relevant to research and the clinical management of PTSD in refugee minors, and also in terms of comparisons with trauma-exposed children and adolescents without a migration background. Re-experiencing symptoms seem to be central in the refugee minor PTSD profile and thus merit special consideration in the diagnostic and treatment evaluation process. Investigating the PTSD network longitudinally and complementing between-subject analyses with within-subject ones might provide further insight into the symptomatology of refugee minors and how to treat them successfully.
HIGHLIGHTS
• This multisite study is the first network analysis involving refugee minors resettled in Europe that investigates their DSM-5 PTSD symptoms.• The study includes a large, heterogeneous and representative refugee minor sample of varying ages, trauma types, and cultural backgrounds from many countries around the globe.• Re-experiencing symptoms such as nightmares and sleeping difficulties seem to play a crucial role in this vulnerable cohort.
Antecedentes: Dado el número sin precedentes de menores traumatizados refugiados en Europa y la prevalencia aumentada de trastornos mentales tales como el TEPT en esta población vulnerable, nuevas metodologías que nos ayuden a una mejor comprensión de su sintomatologiía son cruciales. El análisis de redes podría ayudar a los clínicos, tanto para comprender qué síntomas podrían gatillar otros síntomas y para identificar blancos relevantes para el tratamiento. Sin embargo, a la fecha sólo dos estudios han aplicado la aproximación de análisis de redes a una población de refugiados (adultos) y sólo tres estudios examinaron esta aproximación en niños y adolescentes.
Objetivo: El objetivo de este estudio es explorar la estructura de redes y centralidad de los síntomas de TEPT del DSM-5 en una muestra transversal de menores refugiados severamente traumatizados.
Método: Fueron recrutados un total de N= 419 (edad M= 16.3; 90,7% masculino) menores refugiados en cinco estudios en el sur de Alemania, no acompañados (79,9%) y acompañados (20,1%). Los síntomas de TEPT fueron evaluados usando el Tamizaje de Trauma para niños y adolescentes (CATS por sus siglas en inglés). La red se estimó utilizando modelos de correlación parcial regularizados de última generación utilizando el gráfico de paquete R.
Resultados: Los síntomas más centrales fueron las pesadillas, la reactividad fisiológica y psicológica y los problemas de concentración. Las conexiones más potentes entre síntomas estuvieron establecidas por la reactividad psicológica y fisiológica, la irritabilidad/rabia y conducta autodestructiva/impulsiva, intrusiones y pesadillas, pesadillas y alteraciones del sueño, y entre problemas de concentración y alteraciones del sueño.
Conclusión: Este estudio proporciona información relevante para la investigación y el manejo clínico del TEPT en menores refugiados, y también en términos de comparaciones con niños y adolescentes expuestos a trauma sin antecedentes de migración. Los síntomas de re-experimentación parecen ser centrales en el perfil de TEPT en los menores refugiados y por lo tanto merece una consideración especial en el proceso de evaluación diagnóstica y el tratamiento. La investigación longitudinal de la red del TEPT y la complementación de los análisis entre sujetos con los de otro sujeto podrían proporcionar una mayor comprensión de la sintomatología de los menores refugiados y cómo tratarlos en forma exitosa.
背景:鉴于欧洲受到心理创伤的未成年难民数量空前,且这一弱势群体中PTSD等精神疾患的患病率升高,有利于我们更好地了解其症候学的新方法至关重要。网络分析可以帮助临床医生了解哪些症状可能引发其他症状,并确定相应的治疗靶点。然而,到目前为止,只有两项研究将网络分析方法应用于(成人)难民群体,只有三项研究在儿童和青少年中检验了这种方法。
目标:本研究的目标是在一个受到严重心理创伤的未成年难民横断面样本中,探讨DSM-5下PTSD症状的网络结构和中心性。
方法:在德国南部的五项研究中总共入组419名无人陪伴(79.9%)和有人陪伴(20.1%)未成年难民(平均年龄 = 16.3; 90.7%为男性)。使用《儿童和青少年创伤筛查量表》(CATS)评估PTSD症状。使用R程序包qgraph并用最新的正则化偏相关模型估计网络。
结果:最核心的症状是噩梦、生理和心理反应及注意力问题。症状间最强的关联建立于心理反应与生理反应,易激惹/愤怒与自毁/鲁莽行为,闯入与噩梦,噩梦与睡眠不安,以及注意力问题与睡眠不安之间。
结论:本研究为未成年难民PTSD的研究和临床管理,以及与无移民背景的创伤暴露儿童和青少年的比较提供了相关信息。再体验症状似乎是未成年难民PTSD剖面的核心,因此在诊断和治疗评估过程中值得特别考虑。纵向探究PTSD网络并在个体间分析中补充个体内分析,可以为未成年难民的症候学以及如何成功治疗他们提供更深入的了解。
1. Introduction
In 2018, nearly 190,000 children and adolescents in migration were deemed to first-time applicants for asylum in the European Union, including some 20,000 unaccompanied minors (Eurostats, Citation2019). In Germany alone, 78,270 refugee minors applied for asylum in 2018 and 18,894 refugee minors between January and March 2019 (Federal Office for Migration and Refugees, Citation2019). A growing body of research on the trauma history of accompanied and unaccompanied refugee minors demonstrates that they experience numerous (interpersonal) traumatic events pre-, peri- and post-migration (Jensen, Skårdalsmo, & Fjermestad, Citation2014; Müller, Büter, Rosner, & Unterhitzenberger, Citation2019). A recent study on unaccompanied refugee minors in Germany showed that 98% reported having experienced at least one potentially traumatic event (Walg, Fink, Grossmeier, Temprano, & Hapfelmeier, Citation2017). As a consequence, refugee minors often develop stress- or trauma-related disorders. In addition to high rates of depression and anxiety, 40–60% of refugee minors resettled in western countries present clinically elevated posttraumatic stress disorder (PTSD) symptoms (Fazel, Wheeler, & Danesh, Citation2005; Reavell & Fazil, Citation2017). However, when admitted to psychiatric care, refugee minors often predominantly report sleep disturbances (Hjern, Angel, & Höjer, Citation1991; Montgomery & Foldspang, Citation2001). The association between sleep problems and other posttraumatic stress symptoms (PTSS) such as intrusions (especially nightmares) has not, however, been investigated up to now in refugee minors.
Refugees’ PTSS often persist for months and years (Jensen, Skar, Andersson, & Birkeland, Citation2019; Kaltenbach, Schauer, Hermenau, Elbert, & Schalinski, Citation2018; Vervliet, Lammertyn, Broekaert, & Derluyn, Citation2014). They have a major negative impact on their integration into the host society, partly because insufficient trauma recovery may result in academic and behavioural problems (Dye, Citation2018). Compared to children and adolescents living in Europe and other western societies without a migration background, refugee minors report higher rates of traumatic events and internalizing symptoms such as PTSS (Bean, Derluyn, Eurelings-Bontekoe, Broekaert, & Spinhoven, Citation2007; Fazel & Stein, Citation2002; Huemer et al., Citation2011). Differences in the PTSD symptom profile between refugee and non-refugee minor populations have, however, scarcely been researched up to now. Hence, we need a new methodological perspective to secure better understanding of the symptom picture, the role of sleep disturbances, and the connectivity between PTSD symptoms in refugee minors, also compared to non-migration samples. The network analysis approach might be one way of generating new insights into the PTSD symptoms of refugee minors.
The network analysis is an emerging methodology for investigating the associations of symptoms in mental disorders. The network approach is a graphical theory-based methodology which can be used to analyse the network structure between variables, such as symptoms (Borsboom & Cramer, Citation2013). Contrary to current nosological systems which assume a latent contributory factor to the symptoms, such as the DSM-5 (American Psychiatric Association, Citation2013) or the ICD-11 (World Health Organization [WHO], Citation2018), this approach assumes that symptoms are mutually dependent and thus influence one another. A growing number of studies have investigated the PTSD symptom profile in clinical samples with adults (Armour, Fried, Deserno, Tsai, & Pietrzak, Citation2017; McNally, Heeren, & Robinaugh, Citation2017; Mitchell et al., Citation2017). Refugees, however, experience very specific clusters and an especially high dosage of traumatic events. They have to adjust during flight and refuge, to a number of different host countries and societies and, in the case of unaccompanied minors, without the support of parents and other close family members. To date, only two studies have applied the network analysis approach to a refugee population. A cross-cultural multisite study by Fried et al. (Citation2018) investigated the PTSD network in four traumatized patient samples receiving treatment, among them N = 956 refugees with a permanent residence in Denmark. They found that that four pairs of symptoms showed especially high connections: intrusions and flashbacks; avoidance of thoughts and avoidance of situations; sleeping problems and nightmares; and irritability and startle response. Detachment, intrusions, psychological reactivity and concentration problems had the highest centrality and trauma-related amnesia the lowest. Spiller et al. (Citation2017) also investigated the PTSD symptom structure in a clinical sample of traumatized adult refugees. However, due to the small sample size (N = 151), the study has low power and limited robustness. The findings of this study are therefore rather hard to interpret and need to be replicated.
Network analysis literature on children and adolescents suffering from PTSD is scarce (Cao et al., Citation2019; de Haan et al., Citationin press; Russell, Neill, Carrión, & Weems, Citation2017). A recent study by Bartels et al. (Citation2019) found that in an international sample of 7–17-year-old traumatized children and adolescents (N = 475; heterogeneous but mostly interpersonal trauma) living in western countries, the most central symptoms were intrusions, negative trauma-related cognitions and persistent negative emotional state. The authors further found that symptoms in the negative alterations in cognitions and mood DSM-5 cluster have emerged as key drivers of other PTSD symptoms. Sleep disturbance did not seem to play a central role in the symptom network of traumatized children and adolescents without a refugee background. Most refugee minors resettled in western countries report having experienced various types of interpersonal trauma (Pfeiffer & Goldbeck, Citation2017; Pfeiffer, Sachser, Rohlmann, & Goldbeck, Citation2018) as well, but they came originally from Middle Eastern and African countries. Comparing the results of the network analysis of Bartels et al. (Citation2019) with a network analysis of refugee minors might, therefore, lead to new insights into the impact of culture and migration on PTSD symptomatology in children and adolescents.
The aim of this study is, therefore, to explore the network structure and centrality indices of DSM-5 PTSD symptoms in a heterogeneous cross-sectional multisite clinical sample of more than 400 severely traumatized refugee minors resettled in Germany.
2. Methods
2.1. Sample and study designs
Participants were recruited in five studies in Germany (Müller et al., Citation2019; Pfeiffer & Goldbeck, Citation2017; Pfeiffer et al., Citation2018; Sukale, Rassenhofer, Plener, & Fegert, Citation2016; Unterhitzenberger, Wintersohl, Lang, König, & Rosner, Citation2019). The inclusion criteria for this study were (1) refugee resettled in a European country, (2) aged between 7 and 21, (3) at least one potentially traumatic event in line with the DSM-5 definition, and (4) information provided on the Child and Adolescent Trauma Screen (CATS; Sachser et al., Citation2017) symptom checklist.
This study included baseline data on refugee minors from the following five studies conducted in Germany. In study 1 refugee minors were assessed regarding their psychopathology, resources and treatments received in Germany (data collection: August 2017 – today) (Sukale et al., Citation2016). In study 2 refugee minors were assessed regarding their psychopathology in Bavaria, southern Germany (data collection: April – September 2017) (Müller et al., Citation2019). The aim of study 3 was to evaluate the feasibility and effectiveness of the trauma-focused group intervention ‘Mein Weg’ (English ‘My Way’) in an uncontrolled pre-post pilot study design (data collection: January-April 2016) (Pfeiffer & Goldbeck, Citation2017). The aim of study 4 was to evaluate the intervention ‘Mein Weg’ in comparison to a usual care condition in a single-blind parallel-group randomized controlled trial (RCT) (data collection: November 2016- July 2017) (Pfeiffer et al., Citation2018; Pfeiffer, Sachser, Tutus, Fegert, & Plener, Citation2019). The aim of study 5 was to evaluate the evidence-based treatment trauma-focused cognitive behavioural therapy (TF-CBT) (Cohen, Mannarino, & Deblinger, Citation2016) with refugee minors in Bavaria in an uncontrolled pre-post pilot study design (data collection: January 2016 - July 2018) (Unterhitzenberger et al., Citation2019).
The respective studies were approved by the ethics committees at all participating sites (ethics committee at the University of Ulm (#176/16 and #159/16) and the ethics committee at the Catholic University of Eichstätt-Ingolstadt (2016/23 and 2015/02/16). Prior to the assessment all participants and their legal guardians, in the case of minors, were informed about the respective study protocol and gave their informed written consent.
2.2. Measures
The Child and Adolescent Trauma Screen (CATS) (Sachser et al., Citation2017) assesses individual trauma history using an Event Checklist of 15 potentially traumatic events, and the frequency of each of the 20 posttraumatic stress symptoms (PTSS), based on DSM-5 criteria (American Psychiatric Association, Citation2013) using a 4-point response scale ranging from 0 = ‘never’ to 3 = ‘almost always’. In studies 1, 3 and 4 professional forward-backward translations into the mother tongue of the participants were used. In studies 2 and 5 professional translators translated the German CATS into the respective language during assessment. Within the current sample, the measure showed good reliability indicated by Cronbach’s α = 0.89.
Demographic information (gender, age, country of origin, accompanied/unaccompanied) was assessed in each study separately using non-standardized measures.
2.3. Statistical analyses
The statistical analyses were conducted in three steps: (1) inspection of descriptive statistics, (2) network estimation and (3) network stability. Networks were estimated using state-of-the-art regularized partial correlation models using the R environment. For the 20-item PTSD symptom network, we were interested in examining which symptoms show strong associations and which symptoms are central in the network. Therefore, the strength centrality metric was used. Strength centrality combines all edges of a given symptom with all other symptoms, and then estimates how strongly a node is directly connected with the network. Accuracy and stability estimations were carried out to test whether the results obtained by the regularized partial correlation models are stable. We used the R environment for all analyses (R version 3.6.0). The dataset used for this study did not contain any missing values.
2.3.1. Network estimation
The symptom network was estimated using a Gaussian Graphical Model (GGM; Lauritzen, Citation1996), in which edges (associations between symptoms) represent estimations of partial correlations between nodes (symptoms). Whenever two symptoms are connected in the resulting network, they are dependent after controlling for the connections to all other symptoms in the network. For the emerging network which includes 20 DSM-5 PTSD symptoms, 190 pairwise association parameters were estimated. To estimate the network, edges were calculated based on polychoric correlations as psychopathological symptoms can be considered to be ordered categorically. In order to identify only relevant edges and to control for what are known as ‘spurious connections’ (false positive connections), we applied the least absolute shrinkage and selection operator (LASSO; Friedman, Hastie, & Tibshirani, Citation2008; Tibshirani, Citation1996). It shrinks very small edges to zero. The tuning parameter (λ) was selected empirically by applying the Extended Bayesian Information Criterion (EBIC). A detailed tutorial on how to perform this procedure can be found elsewhere (Epskamp & Fried, Citation2018). To quantify the importance of each symptom (node) in the network, previous studies had computed the centrality indices strength, closeness, and betweenness. However, recent network analysis revealed an unreliable estimation of betweenness and closeness (Armour et al., Citation2017; McNally et al., Citation2017; Mitchell et al., Citation2017). As this was also the case in our study we followed the approach of Fried et al. (Citation2018) and report node strength only. Additionally the predictability of each node, which explains the shared variance of each node with all of its direct neighbours (Haslbeck & Fried, Citation2017), was estimated using the R-package mgm (Haslbeck & Waldorp, Citation2018). Strength and predictability both reflect the connectedness of a node within the network. However, whereas centrality can be seen as a relative metric of how interconnected a node is in the network, predictability can be understood as an absolute measure of interconnectedness and gives us an idea of how clinically relevant the connections are (Haslbeck & Fried, Citation2017). Predictability is also interpreted as an upper bound to controllability and quantifies how much the symptom node can be influenced by intervening in all of its neighbours.
2.3.2. Network stability
To estimate the stability of the network we followed the procedure suggested by Epskamp, Borsboom, and Fried (Citation2018). The R package bootnet was used to investigate the stability of the network. 95% confidence intervals were bootstrapped around the edge weights and the correlation-stability coefficient (cs-coefficent) for the strength centrality metric was estimated (cs-coefficent range 0–1; values > 0.25 imply moderate stability; values > 0.5 strong stability). As a last step, we computed the edge-weights difference test and the centrality difference test for our DSM-5 PTSD symptom network. The strength centrality metric and the predictability metric showed a high correlation (ρs = .91), which reflects their conceptual closeness.
2.3.3. Identification of symptoms underlying the same construct or process
To test whether the strongest associations between symptoms are likely to measure the same underlying construct (i.e. are collinear), we used the goldbricker function within the R package networktools (Jones, Citation2018) to identify potential pairs of nodes that are both correlated strongly with each other and correlate in highly similar patterns with other nodes (topological overlap). We were looking for pairs of items (nodes) that were strongly intercorrelated (r > .50) and were sharing a topological overlap of greater than 75% ((i.e. less than 25% of significantly divergent dependent correlations, p = 0.05) (Bernstein, Heeren, & McNally, Citation2019)).
We further conducted the modularity-based community detection analysis using the spinglass algorithm and exploratory graph analyses to test whether nodes cohere a single large network or, in contrast, emerge as distinct subnetworks that correspond to specialized functional groups of nodes. A description of the analysis and the results can be found in supplementary materials (SM6).
3. Results
3.1. Sample description
Altogether the data from N = 419 refugee minors (study 1: n = 155, 37.0%; study 2: n = 97, 23.2%; study 3: n = 23, 5.5%; study 4: n = 97, 23.2%; study 5: n = 47, 11.2%) were included in the network analysis. Most of the participants were male (n = 379, 90.7%) and unaccompanied (n = 334, 79.9%). They were on average 16.3 (SD = 1.82, range 8–21) years old and had been in Germany for 14.05 months (SD = 12.04, range: 1–60). The countries of origin were heterogeneous (see tables A and B in supplementary materials (SM)) with most participants being born in Afghanistan (n = 176, 42.0%). The participants had experienced on average 7.47 traumatic events (SD = 2.99, range 0–15; see table C in SM for more information). The average CATS sum score was 27.18 (SD = 11.38, clinical cut-off ≥ 21, range 0–60) indicating an overall clinical sample.
3.2. Network analysis
3.2.1. Network estimation
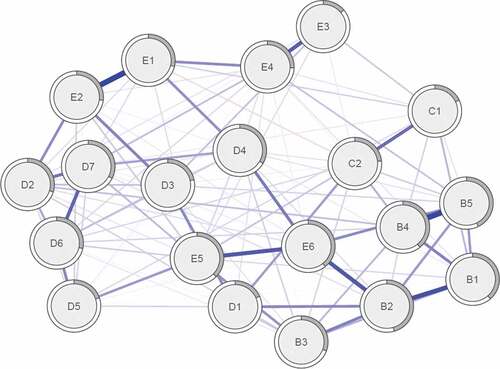
gives the estimated network of the 20 DSM-5 PTSD symptoms. The network resulted in 117/190 non-zero edges, which indicates substantial connections between these symptoms. All associations, with the exception of the connection between E2 irritability/anger and C2 external avoidance within the network structure, were positive. The strongest edges emerged between psychological reactivity (B4) and physiological reactivity (B5), irritability/anger (E1) and self-destructive/reckless behaviour (E2), and between intrusions (B1) and nightmares (B2). Additionally, strong connections were found between nightmares (B2) and sleep disturbance (E6), and between concentrations problems (E5) and sleep disturbance (E6). gives the standardized strength centrality for all 20 DSM-5 PTSD symptoms. The symptoms nightmares (B1), psychological reactivity (B4), physiological reactivity (B5), and concentration problems (E5) revealed the highest strength metric in our network. The average predictability of nodes was 0.34, which indicates that on average 34% of the variation in one node is explained by its direct neighbouring nodes. The predictability of each symptom is shown in and presented as a graph in .The symptoms nightmares (B2), physiological reactivity (B5), psychological reactivity (B4) and sleep disturbance (E6) showed the highest predictability (0.46, 0.43, 0.39 and 0.39).
Table 1. Overview of the 20 DSM-5 posttraumatic stress disorder symptoms. Means, standard deviations and strength centrality and predictability.
Figure 1. Estimated regularized partial correlation network of the 20 DSM-5 PTSD symptoms (n = 419). The thickness and saturation of an edge are an indicator for the strength of the associations between symptoms. The grey area in the rings around the nodes depicts predictability; the variance of a given node explained by all its neighbours. B1 = ”Intrusive thoughts or memories”; B2 = ‘Nightmares’; B3 = ‘Flashbacks’; B4 = ‘Psychological reactivity’; B5 = ‘Psychological reactivity’; C1 = ‘Avoidance of internal reminders’; C2 = ‘Avoidance of external reminders’; D1 = ‘Amnesia’; D2 = ‘Negative trauma-related cognitions’; D3 = ‘Distorted blame’; D4 = ‘Persistent negative emotional state’; D5 = ‘Diminished interest in activities’; D6 = ‘Detachment from others’; D7 = ‘Restricted affect’; E1 = ‘Irritability/Anger’; E2 = ‘Self-destructive or reckless behaviour’; E3 = ‘Hypervigilance’; E4 = ‘Startle Response’; E5 = ‘Concentration problems’; E6 = ‘Sleep disturbance’. Maximum edge value = .43.
3.2.2. Network stability
There are no clear boundaries for the interpretation of the stability analyses (see SM1). The correlation stability coefficient (CS [cor = .7] = .52) for the strength centrality metric exceeded the recommended cut-off of .5 by Epskamp et al. (Citation2018) and thus suggested a reliable estimation. The confidence intervals around the edge weights were large and most of the confidence intervals overlapped, indicating that their order should be interpreted with caution (see SM2). Additionally, we tested whether edges differed significantly from one another in their strength (see SM3), and whether symptoms differed in their node strength (see SM4). The results indicate that many of the symptoms did not differ significantly in strength. The results of the stability analyses are given in the SM.
3.2.3. Symptoms underlying the same construct or process
The identification of symptoms with a topological overlap revealed that there were 6 pairs of symptoms that may have a high conceptual overlap and may be better explained as multiple measurements of the same process or construct: Intrusions (B1) and nightmares (B2), intrusions (B1) and psychological reactivity (B4), intrusions (B1) and physiological reactivity (B5), psychological reactivity (B4) and physiological reactivity (B5), concentration problems (E5) and sleep disturbance (E6), and lastly irritability/anger (E1) and self-destructive/reckless behaviour (E2).
4. Discussion
We conducted a network analysis of symptoms of DSM-5 PTSD in a sample of 419 refugee minors exposed to traumatic events. To our knowledge, this cross-cultural multisite study is the first network analysis with refugee minors resettled in Europe that includes a heterogeneous study sample of varying ages, trauma types, and cultural backgrounds from many countries around the globe.
Generally speaking, connections between symptoms were positive with only one exception (irritability/anger (E2) – external avoidance (C2)). On closer inspection of the data, we found that the pairwise correlation matrix did not, in fact, have any negative associations. This unexpected negative relationship might, therefore, indicate common effect structures. Given their independent connection to the same variable, two unrelated items may display an artificial negative partial correlation (Epskamp & Fried, Citation2018). Except for the connection between nightmares and sleeping difficulties, the strongest connections (edges) were in fact within the same clusters (re-experiencing and hyperarousal).
Although this analysis was conducted with a somewhat heterogeneous sample of children and adolescents with a refugee background from various countries and cultures, the stability coefficient of the network suggested a reliable estimation (CS = .52). This estimation is comparable to the studies by Fried et al. (Citation2018) (DataSet 4: CS = .52), Bartels et al. (Citation2019) (CS = 0.67) and Cao et al. (Citation2019) (CS = .52/.59) and even higher compared to the study by de Haan et al. (Citationin press) (CS = .44) which had the largest sample of traumatized children and adolescents. The average predictability across all nodes was 0.34, indicating 34% of the variance of a node that is not predicted by the intercept model is explained by its neighbours. Compared with predictability results of other network analysis (Haslbeck & Fried, Citation2017), this is an average level of predictability.
The PTSD symptoms nightmares (B2), physiological and psychological reactivity at confrontation (B4, B5), and concentration problems (E5) stood out as highly connected symptoms in refugee minors exposed to traumatic events (strength and predictability). Similar findings were reported by Fried et al. (Citation2018) with adult refugees who found that intrusions and psychological reactivity were among the most central symptoms. These findings support the studies by Cao et al. (Citation2019) and de Haan et al. (Citationin press) who found that symptoms of PTSD re-experiencing were most central in traumatized children and adolescents. Hence, in line with our findings, most discussed studies had found that psychological and physical reactivity/distress when confronted with trauma reminders seem to be particularly important in paediatric PTSD. Since these symptoms will not be captured in ICD-11 PTSD, this finding encourages the clinician to still include the symptoms in clinical assessment and treatment monitoring as they seem to measure different aspects of important underlying processes. The investigation of conceptual overlaps between symptoms further supports this point, as the analysis revealed that the symptoms in the DSM-5 PTSD re-experiencing cluster (except flashbacks) may have a high conceptual overlap and may be better explained as multiple measurements underlying the same construct. This high topological overlap was also found for the symptom pairs concentration problems (E5) and sleep disturbance (E6), as well as irritability/anger (E1) and self-destructive/reckless behaviour (E2).
Beside psychological reactivity (B4), Bartels et al. (Citation2019), however, found the highest centrality for trauma-related cognitions (D2) and persistent negative emotional state (D4) (self- and caregiver report) in children and adolescents who also mostly suffered from interpersonal trauma, but did not have a migration background. The authors, therefore, conclude that symptoms within the DSM-5 D-cluster are key drivers of the symptom network. Our analysis could not back this finding as the most central symptom within this cluster was restricted affect (D7; 0.64). Since Bartels et al. (Citation2019) used the same measure, the same PTSD definition and a comparable sample that suffered mostly from interpersonal trauma, this difference is quite surprising. It is all the more surprising as the symptoms within the D-cluster can partially be allocated to depression which is, in fact, a highly comorbid diagnosis in refugee minors and traumatized children and adolescents in general. An explanation for this finding might be that compared to the sample of Bartels et al. (Citation2019), our sample has a migration background and mostly originates from non-western societies. Symptoms within the D-cluster, such as trauma-related cognitions, might not only be more difficult to assess in refugee minors due to the language barrier, but also be represented differently in eastern cultures. We know, for example, that feelings such as guilt and shame are experienced differently and reported in collectivistic versus individualistic cultures (Bierbrauer, Citation1992). Hence, when assessing PTSD in refugees, clinicians need to keep the individual’s cultural background in mind and consider employing cultural mediators in order to get a better understanding of trauma-related cognitions and feelings.
In line with our findings, problems with concentration (E5) had emerged as a central symptom in various network analyses involving refugees (Fried et al., Citation2018) and children and adolescents (Cao et al., Citation2019; de Haan et al., Citationin press; Russell et al., Citation2017). This might, in fact, be explained by the fact that concentration difficulties can also be considered a symptom of depression and depression is the most frequent comorbid diagnosis in children and adolescents suffering from PTSD (Smith, Dalgleish, & Meiser‐Stedman, Citation2019), especially refugees (Fazel et al., Citation2005).
Regarding the role of sleep disturbances (E6), we did not find this symptom to be particularly central within the network, according to the centrality metric. However, sleep disturbances showed a high predictability within the network (0.39) and did rank among the symptoms with the strongest connection to other symptoms in the network. They were especially strongly connected to concentration problems and nightmares which are, in turn, central symptoms of the network. This is in line with Fried et al. (Citation2018) who found a particularly strong connection between sleep problems and nightmares in adult refugees. Hence, when refugee minors are admitted to psychiatric care due to predominantly sleeping difficulties, the clinician should specifically assess nightmares and concentration problems at school or work and monitor these symptoms closely throughout diagnostics and/or treatment as they might indicate that the young refugee suffers from PTSD.
4.1. Limitations and future research
Several limitations of this analysis need to be addressed in the following. Firstly, this study was conducted solely with cross-sectional data. Although network theory implies causal relations between symptoms, these cannot be confirmed without longitudinal data. Hence, with these results we cannot draw conclusions such as nightmares lead to sleep disturbances and sleep disturbances lead, in turn, to concentration problems. We can only say that sleep disturbances are strongly associated with nightmares and concentration problems, which is plausible, especially from a clinical perspective. Secondly, we only used self-report questionnaire data with a single measurement of PTSD. Although the measure showed good reliability (Cronbach’s α = 0.89), we observed sufficient stability of the network (CS = .52), and most network analyses on children and adolescents have employed questionnaire data, future research should include clinical interviews. We decided not to include caregiver rated symptoms in this analysis as preceding studies revealed that there are low correlations between self-and caregiver-rated PTSS in unaccompanied refugee minors (Derluyn & Broekaert, Citation2007; Pfeiffer et al., Citation2018). Thirdly, we did not control for possible confounding factors such as time since trauma or frequency of reported trauma, because the CATS does not provide information on this. Additionally the study only investigated the symptom network of the 20 DSM-5 PTSD symptoms. In a next step, researchers might include non-symptom variables (e.g. cognitive, biological or social variables) in a hybrid network model, as non-symptoms likely play a causal role in mental disorders (Jones, Heeren, & McNally, Citation2017). Fourthly, although Article 1 of the ‘Convention on the Rights of the Child’ defines minors as children from birth to 17 years of age, we included young refugees up to an age of 21 in this analysis, because they were still living in child welfare facilities (main place of recruitment) and were, therefore, treated like refugee minors in Germany. Moreover, within the German mental health care system, refugees up to an age of 21 are treated in child and adolescent mental hospitals. Fifthly, the study sample mainly included unaccompanied male refugee minors as they mainly represented the refugee minor population in German child welfare programmes at the time of recruitment. A separate analysis of unaccompanied/accompanied or female/male refugee minors was not possible due to the small sample sizes. These findings need to be replicated with more accompanied and/or female refugee minors. In fact, future research in this field should generally focus on replications of network analyses, not only in refugees, but also across different populations of traumatized children and adolescents. Investigating the PTSD network longitudinally and complementing between-subject analyses with within-subject ones might provide further insight into the symptomatology of refugee minors, and how to treat it successfully. Additionally, future network analysis should include a broader range of symptoms, especially depression and anxiety symptoms, to gain insights into potential bridge symptoms between the patterns of trauma-related disorders that are still viewed as distinct.
5. Conclusion
Overall, our results generate new insights to the symptomatology, persistence, and treatment of PTSD in refugee minors, from a network perspective. This study is able to add relevant information for the research and clinical management of PTSD in refugee minors, also compared to trauma-exposed children and adolescents without a migration background. Symptoms of re-experiencing seem to be central in the refugee minor PTSD profile and thus merit special consideration in the diagnostic and treatment evaluation process. Especially because the ICD-11 approach will not include psychological and physiological reactivity within the re-experiencing cluster, clinicians should keep these symptoms in mind. Additionally, sleep disturbances are highly associated with nightmares, concentration problems and other PTSD symptoms. This indicates that when refugee minors are presented to clinicians in the (mental) health care system due to sleeping difficulties, a screening for PTSD might be at least indicated. On a societal level, our findings highlight the need to further improve the access to and financing of mental health care services for accompanied and unaccompanied refugee minors, especially since we already know that people with PTSD also often struggle with interpersonal problems and several mental and physical health comorbidities, which in the end might prevent them from successfully integrating into the host society.
Data availability
The data are available upon request from the authors.
Supplemental Material
Download MS Word (583 KB)Disclosure statement
The authors have nothing to disclose.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5). Arlington: American Psychiatric Publishing.
- Armour, C., Fried, E. I., Deserno, M. K., Tsai, J., & Pietrzak, R. H. (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. Journal of Anxiety Disorders, 45, 49–10.
- Bartels, L., Berliner, L., Holt, T., Jensen, T., Jungbluth, N., Plener, P., … Sachser, C. (2019). The importance of the DSM‐5 posttraumatic stress disorder symptoms of cognitions and mood in traumatized children and adolescents: Two network approaches. Journal of Child Psychology and Psychiatry, 60(5), 545–554.
- Bean, T., Derluyn, I., Eurelings-Bontekoe, E., Broekaert, E., & Spinhoven, P. (2007). Comparing psychological distress, traumatic stress reactions, and experiences of unaccompanied refugee minors with experiences of adolescents accompanied by parents. The Journal of Nervous and Mental Disease, 195(4), 288–297.
- Bernstein, E. E., Heeren, A., & McNally, R. J. (2019). Reexamining trait rumination as a system of repetitive negative thoughts: A network analysis. Journal of Behavior Therapy and Experimental Psychiatry, 63, 21–27.
- Bierbrauer, G. (1992). Reactions to violation of normative standards: A cross-cultural analysis of shame and guilt. International Journal of Psychology, 27(2), 181–193.
- Borsboom, D., & Cramer, A. O. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121.
- Cao, X., Wang, L., Cao, C., Fang, R., Chen, C., Hall, B. J., & Elhai, J. D. (2019). Sex differences in global and local connectivity of adolescent posttraumatic stress disorder symptoms. Journal of Child Psychology and Psychiatry, 60(2), 216–224.
- Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2016). Treating trauma and traumatic grief in children and adolescents. New York: Guilford.
- de Haan, A., Landolt, M. A., Fried, E. I., Kleinke, K., Alisic, E., Bryant, R., … Meiser-Stedman, R. (in press). Dysfunctional posttraumatic cognitions, posttraumatic stress, and depression in children and adolescents exposed to trauma: A network analysis. Journal of Child Psychology and Psychiatry.
- Derluyn, I., & Broekaert, E. (2007). Different perspectives on emotional and behavioural problems in unaccompanied refugee children and adolescents. Ethnicity and Health, 12(2), 141–162.
- Dye, H. (2018). The impact and long-term effects of childhood trauma. Journal of Human Behavior in the Social Environment, 28(3), 381–392.
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212.
- Epskamp, S., & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23(4), 617–634.
- Eurostats. (2019). Asylum and managed migration. Retrieved from https://ec.europa.eu/eurostat/web/asylum-and-managed-migration/data/database
- Fazel, M., & Stein, A. (2002). The mental health of refugee children. Archives of Disease in Childhood, 87(5), 366–370.
- Fazel, M., Wheeler, J., & Danesh, J. (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. The Lancet, 365(9467), 1309–1314.
- Federal Office for Migration and Refugees. (2019). Current statistics [Aktuelle Zahlen]. Retrieved from http://www.bamf.de/SharedDocs/Anlagen/DE/Downloads/Infothek/Statistik/Asyl/aktuelle-zahlen-zu-asyl-maerz-2019.pdf?__blob=publicationFile
- Fried, E. I., Eidhof, M. B., Palic, S., Costantini, G., Huisman-van Dijk, H. M., Bockting, C. L., … Karstoft, K. I. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351.
- Friedman, J., Hastie, T., & Tibshirani, R. (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics, 9(3), 432–441.
- Haslbeck, J. M., & Waldorp, L. J. (2018). How well do network models predict observations? On the importance of predictability in network models. Behavior Research Methods, 50(2), 853–861.
- Haslbeck, J. M. B., & Fried, E. I. (2017). How predictable are symptoms in psychopathological networks? A reanalysis of 18 published datasets. Psychological Medicine, 47(16), 2767–2776.
- Hjern, A., Angel, B., & Höjer, B. (1991). Persecution and behavior: A report of refugee children from Chile. Child Abuse & Neglect, 15(3), 239–248.
- Huemer, J., Karnik, N., Voelkl-Kernstock, S., Granditsch, E., Plattner, B., Friedrich, M., & Steiner, H. (2011). Psychopathology in African unaccompanied refugee minors in austria. Child Psychiatry & Human Development, 42(3), 307–319.
- Jensen, T. K., Skar, A. S., Andersson, E. S., & Birkeland, M. S. (2019). Long-term mental health in unaccompanied refugee minors: Pre- and post-flight predictors. European Child and Adolescent Psychiatry. doi:10.1007/s00787-019-01340-6
- Jensen, T. K., Skårdalsmo, E. M. B., & Fjermestad, K. W. (2014). Development of mental health problems-a follow-up study of unaccompanied refugee minors. Child and Adolescent Psychiatry and Mental Health, 8(1), 29–39.
- Jones, P. (2018). Networktools: Tools for identifying important nodes in networks. R package version 1.2.1. J. Retrieved form https://CRAN.R-project.org/package=networktools
- Jones, P. J., Heeren, A., & McNally, R. J. (2017). Commentary: A network theory of mental disorders. Frontiers in Psychology, 8, 1305.
- Kaltenbach, E., Schauer, M., Hermenau, K., Elbert, T., & Schalinski, I. (2018). Course of mental health in Refugees—A one year panel survey. Frontiers in Psychiatry, 9, 352.
- Lauritzen, S. L. (1996). Graphical models (Vol. 17). Oxford Statistical Science Series. Oxford: Clarendon.
- McNally, R. J., Heeren, A., & Robinaugh, D. J. (2017). A bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. European Journal of Psychotraumatology, 8(sup3), 1341276.
- Mitchell, K. S., Wolf, E. J., Bovin, M. J., Lee, L. O., Green, J. D., Rosen, R. C., … Marx, B. P. (2017). Network models of DSM–5 posttraumatic stress disorder: Implications for ICD–11. Journal of Abnormal Psychology, 126(3), 355–366.
- Montgomery, E., & Foldspang, A. (2001). Traumatic experience and sleep disturbance in refugee children from the Middle East. The European Journal of Public Health, 11(1), 18–22.
- Müller, L. R. F., Büter, K. P., Rosner, R., & Unterhitzenberger, J. (2019). Mental health and associated stress factors in accompanied and unaccompanied refugee minors resettled in germany: A cross-sectional study. Child and Adolescent Psychiatry and Mental Health, 13(8). doi:10.1186/s13034-019-0268-1
- Pfeiffer, E., & Goldbeck, L. (2017). Evaluation of a trauma‐focused group intervention for unaccompanied young refugees: A pilot study. Journal of Traumatic Stress, 30(5), 531–536.
- Pfeiffer, E., Sachser, C., Rohlmann, F., & Goldbeck, L. (2018). Effectiveness of a trauma‐focused group intervention for young refugees: A randomized controlled trial. Journal of Child Psychology and Psychiatry, 59(11), 1171–1179.
- Pfeiffer, E., Sachser, C., Tutus, D., Fegert, J. M., & Plener, P. L. (2019). Trauma-focused group intervention for unaccompanied young refugees: “Mein Weg” - predictors of treatment outcomes and sustainability of treatment effects. Child and Adolescent Psychiatry and Mental Health, 13(18), 1–10.
- Reavell, J., & Fazil, Q. (2017). The epidemiology of PTSD and depression in refugee minors who have resettled in developed countries. Journal of Mental Health, 26(1), 74–83.
- Russell, J. D., Neill, E. L., Carrión, V. G., & Weems, C. F. (2017). The network structure of posttraumatic stress symptoms in children and adolescents exposed to disasters. Journal of the American Academy of Child & Adolescent Psychiatry, 56(8), 669–677.e5.
- Sachser, C., Berliner, L., Holt, T., Jensen, T. K., Jungbluth, N., Risch, E., & Goldbeck, L. (2017). International development and psychometric properties of the child and adolescent trauma screen (CATS). Journal of Affective Disorders, 210, 189–195.
- Smith, P., Dalgleish, T., & Meiser‐Stedman, R. (2019). Practitioner review: Posttraumatic stress disorder and its treatment in children and adolescents. Journal of Child Psychology and Psychiatry, 60(5), 500–515.
- Spiller, T. R., Schick, M., Schnyder, U., Bryant, R. A., Nickerson, A., & Morina, N. (2017). Symptoms of posttraumatic stress disorder in a clinical sample of refugees: A network analysis. European Journal of Psychotraumatology, 8(sup3), 1318032.
- Sukale, T., Rassenhofer, M., Plener, P., & Fegert, J. (2016). Burdens and resources of unaccompanied and accompanied minors with flight experience [Belastungen und Ressourcen unbegleiteter und begleiteter Minderjähriger mit Fluchterfahrung]. Das Jugendamt, 4, 174–183.
- Tibshirani, R. (1996). Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society: Series B (methodological), 58(1), 267–288.
- Unterhitzenberger, J., Wintersohl, S., Lang, M., König, J., & Rosner, R. (2019). Providing manualized individual trauma-focused CBT to unaccompanied refugee minors with uncertain residence status: A pilot study. Child and Adolescent Psychiatry and Mental Health, 13, 22.
- Vervliet, M., Lammertyn, J., Broekaert, E., & Derluyn, I. (2014). Longitudinal follow-up of the mental health of unaccompanied refugee minors. European Child & Adolescent Psychiatry, 23(5), 337–346.
- Walg, M., Fink, E., Grossmeier, M., Temprano, M., & Hapfelmeier, G. (2017). The proportion of unaccompanied refugee minors suffering from psychiatric disorders in Germany [Häufigkeit psychischer Störungen bei unbegleiteten minderjährigen Flüchtlingen in Deutschland]. Zeitschrift Für Kinder- Und Jugendpsychiatrie Und Psychotherapie, 45(1), 58–68.
- World Health Organization. (2018). ICD-11 mortality and morbidity statistics. Retrieved from https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f991786158
