ABSTRACT
Coronary artery ectasia (CAE), a variant of coronary artery anomalies, is a rare clinical entity. Although atherosclerotic coronary artery disease (CAD) is the most common cause of acute coronary syndrome (ACS), CAE also conveys a relatively high risk for potentially life-threatening cardiac events. We report a case of a 35-year-old male with two-vessel CAE, who presented with acute inferior wall ST election myocardial infarction (STEMI). After initiating medical therapy including bivalirudin, emergent percutaneous coronary intervention (PCI) with stenting of postero-lateral branch of right coronary artery (RCA) was performed. Coronary angiography also showed diffuse ectasia of RCA and left anterior descending artery (LAD). The patient tolerated the procedure well and was discharged on appropriate medical therapy. He was followed-up at one month, with no resulting cardiac events. This case highlights the importance of CAE awareness. CAE has drawn the attention of clinicians because of its clinical implications, as well as its seemingly higher prevalence, due to the abundant use of coronary angiograms and advanced cardiac imaging in the contemporary world. Albeit there has been much progress in the understanding and management of the disease, questions still remain regarding the exact pathophysiology, management guidelines and prognosis of CAE, which are worth further study.
1. Case presentation
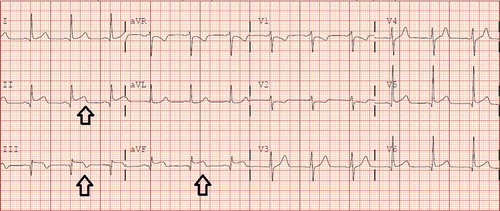
A 35-year-old, healthy male presented with acute onset of severe left-sided chest pain, which started while he was exercising at the gym. This episode was associated with diaphoresis and nausea. He denied any personal history of similar complaints or known medical problems. He also denied a family history of sudden death or congenital heart disease. The pain was significantly relieved with aspirin, nitroglycerin and morphine. Vital signs were stable and physical exam was benign including cardiac exam. The initial electrocardiogram (EKG) was not significant; however, a repeat EKG about 4-hours later showed significant ST segment elevations in the inferior leads (). Initial troponin was 0.04 ng/ml, which jumped to 97 ng/ml in about six hours. Emergent coronary angiogram was performed and revealed total occlusion at the ostium of the right posterolateral artery (RPLA) and mid-to-distal portion of right posterior descending artery (RPDA), with largely patent left coronary circulation. Diffuse ectasia of right coronary artery (RCA) and left anterior descending artery (LAD) was also discovered during angiography (, ). The obstruction at the ostium of RPLA was successfully treated with primary percutaneous transluminal coronary angioplasty (PTCA) and placement of two drug-eluting stents (2.5 × 12 mm and 2.5 × 16 mm Promus Premier DES). The procedure was uneventful with complete chest pain resolution shortly after. Transthoracic echocardiogram showed left ventricular ejection fraction of 60–65% with inferior wall hypokinesis. The patient was discharged with dual anti-platelet therapy (aspirin and prasugrel), atorvastatin, carvedilol, and lisinopril. Follow-up at one month showed no cardiac events.
Figure 1. Resting 12-lead electrocardiogram (EKG) showing ST elevation in inferior leads II, III and aVF (see the black arrows).
2. Discussion
CAE was first described by Bougon in 1812 as a post-mortem finding in a patient who died of symptoms similar to acute coronary syndrome [Citation1]. It is defined as the dilation of a coronary artery by 1.5 times the adjacent normal coronary artery. One or more of the coronary arteries can be affected. CAE can be acquired or congenital, and it has an estimated prevalence of 1.2–4.9% in several coronary angiographic studies [Citation2–Citation4]. More than 50% of cases are reportedly related to atherosclerosis. The exact link between CAE and atherosclerosis has not been well defined. Additionally, questions still linger as to why ectasia develops in some patients with atherosclerosis, while stenosis occurs in the other counterparts. The literature suggests that enzymatic degradation of the media plays a major role in pathogenesis of CAE through ‘exaggerated expansive remodeling’, which in turn is mediated by several factors in atherosclerotic process, such as lipoprotein accumulation in the intima, oxidative stress, inflammatory cell infiltration, altered nitric oxide metabolism, and reduced shear stress. Histologically, ectatic coronary arterial segments reveal the breakdown of the medial collagen and elastin components with disruption of the internal and external elastic lamina [Citation4,Citation5].
CAE may also be caused by vasculitides (Kawasaki disease, Takayasu disease), connective tissue disorders (rheumatoid arthritis), collagenopathies (Marfan’s syndrome), iatrogenic cause (coronary interventions), trauma, congenital malformations, infections (syphilis), etc. Genetic component of the etiology for CAE is still under investigation. The proximal and middle segments of right coronary artery (RCA) are the most common sites for CAE, followed by proximal left anterior descending (LAD) and left circumflex (LCx) arteries. The predilection of CAE for RCA is not clear. Markis et al. proposed classification of CAE based on the extent of anatomic involvement as below [Citation4]:
type I – diffuse ectasia of two or three vessels
type II – diffuse ectasia in ine vessel and localized in another
type III – diffuse ectasia of one vessel only
type IV – localized or segmental ectasia.
Natural history and management of the disease have not been fully understood given the scarcity of the disease. Most patients remain asymptomatic. Some may present with atypical chest pain, stable angina, or acute coronary syndrome. Patients with isolated CAE without significant coronary stenosis can still present with exertional angina, which may be explained by reduced coronary flow reserve and microcirculatory dysfunction in the dilated segment of a coronary artery [Citation6]. Zografos et al. observed that the topographical extent of ectasia is associated with clinical presentation independent of co-existing CAD. The study also concluded that ‘isolated CAE should be considered as suffering conventional CAD’ [Citation7].
The definitive diagnosis is made by coronary angiography, which can also assess the degree of ectasia and the number of involvement of coronary arteries. Intracoronary ultrasound can be used to differentiate a true aneurysm (all three layers of a vessel wall) from a pseudo-aneurysm (disrupted integrity of a vessel wall). Alternatively, non-invasive coronary computed tomography angiography (CCTA) and coronary magnetic resonance angiography (CMRA) may also be used for further exploration [Citation8–Citation10]. Our patient has type I CAE with diffuse ectasia of proximal RCA and proximal LAD. The patient presented with inferior wall myocardial infarction from occlusion of RPLA at the ostium, which was appropriately treated. After discussion, medical management is opted for further care.
Controversies remain regarding the definitive treatment plan and prognosis for CAE. Generally, lifestyle modification to optimize the modifiable risk factors is recommended for all CAE patients due to the association of the disease with coronary atherosclerosis. When co-existing with CAD, the prognosis and treatment of CAE are the same as for CAD alone. Prognosis is better in isolated CAE and anti-platelet therapy is the mainstay of treatment recommended. Myocardial infarction in CAE is often caused by thrombosis within the ectatic coronary lesions with subsequent distal embolism [Citation8,Citation9]. Thrombus formation is attributable to stagnation of coronary flow and reduction of shear stress in the enlarged coronary segment [Citation11]. Some authors suggest anticoagulant therapy to prevent thrombus formation, but this recommendation has not been supported by clinical trials. Nitrates tend to exacerbate myocardial ischemia due to ‘coronary steal phenomenon’ and are not recommended [Citation9]. Cardiac events in CAE may also be caused by coronary spasm, for which medications with vasodilating properties have been proposed [Citation10,Citation12].
In the setting of acute coronary syndrome, thrombolytic therapy may be used for recanalization. However, percutaneous coronary intervention (PCI) is preferable for reperfusion therapy especially for those with double disease burden (co-existent CAE and CAD). Stenotic lesions adjacent to ectatic arteries can be a challenge for selection of an optimal stent size and adequate apposition. Intracoronary ultrasound may be used to help determine the stent size. Nonetheless, extra care must be taken to ensure adequate stent expansion and wall apposition [Citation8,Citation13]. Surgical treatment is reserved for those with multi-vessel diffuse ectasia or refractory symptoms despite optimal conservative medical therapy and those with serious adverse events (coronary artery rupture or dissection). Surgical options include aneurysm ligation, aneurysmectomy and coronary artery bypass grafting (CABG) [Citation14,Citation15]. Our patient was treated conservatively with medical therapy and his one month follow-up showed a favorable outcome.
3. Conclusion
In summary, CAE is one of the rare coronary artery anomalies. It can present with potentially life-threatening cardiac events. This case highlights the importance of CAE awareness, a potential risk factor for acute myocardial infarction. Therefore, a low threshold of suspicion for CAE should be maintained in patients with acute coronary syndrome. Albeit there has been much progress in the understanding and management of the disease, questions still remain regarding the exact pathophysiology, management guidelines, and prognosis of CAE, which are worth further study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Jarcho S. Bougon on coronary aneurysm (1812). Am J Cardiol. 1969;24:551–553.
- Syed M, Lesch M. Coronary artery aneurysm: a review. Prog Cardiovasc Dis. 1997;40:77.
- Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation. 1983;67:134–138.
- Markis JE, Joffe CD, Cohn PF, et al. Clinical significance of coronary arterial ectasia. Am J Cardiol. 1976;37:217–222.
- Antoniadis AP, Chatzizisis YS, Giannoglou GD. Pathogenetic mechanisms of coronary ectasia. Int J Cardiol. 2008;130(3):335–343.
- Akyurek O, Berkalp B, Sayin T, et al. Altered coronary flow properties in diffuse coronary artery ectasia. Am Heart J. 2003;145(1):66–72.
- Zografos, TA, Korovesis S, Giazitzoglou E, et al. Clinical and angiographic characteristics of patients with coronary artery ectasia. Int J Cardiol. 2013;167(4):1536–1541.
- Devabhaktuni S, Mercedes A, Diep J, et al. Coronary artery ectasia - A review of current literature. Curr Cardiol Rev. 2016;12:318–323.
- Eitan A, Roguin A. Coronary artery ectasia: new insights into pathophysiology, diagnosis, and treatment, Coron. Artery Dis. 2016;27:420e428.
- Mavrogeni S. Coronary artery ectasia: from diagnosis to treatment. Hellenic J Cardiol. 2010;51(2):158–163.
- Kuramochi Y, Ohkubo T, Takechi N, et al. Hemodynamic factors of thrombus formation in coronary aneurysms associated with Kawasaki disease. Pediatr Int. 2000;42:470–475.
- Sorrell VL, Davis MJ, Bove AA. Origins of coronary artery ectasia. Lancet. 1996;347:136–137.
- Ozcan OU, Gulec S. Coronary artery ectasia. Cor Et Vasa. 2013;55(3):e242–e247.
- Vijayanagar R, Shafii E, DeSantis M, et al. Surgical treatment of coronary aneurysms with and without rupture. J Thorac Cardiovasc Surg. 1994;107:1532–1553.
- Harandi S, Johnston SB, Wood RE, et al. Operative therapy of coronary arterial aneurysm. Am J Cardiol. 1999;83:1290–1293.