ABSTRACT
Background: Post-traumatic stress disorder (PTSD) is a major cause of morbidity amongst active duty and ex-serving military personnel. In recent years increasing efforts have been made to develop more effective treatments.
Objective: To determine which psychological therapies are efficacious in treating active duty and ex-serving military personnel with post-traumatic stress disorder (PTSD).
Method: A systematic review was undertaken according to Cochrane Collaboration Guidelines. The primary outcome measure was reduction in PTSD symptoms and the secondary outcome dropout.
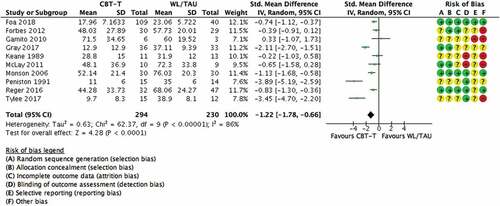
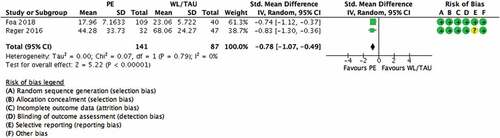
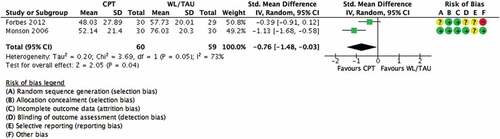
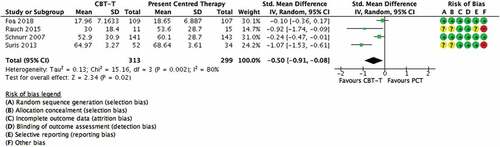
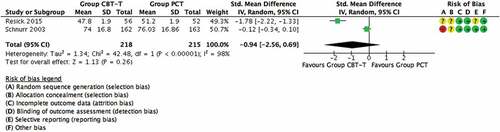
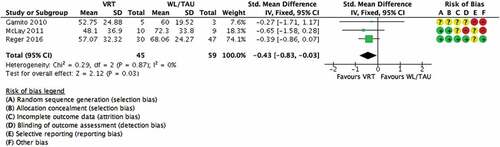
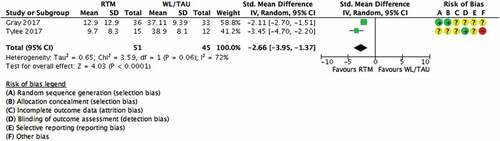
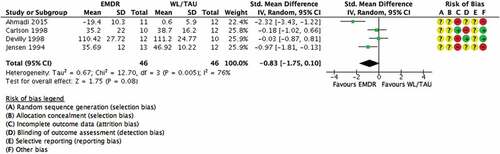
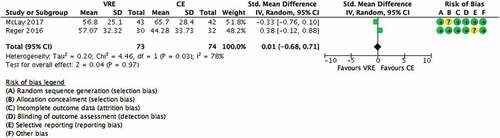
Results: Twenty-four studies with 2386 participants were included. Evidence demonstrated that CBT with a trauma focus (CBT-TF) was associated with the largest evidence of effect when compared to waitlist/usual care in reducing PTSD symptoms post treatment (10 studies; n = 524; SMD −1.22, −1.78 to −0.66). Group CBT-TF was less effective when compared to individual CBT-TF at reducing PTSD symptoms post treatment (1 study; n = 268; SMD −0.35, −0.11 to −0.59). Eye Movement Desensitization and Reprocessing (EMDR) therapy was not effective when compared to waitlist/usual care at reducing PTSD symptoms post treatment (4 studies; n = 92; SMD −0.83, −1.75 to 0.10). There was evidence of greater dropout from CBT-TF therapies compared to waitlist and Present Centred Therapy.
Conclusions: The evidence, albeit limited, supports individual CBT-TF as the first-line psychological treatment of PTSD in active duty and ex-serving personnel. There is evidence for Group CBT-TF, but this is not as strong as for individual CBT-TF. EMDR cannot be recommended as a first line therapy at present and urgently requires further evaluation. Lower effect sizes than for other populations with PTSD and high levels of drop-out suggest that CBT-TF in its current formats is not optimally acceptable and further research is required to develop and evaluate more effective treatments for PTSD and complex PTSD in active duty and ex-serving military personnel.
HIGHLIGHTS
• PTSD is a common psychiatric condition amongst active duty and ex-serving military personnel.• Evidence supports individual CBT-TF as the first-line psychological treatment of PTSD in active duty and ex-serving personnel.• High levels of drop-out suggest that CBT-TF in its current formats of delivery is not optimally acceptable to active duty and ex-serving military personnel.• EMDR currently cannot be recommended as a first line therapy for active duty and ex-serving military personnel and further evaluation is urgently required.
Antecedentes: el trastorno de estrés postraumático (TEPT) es una causa importante de morbilidad entre el personal militar activo y en retiro. En los últimos años se han realizado esfuerzos crecientes para desarrollar tratamientos más efectivos.
Objetivo: determinar qué terapias psicológicas son eficaces en el tratamiento del personal militar en servicio activo y en retiro con trastorno de estrés postraumático (TEPT).
Método: se realizó una revisión sistemática de acuerdo con las Pautas de la Colaboración Cochrane. La medida de resultado primaria fue la reducción de los síntomas de TEPT y la secundaria los abandonos al tratamiento.
Resultados: se incluyeron 24 estudios con 2386 participantes. La evidencia demostró que la Terapia cognitivo conductual centrada en el trauma (TCC-CT) se asoció con la mayor evidencia de efecto en comparación con la lista de espera/atención habitual en la reducción de los síntomas de TEPT después del tratamiento (10 estudios; n = 524; DME -1.22, -1.78 a - 0,66). La TCC-CT grupal fue menos efectivo en comparación con el TCC-CT individual para reducir los síntomas de TEPT después del tratamiento (1 estudio; n = 268; SMD -0.35, -0.11 a -0.59). La terapia de desensibilización y reprocesamiento por movimiento ocular (EMDR) no fue efectiva en comparación con la lista de espera/atención habitual para reducir los síntomas de TEPT después del tratamiento (4 estudios; n = 92; SMD -0.83, -1.75 a 0.10). Hubo evidencia de un mayor abandono de las terapias TCC-CT en comparación con la lista de espera y la terapia centrada en el presente.
Conclusiones: La evidencia, aunque limitada, respalda la TCC-CT individual como el tratamiento psicológico de primera línea del TEPT en el personal militar en servicio activo y en retiro. Existe evidencia de TCC-CT grupal, pero esta no es tan consistente como para TCC-CT individual. No se puede recomendar EMDR como terapia de primera línea en la actualidad y requiere urgentemente una evaluación adicional. Los tamaños de efecto más bajos que para otras poblaciones con TEPT y altos niveles de abandono sugieren que TCC-TC en sus formatos actuales no es óptimamente aceptable y se requiere más investigación para desarrollar y evaluar tratamientos más efectivos para TEPT y TEPT complejo en personal militar en servicio activo y en retiro.
背景:创伤后应激障碍(PTSD)是现役和退役军人的一个主要发病原因。近年来,越来越多的努力投入到开发更有效的治疗方法中。
目的:确定哪种心理疗法可有效治疗患有创伤后应激障碍(PTSD)的现役和退役军人。
方法:系统综述依据Cochrane协作指南进行。主要测量指标是PTSD症状的减轻,次要结果是脱落情况。
结果:入组共24项研究, 2386名参与者。有证据表明,相较于候补/常规护理,聚焦创伤的CBT(CBT-TF)减轻治疗后PTSD症状的实证效应最大(10项研究; n= 524; SMD -1.22,-1.78至- 0.66)。团体CBT-TF相较于个体CBT-TF在减轻治疗后PTSD症状的效果上较差(1项研究; n= 268; SMD -0.35,-0.11至-0.59)。与候补/常规护理相比,眼动脱敏再处理(EMDR)疗法在减轻治疗后PTSD症状方面无效(4项研究; n= 92; SMD -0.83,-1.75至0.10)。有证据表明,与候补和聚焦当下疗法相比,CBT-TF治疗的退出率更高。
结论:证据虽然有限,但仍支持将个体CBT-TF作为现役和退役人员PTSD的一线心理治疗方法。也有团体CBT-TF的实证证据,但不如个体CBT-TF的有力。目前EMDR尚不推荐作为一线治疗,并且迫切需要进一步评估。相较于其他PTSD患者和高流失水平,较低的效应量和较高的退出率表明,当前形式的CBT-TF并非最佳选择,需要进一步研究以开发和评估针对现役和退役人员PTSD更有效的治疗方法。
1. Introduction
Post-traumatic stress disorder (PTSD) is a common psychiatric condition amongst active duty and ex-serving military personnel across the world, creating a significant public health challenge (Steenkamp, Litz, Hoge, & Marmar, Citation2015). For reasons that are not entirely clear, prevalence rates vary between nations with reported rates of 20 to 30% (Richardson, Frueh, & Acierno, Citation2010) in US troops returning from various conflicts from the Vietnam era through to the present day, 6% to 17% in the UK (Stevelink et al., Citation2018), 5% in Canada (Richardson et al., Citation2019), and 3% in the Netherlands (Engelhard et al., Citation2007).
Over the past three decades there has been considerable investment in new treatment models and evaluation of them, leading to advances in the treatment of PTSD in civilian and military populations (Carlson, Chemtob, Rusnak, Hedlund, & Muraoka, Citation1998; Foa et al., Citation2018; Resick et al., Citation2015; Steenkamp et al., Citation2015; Tylee, Gray, Glatt, & Bourke, Citation2017). International clinical practice guidelines unanimously recommend trauma focused psychological therapies (TFPT) in the form of Eye Movement Desensitization Reprocessing (EMDR), and individual Cognitive Behavioural Therapy with a trauma focus (CBT-TF) as first line treatments for PTSD. Cognitive Processing Therapy (CPT), Cognitive Therapy with a trauma focus and Prolonged Exposure (PE) are specific CBT-TFs with enough evidence to merit recommendation as first line treatments in their own right (International Society of Traumatic Stress Studies [ISTSS], Citation2018, NICE, Citation2018). Previous work has suggested that the efficacy of established trauma focused interventions benefit less in serving and ex-serving personnel (Haagen, Smid, Knipscheer, & Kleber, Citation2015; Kitchiner, Roberts, Wilcox, & Bisson, Citation2012).
The US Department of Defence (2017) guidelines on PTSD recommend out-patient trauma focused psychological therapies (TFPT) before pharmacological interventions or other forms of therapy due to the benefits of TFPT being longer-lived (Ostacher & Cifu, Citation2019). Interestingly, the UK NICE PTSD guidelines (2018) also recommend TFPT as a first line of therapy, but not EMDR for combat-related trauma due to the current evidence base (NICE, Citation2018). Steenkamp has criticized the current DoD/VA PTSD treatment guidelines as based primarily on studies with civilian samples, with traumas very different to military deployment and, therefore, findings that may not translate to active duty and ex-serving military personnel (Steenkamp et al., Citation2015). Our 2012 review identified 16 PTSD treatment randomized controlled trials (RCTs) with ex-service personnel but only four studies of TFPTs for PTSD had data available for meta-analysis (Kitchiner et al., Citation2012). These four studies were heterogeneous and included EMDR and CBT-TF interventions which, together, were more effective at reducing PTSD symptoms post treatment than treatment as usual or waitlist, (n = 128; SMD −0.59, 95% CI −1.09, −0.10) (Carlson et al., Citation1998; Devilly, Spence, & Rapee, Citation1998; Keane, Fairbank, Caddell, & Zimering, Citation1989; Monson et al., Citation2006). The completion of a number of studies since 2012 means that it is timely to update the evidence base for treating PTSD in active duty and ex-serving military personnel.
There is a growing literature on efforts to improve the treatment of PTSD in ex-serving and, more recently, active duty personnel. These include novel therapies which use glasses that track REM sleep and play music (Ahmadi, Hazrati, Ahmadizadeh, & Noohi, Citation2015), multi-modular motion assisted memory desensitization reconsolidation (3MDR) using a treadmill, music and images combined with virtual reality (Nijdam & Vermetten, Citation2018; van Gelderen, Nijdam, & Vermetten, Citation2018), PE with virtual reality (Gamito et al., Citation2010; McLay et al., Citation2017, Citation2011), neuro-linguistic programming (NLP) informed exposure based therapy (Gray, Budden-Potts, & Bourke, Citation2017; Tylee et al., Citation2017), couples therapy (Sautter, Glynn, Cretu, Senturk, & Vaught, Citation2015) and intensive PE (Foa et al., Citation2018). Our aim was to update the current evidence base by undertaking a systematic review and meta-analysis of psychological therapy RCTs for the treatment of active duty or ex-serving military personnel with PTSD. We also sought to investigate possible reasons why the benefits from therapy for this population might differ from those observed in civilian populations (NICE, Citation2018; Steenkamp et al., Citation2015).
2. Method
2.1. Selection criteria
This review included RCTs of any defined psychological therapy aimed at the reduction of PTSD symptoms in active duty and ex-serving personnel, in comparison with a control group (e.g. usual care/waiting list), other psychological therapy or psychosocial intervention (e.g. psychoeducation/relaxation training). It was required that 70% of study participants were diagnosed with PTSD with a duration of three months or more, according to DSM or ICD criteria determined by clinician diagnosis or an established diagnostic interview. Only studies of adults aged 18 or over were eligible. There were no restrictions based on symptom severity or trauma type. The diagnosis of PTSD was required to be primary, but there were no other exclusions based on comorbidity. Studies that conducted secondary analyses of data already included in the meta-analyses were excluded. Studies were also excluded if a continuous measure of PTSD severity post-treatment was not available. The initial searches identified 5500 potentially eligible studies. Abstracts were reviewed and full text copies obtained for 203 potentially relevant studies. This resulted in 114 RCTs that were included in an updated review of psychological treatment for PTSD, irrespective of trauma type (Lewis et al, in preparation). Of these, there were 24 RCTs of active duty of ex-serving military personnel with PTSD (see ) with 2386 participants, which allowed for several meta-analyses of the data.
2.2. Search strategy
This systematic review was undertaken alongside a number of reviews for an update of the International Society for Traumatic Stress Studies (ISTSS) Treatment Guidelines (ISTSS, Citation2018). A search was conducted by the Cochrane Collaboration, which updated a previously published Cochrane review with similar inclusion criteria, which was published in 2013 (Bisson, Citation2013). The update search aimed to identify all RCTs related to the prevention and treatment of PTSD, published from 2008 to the 31 May 2018. We searched through all included studies evaluating a psychological intervention in active duty and ex-serving military personnel, which provided a final group of papers included in this review. The searches included results from PubMed, PsycINFO, Embase and the Cochrane database of randomized trials. Terms related to PTSD were combined with terms referring to psychological therapy (using both MeSH terms and text words). We checked reference lists of the included studies. We searched the World Health Organization’s, and the U.S. National Institutes of Health’s trials portals to identify additional unpublished or ongoing studies. We contacted experts in the field with the aim of identifying unpublished studies and studies that were in submission. A complementary search of the Published International Literature on Traumatic Stress (PILOTS) was also conducted. The updated search aimed to identify all RCTs related to the prevention and treatment of PTSD, published from January 2008 to the 31 May 2018, using the search terms PTSD or posttrauma* or post-trauma* or ‘post trauma*’ or ‘combat disorder*’ or ‘stress disorder*’. The searches included results from PubMed, PsycINFO, Embase and the Cochrane database of randomized trials. This produced a group of papers related to the psychological treatment of PTSD in adults.
2.3. Data extraction
Study characteristics and outcome data were extracted by two reviewers, using a form that had been piloted on five of the included studies. The primary outcome measure for the review was reduction in the severity of PTSD symptoms post treatment using a standardized measure. When available, clinician rated measures were included in meta-analyses (e.g. the Clinician Administered PTSD Scale (CAPS) (Blake et al., Citation1995)). If no clinician rated measure was used or reported, self-report measures were included (e.g. the PTSD Checklist for DSM-5 (PCL-5) (Weathers et al., Citation2013)). Study authors were contacted to obtain missing data.
2.4. Risk of bias assessment
All included studies were assessed for risk of bias using Cochrane criteria (Higgins et al., Citation2011). This included: (1) sequence allocation for randomization (the methods used for randomly assigning participants to the treatment arms and the extent to which this was truly random); (2) allocation concealment (whether or not participants or personnel were able to foresee allocation to a specific group); (3) assessor blinding (whether the assessor was aware of group allocation); (4) incomplete outcome data (whether missing outcome data was handled appropriately); (5) selective outcome reporting (whether reported outcomes matched with those that were pre-specified); and (6) any other notable threats to validity (for example, baseline imbalances between groups, small sample size, or premature termination of the study). Two researchers independently assessed each study and any conflicts were discussed with a third researcher with the aim of reaching a unanimous decision.
2.5. Clinical importance, quality of evidence assessment and level of recommendation
We rated findings in terms of clinical importance. We used a definition of clinical importance, which was developed by the ISTSS Treatment Guidelines Committee and approved by the ISTSS Board and membership (Bisson, Berliner, Cloitre, & Forbes et al., Citationin press), building on previous work by the National Institute of Health and Care Excellence (National Collaborating Centre for Mental, Citation2005). To be rated clinically important, an intervention had to demonstrate an effect size of >0.8 for continuous outcomes for wait list and treatment as usual (TAU) control comparisons, >0.4 for placebo control comparisons and >0.2 for active treatment control comparisons. The quality of evidence for each comparison was assessed using the: Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (GRADE, Citation2018) (see ). Evidence was categorized as high quality (indicating that further research is very unlikely to change confidence in the estimate of effect); moderate quality (indicating that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate); low quality (indicating that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate) or very low quality (indicating that we are very uncertain about the estimate). We used the algorithm developed for ISTSS Guidelines Committee (Weathers et al., Citation2013) to determine the strength of any treatment recommendations that could be made. The algorithm combines the clinical importance and quality of evidence assessments along with any other important information (e.g. adverse effect profile).
Table 1. Characteristics of included studies.
Table 2. Meta-analytic results.
2.6. Data synthesis
Meta-analyses were conducted using the Cochrane’s Review Manager 5 (RevMan) software (RevMan, Citation2014). Continuous measures of post-treatment PTSD severity were analysed as standardized mean differences (SMDs). All outcomes were presented using 95% confidence intervals. Clinical heterogeneity was assessed in terms of variability in the experimental and control interventions; participants; settings; and outcomes. Heterogeneity was assessed further using both the I2 statistic and the chi-squared test of heterogeneity, as well as visual inspection of the forest plots. Data were pooled using fixed-effect meta-analyses, except where heterogeneity was present, when random-effect models were used.
2.7. Study characteristics
Study characteristics are summarized in . Ten studies compared CBT-TF vs. waitlist/usual care (Foa et al., Citation2018; Forbes et al., Citation2012; Gamito et al., Citation2010; Gray et al., Citation2017; Keane et al., Citation1989; McLay et al., Citation2011; Monson et al., Citation2006; Peniston & Kulkosky, Citation1991; Reger et al., Citation2016; Tylee et al., Citation2017) (see ). These included two studies of CPT (Forbes et al., Citation2012; Monson et al., Citation2006) (see ), two studies of PE (Foa et al., Citation2018; Nacasch et al., Citation2011; Reger et al., Citation2016) (see ), and two studies of Reconsolidation of Traumatic Memories (RTM) (Gray et al., Citation2017; Tylee et al., Citation2017) (see ), three studies of virtual reality exposure (VRE) therapy vs. waitlist (Gamito et al., Citation2010; McLay et al., Citation2011; Reger et al., Citation2016) (see ) and one study compared Group CBT-TF vs. waitlist/usual care/minimal contact (Castillo et al., Citation2016). Four studies compared EMDR vs. waitlist/usual care (Ahmadi et al., Citation2015; Carlson et al., Citation1998; Devilly et al., Citation1998; Jensen, Citation1994) (see ). Four studies compared CBT-TF vs. PCT (Foa et al., Citation2018; Rauch et al., Citation2015; Schnurr et al., Citation2007; Suris, Link-Malcolm, Chard, Ahn, & North, Citation2013) (see ). One study compared EMDR vs. Relaxation training (Carlson et al., Citation1998). One study compared EMDR vs. Rapid Eye Movement-Desensitization (REM-D) (Ahmadi et al., Citation2015). Two studies compared VRE therapy vs. Control Exposure (McLay et al., Citation2017; Reger et al., Citation2016) (see ). One study compared VRE therapy vs. PCT (Ready, Gerardi, Backscheider, Mascaro, & Rothbaum, Citation2010). Two studies compared Group CBT-TF vs. Group PCT (Resick et al., Citation2015; Schnurr et al., Citation2003) (see ). One study compared Group CBT-TF vs. Individual CBT-TF (Resick et al., Citation2017). One study compared Non-CBT-TF vs. Couples Psychoeducation (Sautter et al., Citation2015). One study compared Relaxation training vs. wait list/usual care (Carlson et al., Citation1998).
Twenty studies were conducted in the USA (Carlson et al., Citation1998; Castillo et al., Citation2016; Foa et al., Citation2018; Gray et al., Citation2017; Jensen, Citation1994; Keane et al., Citation1989; McLay et al., Citation2017, Citation2011; Monson et al., Citation2006; Peniston & Kulkosky, Citation1991; Rauch et al., Citation2015; Ready et al., Citation2010; Reger et al., Citation2016; Resick et al., Citation2017, Citation2015; Sautter et al., Citation2015; Schnurr et al., Citation2007, Citation2003; Suris et al., Citation2013; Tylee et al., Citation2017), two in Australia (Devilly et al., Citation1998; Forbes et al., Citation2012), and one each in Iran (Ahmadi et al., Citation2015), and Portugal (Gamito et al., Citation2010). Fifteen studies included ex-serving personnel who had left the military (Carlson et al., Citation1998; Castillo et al., Citation2016; Devilly et al., Citation1998; Gamito et al., Citation2010; Keane et al., Citation1989; Monson et al., Citation2006; Nacasch et al., Citation2011; Peniston & Kulkosky, Citation1991; Rauch et al., Citation2015; Ready et al., Citation2010; Sautter et al., Citation2015; Schnurr et al., Citation2007, Citation2003; Suris et al., Citation2013; Tylee et al., Citation2017; Yehuda et al., Citation2014). Six studies contained only active duty personnel (Ahmadi et al., Citation2015; McLay et al., Citation2017, Citation2011; Reger et al., Citation2016; Resick et al., Citation2017, Citation2015). Two studies included a mixture of active duty and ex-serving personnel (Foa et al., Citation2018; Schnurr et al., Citation2007). Fifteen studies included only males (Ahmadi et al., Citation2015; Carlson et al., Citation1998; Devilly et al., Citation1998; Foa et al., Citation2018; Gamito et al., Citation2010; Gray et al., Citation2017; Jensen, Citation1994; Keane et al., Citation1989; McLay et al., Citation2017, Citation2011; Nacasch et al., Citation2011; Peniston & Kulkosky, Citation1991; Ready et al., Citation2010; Reger et al., Citation2016; Schnurr et al., Citation2003; Tylee et al., Citation2017). Two studies included only females (Castillo et al., Citation2016; Schnurr et al., Citation2007). Seven studies included both sexes (Forbes et al., Citation2012; Monson et al., Citation2006; Rauch et al., Citation2015; Resick et al., Citation2017, Citation2015; Suris et al., Citation2013; Yehuda et al., Citation2014). One study included the active duty individual and their partner (Sautter et al., Citation2015). One study contained participants who deployed to Korea (Monson et al., Citation2006). Eleven studies contained participants deployed to Vietnam (Carlson et al., Citation1998; Devilly et al., Citation1998; Forbes et al., Citation2012; Gray et al., Citation2017; Jensen, Citation1994; Keane et al., Citation1989; Monson et al., Citation2006; Peniston & Kulkosky, Citation1991; Ready et al., Citation2010; Schnurr et al., Citation2003; Yehuda et al., Citation2014). Thirteen studies contained participants deployed to either Iraq or Afghanistan (Castillo et al., Citation2016; Foa et al., Citation2018; Forbes et al., Citation2012; Gray et al., Citation2017; McLay et al., Citation2017, Citation2011; Monson et al., Citation2006; Rauch et al., Citation2015; Reger et al., Citation2016; Resick et al., Citation2017, Citation2015; Sautter et al., Citation2015; Tylee et al., Citation2017; Yehuda et al., Citation2014). One study contained participants from the Iranian war (Ahmadi et al., Citation2015). One study each contained participants who deployed to Africa (Gamito et al., Citation2010) and Timor (Forbes et al., Citation2012). Two studies did not report where participants had deployed to (Schnurr et al., Citation2007; Suris et al., Citation2013). One study reported participants’ PTSD being due to military sexual trauma (Suris et al., Citation2013). All twenty-four studies determined PTSD diagnosis via a clinician-administered scale.
2.8. Methodological quality of studies
Risk of bias assessments were conducted for the 24 included studies. Eight studies reported a method of random sequence allocation judged to pose a ‘low’ risk of bias, one study a ‘high’ risk and fifteen were ‘unclear’. Allocation concealment was rated as ‘low’ risk of bias in seven studies; the remaining seventeen were rated as ‘unclear’. Fourteen studies were judged to have complete outcome data and ‘low’ risk of bias. Three studies were rated as having ‘high’ risk of bias due to incomplete data and seven as ‘unclear’. Blinding of the outcome assessment was judged as ‘low’ risk in sixteen studies. Three studies were judged as ‘high’ risk and five as ‘unclear’. Selective reporting of results was judged as ‘low’ in six studies and ‘high’ in one study. The remaining seventeen studies were rated as ‘unclear’. Other bias was rated as ‘low’ in eleven studies, compared to ‘high’ in eleven of the studies. Two were rated as ‘unclear’. Eighteen studies failed to reference a published protocol, although there was little evidence of reporting bias. We could not rule out potential researcher allegiance in twelve studies, since many founders of specific therapies evaluated their particular treatment model. All studies presented objectives, but samples sizes were often small.
3. Synthesis of results
Results of the meta-analyses are presented in and the Forest plots (Figures 2–10). In summary, CBT-TF/Exposure therapy was more effective at reducing PTSD symptoms than waitlist/usual care post treatment with the effect maintained at six months but not at 12 months in the one study that explored this. A review of the evidence in relation to specific CBT-TF based interventions, PE was more effective than waitlist at reducing PTSD symptoms post treatment and at six months. CPT was more effective than waitlist at reducing PTSD symptoms post treatment but not at six months and leaving the study early was more likely in the CPT arm. VRE was more effective than waitlist at reducing PTSD symptoms post treatment with leaving the study early was more likely in the waitlist arm. Group CBT-TF was more effective than waitlist at reducing PTSD symptoms post treatment with leaving the study early more likely in the waitlist arm. RTM was more effective than waitlist at reducing PTSD symptoms post treatment with leaving the study early more likely in the RTM arm.
There was no difference between Relaxation Training and waitlist in reducing PTSD symptoms post treatment or leaving the study early. There was no difference between EMDR and waitlist in reducing PTSD symptoms post treatment or leaving the study early. Individual CBT-TF was more effective than Group CBT-TF at reducing PTSD symptoms post treatment but not maintained at 6 months. CBT-TF was more effective than PCT in reducing PTSD symptoms post treatment and at six months. Leaving the study early also favoured the CBT-TF arm. There was no difference between Group CBT-TF and Group PCT in reducing PTSD symptoms post treatment, but group CBT-TF was more effective at 6 and 12 months follow-up. Couples non-CBT-TF was more effective than Couples Psychoeducation in reducing PTSD symptoms post treatment and at 6 months follow-up with no difference between the interventions on leaving the study early.
There was no difference between EMDR and Relaxation Training in reducing PTSD symptoms post treatment, but the relaxation training arm was more likely to leave the study early. There was no difference between EMDR and REM-D in reducing PTSD symptoms post treatment but leaving the study early favoured the REM-D arm. There was no difference between VRE and PCT in reducing PTSD symptoms post treatment. Leaving the study early favoured PCT. There was no difference between VRE and Control Exposure in reducing PTSD symptoms post treatment, at 6 or 12 months. Leaving the study early favoured the VRE arm.
4. Heterogeneity
There was considerable clinical heterogeneity across the psychological therapies aimed at reducing PTSD symptoms, which varied in content and delivery. Eighteen studies included an intervention based on CBT-TF principles, although the exact nature of what was included varied from Implosive flooding therapy to CPT. The method by which the psychological therapy delivered also varied from several sessions delivered in the same week, group therapy, couples therapy or wearing glasses that play music during REM sleep. Duration of treatment ranged from five sessions within one week to thirty weekly sessions. Considerable statistical heterogeneity was evident in all of the pooled comparisons resulting in regular use of a random-effects model (see ).
5. Clinical importance, quality of findings and strength of recommendations
Using the ISTSS guidelines method to rate clinical importance (ISTSS, Citation2018). CBT-TFs collectively had an effect size which met our predetermined threshold of >0.80 or over for comparisons against waiting list or TAU control. For specific interventions, only Group CBT-TF and RTM met this threshold. Similarly, for comparisons against an attention control intervention, only CBT-TF (vs. PCT) and couples non-CBT-TF (vs couples psychoeducation) reached >0.4 or above effect size (Foa et al., Citation2018; Rauch et al., Citation2015; Schnurr et al., Citation2007; Suris et al., Citation2013), and individual CBT-TF meets this threshold against group CBT-TF from a single study (Resick et al., Citation2017) against the active treatment comparisons and reached >0.2 effect size or above. There were no placebo control comparisons or single studies with over 300 participants.
We used the GRADE system (GRADE, Citation2018) to score each comparison, (see ). Five comparisons were rated as Low quality, these included PE (Foa et al., Citation2018; Nacasch et al., Citation2011; Reger et al., Citation2016) vs. wait list, CBT-TF vs. waiting list (Foa et al., Citation2018; Forbes et al., Citation2012; Gamito et al., Citation2010; Gray et al., Citation2017; Keane et al., Citation1989; McLay et al., Citation2011; Monson et al., Citation2006; Nacasch et al., Citation2011; Peniston & Kulkosky, Citation1991; Reger et al., Citation2016; Tylee et al., Citation2017), CBT-TF/Exposure (Foa et al., Citation2018; Rauch et al., Citation2015; Schnurr et al., Citation2007; Suris et al., Citation2013) vs. PCT and VRE vs. Control Exposure (McLay et al., Citation2017; Reger et al., Citation2016), and Group CBT-TF vs. Group Present Centred Therapy (Resick et al., Citation2017). All other comparisons were rated as very low.
Using the ISTSS strength of recommendation algorithm (Higgins et al., Citation2011), no psychological treatments could be given a Strong recommendation. CBT-TFs could be recommended at a Standard level, with PE and CPT both being graded as interventions with Low Effect. CBT-TF, RTM and VRE could be recommended as interventions with Emerging Evidence of effect with there being insufficient evidence to recommend any other intervention.
6. Discussion
6.1. Main findings
Various forms of individual CBT-TF were the most often tested and most effective psychological treatments of PTSD in active duty and ex-serving military personnel in this review. But no intervention could be recommended strongly and only CBT-TF collectively could be recommended at a standard level according to the criteria used for the ISTSS Prevention and Treatment Guidelines (ISTSS, Citation2018). The other therapies tested could be recommended as interventions with Low Effect or Emerging Evidence (CPT, Group CBT-TF, PE, RTM and VRE) or with insufficient evidence to recommend them (EMDR, Relaxation Therapy, REM-D and PCT). Of the specific CBT-TFs, CPT, Group CBT-TF, PE, RTM and VRE were all effective when considered individually but only Group CBT-TF and RTM met our predetermined threshold for clinical importance (Gray et al., Citation2017; Tylee et al., Citation2017). Despite Group CBT-TF being more effective than waitlist and PCT, it was less effective than individual CBT-TF. Of interest, effect sizes in favour of PE and CPT over waiting list/usual care were noticeably smaller than those obtained in similar comparisons in studies of individuals seeking treatment for non-military trauma (Lewis, et al in preparation).
The UK’s NICE PTSD guidelines (Citation2018) recommended that people with combat-related PTSD should not be treated with EMDR due to lack of evidence for its effectiveness in this population (NICE, Citation2018). Our results support this conclusion, however, this is counter-intuitive given the proliferation of EMDR therapy used around the world and non RCT evidence that it is successfully treating PTSD related to active duty (Frappell-Cooke & McCauley, Citation2018) and in ex-serving military personnel (Kitchiner et al., Citation2012). This negative finding may be real but may also be due to chance and several other factors including small sample sizes leading to insufficient power, chronicity and treatment-resistance of participants, and sub-optimal delivery of EMDR (two studies reported novice EMDR therapists with only level one training (2 days) (Carlson et al., Citation1998; Jensen, Citation1994) and two studies offered only two EMDR therapy sessions (Devilly et al., Citation1998; ISTSS, Citation2018; Jensen Citation1994; NICE, Citation2018). Twelve sessions of EMDR were provided in Carlson’s 1998 study but the control condition was biofeedback-assisted relaxation which is an active control condition and the study had several risks of bias. The two EMDR studies that did report significant effects had sample sizes of only 23 (Ahmadi et al., Citation2015) and 25 (Jensen, Citation1994) respectively. Jensen (Citation1994) only offered two EMDR sessions, and several risk of bias concerns were also identified (Jensen, Citation1994); the outcome data should, therefore, be treated with caution. More research is clearly needed to determine whether or not EMDR is effective for PTSD in this population.
Our results also support the UK’s NICE PTSD guidelines (Citation2018) recommendation that people with combat-related PTSD be treated with CBT-TF. The strength and quality of the evidence, however, is relatively weak and using the algorithm developed for the ISTSS Guidelines (ISTSS, Citation2018), no psychological treatment could be recommended as strongly for the treatment of combat-related PTSD as for PTSD related to any traumatic event. There are a number of possible reasons for this but the main ones seem likely to be insufficient power due to the low overall number of studies and, as previously suggested, the possibility that people with combat-related PTSD are more difficult to treat than people with PTSD related to other traumatic events (Kitchiner et al., Citation2012; Steenkamp et al., Citation2015).
It is no surprise that the positive effect of CBT-TF was significantly contributed to by PE and CPT RCTs. More surprising, and encouraging, is the emergence of new, innovative methods of delivery, namely VRE and RMT. The RCTs of RMT, in particular, had very promising effect sizes and is worthy of further exploration. There was evidence of greater drop-out rates from CBT-TF studies compared to waitlist and PCT (Steenkamp et al., Citation2015), although this was primarily accounted for by greater drop-out rates in PE RCTs; none of the other CBT-TFs were associated with statistically significantly greater drop-out rates than wait-list/usual care. Reasons for dropping out will be multi-factorial, and may be due to extended, repeated, and intense nature of deployment trauma (Price, Gros, Strachan, Ruggiero, & Acierno, Citation2013) and service members being exposed to threats to life and morally compromising experiences that may require different treatment approaches (Litz et al., Citation2009; Stein et al., Citation2012). However, the PE finding is striking and suggests it may not be as well tolerated as other forms of CBT-TF and that some forms of CBT-TF may not be optimal and acceptable to active duty and ex-service personnel in their current format of delivery. Future research needs to gain a better understanding of the reasons why individuals drop out and experiment with novel ways to reduce this. We were unable to identify any RCTs evaluating third wave interventions such as Acceptance and Commitment Therapy (ACT) or mindfulness based therapy with serving or ex-serving personnel.
7. Strengths and limitations
This review rigorously followed guidelines set out by the Cochrane Collaboration (Higgins et al., Citation2011). Two authors independently screened the abstracts identified by the literature search; read all potentially relevant studies; assessed each study against the inclusion criteria; extracted data from the written reports; and rated each study for risk of bias. Any disagreements were discussed with a third author, and unanimous decisions were reached for inclusion and classification. Following these procedures minimized the potential for bias, but some unavoidable issues remained. Firstly, it is important to acknowledge the possible influence of publication bias, since only published papers were included in the review. In addition, this review relied only on English language studies, which limits its generalizability.
Sample sizes were small in many studies. It can therefore be argued that the absence of significant differences in some comparisons represents a lack of statistical power rather than true equivalence of the approaches. The quality of individual studies is of importance when interpreting the results of any meta-analysis. Several of these studies were conducted in the 1980/90s and deemed of poor quality methodologically. Many of the included studies demonstrated a lack of independent evaluation, as thirteen of the studies were evaluated by the developers themselves. Participants were predominantly male, white, had relatively low levels of education, and many participants had experienced PTSD symptoms for over 30–40 years and would likely meet the criteria for an ICD-11 diagnosis of Complex PTSD.
8. Clinical implications
This review demonstrates some evidence for individual CBT-TF in the treatment of PTSD in active duty and ex-serving personnel and that it should be offered as the first line treatment. The US Veteran Affairs (VA) department has invested and trained its clinicians in two evidenced based psychological therapies; PE (Foa, Rothbaum, Riggs, & Murdock, Citation1991) and CPT (Resick, Nishith, Weaver, Astin, & Feuer, Citation2002). Our results tentatively support this decision but, unfortunately, despite a national rollout of training and supervision, there is evidence that PE and CPT are rarely used in VA clinics, resulting in non-trauma focused therapies still being offered to active duty and ex-service personnel (Shiner et al., Citation2013). This points to the need for more effective dissemination and implementation of the best evidenced treatments for PTSD and more effective treatments for combat-related PTSD.
It is too early to argue that VRE and RTM should become first-line treatments ahead of, or be considered equivalent to, PE and CPT. The emerging evidence of their efficacy, however, along with some concerns about the acceptability of PE and the minimal imaginal exposure involved in RTM should encourage more work to determine whether they should be seen as valid alternatives to more established paradigms. If individuals have difficulty engaging in standard CBT-TF, alternative forms of delivery could also be considered. For example, intensive CBT-TF with multiple sessions weekly, for active duty personnel may improve uptake due to the short time away from normal duties (Foa et al., Citation2018). The finding of some support for group CBT-TF is encouraging, but as it is not as effective as individual therapy it should not be considered first line at present. The lack of evidence of effect for EMDR should preclude its routine, first-line use in this population. However, given the quality of the current RCT evidence in this population and the evidence from other sources, it would not be unreasonable to consider EMDR in individuals who do not respond to CBT-TF or are unable to tolerate it. Non trauma focused psychological therapies such as PCT could be offered as an alternative to CBT-TF in treatment seeking active duty and ex-serving personnel who do not wish to engage in trauma-focused therapies, or to those who are unable to tolerate them (Foa et al., Citation2018).
It is important to remember that the complexity of a person with PTSD’s biopsychosocial symptoms at presentation may also be a factor that inhibits a reduction in PTSD and other co-morbid symptoms. There continues to be considerable challenges for health care systems who provide mental health treatment to active duty and ex-serving military personnel to find efficient ways to train personnel, promote and disseminate effective treatments for PTSD (Schnurr et al., Citation2007) and also to provide a holistic approach to care that takes social factors, in particular, into account. Careful monitoring is required to make sure that future TFPTs that improve symptoms of PTSD also improve the overall health and lives of active duty and ex-serving military personnel (McLay et al., Citation2011).
9. Research implications
Despite over 40 years of research focused on reducing PTSD in active duty and ex-serving military personnel, effect sizes and acceptability of current therapies remain modest although, as described above, advances have been made and the evidence is more robust than it was when we last reviewed the literature in 2012. Future RCTs should adopt rigorous methodological designs, including more adequately powered, pragmatic effectiveness phase III studies. Other key areas for future research include: replication of the finding that intensive PE is non-inferior to the standard weekly protocol (Foa et al., Citation2018) and research into briefer delivery of other interventions; methods to reduce drop out rates and better explore acceptability; why the results for EMDR appear to be different in this population than other populations; whether there are differences between responses of active duty and ex-service personnel; whether there are differences between those with a diagnosis of PTSD and those with a diagnosis of complex PTSD; and how well treatment gains are maintained with follow-up periods of longer than 6–12 months (Monson et al., Citation2006).
Treatments with emerging evidence of efficacy such as VRE and RTM deserve more attention and future studies of TFPT should consider adding interpersonal skill training components and other techniques to address the core components of complex PTSD (Cloitre et al., Citation2010). Broadening the base of countries and cultures in which treatments are tested will be necessary to increase the confidence that such treatments can be applied globally by therapists with no model specific allegiance (Forbes et al., Citation2012). More research is required to develop and investigate novel therapies (Ahmadi et al., Citation2015), and improve our understanding of cognitive and biological mechanisms of PTSD treatment to help refine treatments and increase rates of response (Rauch et al., Citation2015).
Acknowledgments
We would like to acknowledge the input and support of the Cochrane Collaboration.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Ahmadi, K., Hazrati, M., Ahmadizadeh, M., & Noohi, S. (2015). REM desensitization as a new therapeutic method for post-traumatic stress disorder: A randomized controlled trial. Acta Medica Indonesiana, 47(2), 1–17. PMID: 26260553.
- Bisson, J., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults (Review). Cochrane Database of Systematic Reviews, 12, CD003388.
- Bisson, J. I., Berliner, L., Cloitre, M., Forbes, D., Jensen, TK., Lewis, C., ... Shapiro, F. (in press). The international society for traumatic stress studies. New guidelines for the prevention and treatment of PTSD: Methodology and development process. Journal of Trauma Stress, 32(4), 471–473.
- Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., & Keane, T. M. (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–90. PMID: 7712061.
- Carlson, J., Chemtob, C. M., Rusnak, K., Hedlund, N. L., & Muraoka, M. Y. (1998). Eye movement desensitization and reprocessing (EDMR) treatment for combat-related posttraumatic stress disorder. Journal of Traumatic Stress, 11(1), 3–32.
- Castillo, D. T., Chee, C. L., Nason, E., Keller, J., C’de Baca, J., Qualls, C., & Keane, T. M. (2016). Group-delivered cognitive/exposure therapy for PTSD in women veterans: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice and Policy, 8(3), 404–412.
- Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L., … Petkova, E. (2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry, 167, 915–924.
- Devilly, G., Spence, S., & Rapee, R. (1998). Statistical and reliable change with eye movement desensitization and reprocessing: Treating trauma within a veteran population. Behavior Therapy, 29, 435–455.
- Engelhard, I. M., Van Den Hout, M. A., Weerts, J., Arntz, A., Hox, J. J. C. M., & McNally, R. J. (2007). Deployment-related stress and trauma in Dutch soldiers returning from Iraq. Prospective study. The British Journal of Psychiatry : The Journal of Mental Science, 191, 140–145.
- Foa, E., McLean, C. P., Zang, Y., Rosenfield, D., Yadin, E., Yarvis, J. S., & Peterson, A. L. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. JAMA, 319, 354–364.
- Foa, E., Rothbaum, B. O., Riggs, D. S., & Murdock, T. B. (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715–723. PMID: 1955605.
- Forbes, D., Lloyd, D., Nixon, R. D. V., Elliott, P., Varker, T., Perry, D., … Creamer, M. (2012). A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Anxiety Disorders, 26(3), 442–452.
- Frappell-Cooke, W., & McCauley, M. (2018). Military psychological trauma and therapy: A review of EMDR treatment and supervision in the UK Ministry of Defence. Journal of the Royal Army Medical Corps. doi:10.1136/jramc-2018-001060
- Gamito, P., Oliveira, J., Rosa, P., Morais, D., Duarte, N., Oliveira, S., & Saraiva, T. (2010). PTSD elderly war veterans: A clinical controlled pilot study. Cyberpsychology, Behavior and Social Networking, 13(1), 43–48. PMID: 20528292.
- GRADE. (2018, November 29). Retrieved from http://www.gradeworkinggroup.org
- Gray, R., Budden-Potts, D., & Bourke, F. (2017). Reconsolidation of traumatic memories for PTSD: A randomized controlled trial of 74 male veterans. Psychotherapy Research, 1–19. doi:10.1080/10503307.2017
- Haagen, J. F., Smid, G. E., Knipscheer, J. W., & Kleber, R. J. (2015). The efficacy of recommended treatments for veterans with PTSD: A metaregression analysis. Clinical Psychology Review, 40, 184–194.
- Higgins, J. P., Altman, D. G., Gotzsche, P. C., Juni, P., Moher, D., Oxman, A. D., … Sterne, J. A. C. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928–d5928.
- International Society of Traumatic Stress Studies (ISTSS) [ Online]. (2018, November 26). New ISTSS prevention and treatment guidelines. Retrieved from http://www.istss.org/treating-trauma/new-istss-guidelines.aspx
- Jensen, J. (1994). An investigation of eye movement desensitisation and reprocessing (EMD/R) as a treatment for posttraumatic stress disorder (PTSD) symptoms of Vietnam combat veterans. Behavior Therapy, 25, 311–325.
- Keane, T., Fairbank, J. A., Caddell, J. M., & Zimering, R. T. (1989). Implosive (flooding) therapy reduces symptoms of PTSD in Vietnam combat veterans. Behavior Therapy, 20(2), 245–260.
- Kitchiner, N. J., Roberts, N., Wilcox, D., & Bisson, J. (2012). Systematic review and meta-analyses of psychosocial interventions for veterans of the military. European Journal of Psychotraumatology, 3, 19267.
- Litz, B. T., Stein, N., Delaney, E., Lebowitz, L., Nash, W. P., Silva, C., & Maguen, S. (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29(8), 695–706.
- McLay, R., Baird, A., Webb-Murphy, J., Deal, W., Tran, L., Anson, H., … Johnston, S. (2017). A randomized, head-to-head study of virtual reality exposure therapy for posttraumatic stress disorder. Cyberpsychology, Behavior and Social Networking, 20, 218–224.
- McLay, R., Wood, D. P., Webb-Murphy, J. A., Spira, J. L., Wiederhold, M. D., Pyne, J. M., & Wiederhold, B. K. (2011). A randomized, controlled trial of virtual reality-graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychology, Behavior and Social Networking, 14, 223–229.
- Monson, C., Schnurr, P. P., Resick, P. A., Friedman, M. J., Young-Xu, Y., & Stevens, S. P. (2006). Cognitive processing therapy for veterans with military related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74, 898–907.
- Nacasch, N., Foa, E. B., Huppert, J. D., Tzur, D., Fostick, L., Dinstein, Y., … Zohar, J. (2011). Prolonged exposure therapy for combat- and terror-related posttraumatic stress disorder: A randomized control comparison with treatment as usual NCT00229372. Journal of Clinical Psychiatry, 72, 1174–1180.
- NICE. (2018). Guidelines for post-traumatic stress disorder nice guideline (NG116). Retrieved from https://www.nice.org.uk/guidance/ng116
- Nijdam, M. J., & Vermetten, E. (2018). Moving forward in treatment of posttraumatic stress disorder: Innovations to exposure-based therapy. European Journal of Psychotraumatology, 9, 1.
- Ostacher, M. J., & Cifu, A. S. (2019). Management of posttraumatic stress disorder. JAMA, 321(2), 200–201.
- Peniston, E. G., & Kulkosky, P. J. (1991). Alpha-theta brainwave neurofeedback for Vietnam veterans with combat-related post-traumatic stress disorder. Medical Psychotherapy, 4(1), 47–60.
- Post-Traumatic Stress Disorder (NICE Guideline): National Clinical Practice Guideline. Published by British Psychological Society and RCPsych Publications (2005). ISBN 10: 190467125X ISBN 13: 9781904671251.
- Price, M., Gros, D. F., Strachan, M., Ruggiero, K. J., & Acierno, R. (2013). Combat experiences, pre-deployment training, and outcome of exposure therapy for post-traumatic stress disorder in operation enduring freedom/operation Iraqi freedom veterans. Clinical Psychology & Psychotherapy, 20(4), 277–285.
- Rauch, S., King, A. P., Abelson, J., Tuerk, P. W., Smith, E., Rothbaum, B. O., … Liberzon, I. (2015). Biological and symptom changes in posttraumatic stress disorder treatment: A randomized clinical trial. Depression and Anxiety, 32, 204–212.
- Ready, D. J., Gerardi, R. J., Backscheider, A. G., Mascaro, N., & Rothbaum, B. O. (2010). Comparing virtual reality exposure therapy to present centred therapy with 11 US Vietnam veterans with PTSD. Cyberpsychology, Behavior and Social Networking, 13(1), 49–54. PMID: 20528293.
- Reger, G., Koenen-Woods, P., Zetocha, K., Smolenski, D. J., Holloway, K. M., Rothbaum, B. O., & Gahm, G. A. (2016). Randomized controlled trial of prolonged exposure using imaginal exposure vs. virtual reality exposure in active duty soldiers with deployment-related posttraumatic stress disorder (PTSD). Journal of Consulting and Clinical Psychology, 84, 946–959.
- Resick, P., Nishith, P., Weaver, T. L., Astin, M. C., & Feuer, C. A. (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70(4), 867–879. PMID: 12182270.
- Resick, P. A., Wachen, J. S., Dondanville, K. A., Pruiksma, K. E., Yarvis, J. S., Peterson, A. L., … Young-McCaughan, S. (2017). Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 74(1), 28–36.
- Resick, P. A., Wachen, J. S., Mintz, J., Young-McCaughan, S., Roache, J. D., Borah, A. M., & Peterson, A. L. (2015). A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. Journal of Consulting and Clinical Psychology, 83, 1058–1068. Epub 2015 May 4.
- RevMan. (2014). Review manager 5 (RevMan 5) [Computer program] version 5.3. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration.
- Richardson, J. D., Thompson, A., King, L., Ketcheson, F., Shnaider, P., Armour, C., & Zamorski, M. A. (2019). Comorbidity patterns of psychiatric conditions in Canadian armed forces personnel. Canadian Journal of Psychiatry, 070674371881605. doi:10.1177/0706743718816057
- Richardson, L. K., Frueh, B. C., & Acierno, R. (2010). Prevalence estimates of combat-related post-traumatic stress disorder: Critical review. The Australian and New Zealand Journal of Psychiatry, 44(1), 4–19.
- Sautter, F. J., Glynn, S. M., Cretu, J. B., Senturk, D., & Vaught, A. S. (2015). Efficacy of structured approach therapy in reducing PTSD in returning veterans: A randomized clinical trial. Psychological Services, 12(3), 199–212.
- Schnurr, P., Friedman, M. J., Engel, C. C., Foa, E. B., Shea, M. T., Chow, B. K., … Bernardy, N. (2007). Cognitive behavioural therapy for posttraumatic stress disorder in women. JAMA, 28, 820–830.
- Schnurr, P., Friedman, M. J., Foy, D. W., Shea, M. T., Hsieh, F. Y., Lavori, P. W., & Bernardy, N. C. (2003). Randomized trial of trauma-focused group therapy for posttraumatic stress disorder. Archives of General Psychiatry, 60, 481–489.
- Shiner, B., D’Avolio, L. W., Nguyen, T. M., Zayed, M. H., Young-Xu, Y., Desai, R. A., & Watts, B. V. (2013). Measuring use of evidenced based psychotherapy for post-traumatic stress disorder. Administration and Policy in Mental Health, 40, 311–318.
- Steenkamp, M. M., Litz, B. T., Hoge, C. W., & Marmar, C. R. (2015). Psychotherapy for military-related ptsd: A review of randomized clinical trials. JAMA, 314(5), 489–500.
- Stein, N. R., Mills, M. A., Arditte, K., Mendoza, C., Borah, A. M., Resick, P. A., … Wright, E. (2012). A scheme for categorizing traumatic military events. Behavior Modification, 36(6), 787–807.
- Stevelink, S. A. M., Jones, M., Hull, L., Pernet, D., MacCrimmon, S., Goodwin, L., … Wessely, S. (2018). Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: A cohort study. European Journal of Psychotraumatology, 213(6), 690–697.
- Suris, A., Link-Malcolm, J., Chard, K., Ahn, C., & North, C. (2013). A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. Journal of Traumatic Stress, 26, 28–37.
- Tylee, D. S., Gray, R., Glatt, S. J., & Bourke, F. (2017). Evaluation of the reconsolidation of traumatic memories protocol for the treatment of PTSD: A randomized, wait-list-controlled trial. Journal of Military, Veteran and Family Health, 3(1), 21–33.
- van Gelderen, M. J., Nijdam, M. J., & Vermetten, E. (2018). An innovative framework for delivering psychotherapy to patients with treatment-resistant posttraumatic stress disorder: Rationale for interactive motion-assisted therapy. Front Psychiatry, 9(176). doi:10.3389/fpsyt.2018.00176
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5). Retrieved from the National Center for PTSD www.ptsd.va.gov
- Yehuda, R., Pratchett, L. C., Elmes, M. W., Lehrner, A., Daskalakis, N. P., Koch, E., & Bierer, L. M. (2014). Glucocorticoid-related predictors and correlates of post-traumatic stress disorder treatment response in combat veterans. Interface Focus, 4(5), 20140048.