ABSTRACT
Background:
The long-term health effects of bushfires include the potential to trigger new and exacerbate existing mental health problems.
Objective:
This review aimed to determine the prevalence of long-term mental health issues in Australian populations exposed to bushfires.
Method:
A systematic search was conducted in five databases (Embase, Medline, PsycINFO, Scopus, and Web of Science) to identify studies focusing on Australian populations impacted by bushfires with the prevalence of mental health issues reported at 2+ years after bushfire. The Joanna Briggs Institute prevalence critical appraisal tool was utilised. We conducted meta-analyses to determine the prevalence of general psychological distress in the general population, and a narrative synthesis.
Results:
We included 21 articles based on 5 studies and conducted on 3 bushfire events. Meta-analyses showed a pooled prevalence of 14% (95% CI 12%-16%) for psychological distress in the general population at 2–4 years post bushfire. The overall prevalence of long-term psychological problems in firefighters at 2–7 years ranged from 28% to 47.6%. The prevalence of some psychological issues decreased with time and was directly proportional to the level of bushfire impact.
Conclusions:
As the magnitude of long-term bushfire-related mental health impacts in Australia is severe, it is important to monitor psychological problems and assist communities in future. Future research needs include: (a) more studies on the full range of long-term psychological impacts of bushfires, and (b) consensus on instruments and diagnostic criteria to define mental health issues.
HIGHLIGHTS
First systematic review of long-term bushfire mental health issues in Australia.
Indicating substantial mental health problems among affected populations.
Long-term issues were linked to bushfire impact and elevated among firefighters.
Highlighting need for further rigorous research on long-term disaster sequalae.
Antecedentes: Los efectos a largo plazo de los incendios forestales sobre la salud incluyen la posibilidad de desencadenar problemas de salud mental nuevos y de exacerbar los ya existentes.
Objetivo: Esta revisión tuvo como objetivo determinar la prevalencia de los problemas de salud mental a largo plazo en poblaciones australianas expuestas a incendios forestales.
Métodos: Se realizó una revisión sistemática en cinco bases de datos (Embase, Medline, PsycINFO, Scopus y Web of Science) para identificar estudios enfocados en poblaciones australianas afectadas por incendios forestales con una prevalencia de problemas de salud mental reportados de dos años a más después de los incendios. Se empleó la herramienta de evaluación crítica de prevalencia del Instituto Joanna Briggs. Se realizó un metaanálisis para determinar la prevalencia de la angustia psicológica general en la población general y se realizó una síntesis narrativa.
Resultados: Se incluyeron 21 artículos sobre la base de cinco estudios y realizados en tres diferentes incendios forestales. El metaanálisis mostró una prevalencia acumulada de 14 % (95 %, IC 12 %–16 %) para la angustia psicológica en la población general entre los 2 y 4 años luego del incendio forestal. La prevalencia general de los problemas psicológicos a largo plazo en los bomberos fue del 28 % al 47,6 % luego de 2 a 7 años de los incendios. La prevalencia de algunos problemas de salud mental disminuyó en el tiempo y fue directamente proporcional al nivel del impacto del incendio forestal.
Conclusiones: Dado que la magnitud del impacto de los problemas de salud mental asociados a los incendios forestales en Australia es severa, es importante vigilar los problemas psicológicos y apoyar a las comunidades en el futuro. Las investigaciones posteriores necesitan incluir: a) más estudios sobre la magnitud completa del impacto psicológico de los incendios forestales a largo plazo y b) consensos en los instrumentos y los criterios diagnósticos para definir los problemas de salud mental.
背景:森林火灾对健康的长期影响包括引发新的和加剧现有心理健康问题的可能性。
目的:本综述旨在确定暴露于森林火灾的澳大利亚人群中长期心理健康问题的流行率。
方法:在五个数据库(Embase、Medline、PsycINFO、Scopus 和 Web of Science)中进行了系统搜索,以确定针对受森林火灾影响的澳大利亚人群以及在森林火灾后 2 年及以后报告的心理健康问题流行率的研究。使用了乔安娜布里格斯研究所流行率关键评估工具。我们进行了元分析以确定一般人群中一般心理困扰的流行率,并进行了叙述性综合。
结果:我们纳入了 21 篇基于 5 项研究、针对 3 次森林火灾事件的文章。元分析显示,普通人群在森林火灾后 2-4 年中心理困扰的汇总流行率为 14% (95% CI 12%-16%)。2-7 年内消防员长期心理问题的总体流行率在 28% 到 47.6% 之间。一些心理问题的流行率随时间推移而下降,并且直接与森林火灾的影响程度成比例。
结论:由于澳大利亚森林火灾相关长期心理健康影响严重,在未来监测心理问题并帮助大众非常重要。未来的研究需求包括:(a) 更多对森林火灾的长期心理影响的研究,以及 (b) 对于定义心理健康问题工具和诊断标准的共识。
1. Introduction
Wildfires, often called bushfires in Australia, have become a defining characteristic of the Australian contemporary environment (Sharples et al., Citation2016; Vardoulakis, Jalaludin, Morgan, Hanigan, & Johnston, Citation2020). Three well-known bushfires in Australia, the Ash Wednesday bushfires, Black Saturday bushfires and Black Summer bushfires were all related to high temperature and dryness (Cameron et al., Citation2009; Country Fire Authority, Citation2011; Filkov, Ngo, Matthews, Telfer, & Penman, Citation2020; The Bureau of Meteorology, Citation2020; Zhang et al., Citation2020). Such bushfire events are projected to become more frequent and intense in a changing climate, exposing an increasing number of individuals to further dangers (Berry, Waite, Dear, Capon, & Murray, Citation2018).
According to the World Health Organisation (WHO) (WHO, Citation2018), health is not just the absence of disease, but a state of physical, psychological and social well-being. The health effects of bushfires include physical effects of death and injuries and the deterioration of existing physical and mental health conditions (Australian Institute of Health and Welfare, Citation2020a; McFarlane, Clayer, & Bookless, Citation1997). Extreme adverse events like bushfires can trigger new and exacerbate existing mental health problems (Hayes, Blashki, Wiseman, Burke, & Reifels, Citation2018) either directly through exposure to trauma and physical danger or indirectly through damage to homes, physical infrastructure and livelihoods (Berry, Bowen, & Kjellstrom, Citation2010; Berry et al., Citation2018; Hayes et al., Citation2018).
Although a majority of affected individuals are expected to cope with adverse events (Norris, Tracy, & Galea, Citation2009; North Atlantic Treaty Organisation, Citation2008), many will initially experience some form of psychological distress response (Laugharne, Van de Watt, & Janca, Citation2011). For some, this response can develop into ongoing and more severe mental health issues, such as diagnosable mental disorders over time (Goldmann & Galea, Citation2014; Norris et al., Citation2001). Increasing emphasis in disaster research on varying symptom trajectories (resilience, recovery, chronicity, and delayed onset) (Galatzer-Levy, Huang, & Bonanno, Citation2018), along with the adoption of longitudinal study designs, have underscored the need for a long-term perspective in understanding the mental health impacts of disaster.
Several studies have documented the adverse short-term mental health impacts of bushfires and the prevalence of mental health issues among Australians (Australian Institute of Health and Welfare, Citation2020b), with a focus on the first to second years after disasters (Bryant et al., Citation2018). However, to date, no systematic review has examined the prevalence of long-term mental health issues related to bushfires in Australia. It is necessary for policy makers to understand both short-term and long-term mental health service needs. Therefore, this study presents the first systematic literature review of the empirical evidence on the prevalence of long-term mental health issues (after two or more years) among Australian populations exposed to bushfires. Secondary aims were to consider the prevalence of mental health issues (1) across populations (first responders, burns patients, and the general population), (2) in terms of changes over time, and (3) by level of bushfire impact.
2. Methods
2.1. Inclusion and exclusion criteria
We included cohort and cross-sectional studies of people living in bushfire-affected areas and first responders within Australia. Australian first responders were defined as trained first aid workers such as firefighters who provide assistance in case of emergency (Commonwealth of Australia, Citation2019). English language studies containing quantitative data and conducted in a geographical location within Australia or on an Australian remote offshore territory after 1980 were included. We included studies reporting the prevalence of mental health conditions two or more years after a bushfire. Studies with data that could be utilised to calculate the prevalence were also included. Studies relating to other types of fires such as coal mine fire and house fires were excluded.
The primary outcome of this review was the prevalence of long-term mental health issues (after two or more years). Mental health issues were defined as health conditions involving abnormal emotions, thinking or behaviour (or a combination of these characteristics) which can affect relationships with others (American Psychiatric Association, Citation2018; WHO, Citation2019). The main mental health issues considered in this review included (but were not limited to) posttraumatic stress disorder (PTSD), major depressive episode (MDE), psychological distress, and alcohol misuse. Exposure to bushfires was defined as living in an area with bushfire fatalities, houses lost and property damage (Gibbs et al., Citation2013). All populations were eligible, including first responders, burns patients and the general population (inclusive of adults and children). Post-event follow-up timeframes from 2 years onwards were divided into 2–4 years, 5–7 years and ≥8 years after bushfires for the purpose of this study.
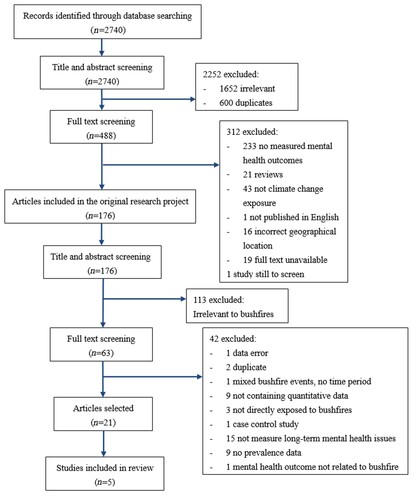
2.2. Search strategy
This literature review built on an earlier systematic literature search completed for a larger research project, which examined the impacts of climate change on mental health in Australia (PROSPERO CRD42020125971). The original search involved five literature databases, namely Embase Classic + Embase, Medline(R), PsycINFO, Scopus, and Web of Science. All database searches were conducted (by MW) on 14th August 2019 and repeated on 24th February 2021 and 30th September 2021. Key search terms were grouped into three tiers pertaining to disaster type, mental health issue and geographical location (). The research protocol for this systematic review was registered on PROSPERO (CRD420201232632).
2.3. Screening
As part of the original project, all article titles and abstracts were initially screened by two researchers (MW and AW) in Covidence, and studies were classified according to the types of climate change exposure. The present systematic review specifically focused on studies examining the impacts of bushfire exposure. Subsequently, two researchers (YZ and HP) further verified the eligibility of studies resulting from the original search and initial screen by conducting additional screening of article titles, abstracts and full texts against the eligibility criteria stated above. Two conflicts were resolved by initial discussion or in consultation with a third researcher (MW).
2.4. Data extraction
Two researchers (YZ and HP) independently extracted the following data from included studies: title, authors, year published, study objectives, study type, year study conducted, population type, age range, mean age, sample size, number and percentage of male and female participants, participation rate, loss to follow up, level of bushfire impact, state/territory, time of follow-up, type of mental health issues measured, assessment instruments, assessment instrument cutoff, prevalence, case numbers, study limitations, and conclusion.
2.5. Quality assessment
The Joanna Briggs Institute (JBI) prevalence critical appraisal tool was utilised to assess the methodological quality of included studies considering aspects of sample frame, sampling method, sample size, study setting, coverage of sample, measurement, data and statistical analysis, and response rate (Joanna Briggs Institute, Citation2020). Two researchers (YZ and HP) independently assessed each included study. Since several publications formed part of the same study, we evaluated the quality of the study overall. The attainment of each of the nine methodological quality aspects was rated as ‘Yes’, ‘No’, ‘Unclear’ or ‘Not applicable’, with overall study scores ranging from zero to nine (). Three disagreements were discussed with four other researchers (MR, LR, AW and MW).
2.6. Narrative synthesis
characterises studies included in this systematic review. It contains the target population, mean age (SD), mental health issues, instruments, time of follow-up (years), the number of people at baseline and follow-up for cohort studies, and the number of participants and response rate for the cross-sectional study. shows the details of mental health issues. The prevalence data were contrasted based on population groups (first responders/burns patients/general population, children/adults/people aged ≥15 years), time frames (2-4 years, 5–7 years, ≥8 years), and the levels of bushfire impact. In accordance with previous research (Bryant et al., Citation2014), different levels of bushfire impact were defined as high-impacted communities (high number of houses lost and fatalities), medium-impacted communities (high number of property damages with small or no fatalities), and low-impacted communities (no evidence of bushfire occurrence) (Bryant et al., Citation2014).
Table 1. Characteristics of studies.
Table 2. Mental health outcomes reported in five studies
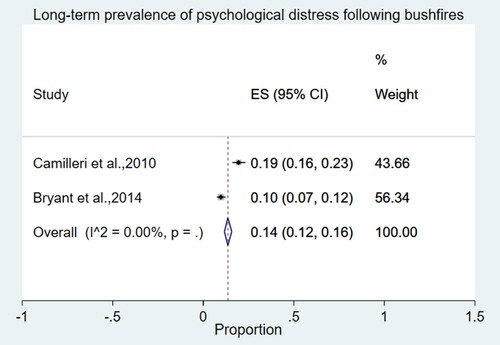
2.7. Meta-analysis
Meta-analyses were performed for studies that were sufficiently similar in (1) population, (2) time frame and (3) reported mental health outcomes. First responders and burns patients were separated from the general population as the bushfire risk they faced was very different from those living in affected communities (Substance Abuse and Mental Health Services Administration, Citation2018). The general population referred to children, and people aged ≥15 years.
Sensitivity analyses were conducted to examine variations in (a) levels of bushfire impact and (b) the homogeneity of participant groups. As the Beyond Bushfire study (Bryant et al., Citation2014) reported both prevalence data for communities with different levels of bushfire impact (low-, medium- and high-impact communities) and overall data for the whole participant sample, we used data from high-impacted communities in the original meta-analysis (for consistency with other high-impacted study samples) and overall participant data in the sensitivity analysis.
Meta-analyses were conducted in STATA 16 (StataCorp, Citation2019) using the ‘metaprop’ command (Nyaga, Arbyn, & Aerts, Citation2014). Meta-analyses with only two studies were conducted using the fixed-effect model because it can be challenging to obtain precise estimates of between-study variation if the number of studies is very small (Chen, Fang, & Wilson, Citation2017). The meta-analysis used the Freeman-Tukey double arcsine to transform prevalence estimates (Barendregt, Doi, Lee, Norman, & Vos, Citation2013) and the overall pooled prevalence estimates were expressed with 95% confidence intervals.
2.8. GRADE
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system was used to assess the quality of the body of evidence (Schünemann, Brożek, Guyatt, & Oxman, Citation2013). All observational studies were initially classified as low quality (Borges Migliavaca et al., Citation2020; Iorio et al., Citation2015; Schünemann et al., Citation2013), and then rated up or down (Joanna Briggs Institute, Citation2020; Schünemann et al., Citation2013).
3. Results
A total of 2740 articles were identified, including 28 from two updated searches. All articles underwent initial title and abstract screening for the original larger project (). After removing irrelevant articles and duplicates, 488 articles were deemed eligible for full-text review. Of those, the 176 articles which met the inclusion criteria of the original project were then selected for the second title and abstract eligibility screening for this systematic review. After removing irrelevant articles, 63 bushfire-related articles underwent full-text screening, of which 21 articles met the inclusion criteria. These 21 articles came from five independent studies, which were ultimately included in this systematic review ().
3.1. Study characteristics
outlines the characteristics of the 5 included studies. Bushfires events related to these studies included the Ash Wednesday bushfires (McFarlane, Citation1986; McFarlane, Policansky, & Irwin, Citation1987)Footnote1, the Black Saturday bushfires (Bryant et al., Citation2014; Pfitzer et al., Citation2016), and the 2003 Canberra bushfires (Camilleri et al., Citation2010). Four studies used cohort study designs (Bryant et al., Citation2014; McFarlane, Citation1986; McFarlane et al., Citation1987; Pfitzer et al., Citation2016), while the other study (Camilleri et al., Citation2010) was cross-sectional. The cross-sectional study was conducted three years following the bushfires. All four cohort studies presented data at 2–4 years after bushfires, while two studies (McFarlane, Citation1986; McFarlane et al., Citation1987) also reported 5–7 and ≥8 years follow-up data, respectively. One study (Bryant et al., Citation2014) covered all three time periods.
Target populations included first responders (mainly firefighters), burns patients and the general population (children and people aged 15 years or over). Among the 21 articles, seven focused on firefighters (Doley, Bell, & Watt, Citation2016; McFarlane, Citation1986; McFarlane, Citation1989; McFarlane, Citation1992; McFarlane, Atchison, Rafalowicz, & Papay, Citation1994; McFarlane & Papay, Citation1992; Spurrell & McFarlane, Citation1993), and eleven on the general adult population (Block et al., Citation2019; Bryant et al., Citation2014; Bryant et al., Citation2017; Bryant et al., Citation2018; Bryant et al., Citation2021; Cowlishaw et al., Citation2021; Gallagher et al., Citation2019; Galletly, Van Hooff, & McFarlane, Citation2011; Lawrence-Wood, Van Hooff, Baur, & McFarlane, Citation2016; McFarlane & Van Hooff, Citation2009; Molyneaux et al., Citation2020). One article each focused on burns patients (Pfitzer et al., Citation2016), children (McFarlane et al., Citation1987), and people aged 15 years or over (Camilleri et al., Citation2010). A total of nine mental health issues were covered: four studies (Bryant et al., Citation2014; McFarlane, Citation1986; McFarlane & Van Hooff, Citation2009; Pfitzer et al., Citation2016) reported PTSD (probable/diagnosis), and three studies (Bryant et al., Citation2014; Camilleri et al., Citation2010; Pfitzer et al., Citation2016) examined general psychological distress. Depression, anxiety and alcohol use were each assessed twice, while other mental health issues (affective disorder, psychiatric impairment, subclinical psychotic experience (SEP), and psychiatric disorder) were only reported once.
3.2. Quality assessment
The five studies scored between six and eight on the JBI prevalence critical appraisal tool, which was considered acceptable quality (the maximum score is nine) (). Four of the nine quality aspects received full marks, meaning that all five studies had appropriate sampling methods, detailed description of study subjects and setting, valid measurement, and clearly reported numerators and denominators. However, only one study (Camilleri et al., Citation2010) had sufficient coverage of the identified sample. Two studies (Bryant et al., Citation2014; Camilleri et al., Citation2010) were classified as ‘Unclear’ for the measurement method, due to the limited information about interviewers. The remaining three aspects on sample frame, sample size and response rate all had a scoring rate of 80%. The cross-sectional study (Camilleri et al., Citation2010) had a 32% response rate, which was considered typical for mail out surveys. Three of four cohort studies (McFarlane, Citation1986; McFarlane et al., Citation1987; Pfitzer et al., Citation2016) had adequate participation rates for the follow-up surveys (72% and 84% for firefighters, 65.6% for children, and 70.6% for burns patients), while the other study (Bryant et al., Citation2014) had a low participation rate with only 16%.
3.3. Prevalence of mental health issues across population groups
3.3.1. General population
A total of seven mental health issues were reported in the general population and the prevalence rates ranged from 3.2% to 36.7% ().
3.3.1.1. Meta-analysis (psychological distress)
Two studies (Bryant et al., Citation2014; Camilleri et al., Citation2010) were included in the meta-analysis of psychological distress. The pooled prevalence of psychological distress among the general population at 2–4 years after bushfires was 14% (95% CI 12%–16%) ().
3.3.1.2. Sensitivity analysis
When the overall participant data for one study (Bryant et al., Citation2014) were included in the meta-analysis (instead of high-impacted community data), the pooled estimate of psychological distress was slightly smaller, 11% (95% CI 10%–13%) ().
3.3.1.3. Other mental health issues
The Beyond Bushfire Study (Bryant et al., Citation2014) reported prevalence data for all three time periods. The prevalence of all four mental health problems (probable PTSD, probable MDE, psychological distress and alcohol use) decreased with time. As an example, the prevalence of psychological distress was 7.9% at 2–4 years after bushfires, decreasing to 5.2% at 5–7 years and to 4.6% after more than 7 years after bushfires ().
Comparing the prevalence in communities with different levels of bushfire impact (high-, medium- and low-impacted) (Bryant et al., Citation2014), the prevalence rates of fire-related probable PTSD, probable MDE and psychological distress were directly proportional to the level of bushfire impact in all three time periods. The prevalence of general probable PTSD had the same trend in the first two periods (). However, it was 2.7% higher in low-impacted communities than in medium-impacted communities in the third period. Distinct from the other mental health issues, the prevalence of heavy drinking in low-affected communities was slightly higher than in medium-affected communities in the first period. It then became the lowest in the following period. More than seven years after bushfires, the proportion of heavy drinking in low-affected communities was the highest, 0.9% and 2.6% higher than that in high- and medium-affected communities, respectively.
3.3.2. Firefighters
Of the five studies, only one (McFarlane, Citation1986) focused on measuring the prevalence of probable PTSD and psychiatric impairment in firefighters. The prevalence of probable PTSD was 30% at 2.5 years after bushfires, and higher at 3.5 years following bushfires (47.6%). It was also noticed that participant numbers in this study reduced from 447 to 337 during the follow-up period.
3.3.3. Burns patients
One small study examined probable PTSD, anxiety and depression symptoms and psychological distress among burns patients at 2–4 years after bushfires (Pfitzer et al., Citation2016). The proportion of anxiety and depression symptoms and psychological distress was the same (33%), followed by probable PTSD (25%).
3.4. GRADE
Two mental health outcomes (probable PTSD and psychological distress) were included in the summary of findings table (). For both outcomes, the risk of bias of these studies was not serious as they all had appropriate sampling and clear numerators and denominators. The high directness was related to the use of valid instruments. Therefore, the qualities of both outcomes were rated up to high level. However, the imprecision and heterogeneity were both marked as ‘serious’ due to the use of different instruments, coverage of different age groups, and small sample size (in one study). Thus, the evidence quality was downgraded back to low. There was no evidence indicating publication bias, which maintained the final evidence quality of the two outcomes at the low level.
4. Discussion
The aim of this review was to determine the prevalence of long-term mental health issues in selected Australian populations exposed to bushfires. We identified five studies assessing nine psychological problems across three time periods after bushfires. This review presents three main findings: Firstly, the pooled prevalence estimate of psychological distress was 14% (95% CI 12%–16%) among the general population 2–4 years after bushfires. Secondly, the overall prevalence of long-term mental health issues (including probable PTSD and psychiatric impairment) ranged from 28% to 47.6% in firefighters 2–7 years following bushfires. Thirdly, the prevalence of long-term mental health issues in the general population decreased with time and it is likely to be directly proportional to the level of bushfire impact in communities.
4.1. Highly prevalent long-term mental health issues after bushfires
Our review indicated that a substantial number of people among the general population experienced long-term mental health issues after bushfire occurrence. This finding is also supported by a cohort study of mental health symptoms after the Fort McMurray wildfire in Canada which followed students aged 11–19 years at 1.5, 2.5 and 3.5 years after the wildfire (Brown et al., Citation2021). It showed that mental health symptoms such as PTSD, depression and anxiety increased at 3.5 years after the wildfire, indicating that mental health status can have a long-term deterioration during this period (Brown et al., Citation2021).
In the context of Australia, although the prevalence of psychological problems in different periods decreased with time, the mental health issues of people exposed to bushfires were still highly prevalent in the long-term. According to the National Health Survey, the prevalence of PTSD was only 1.9% among a general population of adults in 2017–2018 (Australian Bureau of Statistics, Citation2018), which is much lower than what we found in this review (2–4 years: 17.5%, 4–7 years: 14.2%, ≥8 years: 15.1%). Compared with people in general, the mental status of people exposed to bushfires appears to require special attention.
McFarlane and Williams (McFarlane & Williams, Citation2012) indicated that the long-term needs of people suffering from disasters were often underestimated as most people had some form of transitory stress response after disasters. Their mental status was typically expected to improve over time (McFarlane & Williams, Citation2012). Also, it has been found that 33% of people who had long-term severe mental illness after the bushfire did not receive any mental health assistance (Bryant et al., Citation2014). Therefore, it is vital to monitor long-term psychological problems such as PTSD and assist communities in the future. To achieve this, long-term adequate funding is needed (Black Dog Institute, Citation2020; Brown et al., Citation2021), and it is important to focus on strengthening community networks due to its positive effects on mental health (Head to Health, Citation2019).
4.2. Higher bushfire-related mental health issues among firefighters
The prevalence of long-term bushfire-related mental health issues in firefighters was found to be higher than in the general population exposed to bushfires. This finding aligned with previous surveys showing that firefighters have a higher risk of experiencing psychological problems than the general population (Substance Abuse and Mental Health Services Administration, Citation2018; United Voice WA, Citation2018), as well as with a broader systematic review which indicated an elevated risk of PTSD among first responders in disaster contexts compared to the general population (Galea, Nandi, & Vlahov, Citation2005). Additionally, the repeat trauma exposure among firefighters constitutes an occupational hazard that could be a potential contributing cause of the increase in prevalence over time (Harvey et al., Citation2016). This is supported by an American study (Jahnke, Poston, Haddock, & Murphy, Citation2016) that found it was more common for firefighters to have poorer mental health due to repeat trauma exposure, rather than a single event. It also concords with the broader literature on the impacts of repeat disaster exposure (Leppold, Gibbs, Block, Reifels, & Quinn, Citation2022). In view of the large number of volunteer emergency responders involved in the rescue of recent bushfire events in Australia (Mao, Citation2019), sustained psychological support and resources tailored to this particular occupational group are required (Harvey et al., Citation2016; Milligan-Saville et al., Citation2018).
4.3. Long-term mental health issues associated with level of bushfire impact
Unsurprisingly, the prevalence of some long-term mental health issues was related to the degree of bushfire impact. After using overall participant data instead of data from high-impacted communities in the sensitivity analysis, the pooled prevalence estimate for psychological distress was slightly smaller. Also, the prevalence of some psychological problems reported in the Beyond Bushfire study was directly proportional to the degree of bushfire impact in communities. However, there was no such difference in the proportion of alcohol abuse among these affected communities, which indicated that alcohol use might not be related to bushfires. This finding is consistent with previous studies that found few or no new substance use disorders were reported after disasters (Alexander & Ward, Citation2018; Substance Abuse and Mental Health Services Administration, Citation2020; Van Der Velden & Kleber, Citation2009). The proportion of heavy drinking was highest in the first period after bushfires, which also reflected that people with a history of substance use might increase their use after disasters (Alexander & Ward, Citation2018). Therefore, increased alcohol use still should be identified as a potential disaster reaction and coping tips and supports should be provided to survivors (Substance Abuse and Mental Health Services Administration, Citation2020).
4.4. Strengths
There are several strengths in this systematic review. First, this research represents the first systematic review of long-term bushfire-related mental health issues among Australian populations. Second, our systematic review involved a rigorous study search and selection process, including five databases to cover relevant publications. Two updated searches were conducted to include newly published articles. Thirdly, this review systematically considered several sources of bias. We also conducted a sensitivity analysis to test the robustness of estimates. Additionally, this review includes both pooled estimates and specific estimates. While pooled estimates are generally more reliable across contexts, specific estimates can be informative for people in similar circumstances.
4.5. Limitations
Four main limitations were encountered in this systematic review. First, our review only included a small number of studies. Although 21 publications were selected after screening, many of them described the same cohort study looking at different subpopulations, mental health outcomes and time frames. Thus, only five studies were finally included in this review. Second, only one meta-analysis was conducted due to different mental health issues measured in the same population group. From the characteristics of studies, the population and instruments were found to be quite different among the five included studies. Taking psychological distress as an example, although three studies reported the same mental health outcome in the same period, different populations, instruments and cut-off scores could contribute to the variance between results, which could cause a lack of precision of the outcome variable. We therefore included only comparable studies in the meta-analysis. Third, available study prevalence data did not permit more fine-grained systematic outcomes analyses by other key demographics, such as gender and age, that are commonly associated with adverse disaster mental health outcomes. Fourth, due to the common absence of pre-event data in disaster studies, it is difficult to determine how much of the distress is related to the bushfires and how much to other factors. The impact of such events is therefore often assessed by comparing prevalence across different levels of event exposure.
4.6. Suggestions for future studies
We identified several future research needs as a result of this study. First, considering the number of studies is still relatively small, future studies need to focus on the full range of long-term psychological impacts of bushfires among Australian populations. Second, addressing the heterogeneity of outcome measures would facilitate evidence aggregation and meaningful meta-analysis. In this systematic review, due to the use of different instruments and cut-off scores, PTSD was separated into PTSD diagnosis and probable PTSD, which should not be combined. This point was also demonstrated in a recent study on depression, which established that the prevalence of probable depression assessed by the PHQ-9 is approximately twice as high as that using full diagnostic DSM criteria (Levis et al., Citation2020). Thus, if future studies could agree on the use of a core set of comparable outcome measures, it will become more feasible for researchers to accurately compare study outcomes and synthesise the evidence base.
5. Conclusion
This systematic review established that the long-term prevalence of bushfire-related mental health issues is substantial in affected Australian populations, and most pronounced among firefighters, ranging from 28% to 47.6% 2–7 years following bushfires. Additionally, the prevalence of long-term mental health problems decreased with time among adults, and it was likely to be directly proportional to the degree of bushfire impact within communities. As the magnitude of long-term bushfire-related mental health issues is substantial in Australia, it is important to keep monitoring psychological problems and to assist communities in the future. However, with only five studies included in this review, and with considerable heterogeneity between them, there are still substantial gaps in our knowledge of the prevalence of long-term mental health issues after bushfires. More studies are needed to investigate the long-term psychological problems among Australians exposed to bushfires.
Acknowledgements
We would like to acknowledge that this review is associated with a larger systematic review of the climate change and mental health literature in Australia. The systematic review has been registered in PROSPERO [CRD42020125971]. The larger systematic review was supported by seed funding from the Melbourne Sustainable Society Institute at The University of Melbourne.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Notes
1 Studies comprising multiple articles are referred to by their first publication.
References
- Alexander, A. C., & Ward, K. D. (2018). Understanding postdisaster substance use and psychological distress using concepts from the self-medication hypothesis and social cognitive theory. Journal of Psychoactive Drugs, 50(2), 177–186. https://doi.org/10.1080/02791072.2017.1397304
- American Psychiatric Association. (2018). What is mental illness. Retrieved from https://www.psychiatry.org/patients-families/what-is-mental-illness
- Australian Bureau of Statistics. (2018). National health survey: First results. Retrieved from https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release#data-download
- Australian Institute of Health and Welfare. (2020a). Natural Environment and Health. Canberra: AIHW.
- Australian Institute of Health and Welfare. (2020b). Australian Bushfires 2019–20: Exploring the Short-Term Health Impacts. Canberra: AIHW.
- Barendregt, J. J., Doi, S. A., Lee, Y. Y., Norman, R. E., & Vos, T. (2013). Meta-analysis of prevalence. Journal of Epidemiology and Community Health, 67(11), 974–978. https://doi.org/10.1136/jech-2013-203104
- Berry, H. L., Bowen, K., & Kjellstrom, T. (2010). Climate change and mental health: A causal pathways framework. International Journal of Public Health, 55(2), 123–132. https://doi.org/10.1007/s00038-009-0112-0
- Berry, H. L., Waite, T. D., Dear, K. B. G., Capon, A. G., & Murray, V. (2018). The case for systems thinking about climate change and mental health. Nature Climate Change, 8(4), 282–290. https://doi.org/10.1038/s41558-018-0102-4
- Black Dog Institute. (2020). Mental health interventions following disasters. Retrieved from https://www.blackdoginstitute.org.au/wp-content/uploads/2020/04/mental-health-interventions-following-disasters-black-dog-institute-february-2020.pdf?sfvrsn = 0
- Block, K., Molyneaux, R., Gibbs, L., Alkemade, N., Baker, E., MacDougall, C., … Forbes, D. (2019). The role of the natural environment in disaster recovery: ‘We live here because we love the bush’. Health & Place, 57, 61–69. https://doi.org/10.1016/j.healthplace.2019.03.007
- Borges Migliavaca, C., Stein, C., Colpani, V., Barker, T. H., Munn, Z., & Falavigna, M. (2020). How are systematic reviews of prevalence conducted? A methodological study. BMC Medical Research Methodology, 20(1). https://doi.org/10.1186/s12874-020-00975-3
- Brown, M. R. G., Pazderka, H., Agyapong, V. I. O., Greenshaw, A. J., Cribben, I., Brett-MacLean, P., … Silverstone, P. H. (2021). Mental health symptoms unexpectedly increased in students aged 11-19 years during the 3.5 years after the 2016 Fort McMurray wildfire: Findings from 9,376 survey responses. Frontiers in Psychiatry, 12, Article 676256.
- Bryant, R. A., Gallagher, H. C., Gibbs, L., Pattison, P., MacDougall, C., Harms, L., … Lusher, D. (2017). Mental health and social networks after disaster. The American Journal of Psychiatry, 174(3), 277–285. https://doi.org/10.1176/appi.ajp.2016.15111403
- Bryant, R. A., Gibbs, L., Colin Gallagher, H., Pattison, P., Lusher, D., MacDougall, C., … O’Donnell, M. (2021). The dynamic course of psychological outcomes following the Victorian Black Saturday bushfires. Australian and New Zealand Journal of Psychiatry, 55(7), 666–677. Article 0004867420969815
- Bryant, R. A., Gibbs, L., Gallagher, H. C., Pattison, P., Lusher, D., MacDougall, C., … Forbes, D. (2018). Longitudinal study of changing psychological outcomes following the Victorian Black Saturday bushfires. Australian & New Zealand Journal of Psychiatry, 52(6), 542–551. https://doi.org/10.1177/0004867417714337
- Bryant, R. A., Waters, E., Gibbs, L., Gallagher, H. C., Pattison, P., Lusher, D., … Forbes, D. (2014). Psychological outcomes following the Victorian Black Saturday bushfires. The Australian and New Zealand Journal of Psychiatry, 48(7), 634–643. https://doi.org/10.1177/0004867414534476
- The Bureau of Meteorology. (2020). Annual climate statement 2019. Retrieved from http://www.bom.gov.au/climate/current/annual/aus/#tabs = Overview
- Cameron, P. A., Mitra, B., Fitzgerald, M., Scheinkestel, C. D., Stripp, A., Batey, C., … Cleland, H. (2009). Black Saturday: the immediate impact of the February 2009 bushfires in Victoria, Australia. Medical Journal of Australia, 191(1), 11–16. https://doi.org/10.5694/j.1326-5377.2009.tb02666.x
- Camilleri, P., Healy, C., Macdonald, E., Nicholls, S., Sykes, J., Winkworth, G., & Woodward, M. (2010). Recovery from bushfires: The experience of the 2003 Canberra bushfires three years after. Australasian Journal of Paramedicine, 8(1), 1–15. https://doi.org/10.33151/ajp.8.1.112
- Chen, D.-G., Fang, D., & Wilson, J. R. (2017). Meta-analysis of two studies with random effects? Journal of Minimally Invasive Gynecology, 24(5), 689–690. https://doi.org/10.1016/j.jmig.2017.05.008
- Commonwealth of Australia. (2019). The people behind 000: mental health of our first responders. Retrieved from https://parlinfo.aph.gov.au/parlInfo/download/committees/reportsen/024252/toc_pdf/Thepeoplebehind000mentalhealthofourfirstresponders.pdf;fileType=application%2Fpdf
- Country Fire Authority. (2011). Ash Wednesday. updated April. Retrieved from https://webcache.googleusercontent.com/search?q = cache:ZHxUSVuqo0EJ:https://www.cfa.vic.gov.au/documents/20143/74279/Ash-Wednesday.doc/df7684b9-66a1-00c4-2154-5b986c608664+&cd = 2&hl = en&ct = clnk&gl = au
- Cowlishaw, S., Metcalf, O., Varker, T., Stone, C., Molyneaux, R., Gibbs, L., … Forbes, D. (2021). Anger dimensions and mental health following a disaster: Distribution and implications after a major bushfire, Journal of Traumatic Stress, 34(1), 46–55.
- Doley, R. M., Bell, R., & Watt, B. D. (2016). An investigation into the relationship between long-term posttraumatic stress disorder symptoms and coping in Australian volunteer firefighters. The Journal of Nervous and Mental Disease, 204(7), 530–536. https://doi.org/10.1097/NMD.0000000000000525
- Filkov, A. I., Ngo, T., Matthews, S., Telfer, S., & Penman, T. D. (2020). Impact of Australia's catastrophic 2019/20 bushfire season on communities and environment. Retrospective Analysis and Current Trends. Journal of Safety Science and Resilience, 1(1), 44–56. https://doi.org/10.1016/j.jnlssr.2020.06.009
- Galatzer-Levy, I. R., Huang, S. H., & Bonanno, G. A. (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. https://doi.org/10.1016/j.cpr.2018.05.008
- Galea, S., Nandi, A., & Vlahov, D. (2005). The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews, 27, 78–91. https://doi.org/10.1093/epirev/mxi003
- Gallagher, H. C., Block, K., Gibbs, L., Forbes, D., Lusher, D., Molyneaux, R., … Bryant, R. A. (2019). The effect of group involvement on post-disaster mental health: A longitudinal multilevel analysis. Social Science & Medicine, 220, 167–175. https://doi.org/10.1016/j.socscimed.2018.11.006
- Galletly, C., Van Hooff, M., & McFarlane, A. (2011). Psychotic symptoms in young adults exposed to childhood trauma–a 20 year follow-up study. Schizophrenia Research, 127(1-3), 76–82. https://doi.org/10.1016/j.schres.2010.12.010
- Gibbs, L., Waters, E., Bryant, R. A., Pattison, P., Lusher, D., Harms, L., … Forbes, D. (2013). Beyond bushfires: Community, resilience and recovery – a longitudinal mixed method study of the medium to long term impacts of bushfires on mental health and social connectedness. BMC Public Health, 13(1). https://doi.org/10.1186/1471-2458-13-1036
- Goldmann, E., & Galea, S. (2014). Mental health consequences of disasters. Annual Review of Public Health, 35(1), 169–183.
- Harvey, S. B., Milligan-Saville, J. S., Paterson, H. M., Harkness, E. L., Marsh, A. M., Dobson, M., … Bryant, R. A. (2016). The mental health of fire-fighters: An examination of the impact of repeated trauma exposure. The Australian and New Zealand Journal of Psychiatry, 50(7), 649–658. https://doi.org/10.1177/0004867415615217
- Hayes, K., Blashki, G., Wiseman, J., Burke, S., & Reifels, L. (2018). Climate change and mental health: Risks, impacts and priority actions. International Journal of Mental Health Systems, 12(1). https://doi.org/10.1186/s13033-018-0210-6
- Head to Health. (2019). Connecting with community. Retrieved from https://headtohealth.gov.au/meaningful-life/connectedness/community
- Iorio, A., Spencer, F. A., Falavigna, M., Alba, C., Lang, E., Burnand, B., … Guyatt, G. (2015). Use of GRADE for assessment of evidence about prognosis: Rating confidence in estimates of event rates in broad categories of patients. BMJ: British Medical Journal, 350(h870). https://doi.org/10.1136/bmj.h870
- Jahnke, S. A., Poston, W. S. C., Haddock, C. K., & Murphy, B. (2016). Firefighting and mental health: Experiences of repeated exposure to trauma. Work, 53(4), 737–744. https://doi.org/10.3233/WOR-162255
- Joanna Briggs Institute. (2020). CRITICAL APPRAISAL TOOLS. Retrieved from https://jbi.global/critical-appraisal-tools
- Laugharne, J., Van de Watt, G., & Janca, A. (2011). After the fire: The mental health consequences of fire disasters. Current Opinion in Psychiatry, 24(1), 72–77.
- Lawrence-Wood, E., Van Hooff, M., Baur, J., & McFarlane, A. C. (2016). Re-experiencing phenomena following a disaster: The long-term predictive role of intrusion symptoms in the development of post-trauma depression and anxiety. Journal of Affective Disorders, 190, 278–281. https://doi.org/10.1016/j.jad.2015.10.029
- Leppold, C., Gibbs, L., Block, K., Reifels, L., & Quinn, P. (2022). Public health implications of multiple disaster exposures. The Lancet Public Health, 7(3), e274–ee86. https://doi.org/10.1016/S2468-2667(21)00255-3
- Levis, B., Benedetti, A., Ioannidis, J. P. A., Sun, Y., Negeri, Z., He, C., … Thombs, B. D. (2020). Patient health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. Journal of Clinical Epidemiology, 122, 115–128. e1. https://doi.org/10.1016/j.jclinepi.2020.02.002
- Mao, F. (2019). Australia fires: The thousands of volunteers fighting the flames. Retrieved from https://www.bbc.com/news/world-australia-50887982
- McFarlane, A. C. (1986). Long-term psychiatric morbidity after a natural disaster. Implications for disaster planners and emergency services. Medical Journal of Australia, 145(11-12), 561–563. https://doi.org/10.5694/j.1326-5377.1986.tb139497.x
- McFarlane, A. C. (1989). The aetiology of post-traumatic morbidity: Predisposing, precipitating and perpetuating factors. The British Journal of Psychiatry: The Journal of Mental Science, 154, 221–228. https://doi.org/10.1192/bjp.154.2.221
- McFarlane, A. C. (1992). Avoidance and intrusion in posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 180(7), 439–445. https://doi.org/10.1097/00005053-199207000-00006
- McFarlane, A. C., Atchison, M., Rafalowicz, E., & Papay, P. (1994). Physical symptoms in post-traumatic stress disorder. Journal of Psychosomatic Research, 38(7), 715–726. https://doi.org/10.1016/0022-3999(94)90024-8
- McFarlane, A. C., Clayer, J. R., & Bookless, C. L. (1997). Psychiatric morbidity following a natural disaster: An Australian bushfire. Social Psychiatry and Psychiatric Epidemiology, 32(5), 261–268. https://doi.org/10.1007/BF00789038
- McFarlane, A. C., & Papay, P. (1992). Multiple diagnoses in posttraumatic stress disorder in the victims of a natural disaster. The Journal of Nervous and Mental Disease, 180(8), 498–504. https://doi.org/10.1097/00005053-199208000-00004
- McFarlane, A. C., Policansky, S. K., & Irwin, C. (1987). A longitudinal study of the psychological morbidity in children due to a natural disaster. Psychological Medicine, 17(3), 727–738. https://doi.org/10.1017/S0033291700025964
- McFarlane, A. C., & Van Hooff, M. (2009). Impact of childhood exposure to a natural disaster on adult mental health: 20-year longitudinal follow-up study. The British Journal of Psychiatry: The Journal of Mental Science, 195(2), 142–148. https://doi.org/10.1192/bjp.bp.108.054270
- McFarlane, A. C., & Williams, R. (2012). Mental health services required after disasters: Learning from the lasting effects of disasters. Depression Research and Treatment, 2012, Article 970194. https://doi.org/10.1155/2012/970194
- Milligan-Saville, J., Choi, I., Deady, M., Scott, P., Tan, L., Calvo, R. A., … Harvey, S. B. (2018). The impact of trauma exposure on the development of PTSD and psychological distress in a volunteer fire service. Psychiatry Research, 270, 1110–1115. https://doi.org/10.1016/j.psychres.2018.06.058
- Molyneaux, R., Gibbs, L., Bryant, R. A., Humphreys, C., Hegarty, K., Kellett, C., … Forbes, D. (2020). Interpersonal violence and mental health outcomes following disaster. BJPsych Open, 6(1), E1. https://doi.org/10.1192/bjo.2019.82
- Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., … Kaniasty, K. (2001). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry, 65(3), 207–239. https://doi.org/10.1521/psyc.65.3.207.20173
- Norris, F. H., Tracy, M., & Galea, S. (2009). Looking for resilience: Understanding the longitudinal trajectories of responses to stress. Social Science & Medicine, 68(12), 2190–2198. https://doi.org/10.1016/j.socscimed.2009.03.043
- North Atlantic Treaty Organisation. (2008). Psychosocial care for people affected by disasters and major incidents: a model for designing, delivering and managing psychosocial services for people involved in major incidents, conflict, disasters and terrorism.
- Nyaga, V. N., Arbyn, M., & Aerts, M. (2014). Metaprop: A Stata command to perform meta-analysis of binomial data. Archives of Public Health, 72(1). https://doi.org/10.1186/2049-3258-72-39
- Pfitzer, B., Katona, L. J., Lee, S. J., O'Donnell, M., Cleland, H., Wasiak, J., … Ellen, S. (2016). Three years after Black Saturday: Long-term psychosocial adjustment of burns patients as a result of a major bushfire. Journal of Burn Care & Research: Official Publication of the American Burn Association, 37(3), e244–e253. https://doi.org/10.1097/BCR.0000000000000223
- Schünemann, H., Brożek, J., Guyatt, G., & Oxman, A. (2013). GRADE handbook. Retrieved from Andrew Oxman.
- Sharples, J. J., Cary, G. J., Fox-Hughes, P., Mooney, S., Evans, J. P., Fletcher, M.-S., … Baker, P. (2016). Natural hazards in Australia: Extreme bushfire. Climatic Change, 139(1), 85–99. https://doi.org/10.1007/s10584-016-1811-1
- Spurrell, M. T., & McFarlane, A. C. (1993). Post-traumatic stress disorder and coping after a natural disaster. Social Psychiatry and Psychiatric Epidemiology, 28(4), 194–200. https://doi.org/10.1007/BF00797323
- StataCorp. (2019). Stata Statistical Manual: Release 16. College Station, TX: StataCorp LLC.
- Substance Abuse and Mental Health Services Administration. (2018). First Responders: Behavioral Health Concerns, Emergency Response, and Trauma. Retrieved from https://www.samhsa.gov/sites/default/files/dtac/supplementalresearchbulletin-firstresponders-may2018.pdf
- Substance Abuse and Mental Health Services Administration. (2020). Substance Use Disorders and Disasters. Retrieved from https://www.samhsa.gov/dbhis-collections/substance-use
- United Voice WA. (2018). Inquiry into the role of the Commonwealth, state and territory Governments in addressing the high rates of mental health conditions experienced by first responders, emergency service workers and volunteers. Retrieved from file:///C:/Users/AIR/Downloads/sub86_United%20Voice%20Western%20Australia.pdf.
- Van Der Velden, P., & Kleber, R. (2009). Substance use and misuse after disasters: Prevalences and correlates. In Y. Neria, S. Galea & F. Norris (Eds.), Mental health and disasters (pp. 94–115). Cambridge: Cambridge University Press. doi:10.1017/CBO9780511730030.006
- Vardoulakis, S., Jalaludin, B. B., Morgan, G. G., Hanigan, I. C., & Johnston, F. H. (2020). Bushfire smoke: Urgent need for a national health protection strategy. Medical Journal of Australia, 212(8), 349–353. e1. https://doi.org/10.5694/mja2.50511
- WHO. (2018). Mental health: strengthening our response. Retrieved from https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
- WHO. (2019). Mental disorders. Retrieved from https://www.who.int/news-room/fact-sheets/detail/mental-disorders.
- Zhang, Y., Beggs, P. J., McGushin, A., Bambrick, H., Trueck, S., Hanigan, I. C., … Watts, N. (2020). The 2020 special report of the MJA–Lancet Countdown on health and climate change: lessons learnt from Australia’s “Black Summer”.
Appendix
Figure A1. Meta-analysis of psychological distress among the general population (with overall data) 2–4 years after bushfires.
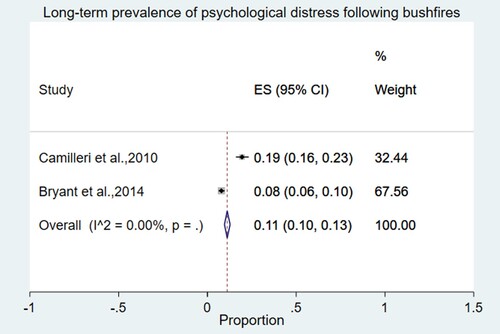
Table A1. Databases, search periods, and related keywords.
Table A2. Methodological quality of the included studies (n = 5) (Joanna Briggs Institute, 2020).
Table A3: Summary of findings: The prevalence of long-term mental health issues in Australians exposed to bushfires.