ABSTRACT
Objective
To perform a systematic and meta-analysis on the prevalence rates of mental health symptoms including anxiety and depression during the COVID-19 pandemic in the general population in Eastern Europe, as well as three select sub-populations: students, general healthcare workers, and frontline healthcare workers.
Data sources
Studies in PubMed, Embase, Web of Science, PsycINFO, and medRxiv up to 6 February 2021.
Eligibility criteria and data analysis
Prevalence rates of mental health symptoms in the general population and key sub-populations during the COVID-19 pandemic in Eastern Europe. Data were pooled using a random-effects meta-analysis to estimate the prevalence rates of anxiety and depression.
Results
The meta-analysis identifies and includes 21 studies and 26 independent samples in Eastern Europe. Poland (n = 4), Serbia (n = 4), Russia (n = 3), and Croatia (n = 3) had the greatest number of studies. To our knowledge, no studies have been conducted in eleven Eastern European countries including Hungary, Slovakia, and Slovenia. The pooled prevalence of anxiety in 18 studies with 22 samples was 30% (95% CI: 24–37%) pooled prevalence of depression in 18 studies with 23 samples was 27% (95% CI: 21–34%).
Implications
The cumulative evidence from the meta-analysis reveals high prevalence rates of clinically significant symptoms during the COVID-19 pandemic in Eastern Europe. The findings suggest evidence of a potential mental health crisis in Eastern Europe during the ongoing COVID-19 pandemic. Our synthesis also reveals a relative lack of studies in certain Eastern European countries as well as high heterogeneities among the existing studies, calling for more effort to achieve evidence-based mental healthcare in Eastern Europe.
HIGHLIGHTS
The pooled prevalence of anxiety and depression in Eastern Europe were 30% and 27%, respectively.
Forty-one per cent of frontline healthcare workers suffered mental health symptoms.
Southeastern Europe (Balkans) had lower prevalence of mental health symptoms than the rest of Eastern Europe.
Objetivo: Realizar un metanálisis sistemático sobre las tasas de prevalencia de síntomas de salud mental, incluidos ansiedad y depresión durante la pandemia de COVID-19 en la población general de Europa del Este, así como en tres subpoblaciones seleccionadas: estudiantes, trabajadores sanitarios generales y trabajadores sanitarios de primera línea.
Fuentes de datos: Estudios en PubMed, Embase, Web of Science, PsycINFO y medRxiv hasta el 6 de febrero de 2021.
Criterios de elegibilidad y análisis de datos: Tasas de prevalencia de síntomas de salud mental en la población general y subpoblaciones claves durante la pandemia de COVID-19 en Europa del Este. Los datos se combinaron mediante un metanálisis de efectos aleatorios para estimar las tasas de prevalencia de ansiedad y depresión.
Resultados: El metanálisis identifica e incluye 21 estudios y 26 muestras independientes en Europa del Este. Polonia (n = 4), Serbia (n = 4), Rusia (n = 3) y Croacia (n = 3) tuvieron el mayor número de estudios. Hasta donde sabemos, no se han realizado estudios en once países de Europa del Este, incluidos Hungría, Eslovaquia y Eslovenia. La prevalencia combinada de ansiedad en 18 estudios con 22 muestras fue de 30% (IC del 95%: 24–37%) y la prevalencia combinada de depresión en 18 estudios con 23 muestras fue de 27% (IC del 95%: 21–34%).
Implicaciones: La evidencia acumulada del metanálisis revela altas tasas de prevalencia de síntomas clínicamente significativos durante la pandemia de COVID-19 en Europa del Este. Los hallazgos sugieren evidencia de una posible crisis de salud mental en Europa del Este durante la pandemia de COVID-19 en curso. Nuestra síntesis también revela una relativa falta de estudios en ciertos países de Europa del Este, así como una gran heterogeneidad entre los estudios existentes, lo que exige un mayor esfuerzo para lograr una atención de la salud mental basada en la evidencia en Europa del Este.
目的: 对东欧普通人群以及三个选定亚组人群 (学生, 普通医疗工作者及前线医护人员) 在 COVID-19 疫情期间包括焦虑和抑郁在内的心理健康症状的流行率进行系统和元分析。
数据来源: 截至 2021 年 2 月 6 日的 PubMed, Embase, Web of Science, PsycINFO 和 medRxiv 中的研究。
资格标准和数据分析: 东欧 COVID-19 疫情期间一般人群和关键亚组人群中心理健康症状的流行率。使用随机效应元分析汇总数据以估计焦虑和抑郁的流行率。
结果: 元分析确定并纳入了东欧的 21 项研究和 26 个独立样本。波兰 (n = 4), 塞尔维亚 (n = 4), 俄罗斯 (n = 3) 和克罗地亚 (n = 3) 的研究数量最多。据我们所知, 尚未在包括匈牙利, 斯洛伐克和斯洛文尼亚在内的 11 个东欧国家进行过研究。在 22 个样本的 18 项研究中, 焦虑的汇总流行率为 30% (95% CI:24%–37%), 而在 18 项研究 (包括 23 个样本) 中抑郁的汇总流行率为 27% (95% CI:21%–34%)。
启发: 元分析的累积证据显示, COVID-19 疫情期间东欧的临床显著症状流行率很高。研究结果表明, 在持续的 COVID-19 疫情期间, 东欧存在潜在的心理健康危机。我们的综合法还揭示了在某些东欧国家的研究相对缺乏, 以及现有研究之间的高度异质性, 呼吁为在东欧实现循证心理保健做出更多努力。
1. Introduction
The COVID-19 pandemic (Pappa et al., Citation2020), with more than 225 million confirmed cases and 4.6 million deaths by September 2021 (Holmes et al., Citation2020), has taken a toll on mental health, due to fear of illness and hospitalization, the effects of social isolation, and economic downturn (Holmes et al., Citation2020; Moroń & Biolik-Moroń, Citation2021; Xiong et al., Citation2020). To assess mental health during the COVID-19 pandemic, several meta-analyses have polled the prevalence of mental health symptoms in several countries or regions, such as China (Chen et al., Citation2021a), Southeast Asia (Pappa et al., Citation2021), and South Asia (Hossain et al., Citation2021). These meta-analytical studies have provided crucial evidence on mental health in specific regions and uncovered important heterogeneity to enable evidence-based healthcare in those regions. Such research should be conducted by regions around the world, since the mental, behavioural and cognitive state under the pandemic may vary across regions for cultural, geosocial and policy or public health-related factors (Ding et al., Citation2021; Kołodziejczyk et al., Citation2021). However, the literature still lacks meta-analytical evidence on the prevalence of mental health symptoms in Eastern Europe – a vast region that has been affected by the COVID-19 pandemic in the past year (Stephen, Zhang, & Gao, Citationin press; Villani, Pastorino, Ricciardi, Ioannidis, & Boccia, Citation2021). Eastern Europe has struggled to manage the pandemic, and has suffered from high mortality and morbidity rates (Grabowski, Witkowska, & Bidzan, Citation2021). Mental health research has historically overlooked Eastern Europe (Krupchanka & Winkler, Citation2016), where mental health epidemiology is still regarded with intense stigma and direct evidence on the topic remains scarce (Franic & Dodig-Curkovic, Citation2020). Even prior to the pandemic, Eastern Europe has been relatively weak in identifying people with mental health symptoms (Krupchanka & Winkler, Citation2016). Furthermore, recent changes in healthcare systems and lack of per capita funding for community mental health resources presents some unique issues in mental health practice at the system level in Eastern Europe (Babicki, Szewczykowska, & Mastalerz-Migas, Citation2021; Krupchanka & Winkler, Citation2016). Such issues have resulted in a lack of evidence-based mental health practices (Franic & Dodig-Curkovic, Citation2020).
This study aims to address this knowledge gap by presenting the first meta-analysis to quantify the prevalence of anxiety and depression during the COVID-19 pandemic in Eastern Europe. We performed a systematic review of the prevalence of anxiety and depression of the general population as well as healthcare workers (HCW) during the COVID-19 pandemic in Eastern European countries. Such meta-analytical pooled prevalence of mental health symptoms provides crucial evidence to enable evidence-based healthcare policies and resource deployment and also creates opportunities for decision-making on prevention.
2. Methodology
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement 2019 and is registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020224458) (Moher et al., Citation2015).
2.1. Data sources and database search strategy
A comprehensive literature search was performed in the following databases on 6 February 2021: Web of Science, PUBMED, EMBASE, and medRxiv based on keywords shown in Appendix A with Boolean operators. Google Scholar cannot be searched with the same set of search procedures systematically. To maintain the same search procedure consistently, we used Google Scholar as a complementary search tool to identify an additional four articles.
2.2. Selection criteria
We selected the empirical studies what reported the prevalence of anxiety, depression, or insomnia symptoms of adult populations from general population, general students, medical students, frontline HCWs, or general HCWs during COVID-19 pandemic in Eastern Europe.
We focused on depression, anxiety, and insomnia because they are the most reported mental health symptoms. Based on the EuroVoc definition of Eastern Europe, we included the following countries: Albania, Armenia, Azerbaijan, Belarus, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Georgia, Hungary, Kosovo, Moldova, Montenegro, North Macedonia, Poland, Romania, Russia, Serbia, Slovakia, Slovenia, Turkey and Ukraine.
We included only the empirical studies published in English using validated measurement tools or scales of anxiety, depression, and insomnia. We excluded non-primary studies including reviews, meta-analyses, qualitative studies, case studies, interventional studies, interviews, or news reports. We also excluded articles that focused on specific adult populations such as COVID-19 patients, inpatients, adults under quarantine, pregnant women, children, or adolescents, and studies that used non-validated mental health instruments or non-validated cut-off scores.
A researcher (WX) emailed the authors of articles that missed essential information in several instances: 1) if the article met our inclusion criteria but did not report the prevalence; 2) if the article surveyed both targeted and excluded populations; 3) if the article reported the overall prevalence without specifying whether the cut-off was above moderate or above mild; or 4) if the article was missing essential coding information such as data collection time, female proportion rate, or respondent rate.
2.3. Data screening
A researcher (JC) imported article information from the above databases into Endnotes to remove duplicates and then imported into Rayyan for screening. Two coders (BZC & AD) independently reviewed titles and abstracts of the empirical studies retrieved based on the above inclusion and exclusion criteria through initial screening criteria. Conflicts of eligibility were referred to a third coder (RKD). The articles included after the title and abstract screening underwent a full-text evaluation.
2.4. Data extraction
A comprehensive screening protocol was developed. The following variables were collected from each study: author, title, country, starting and ending dates of data collection, study design, population, sample size, respondent rate, female proportion rate, age range and mean, outcome, outcome level, instruments, cut-off scores, and prevalence. If possible, we coded the prevalence at the severity of mild above, moderate above, and severe. For those studies that reported the mild, moderate, and severe prevalence, we converted them into mild above, moderate above, and severe prevalence. For these studies that only reported the overall prevalence, we specified their severity if their cut-off points were reported.
The protocol was followed by two independent coders in pairs (WX & AY, BZC & AD, RZC & SM). The corresponding authors of empirical studies without prevalence data or missing essential data were contacted by a designated researcher (WX). The reason(s) for emailing authors and excluding studies were recorded. After both coders in each pair had independently coded their studies, they then cross-checked their information and discussed possible differences. If disagreements remained, a third coder (SM) settled disagreements after independently coding the study.
2.5. Bias risk
Study quality was analysed using a modified version of the Mixed Methods Appraisal Tool (MMAT) to assess risk of bias following published meta-analysis on mental health under COVID (e.g. de Pablo et al., Citation2020; Usher, Jackson, Durkin, Gyamfi, & Bhullar, Citation2020). de Pablo et al. (Citation2020) specifically mentioned that ‘MMAT is considered the best and most comprehensive tool available for appraising multi-method studies (Behghadami et al., Citation2019)’. Throughout the data collection process, two coders used the same protocol as in those meta-analysis studies independently determine the appropriateness of measurement tools, the risk of non-response bias, and the sample representativeness of each empirical study (Hong et al., Citation2018). A quality score ranging from 0 to 7 was assigned to each empirical study. A MMAT quality score higher than 6 indicated low bias risk, a score between 5 and 6 indicated medium risk, and a score below 5 indicated high bias risk (Hong et al., Citation2018). The MMAT scores were compared using a standardized cross-check protocol. A final check of inter-coder consistency was performed by a third independent coder (RKD). A sensitivity analysis was conducted to assess the risk of bias of the study.
2.6. Methods of analysis
Stata 16.1 was used to pool rates of anxiety and depression, using metaprop (Nyaga, Arbyn, & Aerts, Citation2014). We used the random-effects model to calculate the pooled estimates of outcome prevalence between populations based on the assumption that these studies are randomly selected from their targeted populations in Eastern Europe to generalize our results to the comparable studies in the region. We computed prediction intervals to show the range of the effect sizes across studies (Borenstein, Higgins, Hedges, & Rothstein, Citation2017). The I2 statistic was used to calculate variance difference from effect sizes in order to quantify heterogeneity rather than sampling error (Higgins et al., Citation2019). Subgroup analyses were performed on population groups (i.e. general population, students, general HCWs, and frontline HCWs), mental health disorder (i.e. anxiety, depression, and insomnia), outcome severity (i.e. mild above, moderate above, severe). We also performed subgroup analysis on EU (European Union) membership, i.e. EU countries vs. Non-EU countries. Lastly, we did subgroup analysis by regions, i.e. the greater Balkan region known more formally as Southeastern Europe and the rest. The greater Balkan region of southeastern Europe includes Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Kosovo, Montenegro, North Macedonia, Romania, Serbia, Slovenia, and Turkey. The remaining Eastern European countries, including Czech Republic, Poland, Russia, and Ukraine, were categorized as Non-Southeastern Europe.
3. Results
3.1. Screening results
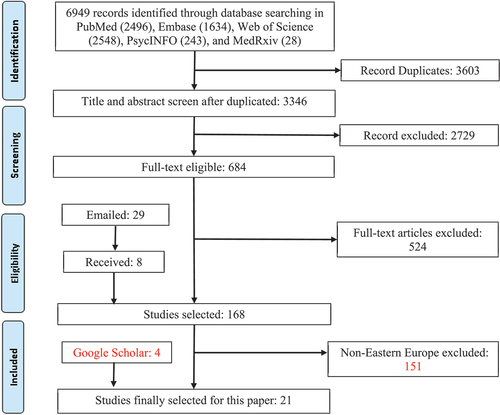
A PRISMA flowchart () illustrates the systematic review process, which is part of a large research effort to examine the prevalence of mental health symptoms across regions and countries during the COVID-19 pandemic. A total of 6949 studies were identified in the search. Of these studies, 3603 were duplicates and were excluded. The initial screening of 3346 studies produced 684 studies eligible for further full-text evaluation. Through detailed full-text evaluation, 524 studies were excluded. Two rounds of emails were sent to the authors of studies with missing data for the meta-analyses. Prevalence data from the email responses was added to 8 of the 29 empirical studies, bringing the total number of empirical studies for the meta-analyses to 168. Of the 168 studies, 23 empirical studies covered Eastern Europe (Antonijevic et al., Citation2020; Bachilo, Barylnik, Shuldyakov, Efremov, & Novikov, Citation2020; Cypryańska, Nezlek, & Capraro, Citation2020; Dzhambov et al., Citation2020; Galić, Mustapić, Šimunić, Sić, & Cipolletta, Citation2020; Gallopeni et al., Citation2020; Karpenko et al., Citation2020; Kowalski, Marchlewska, Molenda, Górska, & Gawęda, Citation2020; Margetić, Peraica, Stojanović, & Ivanec, Citation2021; Markovic et al., Citation2020; Mechili et al., Citation2020; Mosolova, Chung, Sosin, & Mosolov, Citation2020; Nekliudov et al., Citation2020; Rogowska, Kuśnierz, & Bokszczanin, Citation2020a; Rogowska et al., Citation2020b; Salopek-Ziha et al., Citation2020; Secosan, Virga, Crainiceanu, & Bratu, Citation2020; Sigorski et al., Citation2020; Sljivo, Kacamakovic, Quraishi, & Dzubur Kulenovic, Citation2020; Stojanov et al., Citation2020; Vujčić et al., Citation2021; Wańkowicz, Szylińska, & Rotter, Citation2020; Winkler et al., Citation2020). As there were only two studies that examined the prevalence of insomnia (Secosan et al., Citation2020; Wańkowicz et al., Citation2020), insomnia was excluded from further analysis. The meta-analysis included the remaining 21 studies with 26 unique samples that reported 87 prevalence rates. Some empirical studies include multiple independent samples. For example, Stojanov et al. surveyed frontline HCWs and general HCWs (Stojanov et al., Citation2020).
3.2. Characteristics of included studies
shows the characteristics of the 21 studies. The countries that had the most studies are Poland and Serbia (19.1%, n = 4), followed by Croatia and Russia (14.39%, n = 3), Albania (9.5%, n = 2), and one study each from Bosnia and Herzegovina, Bulgaria, Czech Republic, Kosovo, and Ukraine. Samples were distributed between populations as follows: general population (42.3%, n = 11), general HCWs (26.9%, n = 7), general (i.e. non-medical) students (15.4%, n = 4), and frontline HCWs (15.4%, n = 4). The prevalence of mental health symptoms was found for the following categories: mild above (34.5%, n = 30), moderate above (37.9%, n = 33), severe above (19.6%, n = 17), and overall (8.1%, n = 7). Most of the studies (95.7%, n = 20) used cross-sectional designs. The median percentage of female respondents was 68.8% with a range of 0% to 100%. The response rates ranged from 0.7% to 98.5% with a median of 56.7%. The sample size ranged from 83 to 3306 with a median of 843 respondents. Please see Appendix B for studies characteristics.
Table 1. Characteristics of the studies on mental health in Eastern Europe during the COVID-19 pandemic
3.3. Mental health outcome prevalence
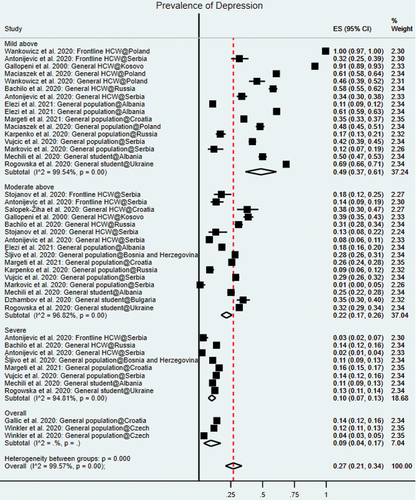
A random-effects meta-analysis model showed the pooled prevalence of depression of 18 empirical studies (Antonijevic et al., Citation2020; Bachilo et al., Citation2020; Dzhambov et al., Citation2020; Galić et al., Citation2020; Gallopeni et al., Citation2020; Karpenko et al., Citation2020; Kowalski et al., Citation2020; Margetić et al., Citation2021; Markovic et al., Citation2020; Mechili et al., Citation2020; Mosolova et al., Citation2020; Nekliudov et al., Citation2020; Rogowska et al., Citation2020b; Salopek-Ziha et al., Citation2020; Secosan et al., Citation2020; Sigorski et al., Citation2020; Sljivo et al., Citation2020; Stojanov et al., Citation2020; Vujčić et al., Citation2021; Wańkowicz et al., Citation2020; Winkler et al., Citation2020) (including 23 samples and 43 prevalence rates) was 27% (95% CI: 21–34%, I2: 99.6%) (). This pooled prevalence represents a total of 22,195 respondents. This finding suggests that on average about 27% of the adults in Eastern Europe during COVID-19 had depression symptoms. The prediction interval of anxiety prevalence across studies is 1% to 93% based on a normal distribution, hence we expect that the prevalence of depression symptoms in any comparable studies will fall in this range. Several depression instruments were used: most frequently the Depression, Anxiety, and Stress Scale (DASS-21) (52.2%), followed by Patient Health Questionnaire (PHQ)-9 (30.4%), Beck Depression Inventory (BDI) (4.4%), Hospital Anxiety and Depression Scale (HADS) (4.4%), and Brief Symptom Inventory (BSI) (4.4%). The pooled prevalence of anxiety was 30% (95% CI: 24–37%, I2: 99.6%) (). Data from 18 studies (Antonijevic et al., Citation2020; Bachilo et al., Citation2020; Cypryańska et al., Citation2020; Dzhambov et al., Citation2020; Galić et al., Citation2020; Gallopeni et al., Citation2020; Karpenko et al., Citation2020; Kowalski et al., Citation2020; Margetić et al., Citation2021; Markovic et al., Citation2020; Mosolova et al., Citation2020; Nekliudov et al., Citation2020; Rogowska et al., Citation2020a, Citation2020b; Salopek-Ziha et al., Citation2020; Secosan et al., Citation2020; Sigorski et al., Citation2020; Stojanov et al., Citation2020; Vujčić et al., Citation2021; Wańkowicz et al., Citation2020; Winkler et al., Citation2020), including 22 samples and 44 prevalence rates), reported anxiety prevalence out of a total of 21,120 participants. This finding suggests that on average about 30% of the adults in Eastern Europe during COVID-19 had anxiety symptoms. The prediction interval of anxiety prevalence among studies vary from 1% to 87%. The DASS-21 was used most frequently (56.5%), followed by Generalized Anxiety Symptoms 7-items scale (GAD-7) (30.4%), HADS (4.4%), and BSI (4.4%).
Table 2. The pooled prevalence rates of mental health symptoms by subgroups of population, outcome, severity, region, and quality
The aggregated prevalence of either anxiety or depression in frontline HCWs was 41% (95% CI: 23–60%) and 33% in general HCWs (95% CI: 22–45%) (, )
Figure 2. (a). Forest plot of anxiety prevalence. (b). Forest plot of depression prevalence.
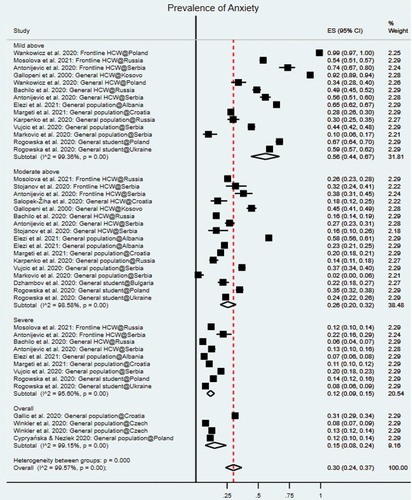
Subgroup analysis revealed that while depression prevalence was 34% for both general HCWs (95% CI: 18–51%) and frontline HCWs (95% CI: 2–79%), anxiety prevalence was significantly higher among frontline HCWs (46%; 95% CI: 25–67%) than among general HCWs (33%; 95% CI: 16–51%) (). The prevalence of anxiety and depression in student populations was 31% and 32%, respectively. In the general population, prevalence of depression and anxiety was 20% and 22%, respectively (). European Union (EU) countries in Eastern Europe had a prevalence of 34% (95% CI: 27–42%), which is a bit higher than that Eastern European countries without EU memberships s (28%; 95% CI: 22–35%). Southeastern Europe countries (the greater Balkan region) had pooled anxiety and depression prevalence rates of 31% (95% CI: 23–40%) and 35% (95% CI: 21–51%), respectively (). In non-Southeastern Europe countries, prevalence of anxiety and depression was 29% (95% CI: 20–40%) and 55% (95% CI: 46–65%) ().
Table 3. Subgroup analyses of anxiety and depression prevalence
3.4. Article quality
We used a modified version of the Mixed Methods Appraisal Tool (MMAT) (Behghadami et al., Citation2019; de Pablo et al., Citation2020; Usher et al., Citation2020) and found that of the 21 studies, 3 studies (14.29%) were categorized as high quality and 18 studies (85.71%) categorized as medium quality (). The subgroup analysis suggests the studies with high quality reported lower prevalence of clinically significant symptoms of mental health symptoms in Eastern Europe ().
3.5. Sensitivity analysis
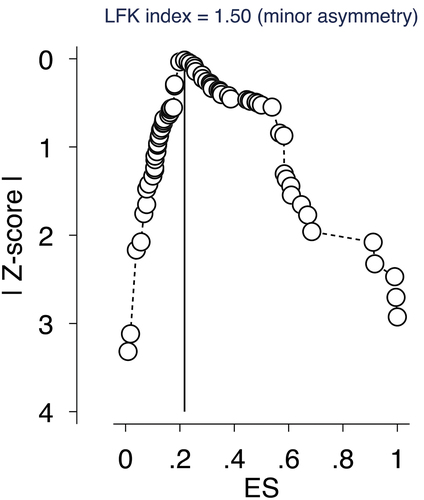
A sensitivity analysis was conducted using a DOI plot and Luis Furuya-Kanamori (LFK) index to detect any publication bias in the meta-analysis. Conventional funnel plots have been previously determined to be inaccurate for meta-analyses of pooled proportion studies (34). Additionally, DOI plots in combination with LFK indices use higher power and sensitivity for bias detection than both funnel plots and Egger’s regression (Furuya-Kanamori, Barendregt, & Doi, Citation2018). A DOI plot, in addition to a LFK index, can better graphically represent publication bias. An asymmetrical triangle indicates potential publication bias whereas a symmetrical triangle suggests no publication bias (Furuya-Kanamori et al., Citation2018). A LFK index score within ±1 indicates ‘no asymmetry’. When the LFK index score exceeds ±1 but is within ±2 it indicates ‘minor asymmetry’ and when the score exceeds ±2 ‘major asymmetry’ is indicated. The studies on Eastern Europe, as shown in , have ‘minor asymmetry’ based on an index score of 1.50 and therefore minor publication bias is likely. The impact of publication status and sample size was tested and no significant influence was found.
4. Discussion
This meta-analysis on 21 empirical studies of 25,246 adults provides the first evidence on the pooled prevalence rates of mental health symptoms in Eastern Europe during the COVID-19 pandemic. The pooled prevalence rates of anxiety and depression in Eastern Europe were 30% and 27% (). Subgroup analyses revealed several key findings: frontline HCWs indicated higher rates of mental disorder symptoms, especially anxiety (46%, 95% CI: 25–67%), a high percentage of adults suffered from mild or greater severity of anxiety (56%, 95% CI: 44–67%), a higher rate of depression was found in non-Southeastern Europe (55%, 95% CI: 46–65%), and the choice of instruments represents a significant source of heterogeneity on the pooled prevalence of anxiety and depression symptoms.
4.1. Comparing with prior meta-analyses
First, we discuss the pooled prevalence rates of this meta-analysis by comparing them with prior meta-analytical findings during the COVID-19 pandemic in other regions as benchmarks. Our pooled prevalence of depression of 27% in Eastern Europe was within the range of similar meta-analyses results in China. Prior meta-analyses of depression in China indicated heterogeneous pooled prevalence ranging from 24% to 32% in adult populations (Chen et al., Citation2021a; Luo, Guo, Yu, Jiang, & Wang, Citation2020; Ren et al., Citation2020; Wu et al., Citation2021). Our pooled prevalence of depression in Eastern Europe was significantly lower than prevalence in Southeast Asia (34%, p < 0.001) (Pappa et al., Citation2021), Spain (35%, p < 0.001) (Chen et al., Citation2021) and Africa (45%, p < 0.001) (Chen et al., Citation2021) and prevalence rates in a cross-continent meta-analysis including empirical studies from China, India, Iran, Iraq, Italy, Japan, Nepal, Nigeria, Spain, and the UK (34%, p < 0.001) (Salari et al., Citation2020).
The pooled prevalence of anxiety of 30% in this Eastern Europe meta-analysis was significantly higher than the pooled rates reported in Spain (20%, p < 0.001) (Chen et al., Citation2021) and was similar to those among the general population in China (30%, p = 0.653) (Wu et al., Citation2021). However, prevalence of anxiety symptoms was significantly lower in Eastern Europe compared to prevalence in Africa (37%, p < 0.001) (40) (Chen et al., Citation2021) and Southeast Asia (41%, p < 0.001) (Pappa et al., Citation2021), and to prevalence in a cross-continent meta-analysis (i.e. China, India, Iran, Iraq, Italy, Japan, Nepal, Nigeria, Spain and the UK) (32%, p < 0.001) (Salari et al., Citation2020).
4.2. Subgroup analyses
Our results show that frontline HCWs suffered from anxiety symptoms at a significantly higher rate compared to other populations in Eastern Europe. Overall, frontline HCWs had the highest prevalence of mental health symptoms including anxiety (46%) and depression (34%), followed by general HCWs (anxiety: 33%, depression: 34%) and subsequently students (anxiety: 31%, depression: 32%) and the general population (anxiety: 22%, depression: 20%). This finding indicates heterogeneity of mental health symptoms among distinct populations in Eastern Europe. The anxiety and depression symptoms of healthcare workers in Eastern Europe are higher than those of healthcare workers (24.9% and 24.8%, respectively) reported by a recent meta-analysis (Sahebi et al., Citation2021), which included seven studies from Brazil, China, India, and UK. Comparatively, a meta-analysis in China also found a lower pooled prevalence of anxiety (27%) and depression (20%) among general HCWs compared to prevalence of anxiety (40%) and depression (24%) in frontline HCWs (Batra, Singh, Sharma, Batra, & Schvaneveldt, Citation2020). Not withstanding this finding, it needs to be emphasized that there are heterogeneous results on the prevalence of psychopathology reported in HCWs in China (Lin et al., Citation2020).
The prevalence of mental health symptoms during the COVID-19 pandemic is not homogeneous across regions. European Union (EU) countries in Eastern Europe had a prevalence of 34%, which a bit higher than that Eastern European countries without EU memberships at 28%. The greater Balkan region of Southeastern Europe and non-Southeastern Europe exhibited a similar rate of anxiety (31% vs. 29%) but a very different rate of depression symptoms (35% vs. 55%). Such mental health symptom differences provide important evidence for future research directions to offer insight into these significant differences. It is possible that the economic, cultural, social, and political factors of individual countries and broader regions as well as heterogeneous COVID-19 policies, such as the length and stringency of shutdowns, lockdowns, and quarantine, may influence mental health symptoms such as anxiety and depression differentially (Hale et al., Citation2021). We also note that the pooled prevalence rates of anxiety and depression are significantly influenced by the choice of the instruments in the primary studies. For example, anxiety prevalence measured by DASS-21 was 25% (95% CI: 16–34%) and 43% using HADS (CI: 17–71%), suggesting future research should pay attention to the choice of the instruments.
4.3. Implications
The systematic review reveals that eleven Eastern European countries had not been subject to a single study on the topic. Future studies should focus on countries without empirical data including Armenia, Azerbaijan, Belarus, Georgia, Hungary, Moldova, Montenegro, North Macedonia, Romania, Slovakia, and Slovenia. For practical purposes, healthcare organizations in locations without country-level evidence on mental health may use our evidence at the regional level as approximate evidence. These findings also emphasize the importance of further empirical research and subsequent meta-analyses on Eastern Europe countries in order to better prioritize resource allocation.
The understanding of mental disorder prevalence within specific regions can help to create targeted healthcare policy by healthcare organizations such as WHO. The responses to the COVID-19 pandemic have been remarkably homogeneous across governments (Hale et al., Citation2021). Available WHO guidance has focused on preventing local progression of infectious diseases rather than achieving regional herd behaviour (Hale et al., Citation2021). Eastern European mental healthcare is dependent on large psychiatric institutions with an emphasis on in-patient psychiatry (Krupchanka & Winkler, Citation2016), which may not be effectively addressing widespread anxiety and depression symptoms. Mental health research has historically been overlooked in Eastern Europe (Krupchanka & Winkler, Citation2016), where mental health epidemiology is still regarded with intense stigma and direct evidence on the topic remains scarce (Franic & Dodig-Curkovic, Citation2020). Existing stigma, along with a lack of evidence-based community-wide mental health services, may be contributing to high prevalence of mental health disorders. Furthermore, recent changes in healthcare systems and lack of per capita funding and access (Grabowski et al., Citation2021) for community mental health resources may contribute to the unique situation in Eastern Europe mental health, which still lacks evidence-based mental health practices (Krupchanka & Winkler, Citation2016). With this backdrop, the meta-analysis provides quantitative evidence revealing a high prevalence of mental health symptoms in Eastern Europe serve as the basis for inform more targeted healthcare practices, such as evidence-based occupational guidelines which identify and focus on vulnerable populations during acute crises (Holmes et al., Citation2020).
4.4. Study limitations
First, as we only included studies in English, there is an expected language bias. Second, our meta-analysis is limited by the limitations of the empirical studies. Due to the nature of lockdowns and social isolation during the pandemic, many of the studies used convenience samples, reducing the accurate representation of respective populations. Varying tools of data collection used different cut-off scores. In future research, mental health evaluation of a random sample would yield representative data. Additionally, the meta-analysis is limited by the populations and mental health symptoms represented in the available empirical studies. Only two studies covered insomnia, and therefore insomnia was not represented in the meta-analysis. Further studies focused on insomnia prevalence would contribute to a pooled prevalence of insomnia and improve supporting data for evidence-based medical interventions.
4.5. Conclusion
Understanding the prevalence of mental health symptoms during the COVID-19 pandemic represents the first step (Babicki et al., Citation2021; Lateef et al., Citation2021) to enable evidence-based medical practices by assessing the mental health situation during the COVID-19 pandemic. We hope the meta-analysis in Eastern Europe can inform mental health practices as well as encourage future research on mental health during the ongoing COVID-19 pandemic.
Author contributions
All authors declare they meet ICMJE conditions for authorship. SXZ and JC designed the study. SZX, RKD and JC designed the coding guide and method and performed the initial literature search. SXZ, SM, and JC performed statistical analysis and led the drafting and editing of the article. RSM edited the article. SM, WX, AY, BZC, AD, RKD, RZC and XW collected the data. All authors approved the final version of the article.
Patient and public involvement
No patient or public was involved in this systematic review and meta-analysis.
Transparency declaration
The corresponding author affirms this manuscript is an honest, accurate, and transparent account of the study being reported. No important aspects of the study have been omitted and any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Disclosure statement
RSM has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation; speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Novo Nordisk, Kris, Sanofi, Eisai,Intra-Cellular, NewBridge Pharmaceuticals, AbbVie. Dr. Roger McIntyre is a CEO of Braxia Scientific Corp.
Data availability statement
The data that support the findings of this study are available through https://www.dropbox.com/scl/fi/gmgyhf1wkpsbmbguqwosu/South-Eastern-Data.xlsx?dl=0&rlkey=fdxubsksmjqmevjuqs4kdup69
Additional information
Funding
References
- Antonijevic, J., Binic, I., Zikic, O., Manojlovic, S., Tosic‐Golubovic, S., & Popovic, N. (2020). Mental health of medical personnel during the COVID‐19 pandemic. Brain and Behavior, 10(12). doi:10.1002/brb3.1881
- Babicki, M., Szewczykowska, I., & Mastalerz-Migas, A. (2021). The mental well-being of health care workers during the peak of the COVID-19 pandemic—A nationwide study in Poland. International Journal of Environmental Research and Public Health, 18(11), 6101. doi:10.3390/ijerph18116101
- Bachilo, E. V., Barylnik, J. B., Shuldyakov, A. A., Efremov, A. A., & Novikov, D. E. (2020). Mental health of medical workers during the COVID-19 pandemic in Russia: Results of a cross-sectional study: Psychiatry and clinical psychology.
- Batra, K., Singh, T. P., Sharma, M., Batra, R., & Schvaneveldt, N. (2020). Investigating the psychological impact of COVID-19 among healthcare workers: A meta-analysis. International Journal of Environmental Research and Public Health, 17(23), 9096. doi:10.3390/ijerph17239096
- Behghadami, M. A., Janati, A., Arab-Zozani, M., Arab-Zozani, M., Arab-Zozani, M., & Arab-Zozani, M. (2019). Assessing preparedness of non-hospital health centers to provide primary emergency care: A systematic review. Bulletin of Emergency and Trauma, 7(3), 201–14. doi:10.29252/beat-070301
- Borenstein, M., Higgins, J. P. T., Hedges, L. V., & Rothstein, H. R. (2017). Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Research Synthesis Methods, 8(1), 5–18. doi:10.1002/jrsm.1230
- Chen, J., Farah, N., Dong, R. K., Chen, R. Z., Xu, W., Yin, A., Chen, B. Z., Delios, A., Miller, S., Wan, X., Zhang, S. X. (2021). The mental health under the COVID-19 crisis in Africa: A systematic review and meta-analysis. medRxiv. doi:10.1101/2021.04.19.21255755
- Chen, J., Zhang, S. X., Wang, Y., Jahanshahi, A. A., Dinanie, M. M., Madavanif, A. N., Nawaserg, K. (in press). The relationship between age and mental health among adults in Iran during the COVID-19 pandemic. International Journal of Mental Health and Addiction.
- Chen, X., Chen, J., Zhang, M., et al. (2021a). One year of evidence on mental health in China in the COVID-19 crisis - A systematic review and meta-analysis. Medrxiv. doi:10.1101/2021.02.01.21250929
- Chen, X., Chen, J., Zhang, M., Chen, R. Z., Dong, R. K., Dong, Z., Ye, Y., Tong, L., Chen, B. Z., Zhao, R., et al. (2021). A systematic review and meta-analysis on mental illness symptoms in Spain in the COVID-19 crisis. Medrxiv. doi:10.1101/2021.04.11.21255274
- Cypryańska, M., Nezlek, J. B., & Capraro, V. (2020). Anxiety as a mediator of relationships between perceptions of the threat of COVID-19 and coping behaviors during the onset of the pandemic in Poland. PLOS ONE, 15(10), e0241464. doi:10.1371/journal.pone.0241464
- de Pablo, G. S., Vaquerizo-Serrano, J., Catalan, A., Arango, C., Moreno, C., Ferre, F., … Fusar-Poli, P. (2020). Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. Journal of Affective Disorders, 275, 48–57. doi:10.1016/j.jad.2020.06.022
- Ding, K., Yang, J., Chin, M.-K., Sullivan, L., Demirhan, G., Violant-Holz, V., … Smith, G. A. (2021). Mental health among adults during the COVID-19 pandemic lockdown: A cross-sectional multi-country comparison. International Journal of Environmental Research and Public Health, 18(5), 2686. doi:10.3390/ijerph18052686
- Dzhambov, A. M., Lercher, P., Browning, M. H. E. M., Stoyanov, D., Petrova, N., Novakov, S., Dimitrova, D. D. (2020). Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environmental Research, 110420. doi:10.1016/j.envres.2020.110420
- Elezi, F., Tafani, G., Sotiri, E., Agaj, H., & Kola, K. (2020). Assessment of anxiety and depression symptoms in the Albanian general population during the outbreak of COVID-19 pandemic. Indian Journal Psychiatry, 62, 470–475.
- Franic, T., & Dodig-Curkovic, K. (2020). Covid-19, child and adolescent mental health - Croatian (in)experience. Irish Journal of Psychological Medicine, 37(3), 214–217. doi:10.1017/ipm.2020.55
- Furuya-Kanamori, L., Barendregt, J. J., & Doi, S. (2018). A new improved graphical and quantitative method for detecting bias in meta-analysis. International Journal of Evidence-Based Healthcare, 16(4), 195–203. doi:10.1097/XEB.0000000000000141
- Galić, M., Mustapić, L., Šimunić, A., Sić, L., & Cipolletta, S. (2020). COVID-19 related knowledge and mental health: Case of Croatia. Frontiers in Psychology, 11, 567368. doi:10.3389/fpsyg.2020.567368
- Gallic, M. M., L.: L, A., Sic, L, and Cipolletta, S. (2020). COVID-19 Related Knowledge and Mental Health: Case of Croatia. Frontiers in Psychology, 11, 567368. https://doi.org/10.3389/fpsyg.2020.567368
- Gallopeni, F., Bajraktari, I., Selmani, E., Tahirbegolli, I. A., Sahiti, G., Muastafa, A., Bojaj, G., Muharremi, V. B., & Tahirbegolli, B. (2020). Anxiety and depressive symptoms among healthcare professionals during the Covid-19 pandemic in Kosovo: A cross sectional study. Journal of Psychosomatic Research, 137, 110212.
- Gallopeni, F., Bajraktari, I., Selmani, E., Tahirbegolli, I. A., Sahiti, G., Muastafa, A., … Tahirbegolli, B. (2020). Anxiety and depressive symptoms among healthcare professionals during the Covid-19 pandemic in Kosovo: A cross sectional study. Journal of Psychosomatic Research, 137, 110212. doi:10.1016/j.jpsychores.2020.110212
- Grabowski, J., Witkowska, N., & Bidzan, L. (2021). Letter to the editor: Excess all-cause mortality during second wave of COVID-19 – The Polish perspective. Eurosurveillance, 26(7). doi:10.2807/1560-7917.ES.2021.26.7.2100117
- Hale, T., Angrist, N., Goldszmidt, R., Kira, B., Petherick, A., Phillips, T., … Tatlow, H. (2021). A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nature Human Behaviour, 5(4), 529–538. doi:10.1038/s41562-021-01079-8
- Higgins, J. P., Thomas, J., Chandler, J., Cumpston, M., Tianjing Li, M. J., Page, V. A. W. (2019). Cochrane handbook for systematic reviews of interventions. John Wiley & Sons.
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., & Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. doi:10.1016/S2215-0366(20)30168-1
- Hong, Q. N., Pluye, P., Fàbregues, S., Boardman, F., Cargo, M., Dagenais, P., … Pluye, P. (2018). The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information, 34(4), 285–291. doi:10.3233/EFI-180221
- Hossain, M. M., Rahman, M., Trisha, N. F., Tasnim, S., Nuzhath, T., Hasan, N. T., … Ma, P. (2021). Prevalence of anxiety and depression in South Asia during COVID-19: A systematic review and meta-analysis. Heliyon, 7(4), e06677. doi:10.1016/j.heliyon.2021.e06677
- Karpenko, O. A., Syunyakov, T. S., Kulygina, M. A., Pavlichenko, A. V., Chetkina, A. S., & Andrushchenko, A. V. (2020). Impact of COVID-19 pandemic on anxiety, depression and distress – Online survey results amid the pandemic in Russia. Consortium Psychiatricum, 1(1), 8–20. doi:10.17650/2712-7672-2020-1-1-8-20
- Kołodziejczyk, A., Misiak, B., Szcześniak, D., Maciaszek, J., Ciułkowicz, M., Łuc, D., … Rymaszewska, J. (2021). Coping styles, mental health, and the COVID-19 quarantine: A nationwide survey in Poland. Frontiers in Psychiatry, 12, 106. doi:10.3389/fpsyt.2021.625355
- Kowalski, J., Marchlewska, M., Molenda, Z., Górska, P., & Gawęda, Ł. (2020). Adherence to safety and self-isolation guidelines, conspiracy and paranoia-like beliefs during COVID-19 pandemic in Poland - associations and moderators. Psychiatry Research, 294, 113540. doi:10.1016/j.psychres.2020.113540
- Krupchanka, D., & Winkler, P. (2016). State of mental healthcare systems in Eastern Europe: Do we really understand what is going on? BJPsych. International, 13(4), 96–99. doi:10.1192/s2056474000001446
- Lateef, T., Chen, J., Tahir, M., Lateef, T. A., Chen, B. Z., Li, J., & Zhang, S. X. (2021). Typhoon Eye effect versus Ripple effect: The role of family size on mental health during the COVID-19 pandemic in Pakistan. Globalization and Health, 17(1). doi:10.1186/s12992-021-00685-5
- Lin, K., Yang, B. X., Luo, D., Liu, Q., Ma, S., Huang, R., & McIntyre, R. S. (2020). The mental health effects of COVID-19 on health care providers in China. The American Journal of Psychiatry, 177(7), 635–636. doi:10.1176/appi.ajp.2020.20040374
- Luo, M., Guo, L., Yu, M., Jiang, W., & Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Research, 291(113190), 113190. doi:10.1016/j.psychres.2020.113190
- Maciaszek, J., Ciulkowicz, M., Misiak, B., Szczesniak, D., Luc, D., Wieczorek, T., … Rymaszewska, J. (2020). Mental health of medical and non-medical professionals during the peak of the COVID-19 pandemic: A cross-sectional nationwide study. Journal of Clinical Medicine, 9(8), 2527. doi:10.3390/jcm9082527
- Margetić, B., Peraica, T., Stojanović, K., & Ivanec, D. (2021). Predictors of emotional distress during the COVID-19 pandemic; A Croatian study. Personality and Individual Differences, 175, 110691. doi:10.1016/j.paid.2021.110691
- Markovic, I., Nikolovski, S., Milojevic, S., Zivkovic, D., Knezevic, S., Mitrovic, A., … Djurdjevic, D. (2020). Public trust and media influence on anxiety and depression levels among skilled workers during the COVID-19 outbreak in Serbia. Vojnosanitetski Pregled, 77(11), 1201–1209. doi:10.2298/VSP200713108M
- Mechili, E. A., Saliaj, A., Kamberi, F., Girvalaki, C., Peto, E., Patelarou, A. E., Bucaj, J., Patelarou, E. (2020). Is the mental health of young students and their family members affected during the quarantine period? Evidence from the COVID-19 pandemic in Albania. Journal of Psychiatric and Mental Health Nursing. doi:10.1111/jpm.12672
- Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1. doi:10.1186/2046-4053-4-1
- Moroń, M., & Biolik-Moroń, M. (2021). Trait emotional intelligence and emotional experiences during the COVID-19 pandemic outbreak in Poland: A daily diary study. Personality and Individual Differences, 168, 110348. doi:10.1016/j.paid.2020.110348
- Mosolova, E., Chung, S., Sosin, D., & Mosolov, S. (2020). Stress and anxiety among healthcare workers associated with COVID-19 pandemic in Russia. Psychiatria Danubina, 32(3–4), 549–556. doi:10.24869/psyd.2020.549
- Nekliudov, N. A., Blyuss, O., Cheung, K. Y., Petrou, L., Genuneit, J., Sushentsev, N., … Munblit, D. (2020). Excessive media consumption about COVID-19 is associated with increased state anxiety: Outcomes of a large online survey in Russia. Journal of Medical Internet Research, 22(9), e20955. doi:10.2196/20955
- Nyaga, V. N., Arbyn, M., & Aerts, M. (2014). Metaprop: A Stata command to perform meta-analysis of binomial data. Archives of Public Health, 72(1), 39. doi:10.1186/2049-3258-72-39
- Pappa, S., Chen, J., Barnet, J., Zhang, A., Dong, R. K., Xu, W., Yin, A., Chen, B. Z., Delios, A., Chen, R. Z., et al. (2021). A systematic review and meta-analysis of the mental health impact of the Covid-19 pandemic in Southeast Asia. doi:10.1101/2021.06.03.21258001
- Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88, 901–907. doi:10.1016/j.bbi.2020.05.026
- Ren, X., Huang, W., Pan, H., Huang, T., Wang, X., & Ma, Y. (2020). Mental health during the Covid-19 outbreak in China: A meta-analysis. The Psychiatric Quarterly, 91(4), 1033–1045. doi:10.1007/s11126-020-09796-5
- Rogowska, A. M., Kuśnierz, C., & Bokszczanin, A. (2020a). Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in Polish sample of university students. Psychology Research and Behavior Management, 13, 797–811. doi:10.2147/PRBM.S266511
- Rogowska, A. M., Pavlova, I., Kuśnierz, C., Ochnik, D., Bodnar, I., & Petrytsa, P. (2020b). Does physical activity matter for the mental health of university students during the COVID-19 pandemic? Journal of Clinical Medicine, 9(11), 3494. doi:10.3390/jcm9113494
- Sahebi, A. N. B., Nejati-Zarnaqi, B., Moayedi, S., Yousefi, K., Torres, M., & Golitaleb, M. (2021). The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Progress in Neuro-psychopharmacology & Biological Psychiatry, 107, 110247. doi:10.1016/j.pnpbp.2021.110247
- Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., … Khaledi-Paveh, B. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health, 16(1), 57. doi:10.1186/s12992-020-00589-w
- Salopek-Ziha, D., Hlavati, M., Gvozdanovic, Z., Gasic, M., Placento, H., Jakic, H., … Simic, H. (2020). Differences in distress and coping with the Covid-19 stressor in nurses and physicians. Psychiatria Danubina, 32(2), 287–293. doi:10.24869/psyd.2020.287
- Secosan, I., Virga, D., Crainiceanu, Z. P., & Bratu, T. (2020). The mediating role of insomnia and exhaustion in the relationship between secondary traumatic stress and mental health complaints among frontline medical staff during the COVID-19 pandemic. Behavioral Sciences, 10(11), 164. doi:10.3390/bs10110164
- Sigorski, D., Sobczuk, P., Osmola, M., Kuć, K., Walerzak, A., Wilk, M., … Bodnar, L. (2020). Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open, 5(5), e000970. doi:10.1136/esmoopen-2020-000970
- Sljivo, A., Kacamakovic, M., Quraishi, I., & Dzubur Kulenovic, A. (2020). Fear and depression among residents of Bosnia And Herzegovina during COVID-19 outbreak - internet survey. Psychiatria Danubina, 32(2), 266–272. doi:10.24869/psyd.2020.266
- Stephen, X., Zhang, F. A. M., & Gao, R. (in press). A second wave? What do people mean by COVID waves? – A working definition of epidemic waves. Risk Management and Healthcare Policy.
- Stojanov, J., Malobabic, M., Stanojevic, G., Stevic, M., Milosevic, V., Stojanov, A. (2020). Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. International Journal of Social Psychiatry, 002076402094280. doi:10.1177/0020764020942800
- Usher, K., Jackson, D., Durkin, J., Gyamfi, N., & Bhullar, N. (2020). Pandemic‐related behaviours and psychological outcomes; A rapid literature review to explain COVID‐19 behaviours. International Journal of Mental Health Nursing, 29(6), 1018–1034. doi:10.1111/inm.12790
- Villani, L., Pastorino, R., Ricciardi, W., Ioannidis, J., & Boccia, S. (2021). Inverse correlates of COVID-19 mortality across European countries during the first versus subsequent waves. BMJ Global Health, 6(8), e006422. doi:10.1136/bmjgh-2021-006422
- Vujčić, I., Safiye, T., Milikić, B., Popović, E., Dubljanin, D., Dubljanin, E., … Čabarkapa, M. (2021). Coronavirus disease 2019 (COVID-19) epidemic and mental health status in the general adult population of Serbia: A cross-sectional study. International Journal of Environmental Research and Public Health, 18(4), 1957. doi:10.3390/ijerph18041957
- Wańkowicz, P., Szylińska, A., & Rotter, I. (2020). Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients. International Journal of Environmental Research and Public Health, 17(16), 5849. doi:10.3390/ijerph17165849
- Winkler, P., Formanek, T., Mlada, K., Kagstrom, A., Mohrova, Z., Mohr, P., & Csemy, L. (2020). Increase in prevalence of current mental disorders in the context of COVID-19: Analysis of repeated nationwide cross-sectional surveys. Epidemiology and Psychiatric Sciences, 29, e173. doi:10.1017/S2045796020000888
- Wu, T., Jia, X., Shi, H., Niu, J., Yin, X., Xie, J., & Wang, X. (2021). Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Affective Disorders, 281, 91–98. doi:10.1016/j.jad.2020.11.117
- Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. doi:10.1016/j.jad.2020.08.001
Appendices Appendix A.
The search strategy of this systematic review and meta-analysis
Appendix B.
Studies included in this meta-analysis