ABSTRACT
Background: Caregivers play a key role in the success of trauma-focused cognitive behavioural therapy (TF-CBT). Yet, the effect of their alliance on treatment outcomes besides the other parties in treatment has hardly been studied.
Objective: This study examined the working alliance (WA) of therapists, patients and caregivers in TF-CBT and its contribution on treatment outcome over time.
Methods: N = 76 children and adolescents (mean age = 12.66 years, range 7–17, M/F ratio: .43) participated in the TF-CBT arm of a randomized controlled trial. The WA was assessed with the Working Alliance Inventory Short Version (WAI-S) at two measurement points, while symptom level of posttraumatic stress symptoms (PTSS) was assessed with the Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA). Paired sample t-tests, intraclass correlations (ICC), and mixed-effects regression models for longitudinal data were performed.
Results: The alliance rating was high across all informants, with caregivers achieving the highest rating. The average level of cross-informant agreement on the alliance was low between therapists and caregivers (ICC = .26) and moderate between therapists and patients (ICC =.65). A significant contribution of an alliance improvement to the reduction of PTSS over time was found in each of the two tested models: therapists with patients model (b = .682) and therapists with caregivers model (b = .807). However, these effects were not detected with all four perspectives in one comprehensive model.
Conclusion: In summary, the potential of caregivers’ views should receive more attention in the therapeutic process of trauma-focused therapy.
Antecedentes: los cuidadores desempeñan un papel clave en el éxito de la terapia cognitivo-conductual centrada en el trauma (TF-CBT por sus siglas en inglés). Sin embargo, el efecto de su alianza en los resultados del tratamiento, aparte de los otros participantes en el tratamiento, apenas se ha estudiado.
Objetivo: Este estudio examinó la alianza de trabajo (WA por sus siglas en inglés) de terapeutas, pacientes y cuidadores en TF-CBT y su contribución en el resultado del tratamiento a lo largo del tiempo.
Métodos: N = 76 niños y adolescentes (edad media = 12,66 años, rango 7-17, relación M/F: 0.43) fueron parte del brazo que recibía TF-CBT en un ensayo controlado aleatorio. La WA se evaluó con la versión abreviada del Inventario de la Alianza de Trabajo (WAI-S por sus siglas en inglés) en dos mediciones, mientras que el nivel sintomático de los síntomas de estrés postraumático (PTSS por sus siglas en inglés) fue evaluado con la Escala de TEPT administrada por el profesional clínico para niños y adolescentes (CAPS-CA por sus siglas en inglés). Se realizaron pruebas t de muestras pareadas, correlaciones intraclase (ICC por sus siglas en inglés) y modelos de regresión de efectos mixtos para datos longitudinales.
Resultados: La calificación de la alianza fue alta en todos los informantes, con los cuidadores logrando la calificación más elevada. El nivel promedio de acuerdo entre informantes sobre la alianza fue bajo entre terapeutas y cuidadores (ICC = .26, p = .002) y moderado entre terapeutas y pacientes (ICC = .65, p = <.001). Se encontró una contribución significativa de una mejora de la alianza a la reducción de PTSS a lo largo del tiempo en cada uno de los dos modelos probados: modelo de terapeutas con pacientes (b = –.682; p = .039) y modelo de terapeutas con cuidadores (b = –.807; p <.001). Sin embargo, estos efectos no se detectaron con las cuatro perspectivas en un modelo integral.
Conclusión: en resumen, el potencial de las opiniones de los cuidadores debería recibir más atención en el proceso terapéutico de la terapia centrada en el trauma.
背景:照顾者在聚焦创伤认知行为疗法 (TF-CBT) 的成功中起着关键作用。然而, 除治疗中其他各方之外, 他们的同盟对于治疗结果的影响几乎未曾被研究过。
目标:本研究考查了TF-CBT中治疗师, 患者和照顾者的工作同盟 (WA) 及其对治疗结果的长期影响。
方法:76名儿童和青少年 (平均年龄为 12.66岁, 范围为7-17岁, 男女比例:0.43) 参与了一项随机对照试验的TF-CBT组。在两个测量时间点上使用《工作同盟量表 (简短版) 》 (WAI-S) 对WA进行评估, 使用《临床用PTSD量表 (儿童和青少年版) 》 (CAPS-CA) 对创伤后应激症状 (PTSS) 的症状水平进行评估。进行配对样本t检验, 类内相关性 (ICC) 以及纵向数据的混合效应回归模型的分析。
结果:同盟得到的评分在各方报告者中都很高, 其中照顾者的评分最高。治疗师和照顾者之间同盟的交叉一致性平均水平较低 (ICC = 0.26, p=.002), 而治疗师与患者之间为中等水平 (ICC = 0.65, p= <.001) 。同盟程度提高对于降低PTSS的重要作用在两个检测模型中显著:治疗师与患者模型 (b =-.682; p=.039) 和治疗师与护理者模型 (b =-.807; p<.001) 。然而这些效应在涵盖四方角度的综合模型中未被发现。
结论:总之, 在聚焦创伤疗法的治疗过程中, 照顾者角度的潜力应给予更多关注。
1. Introduction
Caregivers play a crucial role in psychotherapy for children and adolescents in terms of initiating treatment and ensuring attendance. But beyond these common formal aspects, the effects of caregivers’ empathetic support and active participation in treatment on therapy outcomes for the child, as well as the impacts on parenting and on their own personal development, are complex processes that are not yet fully understood (Holt, Jensen, & Wentzel-Larsen, Citation2014).
Particularly their unique contribution to the therapeutic process is highly relevant to treatment success (Tutus et al., Citation2019). A good caregiver alliance is associated with more sessions attended, greater satisfaction with perceived improvement, and less drop-out in a sample with children presented with disruptive behaviour problems (Accurso, Hawley, & Garland, Citation2012). But what do we know about caregivers as support in the treatment process in trauma therapy with children and adolescents? The effectiveness of TF-CBT as a form of trauma treatment for children and adolescents has been sufficiently demonstrated as well as the long-term sustainability of the treatment gains (Cohen, Berliner, & Mannarino, Citation2010; Cohen, Deblinger, Mannarino, & Steer, Citation2004; Goldbeck, Muche, Sachser, Tutus, & Rosner, Citation2016; Jensen et al., Citation2014; Konanur, Muller, Cinamon, Thornback, & Zorzella, Citation2015). It is a component-based short-term therapy and active parental involvement is an integral part of the concept. Caregivers are viewed as active members of the treatment team (Cohen, Deblinger, & Mannarino, Citation2018; Cohen & Mannarino, Citation2015). Apart from children’s abuse-related attributions and cognitions, parental support is the strongest predictor of treatment outcome in sexually abused children (Cohen & Mannarino, Citation2000). In contrast, a lower level of youth-perceived parental treatment approval and no caregiver attendance at the first therapy session seem to be important predictors for dropout in youth trauma treatment (Ormhaug & Jensen, Citation2018). Therefore, an active and responsive behaviour in treatment by caregivers as well as concrete assistance of the child can contribute to a beneficial outcome in traumatized children and adolescents (Haine-Schlagel & Walsh, Citation2015). Therefore, alliance between caregivers and therapists is a parameter which should be investigated for its contribution to therapy outcome more in detail.
1.1. Working alliance and outcome in the treatment of traumatized children and adolescents
Alliance formation is a necessary precondition for any effective psychotherapeutic treatment process. Psychotherapy research has proven the mediating impact of alliances on outcomes in disorder-specific, cognitive behavioural treatments (Flückiger, Del Re, Wampold, Symonds, & Horvath, Citation2012). Alliance concepts used in research with children and adolescents are often based on those used in adult research, such as Bordin’s (Citation1979) tripartite construct where working alliance (WA) consists of an emotional bond, collaboration on tasks, and of agreement on goals (Bordin, Citation1979). Meanwhile, there is also substantial empirical evidence for a moderate effect of the WA as a predictor of outcome in the psychotherapeutic treatment of children and adolescents (McLeod, Citation2011; Shirk & Karver, Citation2003; Shirk, Karver, & Brown, Citation2011). There is a differential but inconclusive rater effect regarding the association of alliance and outcome. In a meta-analysis, reports from treatment providers were more strongly associated with outcomes than reports from children and adolescents or parents (McLeod et al., Citation2014; Shirk & Karver, Citation2003). Another meta-analysis found parents’ alliance reports were more strongly linked to treatment outcomes than youth and observer reports (McLeod, Citation2011). Analysis of early dropout from therapy found that parent-outcome association was an essential factor (Garcia & Weisz, Citation2002).
Parental involvement and a good alliance with the therapist during treatment of Post-Traumatic Stress Disorder (PTSD) may help mitigate obstacles to therapeutic success such as avoidance or dysfunctional mood regulation (Cloitre, Stovall-McClough, Miranda, & Chemtob, Citation2004), as well as reservations towards exposure techniques (Cohen et al., Citation2018; Zandberg et al., Citation2016). A stable triadic alliance can promote active problem solving and can strengthen engagement (Ormhaug, Jensen, Wentzel-Larsen, & Shirk, Citation2014). Caregivers play an important role in supporting the young patients between sessions and in stabilizing the success of therapy. In a sample of adolescent girls with PTSD participating in a trial with prolonged exposure therapy as one of the treatment conditions, a higher adolescent-to-therapist alliance score contributed significantly more to the improvement of post-traumatic stress symptoms compared to a moderate or low alliance rating over the treatment period (Capaldi, Asnaani, Zandberg, Carpenter, & Foa, Citation2016).
Given the important tasks of caregivers in the treatment of trauma, there is a need for a closer investigation of their perception of alliance in TF-CBT, the first-line treatment for children and adolescents with PTSD (Green, Citation2006; McLeod, Citation2011). Alliance ratings of caregivers during the therapy process have hardly been studied in the context of trauma therapy with children and adolescents.
1.2. Different rater perspectives of working alliances and their agreement in trauma-focused therapy
In TF-CBT for children and their families, the effect of the alliance in the triadic treatment process is now only beginning to be investigated. In a sample of adolescents with PTSD, the alliance rating of therapists and adolescents was moderately but differentially associated with treatment outcomes (Ormhaug et al., Citation2014). In a further study with the same sample, factor structure of therapist item ratings of an alliance rating scale were more organized around item content whereas adolescent ratings concentrated more on item valence, the affectively positive or negative wording of items (Ormhaug, Shirk, & Wentzel-Larsen, Citation2015). This would suggest that these two ratings are not interchangeable. Cross-informant agreement on an alliance between therapists and young clients were significantly but only moderately associated (Ormhaug et al., Citation2015). But to date, neither the alliance association between therapist and caregiver nor the inclusion of the caregiver perspective as an independent outcome predictor in TF-CBT have been included in investigations over the whole age spectrum of young patients. In a community-based Canadian sample of young children (7–12 years) and their caregivers, alliance remained positive and stable over the course of TF-CBT (Zorzella, Rependa, & Muller, Citation2017). The caregivers’ treatment expectancy at the beginning of the TF-CBT treatment phase did not predict a reduction in post-traumatic stress symptoms (PTSS), but their mid-treatment WA rating did do so (Kirsch, Keller, Tutus, & Goldbeck, Citation2018).
1.3. The present study
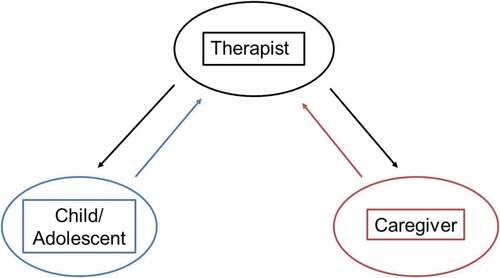
We therefore have scientific grounds for the closer examination of the caregiver’s perspective as a possible predictor of treatment outcome in TF-CBT. Two research gaps exist: First, the effect of the informant perspectives of alliances on treatment outcome, and second, the impact of changes over the course of alliance on treatment outcome regarding main effects of each alliance perspective. The present study aims to extend previous research by investigating the working alliance among participants in a randomized controlled trial of TF-CBT including different perspectives (three raters in the triad and four perspectives). First, we examined the temporal variations of alliance during treatment across informant perspectives (child/adolescent, therapist, and caregiver). We hypothesized that the working alliance would be positive and stable. Second, we examined the agreement of children/adolescents, their caregivers and therapists on the alliance rating. We hypothesized a moderate agreement between the perspectives. Third, we investigated the contribution of each alliance perspective on treatment outcome in terms of PTSS over the course of treatment. We hypothesized that we would detect significant main effects for both the patient and the caregiver alliance to the therapist.
2. Method
2.1. Design
Data for the present study were derived from the TreatChildTrauma study, a single-blind parallel group RCT conducted in eight child and adolescent mental health clinics in Germany. The primary objective of the main study was to establish the superiority of TF-CBT in reducing PTSS, assessed by independent raters at 4 months compared to a waitlist control group. The inclusion criteria were (1) aged between 7 and 17 years; (2) exposure to one or more traumatic event(s) after age 2 and dating back at least 3 months; (3) at least medium severity of PTSS as indicated by a total symptom score of ≥35 and at least one symptom per DSM-IV clusters B, C, and D assessed with the Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA); (4) PTSD as primary disorder; (5) availability of a non-offending adult caregiver for treatment; (6) willingness and ability of patients and their caregivers to attend weekly treatment sessions; (7) safe living conditions; (8) sufficient cognitive ability; and (9) sufficient command of the German language (for further details see Goldbeck et al., Citation2016). The current secondary analysis focused on data from the intervention group.
2.2. Ethical considerations
The study was approved by the Ethics Committee of the University of Ulm. Patients who fulfilled all inclusion criteria after a comprehensive clinical assessment were given written and verbal information about the study and informed consent was obtained from both patients and caregivers.
2.3. Participants
N = 159 children and adolescents aged between 7 and 17 years were randomly assigned to either the intervention group (TF-CBT arm) or waitlist group (for power calculation, see Goldbeck et al., Citation2016). The subsample for the current study (intervention group) consisted of n = 76 patients and their respective accompanying caregivers (). The mean age was 12.66 (SD = 2.92). They had experienced an average of 6.26 (SD = 3.45) different traumatic events. Trauma was defined in the study according to the A criteria of DSM IV. Sexual abuse, sexual assaults, physical violence, and witnessing domestic violence were the most frequently reported traumatic index events. Concerning interpersonal traumatic index events, in 31 cases there was an intrafamilial offender, in 27 cases an extrafamilial offender. (for further details see Goldbeck et al., Citation2016).
A total of 26 trained therapists participated in the study; their mean age was 37.36 (SD = 9.08) and they were predominantly female (n = 18, 69.2%). The study therapists were mainly psychologists (licenced psychotherapists or still in training) or child and adolescent psychiatrists (residents or specialists). Their overall mean therapy experience was 8.32 (SD = 7.93) years and they had an average of 2.89 (SD = 3.05, range = 1–13) study cases. Therapists treated on average three patients over the duration of the study (M = 2.85, SD = 3.07).
A total of 57 caregivers accompanied a patient during the treatment phase. They were predominately female (n = 48, 84.2%), and their mean age was 42.38 (SD = 7.07). The majority had 9–11 years in school (n = 38, 66.7%), were currently employed (n = 40, 70.2%) and did not live together as parents (n = 33, 57.9%). Relationship to the study patient was either a biological parent (n = 57, 75.0%), a foster parent or a responsible social worker (n = 16, 21.1%), or another relative (n = 2, 2.6%).
2.4. Procedure and intervention
Recruitment was performed in eight participating urban and rural study centres. TF-CBT is a component-based, short-term intervention that targets PTSD in children and adolescents (Cohen, Mannarino, & Deblinger, Citation2006). The treatment comprises nine components included in three phases: (1) stabilization and skills development, (2) exposure to and cognitive processing of the trauma, and (3) fostering safety and future development. The study protocol consisted of 12 weekly 90-min parallel or combined sessions with patients and caregivers over a period of 4 months. A gender matching between patient and therapist was undertaken in case of sexual abuse and if a patient expressed an explicit wish.
2.5. Measures
The four alliance perspectives of three informants (child/adolescent and therapist evaluations of their alliance; caregiver and therapist evaluations of their alliance) were assessed at two measurement points: mid-treatment (after session 6) and post-treatment (at least 2 weeks after the last session). Symptoms were evaluated at baseline and at post-treatment ().
2.5.1. The Working Alliance Inventory (WAI)
This is one of the most frequently used and tested instruments to measure alliance levels in adult psychotherapy process research (Horvath & Greenberg, Citation1989). There is a therapist and a patient version. It has also been used in psychotherapy studies with children and adolescents (Anderson et al., Citation2012; Capaldi et al., Citation2016). The short form (WAI-S (Tracey & Kokotovic, Citation1989)) is a 12-item scale, which includes three subscales: goal (agreement on goals in therapy), task (agreement on achieving these goals), and bond (between patient and therapist). Participants rate on a 7-point scale from 1 (never) to 7 (always) the extent to which they agree with each item for their present alliance.
The total scores range from 12 to 84. We adapted the patient (WAI-S-P) and therapist (WAI-S-T) version for use in this study. Both measures were translated and back-translated using a systematic process based on recommendations for good practice (Wild et al., Citation2005). The caregiver-therapist version (WAI-S-CT) and the therapist-caregiver version (WAI-S-TC) were adapted to contain the same items, which were reworded for use in the target population. Cronbach’s alpha for the adapted German versions’ total scores were .88 (WAI-S-P), .95 (WAI-S-T), .86 (WAI-S-CT), and .96 (WAI-S-TC).
2.5.2. The Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA (Nader, Kriegler, & Blake, Citation2002))
This measure is a clinician-administered PTSD interview for children and youths aged 8 to 18 years. It assesses the diagnostic criteria of PTSD according to DSM-IV and provides a total symptom intensity and frequency score. The German version of the CAPS-CA has an interrater-reliability of κ = .68 and the internal consistency of the total symptom score is α = .91 (Steil & Füchsel, Citation2006). In the study, the structured interview was administered by trained and supervised Master students (psychology). They were blinded for the participant’s group allocation. It was assured that the students were not previously involved with the same patient and there was a cross-check before and after each interview.
2.6. Data analysis
Paired t-tests were conducted to compare the means of the alliance reports of different rater perspectives from two measurement points (mid- and post-treatment). Intra-class correlations were performed to assess cross-informant agreement between child/adolescent, caregiver and therapist perspectives on their alliance rating.
2.6.1. Data structure
Clients and caregivers are nested within therapists. Therefore, a reciprocal design was used; data were generated by both patients and caregivers (‘many’) and therapists (‘one’, Marcus, Kashy & Baldwin, Citation2009). The non-independence of the data was considered by calculating mixed-effects regression models for panel data with random time effects, random effects for WA and fixed time*WA interaction effects to extract the contributions of alliance ratings on treatment outcome. The advantages of this method are that they account for the correlated structure of repeated measurements on the same person, contain both fixed and random effects, and include all variables in one model. It was modelled by means of the clustered sandwich estimator for variances and standard errors using the ID (identifier) of the therapist as the cluster variable (Huber Citation1967; White Citation1980). First, two models were fitted (model 1: therapists with patients, model 2: therapists with caregivers): CAPS-CA score as the outcome variable, the WAI scores of each of the perspectives as fixed effects, a random linear time effect indicating changes in PTSD from baseline to post-treatment, and WAI informant perspective*time interaction indicating the moderating effect of WAI on the PTSD change. Since WAI scores were entered in the regression model as centred to the grand mean, the regression coefficient for the interaction effects indicates the change of the linear time effect resulting from a one-unit deviation of the individual WAI score from the mean WAI score. As a second step, both separate models were fitted into one model to determine which alliances predict PTSS while controlling for the other alliances.
WAI-completers of both measurement points did not differ from non-completers (with only one completed measure) with respect to sex, age, type of index event, number of traumatic event types and number of comorbid disorders. Missing values were therefore assumed to be random and all cases were included in the analyses. Analyses were conducted using the SPSS 21 and Stata 14.0 software packages.
3. Results
3.1. Level of alliance and temporal change across informant perspectives
Alliance rating was high across all informants (). Therapists tended to rate the alliance lower than patients and caregivers, while the latter rated it highest (mid-treatment: M = 76.19 (SD = 6.41)), post-treatment: M = 76.49 (SD = 6.08). In the patient-therapist dyad, alliance ratings increased significantly between the mid- to post-treatment phases (patients: t = 3.16 (50), p = <.01, therapists: -t = 2.83 (65), p = .01). Both effect sizes were d = .40.
Table 1. Socio-demographic and clinical characteristics of patients (N = 76)
Table 2. Means and standard deviations of sum scores of the Working Alliance Inventory short form (WAI-S) from four perspectives at mid-treatment and post-treatment; mean differences with paired t-tests, effect sizes (Cohens d)
3.2. Rater agreement on the alliance
There was significant but low cross-informant agreement on the therapist-to-caregiver alliance (ICC = 0.26, p = .002), and significant, moderate agreement between informants on the therapist-to-patient alliance (ICC = 0.65, p = <.001). Patients and caregivers significantly agreed on their alliance with the therapist (ICC = 0.50, p = <.001).
3.3. The working alliance and symptom change
shows the correlation matrix of all working alliance ratings and PTSS score including the two measurement points. We see a clear increase in both the associations between patient-to therapist with therapist-to patient alliance rating from mid- to post-treatment (r = .369, p < .001; r = .659, p < .001) and between therapist-to-caregiver and therapist-to patient alliance rating from mid- to post-treatment (r = .489, p < .001; r = .664, p < .001).
Table 3. Pearson correlation matrix for WAI and CAPS-CA ratings (mid- and post-treatment)
shows the results for the two mixed-effects regression models including the variance components and the model parameters. For model 1 (therapists with patients), the significant negative regression coefficient found revealed that PTSS decreased significantly from baseline to post-treatment by 28.982 points. In addition, the regression coefficient for the time*WAI interaction of b = −.682 (p = .039) indicated that each additional increase of the mean WAI score in the patient-to-therapist direction of the relationship by one unit was significantly associated with a further reduction of the PTSS by .682. In model 2 (therapists with caregivers), an additional reduction of PTSS determined by WAI over time was found in the therapist with caregiver rating (b = −.807, p < .001). In sum, the working alliance increased over the course of therapy and the increase is associated with an improved outcome (reduction of symptoms) in the patient-to-therapist and in the therapist-to-caregiver relationship.
Table 4. Results of the mixed-effects regression analysis
However, when we adjusted one model with all alliance ratings, there were no significant effects anymore (for table with results of the mixed-effects regression analysis, see supplemental material).
4. Discussion
To our knowledge, this is one of the first studies which include different alliance ratings (including the caregiver perspective) and investigates its contribution on treatment outcome over time among children and adolescents with PTSD, treated with TF-CBT. In the first step we tested two separate models (therapists with patients and therapists with caregivers). Contrary to our hypothesis, we did not find significant main effects but only significant time interaction effects, one per model: the increase of patient alliance to therapist rating and therapist to caregiver rating over time was significantly associated with a reduction of PTSS. Both significant effects had the same direction. One explanation why the child (patient) and not the therapist rating is predictive in model 1 could be that the patient experiences a unique with fundamental change with the support of the therapist whereas the therapist has more than one working alliance and views it more generally from a professional point of view. The question why instead the therapist rating and not the caregiver rating is predictive in model 2 is more difficult to interpret. Both therapist and caregiver put much effort in their alliance for the best interest of the child. Therapists might be influenced in their final judgement by their professional success and caregivers are not frequently enough involved in the therapeutic process.
Our data shows more clearly the time effects instead of the main effects. This is underlined by the increase of the strong positive correlations between patient-to therapist and therapist-to patient alliance and between therapist-to-caregiver and therapist-to patient alliance over time. The alliance in the patient-therapist-dyad seems to grow over time and the therapist evaluates their relationship with accompanying caregivers obviously more positive at the end of an intensive collaboration. This is also the case for caregivers in their judgement of the alliance to the therapist, seen in a more moderate correlation. However, we did not detect significant other main or interaction effects anymore when we put all four perspectives in one model and tested them against one another. The reasons why we found significant results in the separate models but not in a comprehensive model are complex: alliance ratings are intercorrelated among themselves and therefore it might be difficult to detect their single unique contribution on PTSS. Even if we do not find an effect it does not mean that there is no effect. A cautions conclusion could be that the increase of alliance over time in both dyads (therapists with-caregivers and therapists with patients) might be a hint that it plays a crucial role in the treatment process. Further research in the field with larger samples might help to determine and to prove our findings.
To date, the effect of the informant perspectives has predominantly been found in other diagnoses (Accurso & Garland, Citation2015; Bickman et al., Citation2012; Hawley & Garland, Citation2008). Increasing alliance strength is positively associated with a decrease of PTSS during trauma-focused therapy. Our findings extend previous results in adolescents with PTSD (Capaldi et al., Citation2016) to a slightly younger sample and also to the therapist-to-caregiver relationship. The alliance between therapists and caregivers has a predictive positive effect on reducing PTSS in trauma-focused therapy. As already indicated in previous studies (Chiu, McLeod, Har, & Wood, Citation2009; Fjermestad et al., Citation2016), our results underline the facilitative role of caregiver alliance in supporting clinical outcomes in trauma-focused therapy for children and adolescents.
On average, the alliance was evaluated particularly high by patients and caregivers. In contrast, therapists rated the alliance somewhat lower. These findings are consistent with other studies on alliances (Accurso & Garland, Citation2015; Hawley & Garland, Citation2008). The discrepancy may reflect the intersubjective views of clients, caregivers and therapists on the alliance construct. It could be that because therapists see multiple patients and therefore rate their alliances to patients more universal. On the contrary, patients and caregivers only see a single therapist. Therefore, they might do their ratings more nuanced. Evidence suggests that therapists’ answers in self-reporting measures cluster more around item content and the commitment level and working ability of the client, whereas patients’ items are structured along emotional aspects. Patients focus more on helpfulness and mutual participation in therapeutic work (Bachelor, Citation2013; Ormhaug et al., Citation2015). The differences suggest that patients and probably also caregivers report a highly helpful and valuable alliance with the therapist, which the latter may not be aware of. Therapists might not recognize the affective importance of the alliance for patients and caregivers because they focus on other factors in therapy. A feedback system on the working alliance during treatment might support therapists in their perception of the quality of the alliance from the viewpoint of patients and caregivers.
We identified a significant improvement in alliance level in the patient-therapist dyad from mid- to post-treatment with small effect sizes, but not in the caregiver-therapist dyad. In adult psychotherapy, it has been demonstrated that the therapeutic relationship established in the early phase of treatment predicts performance in the exposure phase (Cloitre et al., Citation2004). Our results suggest that even during exposure tasks around mid-treatment, the alliance could still further improve. It is recommended that therapists pay closer attention to micro-processes in alliance development between patients and caregivers during the joint psychotherapeutic process in TF-CBT. We found good patient-therapist agreement and even moderate caregiver agreement on their alliance with the therapist. This is consistent with earlier studies (Accurso & Garland, Citation2015; Ormhaug et al., Citation2015) and can be assumed as a common agreement on the goals, tasks and bonds of the three parties in child and adolescent therapy. This is of substantial importance for therapeutic work in trauma-focused therapy and increases in treatment effectiveness.
4.1. Implications for research and practice
The impact of caregivers and the additional benefit which their accompaniment offers to the treatment process of children and adolescents with PTSD needs to be studied in more detail. In particular, it would be interesting to investigate how the quality of the relationship between caregiver and child/adolescent might benefit from treatment as a mid-term or long-term effect. Clinical implications are that therapists should focus more deliberately on the triadic therapy process in child and adolescent therapies considering caregivers’ impressions, too. In joint sessions with caregivers, therapists should emphasize on clarity and guidance about next steps in the therapeutic process and ask about problems and obstacles during the past phase. It creates trust and a sense of belonging together in the therapeutic triad. Clinicians should take the time during the assessment and ongoing treatment phases to build and maintain a positive relationship with their clients and the accompanying adult. One suggestion to implement these research findings would be to continuously obtain direct feedback (via questionnaire) from all parties on the current status of therapy, including on relationship issues.
4.2. Strengths and limitations
The strengths of this study are the standardized data collection in an RCT in urban and rural settings, the inclusion of bidirectional informant perspectives on the alliance at two measurement points, and the use of statistical methods which control for the non-independent structure of a one-with-many design.
The study’s limitations must also be mentioned. Sample size is moderate and may be a restricting factor for the generalization of findings. More frequent measurement points of alliance and PTSS, especially at the beginning of treatment, could help to look at micro-changes between sessions and rupture-and-repair processes. Alliance scores measured by self-report questionnaires for patients and caregivers were in the upper range of the scale. This ceiling effect is also observed in other alliance studies and is therefore not an uncommon problem when people are asked about their personal experiences and satisfaction at the end of a therapy episode. It shows the limitations of self-reporting data in terms of predictive value (Kendall et al., Citation1997). Gender as a possible moderator for the results was also not considered in the analysis. Furthermore, not assessing the working alliance between child and caregiver is a limitation. In the study results, causation might also be implied in the reverse direction: alliance ratings improve when symptoms improve over the course of therapy. Clients might grow to trust therapists more when therapy proves effective.
5. Conclusion
The WA as a predictor seems to be a critical factor in trauma-focused therapy for children and adolescents. The findings demonstrate a stable, strong and even increasing alliance in the therapeutic triad of children and adolescents, caregivers and therapists. The results give hints that there might be a significant impact for the therapist to caregiver alliance on the decrease in PTSS of patients over time, yet the effects could not be detected in a more comprehensive statistical model. Monitoring the WA from all participating parties in the treatment process would be a clinical implication, as it can help therapists remain sensitive to the development of the therapeutic relationship as a significant factor in producing and promoting change.
Supplemental Material
Download MS Word (14.6 KB)Acknowledgments
The authors would like to thank all participating patients and caregivers, the study site directors and coordinators, all study therapists, assessors and research assistants, the clinical consultants, and the members of the study board.
Disclosure statement
No potential conflict of interest.
Data availability statement
Given that the ethical committee agrees, the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request ([email protected]).
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Accurso, E. C., & Garland, A. F. (2015). Child, caregiver, and therapist perspectives on therapeutic alliance in usual care child psychotherapy. Psychological Assessment, 27(1), 347–10.
- Accurso, E. C., Hawley, K. M., & Garland, A. F. (2012). Psychometric properties of the therapeutic alliance scale for caregivers and parents. Psychological Assessment, 25(1), 244–252.
- Anderson, R. E., Spence, S. H., Donovan, C. L., March, S., Prosser, S., & Kenardy, J. (2012). Working alliance in online cognitive behavior therapy for anxiety disorders in youth: Comparison with clinic delivery and its role in predicting outcome. Journal of Medical Internet Research, 14(3), e88.
- Bachelor, A. (2013). Clients’ and therapists’ views of the therapeutic alliance: Similarities, differences and relationship to therapy outcome. Clinical Psychology & Psychotherapy, 20(2), 118–135.
- Bickman, L., de Andrade, A. R. V., Athay, M. M., Chen, J. I., de Nadai, A. S., Jordan-Arthur, B. L., & Karver, M. S. (2012). The relationship between change in therapeutic alliance ratings and improvement in youth symptom severity: Whose ratings matter the most? Administration and Policy in Mental Health and Mental Health Services Research, 39(1–2), 78–89.
- Bordin, E. (1979). The generalizability of the psychoanalytic concept of working alliance.psychology and psychotherapy. Theory, Research and Practice, 16, 252–260.
- Capaldi, S., Asnaani, A., Zandberg, L. J., Carpenter, J. K., & Foa, E. B. (2016). Therapeutic alliance during prolonged exposure versus client-centered therapy for adolescent posttraumatic stress disorder. Journal of Clinical Psychology, 72(10), 1026–1036.
- Chiu, A. W., McLeod, B. D., Har, K., & Wood, J. J. (2009). Child-therapist alliance and clinical outcomes in cognitive behavioral therapy for child anxiety disorders. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 50(6), 751–758.
- Cloitre, M., Stovall-McClough, K. C., Miranda, R., & Chemtob, C. M. (2004). Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 72(3), 411–416.
- Cohen, J. A., Berliner, L., & Mannarino, A. (2010). Trauma focused CBT for children with co-occurring trauma and behavior problems. Child Abuse & Neglect, 34(4), 215–224.
- Cohen, J. A., Deblinger, E., & Mannarino, A. P. (2018). Trauma-focused cognitive behavioral therapy for children and families. Psychotherapy Research: Journal of the Society for Psychotherapy Research, 28(1), 47–57.
- Cohen, J. A., Deblinger, E., Mannarino, A. P., & Steer, R. A. (2004). A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 43(4), 393–402.
- Cohen, J. A., Mannarino, A., & Deblinger, E. (2006). Treating trauma and traumatic grief in children and adolescents. New York: Guilford Publications.
- Cohen, J. A., & Mannarino, A. P. (2000). Predictors of treatment outcome in sexually abused children. Child Abuse & Neglect, 24(7), 983–994.
- Cohen, J. A., & Mannarino, A. P. (2015). Trauma-focused cognitive behavior therapy for traumatized children and families. Child and Adolescent Psychiatric Clinics of North America, 24(3), 557–570.
- Fjermestad, K. W., Lerner, M. D., McLeod, B. D., Wergeland, G. J. H., Heiervang, E. R., Silverman, W. K., … Haugland, B. S. M. (2016). Therapist-youth agreement on alliance change predicts long-term outcome in CBT for anxiety disorders. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 57(5), 625–632.
- Flückiger, C., Del Re, A. C., Wampold, B. E., Symonds, D., & Horvath, A. O. (2012). How central is the alliance in psychotherapy? A multilevel longitudinal meta-analysis. Journal of Counseling Psychology, 59(1), 10–17.
- Garcia, J., & Weis, A. (2002). When youth mental health care stops: Therapeutic relationship problems and other reasons for ending youth outpatient treatment. Journal of Consulting and Clinical Psychology, 70, 439–443.
- Goldbeck, L., Muche, R., Sachser, C., Tutus, D., & Rosner, R. (2016). Effectiveness of trauma-focused cognitive behavioral therapy for children and adolescents: A randomized controlled trial in eight German mental health clinics. Psychotherapy and Psychosomatics, 85(3), 159–170.
- Green, J. (2006). Annotation: The therapeutic alliance–a significant but neglected variable in child mental health treatment studies. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 47(5), 425–435.
- Haine-Schlagel, R., & Walsh, N. E. (2015). A review of parent participation engagement in child and family mental health treatment. Clinical Child and Family Psychology Review, 18(2), 133–150.
- Hawley, K. M., & Garland, A. F. (2008). Working alliance in adolescent outpatient therapy: Youth, parent and therapist reports and associations with therapy outcomes. Child and Youth Care Forum, 37(2), 59–74.
- Holt, T., Jensen, T. K., & Wentzel-Larsen, T. (2014). The change and the mediating role of parental emotional reactions and depression in the treatment of traumatized youth: Results from a randomized controlled study. Child and Adolescent Psychiatry and Mental Health, 8, 11.
- Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the working alliance inventory. Journal of Counseling Psychology, 36(2), 223–233.
- Huber, P. J. (1967). The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. 1, 221–233. Berkeley: University of California Press.
- Jensen, T. K., Holt, T., Ormhaug, S. M., Egeland, K., Granly, L., Hoaas, L. C., … Wentzel-Larsen, T. (2014). A randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. Journal of Clinical Child & Adolescent Psychology, 43(3), 356–369.
- Kendall, P. C., Flannery-Schroeder, E., Panichelli-Mindel, S. M., Southam-Gerow, M., Henin, A., & Warman, M. (1997). Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology, 65(3), 366–380.
- Kirsch, V., Keller, F., Tutus, D., & Goldbeck, L. (2018). Treatment expectancy, working alliance, and outcome of trauma-focused cognitive behavioral therapy with children and adolescents. Child and Adolescent Psychiatry and Mental Health, 12, 16.
- Konanur, S., Muller, R. T., Cinamon, J. S., Thornback, K., & Zorzella, K. P. M. (2015). Effectiveness of trauma-focused cognitive behavioral therapy in a community-based program. Child Abuse & Neglect, 50, 159–170.
- Marcus, D. K., & Kashy, D. A., & Baldwin, S. A. (2009). Studying Psychotherapy using the One-With-Many Design: The Therapeutic Alliance as an Exemplar. Journal of Counseling Psychology, 56, 537–548. doi:10.1037/a0017291.
- McLeod, B. D. (2011). Relation of the alliance with outcomes in youth psychotherapy: A meta-analysis. Clinical Psychology Review, 31(4), 603–616.
- McLeod, B. D., Islam, N. Y., Chiu, A. W., Smith, M. M., Chu, B. C., & Wood, J. J. (2014). The relationship between alliance and client involvement in CBT for child anxiety disorders. Journal of Clinical Child & Adolescent Psychology, 43(5), 735–741.
- Nader, K., Kriegler, J., & Blake, D. (2002). The clinician- administered PTSD scale for children and adolescents for DSM-IV (CAPS-CA). White River Junction: National Centre for PTSD.
- Ormhaug, S. M., & Jensen, T. K. (2018). Investigating treatment characteristics and first-session relationship variables as predictors of dropout in the treatment of traumatized youth. Psychotherapy Research: Journal of the Society for Psychotherapy Research, 28(2), 235–249.
- Ormhaug, S. M., Jensen, T. K., Wentzel-Larsen, T., & Shirk, S. R. (2014). The therapeutic alliance in treatment of traumatized youths: Relation to outcome in a randomized clinical trial. Journal of Consulting and Clinical Psychology, 82(1), 52–64.
- Ormhaug, S. M., Shirk, S. R., & Wentzel-Larsen, T. (2015). Therapist and client perspectives on the alliance in the treatment of traumatized adolescents. European Journal of Psychotraumatology, 6, 27705.
- Shirk, S. R., & Karver, M. (2003). Prediction of treatment outcome from relationship variables in child and adolescent therapy: A meta-analytic review. Journal of Consulting and Clinical Psychology, 71(3), 452–464.
- Shirk, S. R., Karver, M. S., & Brown, R. (2011). The alliance in child and adolescent psychotherapy. Psychotherapy (Chicago, ILL.), 48(1), 17–24.
- Steil, R., & Füchsel, G. (2006). IBS-KJ. Interviews zu Belastungsstörungen bei Kindern und Jugendlichen. IBS-KJ. Interviews zu Belastungsstörungen bei Kindern und Jugendlichen. Diagnostik der Akuten und der Posttraumatischen Belastungsstörung. Göttingen: Hogrefe-Verlag.
- Tracey, T. J., & Kokotovic, A. M. (1989). Factor structure of the working alliance inventory. Psychological Assessment, 1, 207–210.
- Tutus, D., Goldbeck, L., Pfeiffer, E., Sachser, C., & Plener, P. L. (2019). Parental dysfunctional posttraumatic cognitions in trauma-focused cognitive behavioral therapy for children and adolescents. Psychological Trauma: Theory, Research, Practice and Policy, 11(7), 722–731.
- White, H. L., Jr. (1980). A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica, 48, 817–838.
- Wild, D., Grove, A., Martin, M., Eremenco, S., McElroy, S., Verjee-Lorenz, A., & Erikson, P. (2005). Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) Measures: Report of the ISPOR task force for translation and cultural adaptation. Value in Health, 8(2), 94–104.
- Zandberg, L., Kaczkurkin, A. N., McLean, C. P., Rescorla, L., Yadin, E., & Foa, E. B. (2016). Treatment of adolescent PTSD: The impact of prolonged exposure versus client-centered therapy on co-occurring emotional and behavioral problems. Journal of Traumatic Stress, 29(6), 507–514.
- Zorzella, K. P. M., Rependa, S. L., & Muller, R. T. (2017). Therapeutic alliance over the course of child trauma therapy from three different perspectives. Child Abuse & Neglect, 67, 147–156.