ABSTRACT
Background: Hospital readmissions have been a major challenge to the US health system. Medicare data shows that approximately 25% of Medicare skilled nursing facility (SNF) residents are readmitted back to the hospital within 30 days. Some of the major reasons for high readmission rates include fragmented information exchange during transitions of care and limited access to physicians round-the-clock in SNFs. These represent safety, quality, and health outcome concerns.
Aim: The goal of the project was to reduce hospital readmission rates from SNFs by improving transition of care and increasing physician availability in SNFs (five to seven days a week physical presence with 24/7 accessibility by phone).
Methods: We proposed a model whereby a hospitalist-led team, including the resident on the geriatrics rotation, followed patients discharged from the hospital to one SNF. Readmission rates pre- and post-implementation were compared.
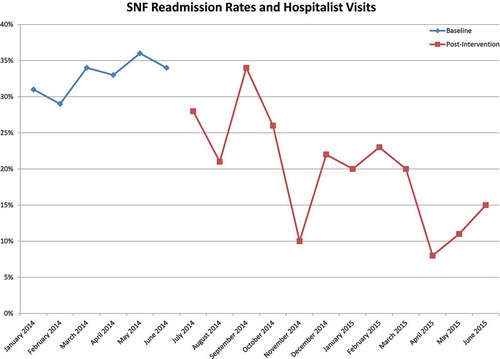
Study results: The period between January 2014 and June 2014 served as the baseline and showed readmission rate of 32.32% from the SNF back to the hospital. After we implemented the new hospitalist SNF model in June 2014, readmission rates decreased to 23.96% between July 2014 and December 2014. From January 2015 to June 2015, the overall readmission rate from the SNF reduced further to 16.06%. Statistical analysis revealed a post-intervention odds ratio of 0.403 (p < 0.001).
Conclusion: The government is piloting several care models that incentivize value- based behavior. Our study strongly suggests that the hospitalist-resident continuity model of following patients to the SNFs can significantly decrease 30-days hospital readmission rates.
1. Introduction
Over the last several decades, the role of the nursing home has changed dramatically from a purely residential setting where predominantly older, cognitively impaired and functionally dependent individuals lived to a post-acute facility providing skilled care to medically complex patients discharged from hospitals [Citation1]. To qualify for Medicare skilled nursing facility (SNF) services, a beneficiary requires daily skilled nursing or rehabilitative therapy services, generally within 30 days of a hospital stay of at least three days duration. In addition, they must be admitted to the nursing home due to a condition related to that hospitalization.
Skilled nursing facility residents often experience potentially avoidable inpatient hospitalizations. These hospitalizations are expensive, disruptive, and disorienting for frail elders and people with disabilities [Citation2,Citation3,Citation4]. Nursing facility residents are especially vulnerable to the risks that accompany hospital stays and transitions between nursing facilities and hospitals, including medication errors and hospital-acquired infections [Citation5–Citation8].
Many nursing facility residents are enrolled in both the Medicare and Medicaid programs (Medicare-Medicaid enrollees). According to Mor et al. [Citation9], an analysis of SNF data from 2006 Medicare claims merged with the Minimum Data Set (MDS), 23.5% of SNF stays resulted in rehospitalization within 30 days of the initial hospital discharge. The average Medicare payment for each readmission was $10 352 per hospitalization, for a total of $4.34 billion. Of these rehospitalizations, 78% were deemed potentially avoidable. Applying this figure to the aggregate cost indicates that avoidable hospitalizations resulted in an excess cost of $3.39 billion (78% of $4.34 billion) to Medicare [Citation9,Citation10].
Although nursing homes may hospitalize residents primarily for clinical reasons, research indicates that several nonclinical factors can also influence homes’ decisions to hospitalize residents. These factors include the availability and training of nursing staff in the home, resident and family member preferences, and physician availability and preferences [Citation9,Citation11]. Additionally, aspects of Medicare payment policies and other economic factors can influence hospitalization rates [Citation8,Citation12].
This study sought to assess impact on hospital readmission rates by providing close follow up to our nursing home residents through a team of hospitalist – Internal Medicine residents.
1.1. Problems
Traditionally, primary care physicians (PCPs) followed their patients after discharge from hospitals to SNFs. This model sufficed in prior days when PCPs followed their patients across all settings (outpatient, inpatient, and SNFs). However, almost 80% of all patients in hospitals are seen by hospitalists. There is often a communication gap between hospitalists and PCPs.
The demands of outpatient medicine have increased and this has made it difficult for PCPs to follow their patients across different settings given the time constraint.
1.2. Potential solutions
Hospitalists with involvement of internal medicine (IM) residents could follow patients in SNFs after hospital discharge. One advantage of this model is that communication gaps are reduced as the same group of physicians follows patients in SNFs.
Increasing physician availability in SNFs (five to seven days a week physical presence with 24/7 accessibility by phone) can prevent many of the early readmissions back to hospital during the early post discharge period which is the most crucial time for readmissions. By providing better physician availability to SNFs, many of the problems can be solved right away rather than sending patients back to an emergency room (ER) for evaluation.
2. Methods
2.1. Setting and study design
The study was conducted in a SNF facility nearby the community hospital. The hospitalist-IM resident team started following up on patients in SNF post discharge. Baseline readmission rates for six months were obtained prior to the introduction of this model. Thereafter, monthly readmission rates were collected for one year.
3. Data analysis and results
The period between January 2014 and June 2014 served as the baseline and showed a readmission rate of 32.32% from SNF back to the hospital. After the new hospitalist-resident model implementation in June 2014, readmission rates decreased to an average of 23.96% between July 2014 and December 2014. Between January 2015 and June 2015, the overall readmission rate from the SNF reduced even further to an average of 16.06% (). To test whether or not implementation impacted readmission rates, we analyzed the dataset of 825 cases using a multivariate approach. We developed a logistic regression model predicting whether or not each case was readmitted. Month-to-variation was modeled through the use of dummy codes representing each month. The effect of implementation was tested through the further addition to the model of a dummy code representing whether the case occurred before intervention or after it had begun. Controlling for monthly variation in readmission, the effects of the implementation were significant (beta coefficient = −0.91, p < 0.001). The odds ratio (comparing post-implementation likelihood to pre-implementation likelihood) was 0.40, indicating that the likelihood of readmission decreased by over half during implementation.
4. Discussion
Given evidence that nearly one out of every four Medicare beneficiaries discharged from acute care hospitals who subsequently received care in a SNF were readmitted to the hospital within 30 days [Citation9], monitoring hospital readmissions of beneficiaries utilizing SNFs is an important policy area for Center for Medicare and Medicaid Services (CMS) [Citation6,Citation9,Citation13]. As a part of the Nursing Home Quality Initiative, CMS directed RTI (Research Triangle Institute) International to develop the skilled nursing facility 30-Day All-Cause Readmission Measure (SNFRM). The goal of the SNFRM is to measure facility-level readmission rates among beneficiaries utilizing SNFs [Citation14].
The intent of the SNFRM is to encourage SNF providers to monitor and reduce hospital readmissions, thereby reducing costs and improving the quality of care that Medicare beneficiaries receive during their SNF stay. Our approach to decreasing readmissions was to redesign the care model by ensuring that the same provider group followed these patients across two different healthcare settings. Our model improved transition of care between the two facilities and provided increased accessibility to physicians. This ensures smooth transition of care without losing crucial patient health information. By having the same provider group taking care of patients in both hospital and SNF settings, we showed a reduction in hospital readmission rates. This had a positive impact on medical education as well, as the residents understood better about the pitfalls that occur during transitions of care [Citation15].
Continued refinement and development of readmission measures for SNFs is underway, and the SNFRM will be one of CMS’s portfolios of readmission measures for post-acute care facilities [Citation14].
5. Limitations
This study was conducted in an academic community hospital and thus the reported results need to be confirmed in a large sample including multiple SNFs and in non-academic settings.
6. Conclusion
This novel idea of a hospitalist-resident continuity model of following patients to SNFs can significantly decrease readmissions back to the hospital from SNFs within 30 days. Since the same group of physicians take care of patients in SNFs following hospital discharge, there is improved overall continuity of care and follow up of patient in SNFs. This model will also provide better availability of physicians in skilled nursing facilities which also appeared to be one of the major reasons for hospital readmissions. By providing better availability of physicians, many of the problems commonly leading to the ER visits could be solved in the nursing facility itself.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Burke RE, Juarez-Colunga E, Levy C, et al. Rise of post-acute care facilities as a discharge destination of US hospitalizations. JAMA Int Med. 2015;175:295–296.
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009 Apr 2;360(14):1418–1428. DOI:10.1056/NEJMsa0803563
- Ouslander J, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc. 2010;58(4):627–635. DOI:10.1111/j.1532-5415.2010.02768.x
- Ouslander J, Lamb G, Tappen R, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc. 2011;59(4):745–753. DOI:10.1111/j.1532-5415.2011.03333.x
- Coleman E, Min S, Chomiak A, et al. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39(5):1449–1466. DOI:10.1111/j.1475-6773.2004.00298.x
- King B, Gilmore-Bykovskyi A, Roiland R, et al. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc. 2013;61(7):1095–1102. DOI:10.1111/jgs.12328
- Boockvar K, Fishman E, Kyriacou C, et al. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Int Med. 2004;164(5):545. DOI:10.1001/archinte.164.5.545
- Tjia J, Bonner A, Briesacher B, et al. Medication discrepancies upon hospital to skilled nursing facility transitions. J Gen Int Med. 2009;24(5):630–635. DOI:10.1007/s11606-009-0948-2
- Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Project Hope). 2010;29(1):57–64. DOI:10.1377/hlthaff.2009.0629
- Mechanic R Post-acute care — the next frontier for controlling medicare spending. N Engl J Med. 2014 Feb 20;370(8):692–694. DOI:10.1056/NEJMp1315607
- Ottenbacher K, Karmarkar A, Graham J, et al. Thirty-day hospital readmission following discharge from postacute rehabilitation in fee-for-service medicare patients. JAMA. 2014;311(6):604. DOI:10.1001/jama.2014.8
- Ackerly DC, Grabowski DC. Post-acute care reform — beyond the ACA. N Engl J Med. 2014 Feb 20;370(8):689–691. DOI:10.1056/NEJMp1315350
- A data book: health care spending and the medicare program. Washington (DC): Medicare Payment Advisory Commission; 2015 [ cited 2016 May 17]. Available from: http://www.medpac.gov/documents/data-book/june-2015-databook-health-care-spending-and-the-medicare-program.pdf
- Smith L, West S, Coots L, et al. Skilled nursing facility readmission measure (SNFRM) NQF #2510: all-cause risk-standardized readmission measure – SNFRM-technical-report-3252015.pdf [ cited 2016 May 17]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/SNFRM-Technical-Report-3252015.pdf
- Ward K, Eslami M, Garcia M, et al. Do internal medicine residents know enough about skilled nursing facilities to orchestrate a good care transition? J Am Med Dir Assoc. 2014;15(11):841–843. DOI:10.1016/j.jamda.2014.08.004